CLINICIAN'S CAPSULE
What is known about the topic?
A lung ultrasound has good accuracy in finding the cause of acute dyspnea.
What did this study ask?
Can a simple lung ultrasound score, done early, detect dyspneic patients who will require intensive care?
What did this study find?
A modified lung ultrasound (MLUS) has very good accuracy in predicting intensive care unit admission and/or death.
Why does this study matter to clinicians?
Dyspneic patients with a high MLUS should be monitored and treated early.
INTRODUCTION
Dyspnea, a frequently encountered presentation in the emergency department (ED),Reference Malas, Cağlayan and Fidan1, Reference Mueller, Scholer and Laule-Kilian2 can manifest with many different degrees of clinical severity.Reference Ray, Birolleau and Lefort3 Although dyspnea is a subjective symptom, it represents a severe symptom for many conditions and has been associated with significant morbidity and mortality,Reference Vinson, Rich and Sperry4, Reference Marrie5 notably in cardiovascularReference Abidov, Rozanski and Hachamovitch6 and chronic respiratory diseases.Reference Celli, Cote and Marin7 Although there are degrees of severity of disease scores,Reference Le Gall, Loirat and Alperovitch8, Reference Knaus, Draper, Wagner and Zimmerman9 they are only recorded in intensive care units (ICUs), and their low sensitivity limits their use in triage assessment on an individual basis.Reference Lemeshow, Klar and Teres10, Reference Glance, Osler and Shinozaki11 Dyspnea is also problematic when it comes to diagnosis,Reference Mueller, Scholer and Laule-Kilian2 especially for elderly patients where elements of their medical history, such as cardiovascular and respiratory symptoms, are intricately linked.Reference Ray, Birolleau and Lefort3, Reference Lien, Gillespie, Struthers and McMurdo12 Lung ultrasound has value in diagnosing dyspnea.Reference Lichtenstein and Mezière13–Reference Volpicelli, Mussa and Garofalo17 Specifically, it allows us to assess lung aeration and the location and severity of pulmonary edema. Point-of-care ultrasound (POCUS) can quickly help stratify dyspneic ED patients who should undergo a more detailed evaluation.Reference Zanobetti, Scorpiniti and Gigli18 For ICU patients, lung ultrasound has reportedly played a role in determining the diagnosis, prognosis, and clinical severity,Reference Bouhemad, Zhang, Lu and Rouby19–Reference Mongodi, Via and Girard24 but the value of an early evaluation by lung ultrasound for the triage of dyspneic ED patients has not been known.
The objective of this study was to evaluate the accuracy of early lung ultrasound scores in predicting the severity of acute dyspnea in patients over age 64.
METHODS
Materials
This observational single-centre study was conducted from November 2015 to March 2016. The study protocol was approved by the ethics committee of the French Society of Anesthesia and Intensive Care Medicine, who waived the requirement for informed consent because the study was observational. We declared our study to the National Commission for Data Processing and Civil Liberties (CNIL). The study analysed the records of patients admitted for acute dyspnea in an ED of the University Hospital of Marseille. Approximately 83,000 patients a year are admitted to this ED.
Patients
Because an association between diagnosis and prognosis is shown in this population,Reference Ray, Birolleau and Lefort3 we chose to study 64-year-old dyspneic patients. Patients were included if they were over age 64, were admitted for acute dyspnea, were on spontaneous ventilation, and presented with oxygen saturation levels measured by pulse oximeter (SpO2) that were strictly below 94% in room air. Patients with a history of lung surgery or pneumothorax were not included, due to the inapplicability of the ultrasound score.
Aim
The objective of our study was to determinate the accuracy of a lung ultrasound score (modified lung ultrasound [MLUS] score) obtained upon admission of acutely dyspneic patients over 64 years of age to predict ICU admission or death within 48 hours of ED admission. The primary end point was either admission to an ICU after the ED or patient death within 48 hours of ED admission. Patients meeting these criteria were included in the critical care (CC) group. It was the intensivist who made the decision to admit the patient to the ICU. If the intensivist thought that the patient was serious enough to be admitted to the ICU, although an end-of-life decision was decided upon, then the patient was classified in this group. The notion of ICU nonadmission according to an end-of-life decision was sought in the medical files. Patients without these criteria were included in the standard care (SC) group.
Measurements
Epidemiological data collected included gender, age, vital signs on hospital admission, medical history of cardiovascular or respiratory problems, and cardiovascular risk factors as well as the dyspnea score according to the New York Heart Association (NYHA) classification system.Reference Hurst, Morris and Alexander25 The final diagnosis was based on the electronic medical record. The time to obtain the MLUS score was considered the time between ED admission and the obtaining of the score.
