LEARNING OBJECTIVES
After reading this article you will be able to:
• use principles from CBT to help people with common mental health problems to understand how their tobacco dependence and mental health are linked
• understand how the tobacco withdrawal cycle, conditioned craving and possible increases in side-effects of prescribed medications on cessation can all mimic the symptoms of common mental health problems such as anxiety, depression, low mood or stress
• understand how breaking the tobacco withdrawal cycle, better coping with cravings and developing greater self-control can all improve mental health.
This guide is for healthcare professionals who are involved in routine healthcare for people who have common mental health problems such as anxiety, depression, low mood or stress, and who smoke tobacco. They might be nurses, psychological well-being practitioners, psychiatrists, general practitioners, therapists or clinical psychologists, working in any healthcare setting where there is the opportunity to offer a brief or intensive behavioural intervention to encourage or support smoking cessation. Practitioners do not need to be experts in tobacco addiction or CBT to use, read or apply this review and guide. Although the focus of this article is primarily on those with common mental health problems, it may also be a useful guide in consulting with patients who report stress and other mood disturbances.
Background
Smoking tobacco is the world's leading cause of preventable illness and death (World Health Organization Reference Weinberger, Platt and Copeland2011). One in every two smokers will die of a smoking-related disease, unless they stop smoking (Doll Reference Doll, Peto and Boreham2004; Pirie 2013). In the UK, smoking prevalence has decreased from 46% during the 1970s to about 14% in recent years (Office for National Statistics 2020). However, approximately 34% of people with depression and 29% of people with anxiety in the UK smoke tobacco (Taylor Reference Taylor and Munafò2020a). People with depression and anxiety are more heavily addicted, suffer from worse withdrawal (Royal College of Physicians Reference Rabin, Ashare and Schnoll2013) and find it harder to quit (odds ratio 0.81, 95% CI 0.67–0.97) (Hitsman Reference Hitsman, Papandonatos and McChargue2013). These inequalities at least partly contribute to a reduction in life-expectancy in people with mood disorders when compared with the general population (mortality rate ratio 1.92 (95% CI 1.91–1.94) (Plana-Ripoll Reference Parrott2019).
Most healthcare professionals are aware that stopping smoking is one of the greatest changes that people can make to improve their health. However, smoking cessation can be a difficult topic to raise. Many people say that smoking tobacco helps them to alleviate stress, cope with mental health difficulties such as low mood or anxiety and that smoking brings them relaxation or pleasure (Malone Reference Lapshin, Skinner and Finkelstein2018; Taylor Reference Taylor, Sawyer and Kessler2020b). When discussing smoking cessation, healthcare professionals can sometimes feel that they might be depriving people of one of their pleasures or ability to cope with stress. They can also feel that they might undermine their relationship with patients and the patients’ trust, which could compromise future consultations and treatment plans (Sheals Reference Sheals, Tombor, McNeill and Shahab2016).
Traditionally, tobacco addiction and mental illness have been treated separately, usually focusing on mental illness first (Baker Reference Baker, Denham, Pohlman, Badcock and Paulik2019). Research shows that people with mental health problems are as motivated to quit as the general population, with more than half contemplating quitting within 6 months, or preparing to quit within 30 days (Richardson Reference Plana-Ripoll, Pedersen and Agerbo2019). However, for many people, mental health conditions can be recurring over the longer term. So, when is ‘the right time’ to quit smoking? People with mood disorders are most likely to die from smoking-related diseases (Plana-Ripoll Reference Parrott2019). How best can healthcare professionals address smoking cessation when their main presenting concern is the patient's mental health?
It is not yet widely known that smoking tobacco might actually cause mental health problems (Taylor Reference Stevenson, Oliver and Hallyburton2019a) and that stopping smoking may improve mental health (Taylor Reference Segan, Baker and Turner2014, Reference Taylor, Aveyard and Bartlem2020c). In fact, the size of improvement in mental health observed when people stop smoking is similar to the size of effect observed when people take antidepressants (Taylor Reference Segan, Baker and Turner2014). This improvement can be at least partly explained by breaking the tobacco withdrawal cycle. Tobacco addiction leads to periods of withdrawal shortly after having a cigarette, whereby the person experiences psychological symptoms such as low mood, anxiety, poor concentration and irritability (Benowitz Reference Benowitz, Hukkanen, Jacob, Henningfield, London and Pogun2010). If the person smokes on a regular basis they will feel these withdrawal symptoms much of the time, with short periods of relief only while they smoke and shortly after.
There are ways that healthcare professionals can compassionately approach smoking cessation and remain respectful of the patient's autonomy. It is important to share new research findings, reassuring patients that stopping smoking will not have a negative impact on their overall mental health and could actually improve mental health in the long term. This knowledge could empower patients and motivate smoking cessation. Smoking cessation treatments are effective in people with mental health problems (Taylor Reference Taylor and Munafò2020a). However, as people with mental health problems often experience higher levels of tobacco dependence, they can require higher doses over longer periods of time of some smoking cessation medicines, such as nicotine replacement therapy (NRT) (NCSCT 2019; NICE 2020), and tailored behavioural support during their quit attempt (NICE Reference Miller and Rollnick2013; NCSCT 2019) specifically targeting mood (van der Meer Reference Taylor, Itani and Thomas2013).
