Introduction
The term double burden of malnutrition (DBM) refers to the simultaneous occurrence of undernutrition and overnutrition (overweight and obesity) in the same individuals, households, and populations at the national and international levels throughout the life course.(Reference Gavin-Smith, van Zutphen and Kraemer1) It may, for instance, manifest at the individual level as obesity accompanied by a vitamin or mineral deficiency or as overweight adulthood following childhood stunting. Similarly, it could show up as an overweight or anaemic mother with underweight children or grandparents at the household level. The prevalence of both undernutrition and overweight/obesity can occur in the same community, country, or region when it occurs at the population level.(Reference Gavin-Smith, van Zutphen and Kraemer1–Reference Shimpton and Rokx3)
According to the WHO, adolescence is the age between 10 and 19 years and serves as a transition between childhood and adulthood.(4) Due to accelerated growth and development, it is a crucial time in a person’s life after infancy.(Reference Azzopardi, Hearps and Francis5) It is also a time when higher food intake is necessary for their rapid growth as a result of developmental changes.(Reference Das, Salam and Thornburg6,Reference Nicholson, Fawzi, Canavan and Keshavjee7)
Multiple types of malnutrition are experienced and faced by all of the global countries at all levels of development and socio-economic status.(8,9) Especially in the previous three decades, different regions of the world have experienced accelerated and varying degrees of dietary change. Moreover, the nutrition transition occurred with different changes in health, epidemiologic, demographic, and socio-economic factors coupled with dietary and activity pattern changes. This shift leads to highly increased overnutrition and diet-related non-communicable diseases (DR-NCDs) in addition to the already existing undernutrition and micronutrient deficiency.(Reference Gavin-Smith, van Zutphen and Kraemer1) The common driving forces of DBM were early-life nutrition, diet quality, biology-related factors, epigenetics, food environments, food systems, socio-economic factors, and poor governance.(8,10–Reference Wells, Sawaya and Wibaek12) Of these, four are the most modifiable drivers for multiple forms of malnutrition. These are dietary quality, early-life nutrition, socio-economic factors (e.g. poverty, poor educational status, poor occupational status), and food environments (e.g. lack of nutritious foods, increased availability packed foods in the market, processed foods).(Reference Wells, Sawaya and Wibaek12,Reference Popkin, Corvalan and Grummer-Strawn13)
Globally, nearly a quarter of adolescents worldwide are undernourished and overweight, and obesity is increasing rapidly in nearly every country of the globe.(Reference Gavin-Smith, van Zutphen and Kraemer1,14) In summary, various studies conducted among adolescents worldwide have revealed that the prevalence of DBM ranges from 2.7% to 73.33%. Specifically, the prevalence of thinness ranges from 3% to 39.4%, overweight ranges from 5.9% to 65%, and obesity ranges from 2.7% to 73.33%.(Reference Tanwi, Chakrabarty and Hasanuzzaman15–Reference Massad, Deckelbaum, Gebre-Medhin, Holleran, Dary and Obeidi19) In African countries, the prevalence of DBM varies significantly. The prevalence ranges from 1.8% to 25%, with specific rates for thinness, overweight, and obesity ranging from 6.3% to 11.2%, 2.2% to 25%, and 1.8% to 6.1%, respectively.(Reference Erismann, Knoblauch, Diagbouga, Odermatt, Gerold and Shrestha20–Reference Musa, Toriola, Monyeki and Lawal25) Similarly, in Ethiopia, various studies conducted in the country report the prevalence of DBM ranging from 2.39% to 55.0%. Specifically, the prevalence of thinness ranges from 4.7% to 55.0%, overweight ranges from 3.3% to 20.6%, and obesity ranges from 2.39% to 4.7.(Reference Berbada, Haidar, Gebremichael and Haftu26–Reference Getacher, Ademe and Belachew35)
To end widespread hunger and eradicate all forms of malnutrition, the UN Decade of Action on Nutrition aims to intensify actions within the global agenda of Sustainable Development Goals (SDGs). This effort addresses both undernutrition and overnutrition. The SDGs 1 (‘end poverty’) and 2 (‘end hunger, achieve food security and improved nutrition’) are directly related to tackling DBM. Target 1.1 aims to eradicate extreme poverty by 2030, and target 2.2 aims to end all forms of malnutrition by 2030. Progress towards these goals is slow and uneven, making timely achievement unlikely. Furthermore, the progress to achieve the 2012 global nutrition targets is very slow and unfair. The achievement of these objectives is highly unlikely in the next few years before that date without a miracle.(Reference Gavin-Smith, van Zutphen and Kraemer1,14,36–Reference Hawkes, Ruel, Salm, Sinclair and Branca38)
With regard to the nutritional interventions implemented to reduce the effect of DBM, several studies have shown that nutritional interventions are effective in reducing nutrition-related problems.(Reference Bhutta, Das and Rizvi39,40) Although different forms of malnutrition can coexist simultaneously in lower- and middle-income countries (LMICs), most previous nutrition interventions targeted only one form of malnutrition, which is undernutrition.(11,Reference Hawkes, Ruel, Salm, Sinclair and Branca38,Reference Hawkes, Demaio and Branca41) The 2018 WHO guidelines recommend evidence-informed interventions and policies for adolescent nutrition.(4) Among the most essential nutritional interventions are (1) promoting healthy diets in adolescents, (2) preventing adolescent pregnancy and poor reproductive outcomes, (3) promoting preconception and antenatal nutritional care in adolescents, (4) providing access to a safe environment and hygiene for adolescents, (5) promoting physical activity in adolescents, and (6) preventing and managing disease in adolescents. Moreover, the 2017 WHO policy brief and the 2020 Lancet Series on the DBM highlight that overweight and obesity are forms of malnutrition that now coexist with the persistent problems of nutritional deficiencies in most countries around the world, especially in LMICs, forming a ‘new nutrition reality’ that will require new interventions, strategies, programmes, and policies to successfully tackle it.(11,Reference Getacher, Ademe and Belachew31,Reference Hawkes, Ruel, Salm, Sinclair and Branca38,Reference Hawkes, Demaio and Branca41,Reference Pradeilles, Baye and Holdsworth42)