Procedure
All patients meeting the inclusion criteria received a lung ultrasound and a calculation of an MLUS score upon admission to the ED. Five emergency physicians (EPs) performed the ultrasound. All EPs were certified with a university diploma in clinical ultrasound and routinely performed a lung ultrasound. One EP in particular was present to do the lung ultrasound for the study. The operators did not perform a clinical exam on the patients. The patients then received SC from a team blinded to the MLUS results. The responsible care physician did not know the results of the MLUS and could do a POCUS.
Ultrasound (Figure 1)
The study used a portable Logiq E ultrasound system manufactured by General Electric (GE Healthcare, Milwaukee, Wisconsin, USA) with a 1–5 MHz sector array transducer, only using the 2D mode. A lung ultrasound was carried out to calculate the MLUS score. Here, this score will be called the MLUS (the modified LUS [lung ultrasound (score)]) as described by Bouhemad et al.Reference Bouhemad, Mongodi, Via and Rouquette26 Both lungs were examined with the patient in a supine or semi-seated position, covering six zones on each lung. Thus, there were a total of 12 zones, 2 anterior, 2 lateral, and 2 posterior zones per lung, as described by Bouhemad et al.Reference Bouhemad, Mongodi, Via and Rouquette26 (see Figure 1). Four types of lung aeration were evaluated according to international guidelinesReference Volpicelli, Elbarbary and Blaivas27 (see Figure 1), as follows:
• Normal aeration (0 points), corresponding to the presence of lung sliding associated with A-lines or fewer than three B-lines
• Moderate damage (1 point), suggesting interstitial syndrome, with B-lines of 7 mm apart or less, that is, at least three B-lines on the same ultrasound
• Serious damage (2 points) corresponding to alveolar interstitial syndrome, with B-lines of 3 mm apart or less
• Pulmonary consolidation and/or pleural effusion, with a minimum distance of 20 mm or more between the parietal and visceral pleurae on a transverse scan (3 points).
We thought we should highlight and evaluate potential pleural effusion, which could affect the short-term prognosis.Reference Volpicelli, Elbarbary and Blaivas27 In cases where the quality of the examination was considered poor (i.e., uninterpretable), the patient was excluded from the study.
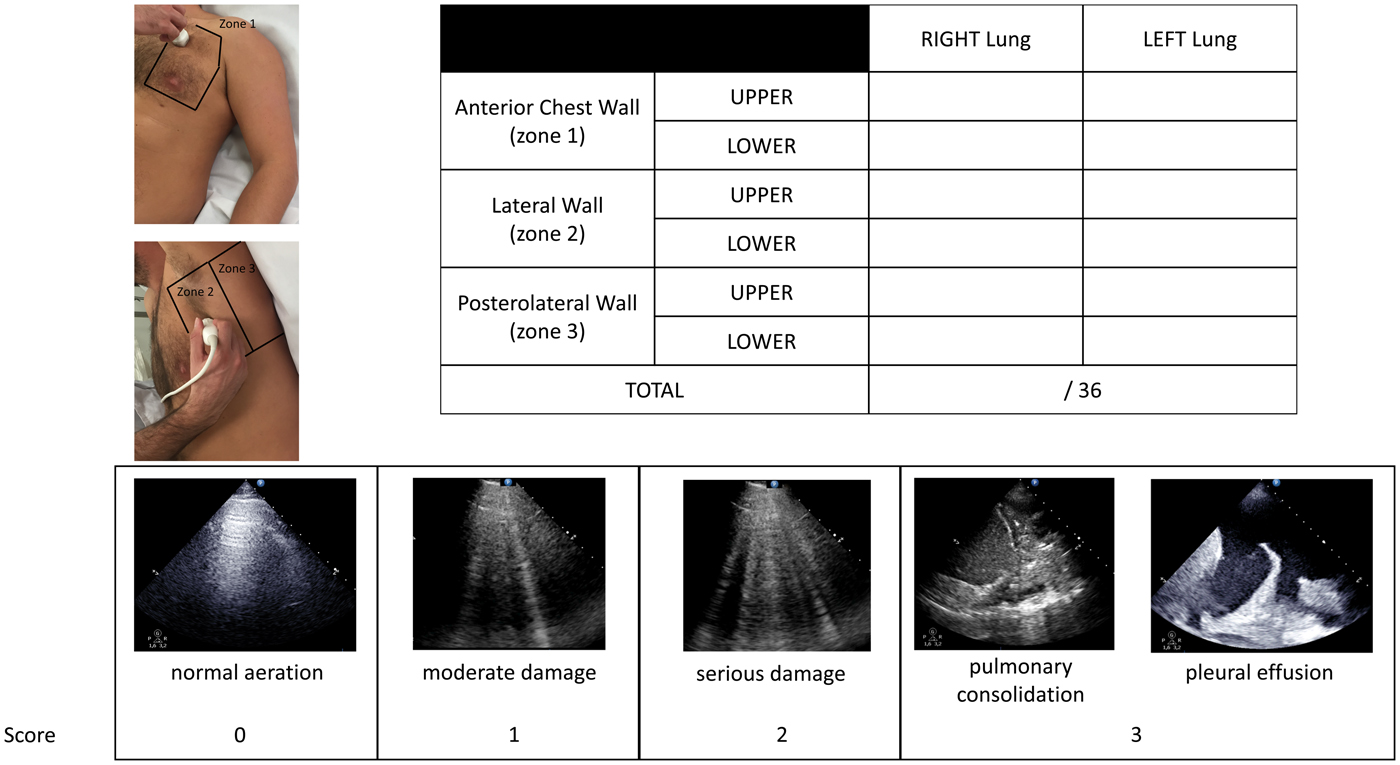
Figure 1. Modified lung ultrasound score calculation.