Understanding cognitive–behavioural therapy principles
The basic principles of cognitive–behavioural therapy (CBT) are a useful way to help patients to see how their thoughts, emotions, behaviour and physical sensations are interlinked (Fig. 1). CBT is usually used to treat conditions such as anxiety, depression, low mood and stress, but can also be used to treat smoking, alcohol and other drug problems. Recently, a dual process theory of addiction has been proposed, whereby addictive behaviour is the result of the predominance of implicit, automatic and mainly non-conscious cognitive processes over explicit, controlled and mainly conscious processes (Heather Reference Heather, Segal, Heather and Segal2016). CBT helps people focus on their present challenges and how these are linked with their thoughts, emotions, behaviour and physical sensations. Using this model can help people to recognise, assess and respond to their problems, by establishing greater behavioural and cognitive control over impulsive urges and preventing relapse (Heather Reference Heather, Segal, Heather and Segal2016).
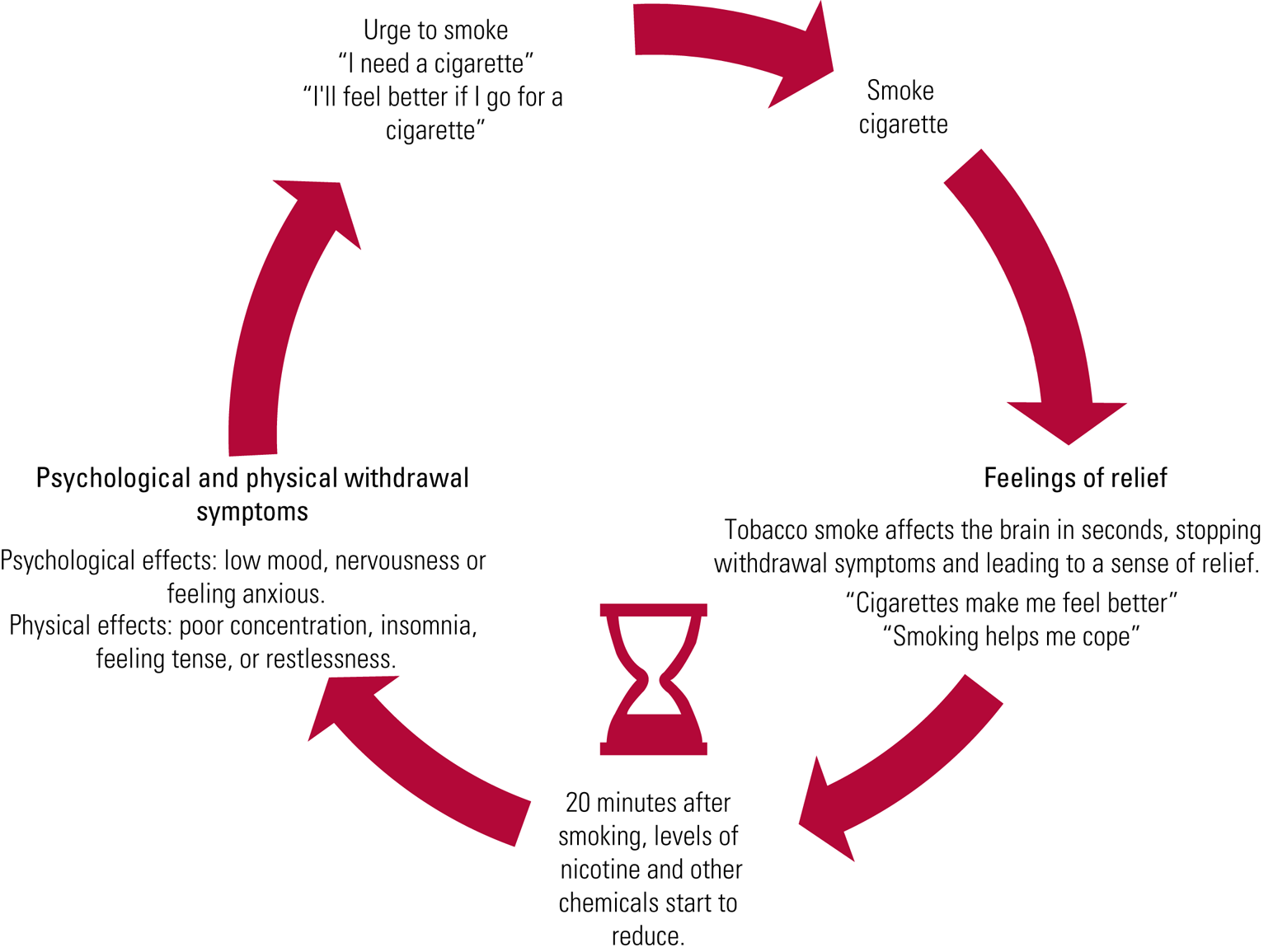
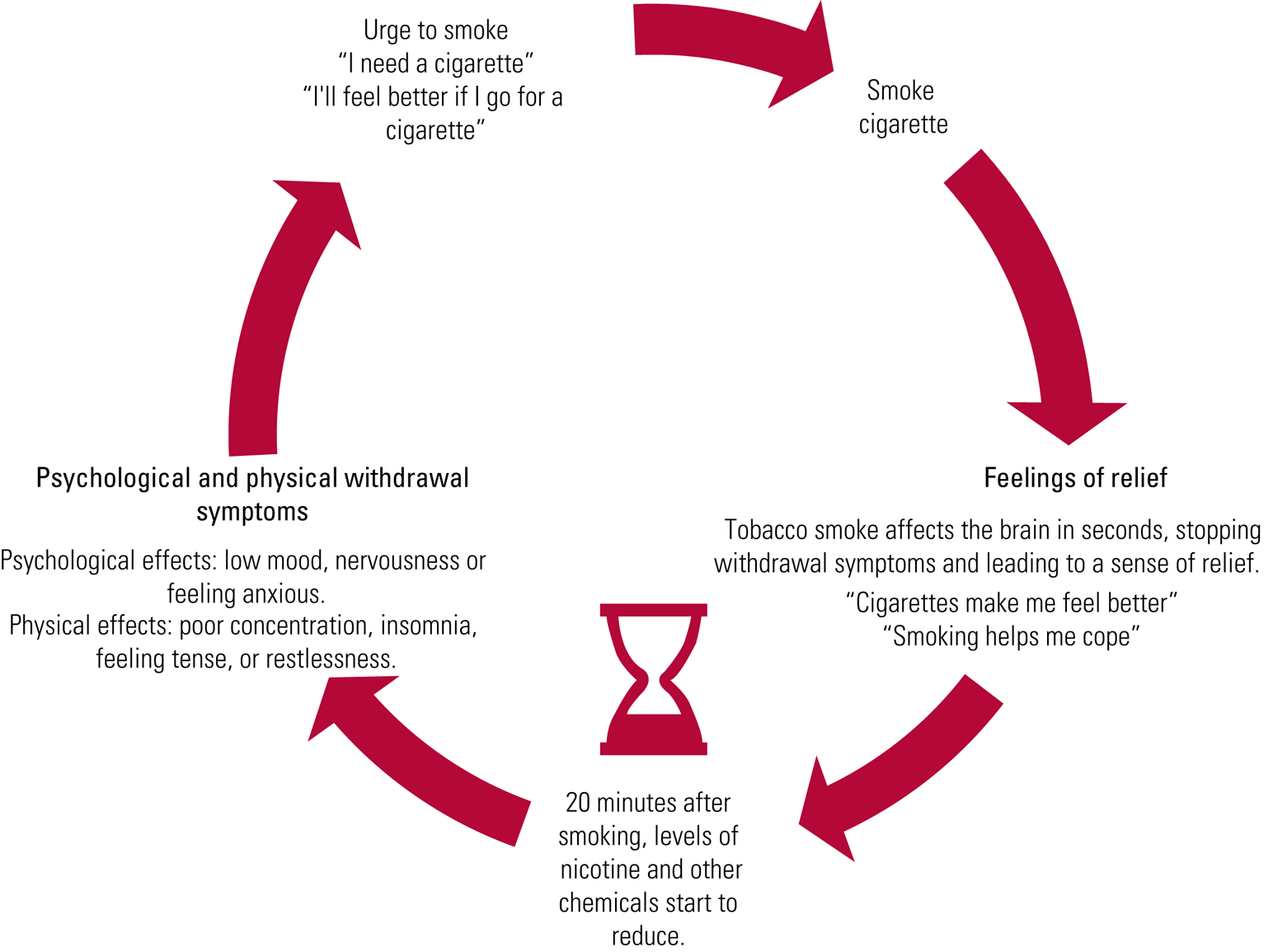
FIG 1 Tobacco addiction maintenance cycle.
Linking mood and other mental health symptoms with smoking using a CBT model
Using a CBT model can also be used to help people to see how their thoughts, emotions, behaviour and physical sensations are interlinked in the context of their tobacco dependence and mental health (Fig. 1). To promote smoking cessation for people with depression or anxiety, self-monitoring of mental health symptoms and medication side-effects increases understanding about their links. Monitoring that starts pre-cessation and continues for a few weeks post-cessation may help to distinguish temporary nicotine withdrawal symptoms from a relapse of mental illness and, for those taking medication, can track common adverse side-effects that can increase with quitting (Segan 2017). Of course, monitoring can also help to address symptoms regardless of their cause.
One such monitoring tool, used by Quitline Victoria (Segan 2017), is outlined in Box 1. It includes the 8-item Minnesota Nicotine Withdrawal Scale (Hughes Reference Hughes2007a), which is referred to as a ‘mood and experiences scale’ because smokers might be confused by completing a ‘withdrawal’ scale prior to cessation and sometimes, post-cessation, may not report a symptom if they do not believe that it is due to withdrawal. The term ‘symptom’ is also avoided, as it is very clinical and can imply that something is wrong and needs fixing; instead, the phrases ‘moods and experiences’ and ‘possible side-effects’ are used.