Double-duty interventions (DDIs) are interventions that have the potential to simultaneously tackle the burden of both undernutrition and overnutrition in a comprehensive manner.(11,Reference Ruel and Hawkes43,Reference Hawkes44) These interventions can be achieved in three ways. First, by not harming the existing interventions for malnutrition. Second, through retrofitting the existing intervention to address all types of malnutrition. Third, through the development of de novo integrated interventions (starting from the beginning, anew, or a new) aimed at the DBM.(11,Reference Hawkes, Ruel, Salm, Sinclair and Branca38,Reference Hawkes, Demaio and Branca41) Selected DDIs applied in this study were optimised through strong education and nutrition behaviour change communication (NBCC) focused on promoting healthy diets (adequate adolescent nutrition, dietary diversity), physical activity (performing proper physical exercise, avoiding sitting for long time), preventing undue harm from energy-dense foods (avoiding junk processed foods, avoiding sugar-sweetened drinks, street fast foods, chips, salt, sugar, etc.), and regulations on marketing foods from the customer side (e.g. buying packed foods frequently).(11,Reference Hawkes, Ruel, Salm, Sinclair and Branca38,Reference Hawkes, Demaio and Branca41)
Previously, actions applied to address undernutrition and overnutrition were developed and delivered separately, and they are still isolated from each other. Unintentionally, as some evidence has shown, programmes that address undernutrition have increased risks for obesity and DR-NCDs, especially in LMICs, where food environments are changing rapidly. Until now, different countries of the world, including Ethiopia, have failed to consider these risks in their policies and interventions.(Reference Hawkes, Ruel, Salm, Sinclair and Branca38) In contrast, DDIs can simultaneously tackle the risk of both nutritional deficiencies leading to stunting, underweight, or micronutrient deficiencies and obesity or DR-NCDs by the same intervention. These interventions assume that all forms of malnutrition share common determinants that can be addressed through interventions that have a double impact in a holistic approach.(11,Reference Hawkes, Ruel, Salm, Sinclair and Branca38)
Evidences show that theory-based behavioural theories are very effective for the acceptance of the intervention.(Reference Glanz and Bishop45,Reference Hagger and Weed46) Among the effective behavioural theories health belief model (HBM) is one of them. The HBM comprises six theoretical constructs assessing individuals’ health behaviours: perceived susceptibility, severity, benefits, barriers, cues to action, and self-efficacy. This study evaluates adolescents’ perceptions regarding these constructs in relation to DBM. It examines how dietary intake impacts the DBM risk, the consequences of dietary habits on DBM outcomes, views on dietary improvements and physical activity, obstacles to nutritional enhancement, cues prompting action, and confidence in adopting healthy behaviours to improve nutritional status. However, previous studies conducted on the reduction of malnutrition did not use theory-based behavioural theories among adolescents. Hence, to boost the acceptance of the DDIs in the study area, this study applied HBM to reduce DBM. Moreover, there is a gap in interventional research, policies, and actions related to DBM among adolescents and its consequences on their health, nutritional status, frequency of morbidity, and linear growth in developing countries such as Ethiopia.(Reference Getacher, Ademe and Belachew31,Reference Getacher, Ademe and Belachew35) Most of the studies are cross-sectional with insufficient evidence on DBM. In addition, most studies conducted on the relationship between DBM and its negative effects on adolescent health were mostly from most affluent and moderately affluent countries.(Reference Taklual, Baye, Mekie and Andualem34,Reference Alamu, Eyinla, Sanusi and Maziya-Dixon47–Reference Mekonnen, Birhanu, Menber, Gebreegziabher and Belay50) Therefore, the main objective of this study was to examine the effect of selected DDIs on the DBM among secondary school adolescents in Debre Berhan City, Central Ethiopia, 2022/23.
Methods and materials of the study
Study area, period, and design
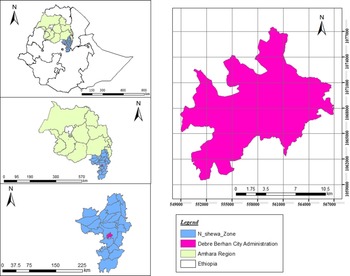
This study was conducted in Debre Berhan Regiopolitan City, North Shoa Zone, Amhara Region, Central Ethiopia (Fig. 1). The city is 690 km far from Bahir Dar (the seat of the Amhara region) and 130 km from Addis Ababa (the capital of Ethiopia). It is the capital city of the North Shoa Zone of the Amhara region and was built by Emperor Zara Yakoob. The coordinates for the city are 9°41′N and 39°32′E. This study was conducted from 13 October 2022 to 30 June 2023, using a 9-month two-arm parallel design school-based cluster randomised controlled trial considering schools as a unit of randomisation.