Number of subjects
The sample size was calculated based on a study by Ray et al.,Reference Ray, Birolleau and Lefort3 who found that the rate of ICU admission was 29%. To have a specificity of 95% with a two-tailed alpha risk of 0.05, we needed to include 104 subjects, with 30 patients requiring ICU admission. To allow for any data loss, we planned to include 5% more patients. Given the number of dyspneic patients usually admitted in our ED during the period, records were taken during eight random periods of 5 days each, spread over the 5 months of the study.
Data analysis
Quantitative data are expressed as mean ± standard deviation (SD) or median with the 25th and 75th percentiles (25th percentile–75th percentile), according to the variable distribution. The qualitative variables are expressed as the frequency with percentage. The variables compared between the two groups included age, gender, past medical history (cardiac history, diabetes, hypertension, dyslipidemia, current smoker, lung history), clinical state (oxygen saturation, respiratory rate, dyspnea NYHA class, systolic arterial pressure, temperature, Glasgow coma score), the Boston score,Reference Volpicelli, Elbarbary and Blaivas27 the Geneva score, the serum lactate level, and the MLUS. A comparison of quantitative variables among the different groups was performed via the student's t-test. When the conditions of validity of this test were not verified, the nonparametric Mann–Whitney U test was used. The chi-square or Fisher exact test was used for qualitative variables. We also performed a multivariate analysis using a multiple logistic regression. Variables with a significance level of at least 0.1 were included in the logistic model. The receiver operating characteristic (ROC) curve analysis was used to assess the discriminatory power of the prognostic factor. Subsequently, the optimal cut-off points were determined via the ROC curve based on the Youden index. All tests were two-tailed. The statistical significance was defined as p < 0.05. Statistical analysis was performed using PASW Statistics version 20 (IBM SPSS Inc., Chicago, IL, USA).
RESULTS
Participants
During the data collection period, 520 patients over age 64 years were admitted to the ED. Among these patients, 140 (27%) received an early lung ultrasound. Within this population, 3 (2%) were excluded from the study due to a history of pneumonectomy. There were no exclusions reported for mediocre ultrasound imaging. The five different operators performed a number of ultrasound scans as follows: 18 (13%), 21 (15%), 26 (19%), 32 (24%), and 40 (29%). Epidemiological data are provided in Table 1.
Table 1. Baseline patient characteristics and final diagnoses
Notes: Qualitative data are expressed as frequency with percentage: n (%); quantitative variables are expressed as means and standard deviation (m ± SD) or median with 25th and 75th percentiles (m [25th percentile−75th percentile]); COPD = chronic obstructive pulmonary disease; CPO = cardiogenic pulmonary edema; HTA = hypertension; MLUS = modified lung ultrasonography; NYHA = New York Heart Association; SpO2 = saturation levels measured by pulse oximeter.