BOX 1 The Quitline Victoria smoking cessation monitoring tool
Structured monitoring of:
(a) nicotine withdrawal symptoms or 'mood and experiences' (Segan Reference Segan, Baker and Turner2017), using the 8-item Minnesota Nicotine Withdrawal Scale (Hughes Reference Hughes2007a):
• anger/irritability/frustration
• anxiety or nervousness
• depression/sad mood
• desire/craving to smoke
• difficulty concentrating
• increased appetite/hunger/weight gain
• insomnia/sleep problems/awakening at night
• restlessness/impatience
(b) the most common adverse side-effects of psychiatric medications (Lapshin Reference Kay-Lambkin, Edwards and Baker2006), or 'possible side-effects' (Segan Reference Segan, Baker and Turner2017):
• dry mouth or increased salivation
• increased thirst
• headache
• nausea
• drowsiness, tiredness, fatigue
• increased sleep
• blurred vision
• dizziness
• increased sweating
In the case of anxiety, depression, low mood and stress, the five areas of the CBT model can help us understand that these conditions and their associated feelings can be a trigger for smoking. People report smoking in an effort to calm themselves down, reduce anxiety, make themselves feel relaxed, give themselves a break or to self-medicate. As smoking provides short-term relief from withdrawal, and as the person thinks they feel better after a cigarette, this reinforces their smoking behaviour. However, as little as 20 minutes after smoking a cigarette this cycle will happen again (Benowitz Reference Benowitz, Hukkanen, Jacob, Henningfield, London and Pogun2009), generating further feelings of anxiety, sadness, hopelessness and so on. Figures 2–4 show how these areas interact with one another to maintain an unhelpful coping behaviour or maintain a pattern of low mood or anxiety. An animation by the Addiction and Mental Health Group (AIM) available at https://youtu.be/HiYBGOQ-PIo summarises this approach. Another animation by AIM available at https://www.youtube.com/watch?v=iQn4MbWbiSU, about the tobacco withdrawal cycle, might be a useful tool when explaining links between tobacco use and depression/anxiety symptoms to patients.
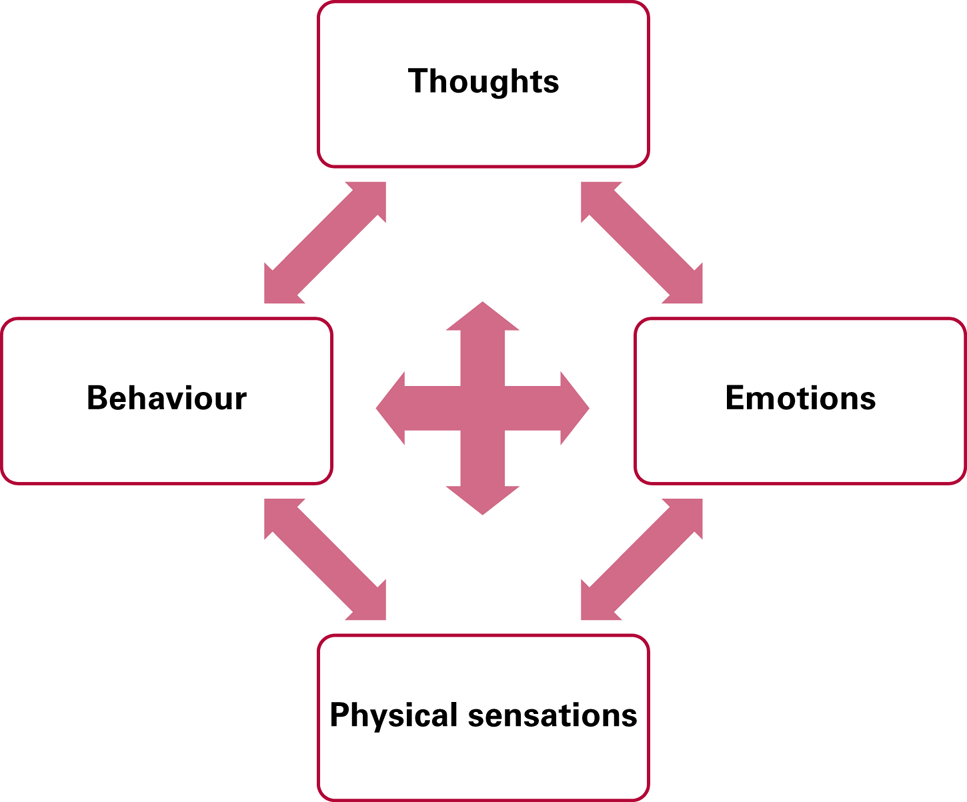
FIG 2 Reinforcement of smoking behaviour: the cognitive–behavioural model.
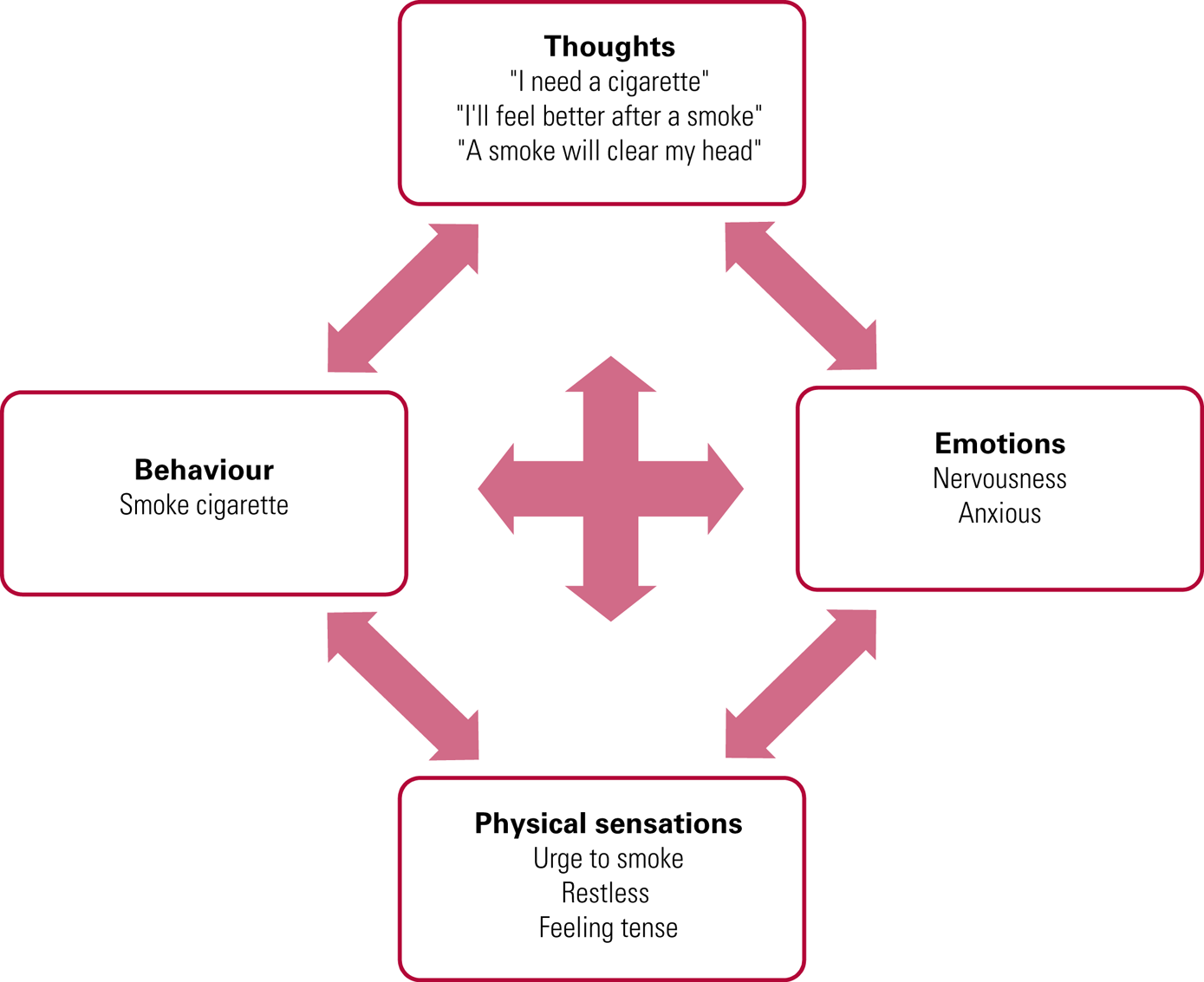
FIG 3 The anxiety cycle in smoking: the trigger is an anxiety-provoking event.
Integrating CBT principles for smoking and mental health into routine care
These CBT principles are designed to be used as a tool, not as a sole treatment, and are best used as part of a recommended smoking cessation treatment. The National Institute for Health and Care Excellence (NICE) (2018), for example, recommends behavioural support in combination with pharmacotherapy for smoking cessation. Depending on time available and circumstances, support might be very brief advice or more in-depth behavioural support; or it might involve developing a collaborative model or ‘formulation’ of the person's smoking and a plan for cognitive and behavioural change involving such approaches as behavioural activation, mindfulness, coping with cravings and relapse prevention. Pharmacotherapy choice will depend on previous experience, preference and whether or not the person will also consult a medical practitioner for a prescription. Pharmacotherapy