It was recently reported that more than 30 000 people in Japan die by suicide annually (the suicide rate in 1998 was 25.4 per 100 000), one of the highest suicide rates in the world, and that more than 40% of Japanese suicide victims are middle-aged (in their 40s and 50s; Reference TakahashiTakahashi, 2002). Heavy alcohol consumption is among the well-known risk factors for suicide (Reference Harris and BarracloughHarris & Barraclough, 1997; Reference MannMann, 2002), and the lifetime suicide rate is estimated to be 7% among those who misuse alcohol (Reference Inskip, Harris and BarracloughInskip et al, 1998). However, few studies have investigated the association between alcohol consumption and subsequent completion of suicide using a validated measurement of alcohol consumption in a large population-based cohort. The purpose of the present study was to investigate the association between alcohol consumption and suicide based on the data obtained from middle-aged males in the Japan Public Health Centre-Based Prospective Study (JPHC Study) cohort.
METHOD
Study cohort
This study was conducted as part of the JPHC study, which began in 1990 for Cohort I and in 1993 for Cohort II. The study population was defined as all residents aged 40–59 years in Cohort I and 40–69 years in Cohort II at baseline who had registered their addresses in 27 municipalities supervised by nine public health centres. We established a population-based cohort of 57 714 men (27 063 in Cohort I and 30 651 in Cohort II). Details of the study design have been reported elsewhere (Reference Watanabe, Tsugane and SobueWatanabe et al, 2001). The JPHC study was approved by the institutional review board of the National Cancer Centre, Tokyo, Japan.
Baseline questionnaire survey
A self-administered questionnaire was distributed to all cohort members in 1990 (Cohort I) and 1993–4 (Cohort II), mostly between February and March, to determine socio-demographic characteristics, personal medical history, smoking status, alcohol intake, alcohol-related flushing, physical activity, and other lifestyle-related factors (e.g. food intake). The questionnaire used for Cohort II was modified to include questions on social support.
Alcohol consumption
In Cohort I, we defined non-drinkers (<1 day/month), occasional drinkers (1–3 days/month) and regular drinkers (1–2 days/week or more) based on the frequency of alcohol consumption. Subjects in Cohort II were asked about their alcohol consumption habits, i.e. whether they were never, ex-, or current drinkers. To match the variables of alcohol intake in the two cohorts, the ‘non-drinker’ category was defined as never drinkers and ex-drinkers combined in Cohort II. Current drinkers were divided into occasional drinkers (1–3 days/month) and regular drinkers (1–2 days/week or more), based on the frequency of consumption. Among regular drinkers, weekly ethanol intake was calculated by multiplying frequency per week by the amount of alcohol consumed daily. The amount of ethanol in each alcoholic drink was calculated as follows: 180 ml sake (rice wine) as 23 g ethanol, 180 ml shochu or awamori (white spirits) as 36 g, 633 ml beer as 23 g, 30 ml whisky or brandy as 10 g and 60 ml wine as 6 g. The method for calculating ethanol intake has been reported in detail elsewhere (Reference Tsugane, Fahey and SasakiTsugane et al, 1999; Reference Sobue, Yamamoto and WatanabeSobue et al, 2001). Participants were classified into six groups: non-drinkers, occasional drinkers, and four groups of regular drinkers according to the quartile of weekly ethanol intake (<138 g/week, 138–251 g/week, 252–413 g/week and ≥414 g/week).
To evaluate the validity of the estimation of alcohol intake from the baseline questionnaires, we collected four 7-day dietary records (a total of 28 days) from volunteers in each cohort. Spearman's rank correlations for estimated alcohol intake between the baseline questionnaires and dietary records were 0.79 in 94 men in Cohort I (Reference Tsubono, Kobayashi and SasakiTsubono et al, 2003) and 0.59 in 176 men in Cohort II (unpublished data). This indicates that our questionnaire had moderate validity for ranking participants according to their alcohol consumption.