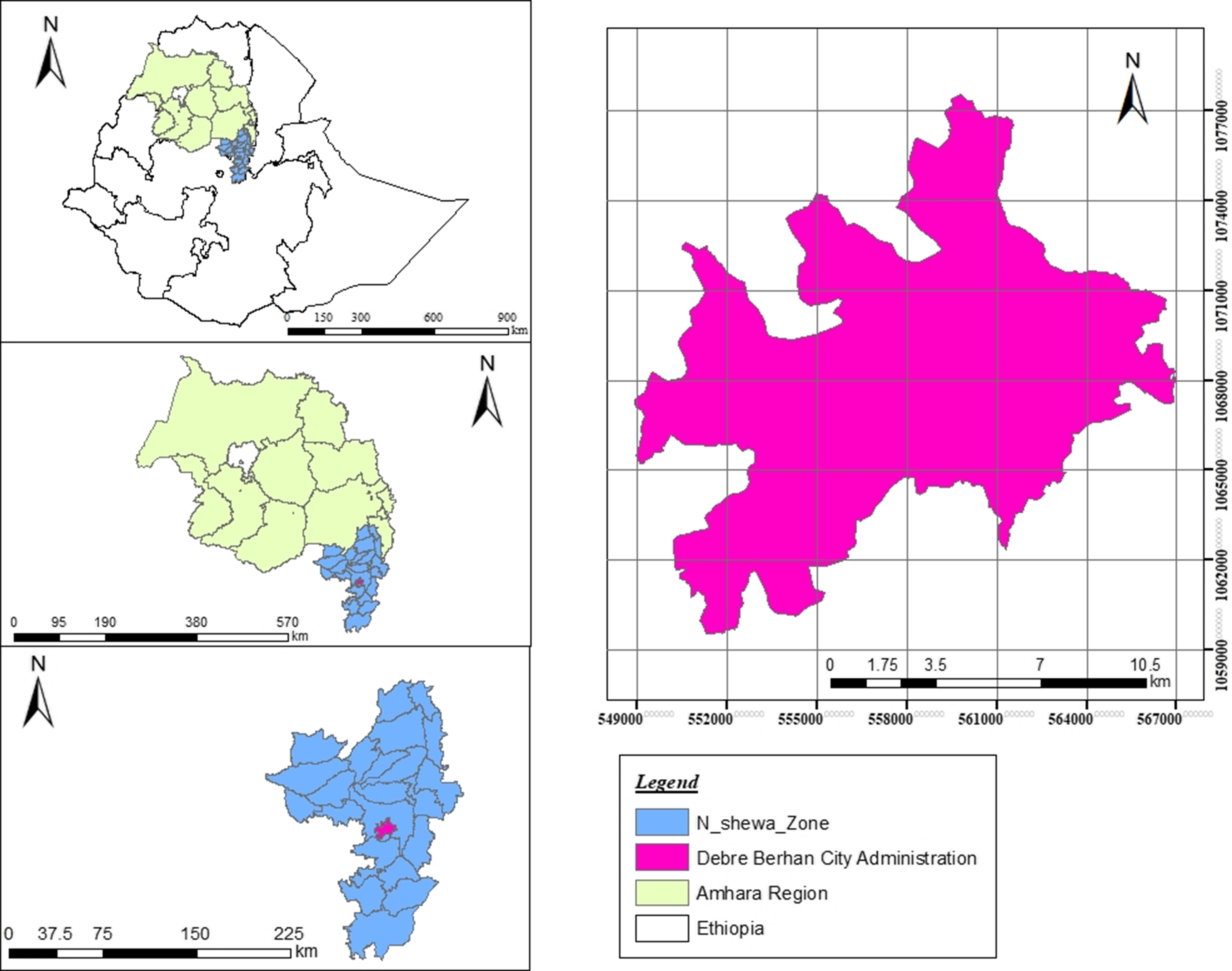
Figure 1. Map of the study area (Source: Municipal of Debre Berhan City administration).
Study population, eligibility criteria, and sample size determination
The source population of the study was all secondary school adolescents in the city, whereas the study population was all adolescents in six selected clusters of the city during the study period. The inclusion criteria were adolescents who had followed their teaching learning process in the selected schools and who had no intention of leaving the schools until the end of the study. Regarding the exclusion criteria, adolescents who were not able to respond to an interview due to not choosing to participate or illness and who had physical disabilities, including deformities such as kyphosis, scoliosis, and limb deformities that prevent them from standing erect, were excluded from the study.
The sample size was calculated using the G power 3.1.9.2 programme with a power of 80.5% for Fisher’s exact test (proportions for inequality and two independent groups) using a double proportion formula, a precision (alpha) of 5%, a 10% loss to follow-up, a design effect of 2, and proportions of indicators of DBM (P0 = 15.8%(Reference Hadush, Seid and Wuneh51) and P1 = 6.2%(Reference Gebreyohannes, Shiferaw, Demtsu and Bugssa28)). Thus, the calculated sample size was 648. Thus, 324 children in the intervention group (IG) and 324 children in the control group (CG) were enrolled with an allocation ratio of one. However, due to the cluster sampling method, the final sample size used for the study was 745. Of these, at baseline measurement, 742 adolescents (IG = 375, CG = 367) received complete information and were randomly assigned to intervention and control groups. At end-line measurement, 708 respondents (IG = 356, CG = 352) were included in the study.
Sampling techniques, randomisation, and recruitment
A multistage cluster sampling technique was applied to select adolescents from respective secondary schools in the Debre Berhan Regiopolitan City (DBRPC), which were divided into five sub-cities and thirty-seven kebeles. There are ten schools in the city. Of these schools, eight are government and two are private schools. Using a simple random sampling method, six secondary schools were selected from ten schools randomly and allocated into intervention and control groups using a randomisation table. The number of adolescents in each selected cluster was taken from all these school documentations. For the data collection and providing the interventions, sections were used in the selected schools. When an eligible study participant was absent during the first visit, a revisit was conducted three times. They were considered nonresponsive if the study participants were absent in three visits. Schools in the city were considered as clusters for the unit of randomisation instead of individuals to prevent contamination of message of the intervention as well as for better logistical suitability. To avoid information contamination, nonadjacent kebeles that contained these schools were randomly assigned into intervention and control groups using a simple random method.