includes nicotine replacement therapy (usually a combination of nicotine patches and one or more short-acting forms such as gum, lozenges, spray or vaporiser), varenicline or bupropion (depending on country). Smokers may also want to try e-cigarettes as a nicotine replacement product, which is supported by Public Health England (McNeill Reference McNeill, Brose, Calder, Bauld and Robson2020). Adherence to medications is important and this can be monitored along with mood and experiences to enhance discussion of how smoking cessation medication helps to alleviate withdrawal.
Very brief advice for smoking cessation
The ‘very brief advice’ approach recommended by the National Centre for Smoking Cessation and Training (NCSCT) is being increasingly used (Box 2). A systematic review and meta-analysis of brief opportunistic interventions for smoking cessation found that healthcare professionals can be more effective in promoting attempts to stop smoking by offering help to all smokers, rather than offering assistance only to those who state that they want to stop smoking (Aveyard Reference Aveyard, Begh and Parsons2012). Brief interventions in settings such as primary care can be very effective in improving lifestyle behaviours (Aveyard Reference Aveyard, Lewis and Tearne2016).
BOX 2 Very brief advice (the three A's)
Ask – establish smoking status: ‘Do you smoke tobacco cigarettes or roll-ups?’
Advise – that the best way of stopping smoking is to use a combination of behavioural support and drug treatment: ‘Did you know that smoking cessation medicine plus smoking cessation counselling can double your chances of quitting?’
Act – provide a referral or offer behavioural support using the CBT model as a tool, and follow-up appointments: ‘Would you like to meet again to talk about smoking cessation options?’, ‘I can refer you to a smoking cessation specialist, if you like?’
(Aveyard Reference Aveyard, Begh and Parsons2012; NCSCT 2020)Smokers may say that they are ‘too stressed out to stop’, that they would like to ‘deal with their mental health problem before they stop smoking’, or that they ‘won't be able to cope without cigarettes’. This may be an ideal opportunity to implement the CBT principles for smoking and mental health (Figs 1–4) to explore their mental health and tobacco dependence. This might encourage them to think about stopping smoking or even prompt a quit attempt.
Standard behavioural support for smoking cessation
For healthcare professionals who are regularly consulting with the person, are involved in offering behavioural support to change lifestyle behaviours, or in the provision of behavioural support for smoking cessation, the CBT principles for smoking and mental health discussed here can be integrated into the standard smoking cessation treatment programme designed by the NCSCT (2019). For example, the NCSCT recommends that standard behavioural support for smoking cessation involves of 110 minutes of behavioural support over 6 sessions. During each of these sessions, there are opportunities to provide support for any concerns the person is having about quitting smoking and their mental health, psychoeducational opportunities about the withdrawal cycle and mental health, and explaining the mental health benefits of smoking cessation.