Facial flushing
Previous studies have indicated that approximately half of those from East Asia have very low aldehyde dehydrogenase 2 (ALDH2) activity. This enzyme limits alcohol intake by means of the unpleasant symptoms that occur after alcohol consumption owing to the low capacity to metabolise aldehyde (Reference Ferguson and GoldbergFerguson & Goldberg, 1997). Facial flushing after alcohol consumption is an excellent indicator of the presence of inactive ALDH2 (Reference Takeshita, Morimoto and MaoTakeshita et al, 1993; Reference Yokoyama, Muramatsu and OhmoriYokoyama et al, 1997). Moreover, facial flushing is well known to be associated with reduction in both drinking and progression to alcoholism (Reference Higuchi, Parrish and DufourHiguchi et al, 1992). Thus since the mechanism underlying the association of alcohol consumption and suicide is not clear (Reference HuffordHufford, 2001) we also investigated the relationship between alcohol consumption and suicide in individuals with and without facial flushing. A facial flushing questionnaire was used, which Yokoyama et al (Reference Yokoyama, Muramatsu and Ohmori1997) reported had good reliability (high sensitivity and specificity) for inactive ALDH2.
Follow-up and identification of suicide
We followed all participants from baseline until 31 December 1999 for Cohort I and 31 December 2000 for Cohort II. Data on migration were obtained from the residential registry annually. Of the initial participants, 1966 (4.3%) moved out of the study area and 36 (0.08%) were lost to follow-up. Data on deaths of participants who remained in their original area were based on death certificates from the local public health centre. For those who died after moving from their original area, the cause of death was extracted from death certificates kept by the Ministry of Health, Labour and Welfare, Japan. Death by suicide was defined according to ICD–10 (World Health Organization, 1992) as codes X60–X84. All death certificates in Japan are submitted to a local government office and forwarded to the public health centre in the area of residence. Mortality data are then sent to the Ministry of Health, Labour and Welfare and coded for National Vital Statistics. Registration of deaths is mandatory in Japan under the Family Registration Law and death certificates must be completed by a licensed physician. The verdict of suicide is based on the results of the medico-legal examination by a licensed physician and the police investigation as required by Japanese law. Thus, the data are believed to be sufficient in terms of quality and completeness.
Statistical analysis
Person-years of follow-up were calculated from baseline until the date of suicide, the most recent date when survival status was confirmed in censored cases, and at the end of the study periods (31 December 1999 for Cohort I and 31 December 2000 for Cohort II) for survivors, whichever occurred first. The crude suicide rate was calculated by dividing the number of suicide cases by the number of person-years. For each cohort, the Cox proportional hazards model was used to estimate relative risk (RR) and 95% confidence intervals (CIs) of suicide related to alcohol consumption at baseline using the SAS program version 8.2 for Windows (PROC PHREG; SAS Institute, Cary, North Carolina, USA). The RRs were adjusted for age, area, living alone and unemployment. Linear trends were tested in the Cox proportional hazards models by treating the categories as ordinal variables. The interaction test was performed for facial flushing status. All P values reported are two-sided and the significance level was set at P<0.05.
We used the fixed-effects model to combine the loge RRs; the cohort-specific RRs were weighted by the inverse of their variance after testing for heterogeneity among cohorts (Reference PetittiPetitti, 1994). The pooled P value for the interaction test was calculated by the sum of logs method (Reference Becker, Cooper and HedgesBecker, 1994).
RESULTS
A total of 45 452 men (79%), 20 658 in Cohort I and 24 794 in Cohort II, returned the questionnaire. We excluded those for whom information on alcohol consumption was incomplete (2069 men (4.6%), including 6 who died by suicide). Among 367 817 person-years of observation of 43 383 men (mean follow-up=8.5 years), there were 168 (0.39%) suicides (97 in Cohort I and 71 in Cohort II). At baseline (Table 1), regular drinkers in Cohorts I and II who consumed more than 414 g of ethanol per week were more likely to smoke and less likely to have facial flushing than occasional drinkers. Non-drinkers were more likely to be receiving medication and to be unemployed. The proportion of men taking medication was highest among the exdrinkers. Data on social support variables were available for Cohort II. Non-drinkers were less likely to have close friends and confidants than others. These data were not available for Cohort I.