Intervention packages of the study
The packages of the DDIs were modified and adapted from the 2017 WHO policy brief report and Hawkes et al..(Reference Hawkes, Ruel, Salm, Sinclair and Branca52) These interventions were delivered through robust NBCC focused on the promotion of healthy diets (adequate adolescent nutrition, dietary diversity), physical activity (do moderate intensity physical exercise, avoiding sitting for a long time), prevention of undue harm from energy-dense foods (avoiding junk processed foods, avoiding sugar-sweetened beverages, street fast foods, chips, salt, sugar, fats, etc.), and regulations on marketing foods from the customer side point of view (e.g. avoiding buying packed foods frequently).(11,Reference Hawkes, Ruel, Salm, Sinclair and Branca52)
In a school-based setting, an NBCC tool using a theory-based HBM was used to deliver the intervention packages of this study in the sections of selected schools through multimodal approaches. The interventions were provided for secondary school adolescents within the selected intervention schools, particularly in the selected section of the students. Each adolescent had at least twelve contacts through multimodal approaches (NBCC through direct contact in the class of students, school media and health clubs established in each school, brochure, message text, and phone call). The first contact was cluster-based NBCC, nutrition education, and nutrition counselling on the core points of the intervention package through school visits. During this communication, a client-centred communication approach was used to recognise the nutritional problems of adolescents in the study area. After the first contact, a one-page brochure was prepared in the local language (Amharic) with the core messages of the intervention package and delivered for each of the IG adolescents to take home. For data collection and measurement, the data were collected and measured from selected adolescents.
Nutrition educators and communicators considered the adolescents’ identified gaps during baseline data collection affordable, acceptable, and available diets and dietary recommendations. NBCC was delivered every 2 months (at the first, third, fifth, and 7 months) throughout the study period using NBCC tools. On average, each communication took 60–90 min at the cluster level. The communications and intervention packages were given after the baseline data collection had finished. The communication was focused on school adolescents’ nutrition, physical activity, control of highly energy-dense and junk foods, control of purchased market foods, and causes, effects, and consequences of DBM. The study participants were reminded of the key mottos of the interventions highlighted during the training through text messages every 2 months and phone calls every 2 months. However, the CG received the standard care given by the health care system. The compliance of the intervention was measured by the number of participants who attended the NBCC, number of participants who received the message, number of participants who received the phone call, and number of participants who received the leaflet, frequency, and attendance of participants for the training sessions (Supplementary file 1).
Data collection methods, procedures, and measurements
Data collection methods and procedures
To collect the required data for this study, a pretested and structured interviewer-administered questionnaire was used. It was first organised in the English language and delivered in a face-to-face approach in the class of respondents. To easily run the data collection process, this questionnaire was translated into the language spoken in the study area (Amharic) by language experts. Then, to retain its reliability, it was translated back to English by an independent language expert for both languages. A digital system data collection using a Kobo toolbox tool was performed. Twelve and six health professionals (nurses and health officers) were the data collectors and supervisors of the study, respectively.
The questionnaire included questions related to the dependent variable, which is the double burden of malnutrition (DBM). Additionally, the questionnaire addressed several independent variables such as sociodemographic factors, dietary practice, home garden practice, meal frequency, and HBM theoretical constructs. The HBM constructs included perceived susceptibility to DBM, perceived severity of DBM, perceived benefits of preventing DBM, perceived barriers to preventing DBM, cues to action, and self-efficacy for the prevention of DBM. The questionnaire also includes about DDI packages. Sociodemographic data were collected at baseline to establish the initial context. Questions related to adolescent dietary practices, HBM theoretical constructs, and anthropometric measurements were assessed at both baseline and end-line periods to assess changes over time and evaluate the impact of the interventions.
The nutrition behaviour change communicators and supervisors of the nutrition communication process were six bachelor’s degree nutritionists and three master’s degree nutritionists, respectively. Based on their previous nutrition communication experience, nutrition communicators and supervisors were selected for communication services. Before the actual data collection, they participated in a 3-d exhaustive training with fieldwork and role-playing activities. The training was focused on the data collection procedures, intervention packages, tools, objectives of the study, and ethical issues using a training manual prepared by the research team. In addition, to preserve workers relieved of consistent measures over time after 3 months of intervention enactment, a 1-d extra training was given for both nutrition communicators and supervisors.
Measurements
The weight of secondary school adolescents was measured to the nearest 0.1 kg using a calibrated portable electronic digital scale with the participants’ shoes taken off and wearing light clothes (Seca Germany Brand). A known object weight was used to check the validity of the scale between the measurements and every morning. A CV of less than 0.03 (<3%) was performed for the standardisation of the anthropometrists. Furthermore, the height was measured to the nearest 0.1 cm using a portable wooden height-measuring board with a sliding head bar following standard anthropometric techniques with the shoe removed. The participants were positioned at the Frankfurt Plane. Moreover, the four points (shoulder, calf, heel, and buttocks) touched the vertical stand, and their shoes were taken off. Calibration rods were used to check the stadiometer before starting the measurement. All anthropometric measurements were collected in duplicate, and the average values were used for analysis if there were variations in measurements.
The WHO AnthroPlus software was employed for the analysis of anthropometric data. Through the application of this software, the outcome variable was categorised into three groups (thinness, normal weight, and overweight/obesity). Thinness was categorised as having a z-score less than –2, while overweight/obesity was categorised as having a z-score greater than +1. The Wealth Index was derived using principal component analysis, which considered various household assets such as domestic animals, durable assets, and housing characteristics. Subsequently, the variable was categorised into three groups: poor, medium, and rich. Home garden refers to the cultivation of vegetables and fruits within the participants’ compound. It was assessed using a single question: ‘Do you have a home garden in your compound? The meal frequency was assessed based on how often participants reported eating meals within a 24-h period.