In the ESCAPE trial (Taylor Reference Taylor, McNeill and Girling2019b), psychological well-being practitioners are integrating smoking cessation treatment into psychological services for common mental health problems, using a smoking cessation intervention checklist (Table 1). Using this checklist, they are tailoring the intervention content to the person's needs. Psychological well-being practitioners dedicate time during each session to address the person's beliefs about smoking and mental health, and tailor intervention components using their knowledge about smoking and mental health, and mental health and tobacco withdrawal.
TABLE 1 National Centre for Smoking Cessation and Training standard treatment programme with additional mental health support for smoking cessation
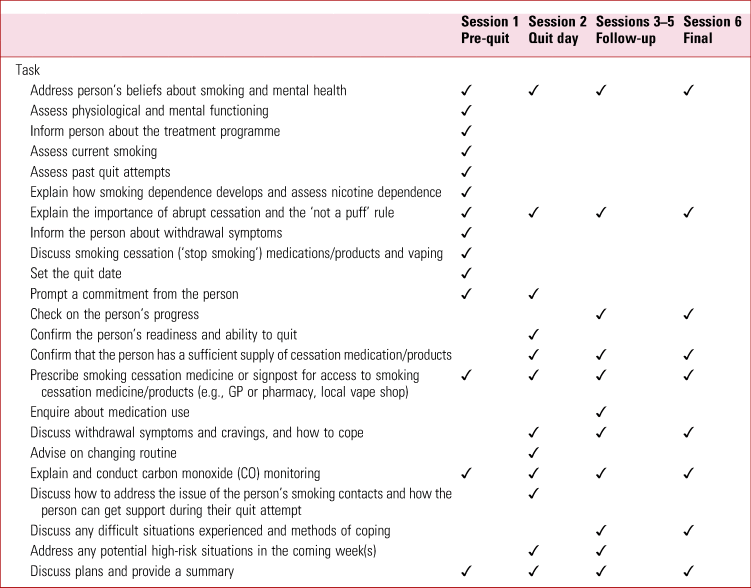
GP, general practitioner.
Sources: NCSCT (2019); Taylor et al (Reference Taylor, McNeill and Girling2019b).
Understanding links between tobacco use and mental health problems
When someone starts smoking, there are some rewarding effects of tobacco on mood and cognition. Social reasons, such as feelings of belonging, can also be important. Smoking is also used as an appetite suppressant. However, as the person becomes used to the effects of tobacco, these reasons for smoking tend to diminish as the alleviation of withdrawal symptoms such as low mood, irritability, poor concentration, restlessness and anxiety gain prominence (Benowitz Reference Benowitz, Hukkanen, Jacob, Henningfield, London and Pogun2010; Hughes Reference Hughes2007b). Nevertheless, the initial rewarding effects of smoking tend to remain important in the minds of smokers and it is these rewards that can tempt them back to smoking, even long after cessation has been achieved (Stevenson Reference Schauer, King and McAfee2017).
Regular smoking causes neuroadaptations in nicotinic pathways in the brain. Neuroadaptations in these pathways are associated with occurrence of depressed mood, agitation and anxiety shortly after a cigarette is smoked (Benowitz Reference Benowitz2009). This withdrawal cycle is marked by fluctuations in a smoker's psychological state throughout the day and can worsen mental health (Parrott 2004). There is evidence that some systems that are compromised during longer-term tobacco exposure recover after smoking cessation (Mamede Reference Malone, Harrison and Daker-White2007).
People who smoke regularly will feel these withdrawal symptoms much of the time, with short periods of relief only while they smoke and shortly after (Fig. 4). When caught in this cycle, people can mistakenly believe that smoking helps relieve symptoms of anxiety, depression, low mood or stress (Parrott 2004). But this is not the case – these symptoms are caused by tobacco withdrawal. Stopping smoking will eventually alleviate these symptoms altogether. Improvements in these symptoms usually start several weeks after stopping smoking, and then the cycle is broken (Taylor Reference Segan, Baker and Turner2014). Lapses in cessation can be associated with recalling the initial pleasures associated with smoking or beliefs about dealing with stress. Lapses can be seen as learning opportunities towards eventual cessation.

FIG 4 The depression cycle in smoking: the trigger is feeling depressed at home in the evening.
Tobacco use is a vicious cycle that can negatively affect mental health. It is useful to explain this cycle to smokers with mental health problems, to help them understand how their smoking and mental health are linked. This information can be formulated as part of their presentation and a clear understanding can be sought about how smoking can become a maintenance factor in their mental health difficulties. Figure 1 shows that 20 minutes after smoking a cigarette, levels of nicotine and other chemicals start to reduce (Benowitz Reference Benowitz2009). This leads to physical and psychological tobacco withdrawal with symptoms such as poor concentration, insomnia, feelings of tension, restlessness, low mood and anxiety. It is easy to see how most of these symptoms might be mis-attributed as symptoms of mental illness.
Can smokers cope without tobacco?
There are many reasons why people report smoking tobacco. People with mental health problems usually report smoking cigarettes to alleviate emotional problems and feelings of depression and anxiety, to stabilise mood, and for relaxation and stress-relief (Malone Reference Lapshin, Skinner and Finkelstein2018).