Table 1 Baseline characteristics of Cohorts I and II of the Japan Public Health Centre-Based Prospective Study Group (men aged 40-69) according to alcohol consumption
| Non-drinkers | Occasional drinkers | Regular drinkers1, weekly ethanol intake (g) | |||||
|---|---|---|---|---|---|---|---|
| Never drinkers | Ex-drinkers | <138g | 138-251g | 252-413g | ≥414g | ||
| Cohort I | |||||||
| Number of men | 4287 | 2200 | 2978 | 3785 | 3436 | 3522 | |
| Age, years: mean | 50.2 | 49.0 | 49.3 | 49.3 | 49.6 | 49.3 | |
| Living alone, % | 3.0 | 3.0 | 2.7 | 2.4 | 1.9 | 2.1 | |
| Unemployed, % | 8.5 | 3.2 | 3.0 | 1.8 | 2.0 | 2.5 | |
| Any medicines, % | 27.4 | 19.0 | 20.9 | 21.3 | 22.9 | 24.6 | |
| Current smokers, % | 47.5 | 46.3 | 45.4 | 52.7 | 59.4 | 64.4 | |
| Flushers, % | 65.8 | 64.7 | 57.5 | 51.9 | 46.5 | 44.0 | |
| Cohort II | |||||||
| Number of men | 5018 | 1021 | 1966 | 3614 | 3847 | 3605 | 4104 |
| Age, years: mean | 56.5 | 59.2 | 52.2 | 52.8 | 54.1 | 53.4 | 53.6 |
| Living alone, % | 4.1 | 4.6 | 3.9 | 3.5 | 2.8 | 3.3 | 3.3 |
| Unemployed, % | 13.8 | 23.7 | 5.3 | 6.1 | 6.3 | 4.3 | 5.1 |
| Having no person who makes you feel comfortable and/or safe, % | 26.0 | 25.7 | 24.0 | 18.8 | 22.0 | 22.4 | 24.6 |
| Having no friend who you talk to once a week or more, % | 18.3 | 20.7 | 15.4 | 14.8 | 15.8 | 15.3 | 14.9 |
| Having no person who agrees with and/or supports your actions and/or ideas, % | 19.4 | 20.3 | 14.1 | 13.0 | 13.5 | 13.4 | 16.4 |
| Having no person to whom you can talk about personal feelings or secrets, % | 25.0 | 24.3 | 23.3 | 19.8 | 22.5 | 21.5 | 22.9 |
| Any medicines, % | 35.6 | 65.8 | 26.5 | 28.7 | 30.1 | 28.4 | 29.0 |
| Current smokers, % | 47.5 | 43.3 | 47.5 | 43.8 | 50.8 | 58.1 | 61.9 |
| Flushers, % | 70.1 | 48.0 | 62.3 | 53.0 | 43.8 | 36.6 | 32.5 |
The association between alcohol consumption at baseline and subsequent death by suicide is shown in Table 2. Compared with occasional drinkers, the pooled multivariate RRs for non-drinkers and regular drinkers who consumed more than 414 g of ethanol per week were 2.3 (95% CI 1.2–4.6) and 2.3 (95% CI 1.2–4.7) respectively. Among non-drinkers in Cohort II, ex-drinkers had a significantly increased risk of suicide compared with occasional drinkers, but never drinkers did not, even after adjusting for potential confounders. Among drinkers the risk of suicide increased with the amount of ethanol consumed, and the trend test revealed statistical significance (P for trend=0.004). There is a U-shaped association between alcohol consumption and subsequent death by suicide (Fig. 1).
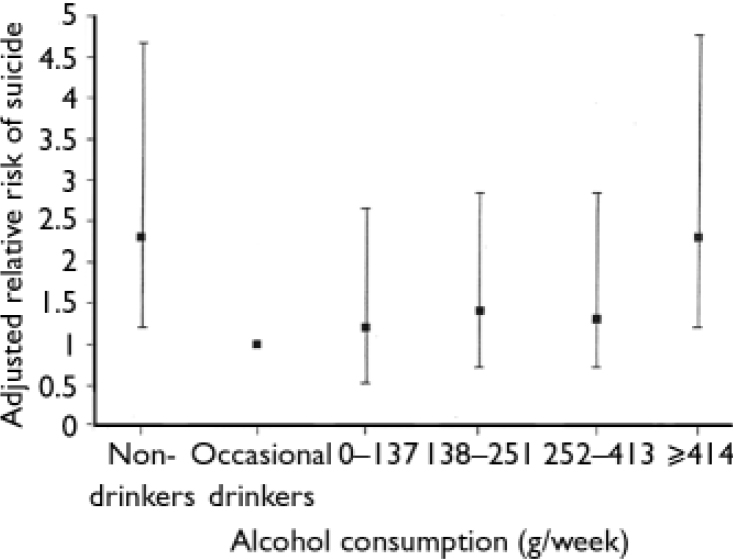
Fig. 1 Relative risk of suicide after adjustment for age, area, living alone and employment status according to alcohol consumption. Bars represent 95% confidence intervals.