Data quality control and intervention fidelity
Data quality control
To maintain the quality and reliability of the questionnaire, pretest, retranslation, and contextualisation of the adapted and further developed English language version questionnaire into the Amharic language version were performed by an Amharic language speaker who qualified in the Amharic language. Again, retranslation back to the English language was done by a person who qualified in the English language. To retain the consistency of the two versions, a comparison was made. The data collection was carried out using the translated and pretested Amharic version questionnaire. After the pretest was completed, the questionnaire was further modified. All the details of the study were informed by the interviewers during data collection. Data collectors were trained for 3 d lasting 4 h for each session in the morning and afternoon on the objective of the study, manner of data collection, data collection tools, and the pattern of how each variable on the questionnaire is measured. There was also a practical session and actual demonstration on how to interview and take anthropometric measurements.
A standardisation exercise was conducted for anthropometric measurements to reduce interobserver error. The relative technical error of measurement (% TEM) was calculated to minimise random errors in these measurements. Data collectors’ accuracy in taking anthropometric measurements was standardised with their trainer during training and pretesting. For each adolescent, two separate height and weight measurements were taken, and if the variation between the two measurements exceeded 0.1 kg for weight or 0.1 cm for height, the measurements were repeated. The functionality of digital weight scales was verified each morning using a known weight before data collection began. Additionally, before every weight measurement, data collectors ensured that the scale reading was exactly at zero. School adolescents were encouraged to feel comfortable during the interview, and interviewers were informed about the confidentiality of the responses, assuring participants that their information would not be shared beyond the research team. Adolescents who were willing to participate and had signed informed consent documents from their parents or guardians, along with their own assent forms, were then interviewed.
Intervention fidelity
To assess the fidelity of the DDI, criteria were set up according to the National Institutes of Health Behavioural Change Consortium recommendations.(Reference Bellg, Resnick and Minicucci53) The fidelity criteria included checklists to assess the DDI design, training of nutrition behaviour change communicators, process of NBCC, receipt of the interventions, and enactment of skills gained from the DDI.(Reference Murphy and Gutman54–Reference Demilew, Alene and Belachew60)
The DDI design had a theoretical background to be implemented in this study.(Reference Hawkes, Demaio and Branca41,Reference Hawkes44,61) In this study, for both the intervention and control arms, equal numbers of clusters were taken from each cluster to balance the variations between different clusters in the city. Moreover, to overcome the possibility of information contamination between clusters, nonadjacent kebeles that contain the schools were selected by creating a buffer zone between adjacent clusters. In addition, the trial used a CG to compare the effectiveness of the DDIs. Furthermore, the intervention process was pretested in an area other than the study area with a similar set-up before the application of the actual trial. In addition, each cluster received equivalent numbers and frequencies of NBCC. Additionally, to make the process homogenous, the lengths of interactions within an IG were comparable and analogous.
Nutrition behaviour change communicator training was prearranged and provided in a group using a training manual, role-playing, demonstrations, and mock communication practice. The knowledge and skill of communicators were assessed using practical evaluation and before and after training tests. The process evaluator evaluated the communication sessions by randomly selecting for process evaluation, and all selected sessions were evaluated. The process evaluator rated the communicator using a ‘yes/no’ rating system on items such as using a communication guide, provision of the whole content, duration and frequency of communication, preparedness, accuracy, and ability to properly respond to questions.
Intervention receipt was assessed using checklists on the knowledge of the secondary school adolescents on DDI packages through interviewing about their understanding of the core contents of the intervention. Intervention enactment was also assessed using the checklist on a demonstration of food preparation and consumption of the adolescents.
Due to the nature of the DDIs, participant allocation concealment was not possible. However, data collectors, participants, and intervention providers were blinded to the study hypotheses. In addition, by using and labelling a nonidentifiable unique number, the data entry clerk was blinded until data analysis was finalised. The communication process was supervised by the supervisors and principal investigator. An interim analysis was performed to see the status and effect of the intervention. The trial was terminated since the predicted outcome was met and statistically valid experiments were obtained via statistical tests and adjusted models.
Data management and analysis methods
The principal investigator conducted a visual inspection of all the completed questionnaires to ensure they were complete and consistent. Data collection was carried out using the Kobo toolbox online tool, and the collected data were exported to SPSS version 25 for cleaning, which involved addressing missing values and outliers before proceeding with the analysis. Simple descriptive statistics, such as simple frequency distribution, mean (standard deviation), and percentages were employed to summarise the demographic, socio-economic, and adolescent-related characteristics of the participants. For continuous data, normality assumptions were assessed using various methods, such as histograms, mean, median, mode, and Kolmogorov–Smirnov test, which was chosen due to the sample size being greater than 50.
To compare and contrast the baseline characteristics of the intervention and control groups, a chi-square test was conducted. Anthropometric measurements within the intervention and control arms were compared using paired and independent t tests, respectively. The analysis included all study respondents who followed the predetermined protocol and guidelines. The final analysis included adolescents who actively participated in all organised gatherings and provided end-line data, constituting a per-protocol analysis. The model fitness (goodness of fit) was assessed using the quasi-likelihood under the independence model criterion.