Studies have followed people making a quit attempt and show that when they stop smoking their mental health improves and, conversely, when they relapse, their mental health worsens to where it was before (Taylor Reference Segan, Baker and Turner2014). Similarly, there is good evidence that taking up smoking early in adolescence is associated with developing depression and anxiety (Wu Reference West, Kale and Brown1999; Jamal Reference Humfleet, Muñoz and Sees2011, Reference Jamal, Does and Penninx2012).
Smoking cessation can increase the blood levels, and hence side-effects, of some psychotropic medications as well as alcohol and caffeine (Segan 2017). This is because the tar in cigarette smoke (not the nicotine) causes the body to break down some substances more quickly than usual. Nicotine and nicotine replacement therapies do not affect medication, caffeine or alcohol levels in this way. Monitoring these side-effects with the person quitting smoking can be helpful and we describe how to do so in Box 1.
Will stopping smoking harm mental health?
Stopping smoking will not harm mental health. Evidence to date suggests that there may be a causal effect of smoking on mental illness, such that starting smoking increases risk of depression, schizophrenia (Taylor Reference Stevenson, Oliver and Hallyburton2019a) and bipolar disorder (Vermeulen Reference Vermeulen, Wootton and Treur2019). A systematic review and meta-analysis of 26 longitudinal studies found that stopping smoking was also associated with long-term improvements in mental health similar in effect size to taking antidepressants, and the benefit was at least as large in people with psychiatric conditions (Taylor Reference Segan, Baker and Turner2014). Another study found no consistent evidence that varenicline, an effective medicine for smoking cessation, was associated with greater odds of depression, neurotic disorder, antidepressant or hypnotic/anxiolytic prescription in people with or without mental disorders (Taylor Reference Taylor and Munafò2020a). In general, this study found that varenicline was associated with improved mental health outcomes, such as reductions in antidepressant and anxiolytic prescriptions up to 2 years after taking medicine to stop smoking (Taylor Reference Taylor and Munafò2020a).
What about patients with comorbid mental health problems, tobacco dependence and substance/alcohol use?
In people with comorbid substance and/or alcohol use, smoking rates are more than double those in non-users with similar demographic characteristics (Guydish Reference Guydish, Passalacqua and Pagano2016). Importantly, many people who use substances and/or alcohol and who smoke tobacco are motivated to quit smoking tobacco, but report lack of support (Gentry Reference Gentry, Craig and Holland2017).
Some studies show that cannabis co-use is associated with worse tobacco-smoking cessation outcomes, compared with tobacco-only use (Abrantes Reference Abrantes, Lee and MacPherson2009; Schauer Reference Richardson, McNeill and Brose2017; Vogel Reference Van Zundert, Kuntsche and Engels2018; Weinberger Reference Vogel, Rubinstein and Prochaska2018; McClure Reference Mamede, Ishizu and Ueda2019). However, other studies show that cannabis use is not associated with tobacco cessation outcomes (Humfleet Reference Hughes1999; Hendricks Reference Hendricks, Delucchi and Humfleet2012; Rabin Reference Pirie, Peto and Reeves2016). Similarly for alcohol, co-use is associated with worse smoking cessation outcomes compared with tobacco-only use (Humfleet Reference Hughes1999; Van Zundert Reference Taylor, McNeill and Farley2012; Haug Reference Haug, Schaub and Schmid2014, Reference Haug, Paz Castro and Kowatsch2017; Weinberger Reference Verplaetse and McKee2017); alcohol use is also associated with increased tobacco cravings, and vice versa (Cooney Reference Cooney, Litt and Cooney2007; Verplaetse Reference van der Meer, Willemsen and Smit2017). People with alcohol or opioid dependence report several barriers to quitting smoking tobacco, including anxiety, tension/irritability and concerns about the ability to maintain abstinence from their primary substance of misuse (McHugh Reference McClure, Baker and Hood2017). Those who report more barriers to smoking cessation while using substances or alcohol report low confidence in the ability to change their tobacco-smoking behaviour (McHugh Reference McClure, Baker and Hood2017).
Historically, substance/alcohol use and tobacco dependence are treated separately. However, more recently, there has been a movement towards interventions that target multimorbidity, including dual tobacco and substance/alcohol use, in people with mental disorders (Kay-Lambkin Reference Jamal and AJ2013; Baker Reference Baker, Kavanagh and Kay-Lambkin2014; Apollonio Reference Apollonio, Philipps and Bero2016). A Cochrane review of interventions for tobacco use cessation among people in treatment for or recovery from substance use found that offering pharmacotherapy for smoking cessation increased tobacco abstinence (risk ratio RR = 1.88, 95% CI 1.35–2.57), as did combined counselling and offering pharmacotherapy for smoking cessation (RR = 1.74, 95% CI 1.39–2.18) compared with usual care or no intervention. The review found that tobacco cessation interventions were associated with smoking cessation for people in treatment for substance use (RR = 1.99, 95% CI 1.59–2.50) and people in recovery (RR = 1.33, 95% CI 1.06–1.67), for people with alcohol dependence (RR = 1.47, 95% CI 1.20–1.81), and people with other drug dependencies (RR = 1.85, 95% CI 1.43–2.40). Importantly, there was no evidence that offering tobacco cessation interventions to people in drug dependence treatment or recovery affected abstinence from alcohol and other drugs (RR = 0.97, 95% CI 0.91–1.03).