Outcomes
Among the patients who had the protocol analysis, 94 (69%) were categorized into the SC group, whereas 43 (31%) were put into the CC group. In the CC group, 14 (33%) patients died while staying in the hospital. Epidemiological data for both populations are provided in Table 1. The MLUS was calculated 30 ± 22 minutes after a patient arrived in the ED. The area under the ROC curve for predicting admission to the ICU or death within 48 hours, using MLUS, was 0.97 (0.92–0.99; p < 0.01), with a cut-off set strictly above 17 for 93% sensitivity (81–99), 99% specificity (94–100), a positive predictive value of 98% (87–100), a negative predictive value of 97% (91–99), a positive likelihood ratio of 86, a negative likelihood ratio of 0.07, and a diagnostic accuracy of 97% (93–99) (Figure 2). Univariate analysis of the differences between the CC and SC groups revealed factors linked to clinical presentation, lactate concentration, and the MLUS. For the MLUS, a cut-off set at 17 seemed particularly discriminating. In the multivariate analysis, the MLUS was the only remaining prognostic factor independent of severity with a cut-off at 17 (Table 2).
Figure 2. Receiver operating characteristic curve depicting the relationship between the modified lung ultrasound score with a cut-off set strictly above 17 and the critical care group.
Table 2. Factors associated with the critical care group
CI = confidence interval; MLUS = modified lung ultrasound; OR = odds ratio.
DISCUSSION
Main results
An LUS recorded on admission to the ED efficiently allowed us to triage dyspneic patients over 64 years old. In other words, its calculation was associated with the rapid and adaptive triage of elderly patients with dyspnea. In the context of an ED, it is important to determine what constitutes a reasonable amount of time for conducting this evaluation. Zanobetti et al. showed a good concordance between the diagnoses reached after POCUS evaluation and after standard ED evaluation in the differential diagnosis of dyspneic patients, with a POCUS diagnosis time of 24 minutes.Reference Zanobetti, Scorpiniti and Gigli18 The authors concluded that POCUS may help stratify patients who should undergo a second-level diagnostic test. Our study showed that, in approximately the same time, the calculation of the MLUS score accurately predicted the outcome for severely ill patients.
Originality of the study
Dyspnea management in the ED includes both rapid hypothetical diagnosis and patient-oriented triage. The value of lung ultrasound in diagnosing dyspnea has already been proven.Reference Lichtenstein and Mezière13–Reference Zanobetti, Scorpiniti and Gigli18, Reference Volpicelli, Elbarbary and Blaivas27–Reference Laursen, Sloth and Lassen31 Lung ultrasound is more accurate than chest X-rays to diagnose the main causes of acute dyspnea.Reference Bataille, Riu and Ferre30–Reference Lichtenstein, Goldstein and Mourgeon35 The value of lung ultrasound in prognosis has also been indicated for patients suffering from dyspnea or chest painReference Frassi, Gargani and Tesorio36 and acute respiratory distress syndrome.Reference Li, Yang and Li22, Reference Zhao, Jiang and Xi23, Reference Leblanc, Bouvet and Degiovanni37 If the diaphragmatic excursion measurement can predict the use of a ventilation technique,Reference Bobbia, Clément and Claret38 then the value of lung ultrasound in helping with patient triage on admission to the ED has not yet been reported clearly. The additional diagnostic value of simultaneous echocardiogram and lung ultrasound recordings is also obvious, but it is time-consuming and, therefore, is less applicable in the context of triage.Reference Bataille, Riu and Ferre30 We chose to change an existing score: the LUS.Reference Bouhemad, Mongodi, Via and Rouquette26 This score seemed simple to achieve and was described in critical patients.
Limits
Nevertheless, our study has its limits. Firstly, this study is monocentric; therefore, multicentre studies will probably be required to confirm our results and to assess the MLUS score as a prognostic score for dyspnea. Secondly, none of the patients were followed up more than 48 hours post-admission, and only initial data were taken into account when categorizing patients into the CC and SC groups. It would be advisable to study the population's progress over at least 30 days to more accurately evaluate the usefulness of an early LUS as a prognostic factor. Thirdly, if the operators did not perform a clinical exam on the patients, then the operators saw the patients. It is possible that the clinical state of the patients changed after their ultrasound interpretation. Fourthly, there is little evidence for the diagnostic interest of pulmonary ultrasound scoring. Finally, in our study, most ICU patients had cardiogenic pulmonary edema (CPO), and the majority of CPO patients went to the ICU. It is possible that the accuracy of the MLUS would have been lower in a different distribution of diagnoses.
CONCLUSION
Our study showed that an early LUS can predict with good accuracy the clinical severity of elderly dyspneic patients, as defined by the need for ICU admission and/or death within 48 hours of being admitted to the ED.
Competing interests
XB and LZ declare a competing interest as a U.S. teacher for GE (GE Medical Systems Ultrasound) customers. The other authors state that they have no competing interests.