The difference-in-difference (DID) analysis between the intervention and control arms was compared using a McNemar test. Moreover, a generalised estimating equation (GEE) model was employed to evaluate the impact of the DDI on the outcomes of interest over time, which accounts for the correlation between repeated measurements (before and after interventions) and the clustering of data within subjects. The model utilised a multinomial probability distribution, which is suitable for analysing data with multiple nominal outcome categories. The multinomial categories of the outcome variable were thinness (undernutrition), normal, and overweight/obesity (overnutrition). To determine the relationship between the intervention and the outcomes, a cumulative logit link function was used. This link function allows for the modelling of nominal response variables, such as the different categories of DBM status in this study. In addition, an exchangeable working correlation structure was employed within the GEE model. The exchangeable structure assumes that the correlations between repeated measurements within the same cluster (e.g. participants within the same school) are equal. This structure accounts for the potential correlation between observations within the same cluster and helps to adjust for the clustering effect in the analysis. Furthermore, the model was adjusted for variables including time of measurement (baseline and end line), group (intervention and control group), the interaction between time of measurement and IG (i.e. end-line measurement*IG), sex of adolescents, home garden practice, father’s educational status, residence, and alcohol use. The interaction between time (baseline and end line) and intervention was used to assess the effect of the intervention on DBM. Adjusted ORs with corresponding 95% CIs were calculated. Statistical significance was defined as results with P values less than 0.05.
Results
Sociodemographic characteristics of the respondents
In this investigation, 745 study participants were enrolled during the baseline data collection. At the baseline measurement, 742 (IG = 375, CG = 367) adolescents were provided full information and randomly assigned to the intervention and control groups. At the end-line measurements, 708 (IG = 356, CG = 352) respondents strictly adhered to the protocol. During the baseline data investigation, there was no significant variation between the intervention and control groups’ baseline sociodemographic characteristics (P > 0.05) (Table 1). The detailed baseline sociodemographic characteristics of the respondents were published before.(Reference Getacher, Ademe and Belachew31) The results of this trial were reported using Consolidated Standards of Reporting Trials (CONSORT) guidelines(Reference Schulz, Altman and Moher62,Reference Campbell, Piaggio, Elbourne and Altman63) (Fig. 2).
Table 1. The baseline sociodemographic characteristics of adolescents in the intervention (n = 375) and control (n = 367) groups in Debre Berhan City, 2022/23

* Tigrai, Gurage.
** Pagan.

Figure 2. Schematic presentation of the sampling procedure for the participant selection process based on CONSORT guideline criteria.
Comparison of HBM constructs before and after the intervention
An independent and paired sample t tests were conducted to compare the six HBM constructs of adolescents about DBM between and within intervention and control groups. The scores of the HBM constructs among the IG improved significantly (P < 0.05) from baseline to end-line visits compared to the CG. Except for perceived susceptibility and self-efficacy, there was no visible change in the HBM constructs at the baseline measurements (Table 2). In this study, the correlation between HBM construct scores and BAZ (BMI-for-age z scores) was compared both within and between the intervention and control groups. Adolescents in the IG outperformed those in the CG and their baseline scores in terms of their HBM construct scores (P < 0.05). All HBM components showed a significant positive connection with BAZ after the intervention was implemented (P < 0.05) (Table 3).
Table 2. The comparison of the health belief model (HBM) construct scores within and between the intervention and control groups among school adolescents in Debre Berhan City, Ethiopia, 2022/23
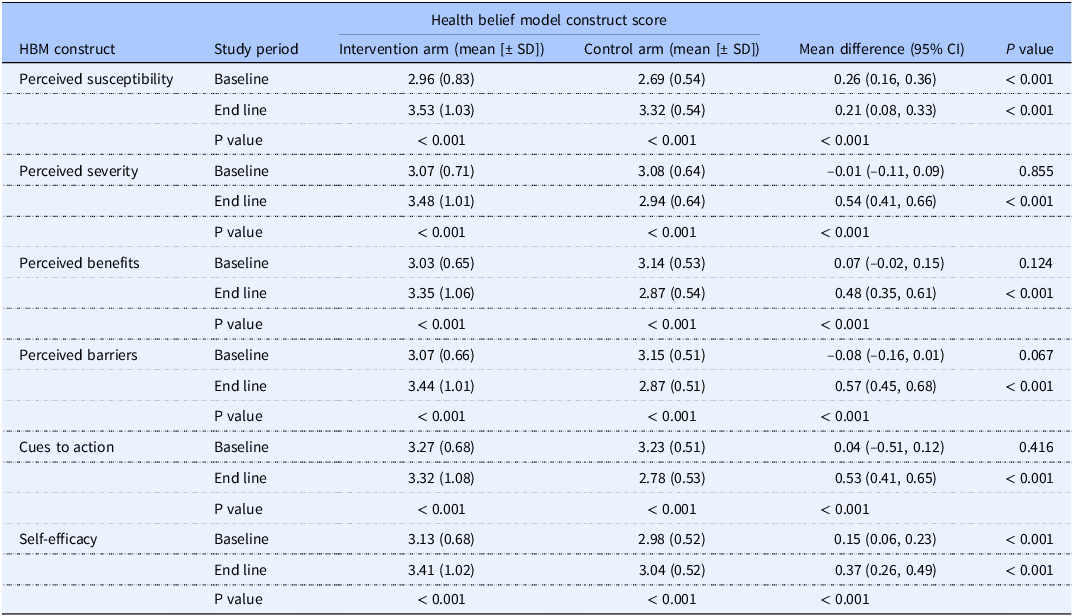
Table 3. Correlations between BAZ and HBM constructs among school adolescents in Debre Berhan City, Ethiopia, 2022/23
BAZ, BMI-for-age z-score; HBM, health belief model.
* Correlation is significant at the 0.05 level (2-tailed).