How to discuss smoking without seeming didactic
Smoking cessation can be a sensitive topic. Linking the person's smoking to their mental health problems and personal values can help to break down the barriers to discussion (Miller Reference Miller and Rollnick2013). It is important not to focus prematurely on smoking. Actively listen to the person's main concerns (such as feelings of depression). Introduce smoking by asking open-ended questions about any possible links between smoking and their main concern (e.g., mood): ‘What links have you noticed between smoking and your moods?’. Seek permission to provide information about these links (e.g., ‘I wonder if you'd be interested in hearing about recent research findings about how smoking affects mental health?’). It can also be useful to spend a few moments debunking the myths about smoking: ‘A lot of people think that smoking is a stress reliever, but most people when they stop feel less stressed. Research shows their mental health improves’. After providing information (as outlined in this article), ask ‘What do you make of that?’. Explore with them their concerns about how smoking may be influencing their own mental health. Most people have other concerns about smoking, so ask them, ‘What other concerns do you have? What concerns you the most?’. Then move the person towards consideration of cessation by asking ‘What's the next step?’.
When people are not contemplating quitting in the foreseeable future, it can be worthwhile to open the conversation up, acknowledging the pleasures initially experienced in the early days of smoking: ‘Tell me some of the reasons you smoke’. Often people will reply that, although they did once enjoy being seen as ‘cool’ or part of the social crowd smoking while out drinking, such pleasures have long been outweighed by concerns such as addiction and cost. Reflect on these concerns. If no concerns are mentioned, ask ‘Tell me what reasons you might have to want to quit?’. Here, the person's values may be raised, for example many people talk about wanting to be good parents, to be around to see their children grow up and to be available for family members. Normalising the person's feelings can help, for example ‘That's a common concern’. It is important to encourage the person and boost their confidence in their ability to quit: ‘Did you know that you can double your chances of quitting with help from our local stop smoking services?’. Again it can be useful to spend a few moments debunking the myths about smoking: ‘Can I tell you a few things about smoking that might surprise you and help you to quit?’, ‘I wonder, did you know that quitting smoking can improve your overall mental health?’, ‘Many people think its the nicotine in cigarettes that's harmful, but it's the components in the tobacco smoke that are the most harmful’.
Conclusions
Stopping smoking is one of the greatest changes that people can make to improve their health. However, smoking cessation can be a difficult topic to raise, especially when a person's main reason for consulting is their mental health or another health concern. Evidence suggests that smoking may cause some mental health problems and that the tobacco withdrawal cycle partly contributes to worse mental health. By stopping smoking, a person's mental health may improve, and the size of this improvement might be equal to that of taking antidepressants. By drawing on evidence-based methods such as behavioural support and CBT, healthcare professionals can address smoking cessation in a compassionate and respectful manner and successfully integrate smoking cessation treatment into routine care.
Author contributions
G.M.J.T. led on conceptualisation, investigation, writing the manuscript, reviewing and editing the manuscript and coordinating project administration. P.A. and M.R.M. supervised and mentored G.M.J.T. in writing the manuscript. P.A., A.L.B., D.S.K., M.R.M. and N.F. all contributed equally to conceptualisation, investigation, writing the manuscript, and reviewing and editing the manuscript. All authors contributed to the content of the manuscript.
Funding
G.M.J.T. is funded by a Cancer Research UK Population Researcher Postdoctoral Fellowship (C56067/A21330). A.L.B. is funded by a National Health and Medical Research Council (NHMRC) Senior Research Fellowship (G1601524). P.A. is a National Institute for Health Research (NIHR) senior investigator and is funded by NIHR Oxford's Biomedical Research Centre and Applied Research Centre. M.R.M. is a programme lead in the Medical Research Council Integrative Epidemiology Unit at the University of Bristol (MC_UU_00011/7).
Declaration of interest
G.M.J.T. and M.R.M. have previously received funding from Pfizer, who manufacture smoking cessation products. P.A. led a trial funded by the NIHR and GlaxoSmithKline donated nicotine patches to the NHS in support of the trial. A.L.B. led trials funded by the NHMRC and GlaxoSmithKline donated nicotine replacement therapy in support of the trials.
ICMJE forms are in the supplementary material, available online at https://doi.org/10.1192/bja.2020.52.
MCQs
1 The best way to support smoking cessation for people with common mental health problems is:
a to recommend that they try to quit once their mental health improves
b to recommend a combination of smoking cessation medicine and behavioural support for smoking cessation
c to suggest that they use will power and nicotine replacement therapy
d to suggest that they go to their pharmacy for over-the-counter nicotine replacement therapy
e not to recommend smoking cessation, as smoking tobacco offers stress relief.
2 In the ‘very brief advice’ approach to smoking cessation, the three A's stand for:
a ask, advise, act
b avoid, advise, assist
c argue, advise, assist
d ask, assess, assist
e aid, assess, advise.
3 After smoking a cigarette, tobacco withdrawal symptoms start within:
a 1 hours
b 24 hours
c 20 minutes
d 2–3 hours
e 12 hours.
4 Generally, quitting smoking is associated with:
a worse mental health recovery
b inability to cope with symptoms of mental health problems
c long-term improvements in common mental health problems
d needing a higher dose of antidepressants
e none of the above.
5 Smoking is a risk factor in the development of:
a cancers and heart disease
b depression
c schizophrenia
d poor quality of life
e of the above.
MCQ answers
1 b 2 a 3 c 4 c 5 e








eLetters
No eLetters have been published for this article.