** Correlation is significant at the 0.01 level (2-tailed).
Effect of double-duty interventions on DBM among adolescents
Effect interventions on DBM using difference-in-difference (DID) analysis
Adolescents in the IG had lower DBM status because of the DDI than those in the CG. In the IG at the end-line measurement, the overall prevalence of DBM among the IG was decreased by 6.9% in the study area using the McNemar test. More specifically, thinness was decreased by 4.7%, and overnutrition was reduced by 2.2% compared to the CG (P < 0.05) (Table 4)
Table 4. The difference-in-difference analysis of double burden of malnutrition (DBM) by time of measurements and groups among adolescents in Debre Berhan City, Ethiopia, 2022/23
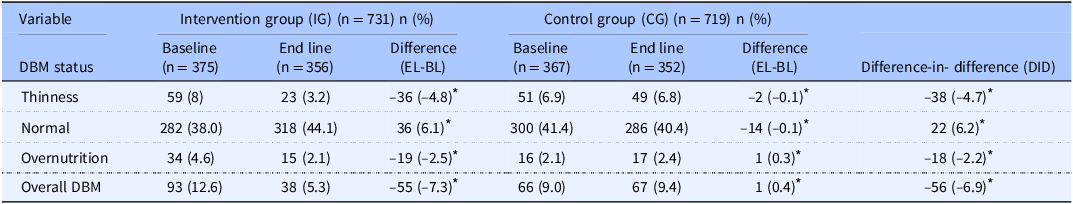
* P < 0.005, DID = IG-CG
Effect interventions on DBM using the GEE model
At the end of the measurement, adolescents in the IG showed a substantial improvement in their nutritional status. After adjusting for potential confounders, the multivariable GEE model analysis revealed that adolescents in the IG had a 67% lower proportion of being thinness (AOR = 0.33, 95% CI [0.21, 0.53]) and 49% lower proportion of being overweight/obese (AOR = 0.51, 95% CI [0.32, 0.82]) than those in the CG. In addition, adolescents in the IG were 34% less likely to have DBM (thinness and overnutrition) than those in the CG (AOR = 0.66, 95% CI [0.46, 0.94]). Besides, the likelihood of DBM decreased by nearly 60% (AOR = 0.41, 95% CI [0.03, 0.92]) among adolescents at the end-line measurement compared to the baseline. Similarly, adolescents in the time-group interaction were 44% less likely to have higher DBM status (AOR = 0.56, 95% CI [0.02, 0.38]) compared to their counterparts (Table 5).
Table 5. Modelling the effect of intervention on DBM using generalised estimating equation modela among adolescents in Debre Berhan City, Ethiopia, 2022/23
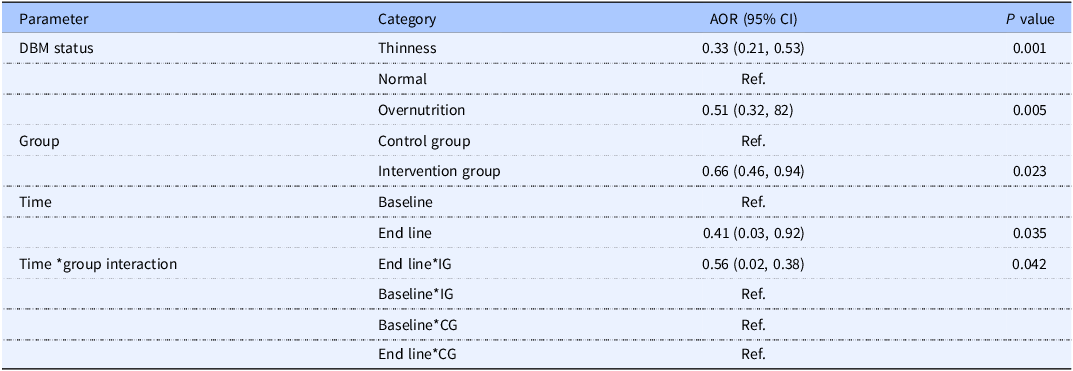
AOR, adjusted OR; DBM, double burden of malnutrition; Ref., reference category; IG, intervention group; CG, control group.
a The model was adjusted for various variables such as meal frequency, home garden practice, age, sex of adolescent, father’s education, residence, alcohol use, etc.
Discussion
This study employed the impact of selected DDI packages on DBM using an HBM to boost the acceptance of the intervention among adolescents in the study area. In the IG at the end-line measurement, the overall prevalence of DBM was reduced compared to the baseline measurements. Moreover, adolescents in the IG demonstrated a significant improvement in their nutritional status than the CG.
In DID analysis, when compared to adolescents in the CG, the proportion of adolescents who had DBM was considerably lower in the IG. Adolescents in the IG saw a nearly 5% decrease in thinness and more than 2% decrease in overnutrition. The total prevalence of DBM within the IG had dropped by almost 7% compared to the control arm. This result was in line with different studies performed elsewhere. Different forms of malnutrition were the focus of a systematic review conducted in LMICs, which consolidated the evidence on the impact of interventions on adolescent nutrition and educational outcomes.(Reference Shinde, Wang, Moulton and Fawzi64) Interventions to enhance nutrition and prevent obesity had a marginal impact on lowering BMI, according to a systematic review and meta-analysis.(Reference Salam, Hooda and Das65) According to studies performed in Indonesia,(Reference K, Anwar, Kustiyah and Riyadi66) Kenya,(Reference Florence, Ochola and Irene67) Mexico(Reference Shamah Levy, Morales Ruán, Amaya Castellanos, Salazar Coronel, Jiménez Aguilar and Méndez Gómez Humarán68) and South Africa,(Reference Grace, Biggs, Naicker and Moss69) the nutritional status (overweight and obesity) of teenagers has decreased as a result of a combination of nutrition education and physical activity intervention. However, none of them execute the full packages of DDIs to lower DBM on both sides. The present study applied double-duty nutrition interventions together with physical activities that are appropriate for DBM over the previous evidence.
According to the GEE model analysis, after the implementation of DDIs, adolescents in the IG had a nearly 50% reduction in being overweight/obese and a 67% reduction in being thin than those in the CG. Additionally, adolescents in the IG had a more than 33% reduction of DBM than adolescents in the CG. The proportion of DBM was decreased by nearly 60% among adolescents in the end-line measurement compared to adolescents in the baseline measurement. Similarly, adolescents in the time-group interaction category had a 44% reduction of DBM than their counterparts. This is consistent with studies conducted in Ethiopia,(Reference Paponetti, Zwolski, Porter and Paterno70) Brazil,(Reference Cunha, da Souza, Pereira and Sichieri71) global,(Reference Salam, Hooda and Das65) LMICs,(Reference Shinde, Wang, Moulton and Fawzi64) small island developing states,(Reference Augustus, Haynes and Guell72) Croatia,(Reference Jovanovi´, Jankovi´ and ŽeŽelj73) Ghana,(Reference Wiafe, Apprey and Annan74) Turkey,(Reference Akdemir, Donmez and Polat75) and Poland.(Reference Zalewska and Maciorkowska76) Nevertheless, the present study implemented a comprehensive approach by combining diverse nutrition interventions and appropriate physical activities specifically designed for individuals with DBM. This approach aimed to effectively reduce DBM on both sides of the crisis. By incorporating a wider range of interventions, the study sought to build upon and expand the existing body of evidence in this field.
As a significant practical implication, it’s noteworthy that Ethiopia ratified a food and nutrition policy in 2018, with the overarching goal of achieving food and nutrition security for all its citizens.(77,78) However, it’s crucial to recognise that the current policy framework lacks comprehensive integration of DDIs, which are specifically designed to simultaneously tackle the coexistence of undernutrition and overnutrition. This gap in policy inclusivity implies that the existing strategies may not effectively address the multifaceted challenges posed by DBM. Therefore, a compelling recommendation arises for the policy to undergo updates, incorporating these intervention packages, not only within the confines of the study area but also on a national scale. By integrating DDIs into the policy framework, Ethiopia can proactively address the intricate interplay between undernutrition and overnutrition, thus mitigating their adverse health effects. Such a strategic update holds the potential to significantly reduce the prevalence of malnutrition across the country and alleviate the associated consequences, thereby fostering improved health outcomes and overall well-being among the population. In developing countries like Ethiopia, researchers and decision-makers can tailor DDIs to address DBM by focusing on contextual adaptation, stakeholder engagement, capacity building, and robust monitoring and evaluation.
When considering the strengths and limitations of the study, one notable strength is its incorporation of a theory-based HBM, coupled with a DDI approach, which effectively enhanced the implementation of interventions. Additionally, the study employed a multimodal delivery method, utilising text messages, phone calls, and targeted communication to promote behaviour change and educate participants. However, the study did have some limitations. One such limitation was the potential for recall bias, social desirability bias, and reporting bias. To mitigate these limitations, the researchers took thorough measures to ensure accurate reporting and minimise biases through rigorous protocols and careful attention to data collection and analysis.
Conclusion
Owing to the implementation of the DDIs, adolescents in the IG experienced a lower prevalence of DBM compared to those in the CG. The IG demonstrated a significant reduction of nearly 5% in the levels of thinness and more than 2% in overnutrition in comparison to the CG. At the end of the trial, the total prevalence of DBM within the study area had decreased by approximately 7% in the IG. Furthermore, adolescents in the IG showed a substantial improvement in their nutritional status at the end of the measurement period in the GEE model. Given these positive outcomes, it is recommended that the DDIs supported by HBM be integrated into national guidelines as part of the country’s overall strategy and nutrition policy. By doing so, the interventions can be disseminated on a larger scale, leading to an improved nutritional status and a reduction in the occurrence of DBM among adolescents nationwide.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/jns.2024.68.
Availability of data and materials
The dataset supporting the conclusions of this article is available from the corresponding author upon reasonable request.
Acknowledgements
We would like to express our deepest thanks to Jimma University and Debre Berhan University for their financial support. We are also grateful to the study participants, data collectors, supervisors, language translators, office administrators, and everyone who participated directly or indirectly in the accomplishment of this study.
Authors’ contributions
LG: Participated in the conception and design of the study, performed the data collection, performed the statistical analysis, and served as the lead author of the manuscript. BWA and TB: Participated in the design of the study, revised subsequent drafts of the paper, supported statistical analysis, and critically reviewed and finalised the manuscript. All authors read and approved the final manuscript.
Funding
Jimma University and Debre Berhan University funded this study through minister of education of Ethiopia. The funders had no role in the data collection, data analysis, and interpretation of the results.
Competing interests
The authors have declared that no competing interests exist.
Consent for publication
None declared.
Ethical consideration
The study was conducted following the criteria of the Helsinki Declaration and the principles of good clinical practice.(79) The research protocol was approved by the Institutional Review Board (IRB) of Jimma University, and ethical clearance was obtained on 10 August 10 2022 with a reference number of JUIH/IRB/104/22, which is before the starting date of data collection. Written informed consent was secured from each participant’s parents/guardian and an assent form from adolescents before starting the trial to confirm willingness after clarification of the study purpose and its benefits. For parents/guardians of adolescents who could not read and write, a fingerprint was used. The study participants were assured that they were free to withdraw their consent and discontinue participation in the study without any form of prejudice at any time during the study period. Privacy and confidentiality of the collected data were ensured throughout the study. Moreover, the trial was prospectively registered in Clinical Trials.gov with the registration number NCT05574842.