Table 2 Relative risk of suicide according to alcohol consumption
| Never drinkers | Ex-drinkers | Non-drinkers | Occasional drinkers | Regular drinkers1, weekly ethanol intake (g) | P for trend among drinkers | ||||
|---|---|---|---|---|---|---|---|---|---|
| <138 g | 138-251 g | 252-413 g | ≥414 g | ||||||
| Cohort I | |||||||||
| Number of suicides | 29 | 7 | 10 | 14 | 12 | 25 | |||
| Person-years | 41 216 | 21 310 | 28 956 | 36 778 | 33 349 | 33 864 | |||
| Crude suicide rate | 70.4 | 32.8 | 34.5 | 38.1 | 36.0 | 73.8 | |||
| Age/area-adjusted RR (95% Cl)2 | 2.2 (0.9-4.9) | 1.0 | 1.1 (0.4-2.8) | 1.2 (0.5-3.0) | 1.2 (0.5-3.0) | 2.3 (0.98-5.4) | 0.02 | ||
| Multivariate RR (95% Cl)3 | 2.2 (0.96-5.1) | 1.0 | 1.0 (0.4-2.6) | 1.2 (0.5-3.1) | 1.2 (0.5-3.1) | 2.3 (0.99-5.4) | 0.01 | ||
| Cohort II | |||||||||
| Number of suicides | 13 | 10 | 23 | 3 | 9 | 10 | 10 | 16 | |
| Person-years | 36 866 | 7116 | 43 982 | 14 855 | 27 065 | 28 744 | 27 007 | 30 691 | |
| Crude suicide rate | 35.3 | 140.5 | 52.3 | 20.2 | 33.3 | 34.8 | 37.0 | 52.1 | |
| Age/area-adjusted RR (95% Cl)2 | 1.8 (0.5-6.2) | 7.0 (1.9-25.9) | 2.6 (0.8-8.7) | 1.0 | 1.6 (0.4-6.1) | 1.7 (0.5-6.1) | 1.7 (0.5-6.4) | 2.5 (0.7-8.6) | 0.13 |
| Multivariate RR (95% Cl)3 | 1.7 (0.5-6.2) | 6.7 (1.8-25.0) | 2.5 (0.7-8.5) | 1.0 | 1.6 (0.4-6.1) | 1.7 (0.5-6.1) | 1.8 (0.5-6.5) | 2.5 (0.7-8.7) | 0.12 |
| Pooled estimates | |||||||||
| Multivariate RR (95% Cl)3 | 2.3 (1.2-4.6) | 1.0 | 1.2 (0.5-2.6) | 1.4 (0.6-2.9) | 1.3 (0.6-2.9) | 2.3 (1.2-4.7) | 0.004 | ||
To maintain statistical power, we recategorised drinkers into three groups. Because groups of occasional drinkers and regular drinkers who consumed 138–251 g ethanol showed almost the same risk as groups of regular drinkers who consumed less than 138 g and 252–413 g ethanol respectively, we combined these categories. Thereafter, we analysed the association between alcohol consumption and subsequent death by suicide among drinkers further adjusting for flushing status. Regular heavy drinkers who consumed more than 414 g of ethanol per week had a significantly higher risk of suicide than those who drank occasionally or consumed less than 138 g of ethanol per week (pooled multivariate RR=2.3, 95% CI 1.4–3.8).
Among men for whom data on alcohol-related flushing status were available (n=39 241), 43.2% reported being non-flushers and 56.8% being flushers. Flushers did not have a significantly increased risk of suicide compared with non-flushers (pooled multivariate RR=1.3, 95% CI 0.9–1.8). To determine whether alcohol consumption differed in terms of subsequent death by suicide between non-flushers and flushers, we analysed the data in separate facial flushing strata. Among non-flushers, a non-significant elevated risk was observed for regular drinkers who consumed more than 414 g of ethanol per week (pooled multivariate RR=2.1, 95% CI 0.9–4.7) compared with those who drank occasionally or consumed less than 138 g of ethanol per week; a borderline significant positive trend was also found (P for trend=0.07; Fig. 2). Among flushers, regular drinkers who consumed more than 414 g of ethanol per week had a significantly increased risk (pooled multivariate RR=2.5, 95% CI, 1.3–4.8) compared with those who drank occasionally or consumed less than 138 g of ethanol per week, and a positive trend was observed (P for trend=0.007). The interaction test for facial flushing status did not show statistical significance (P=0.96).
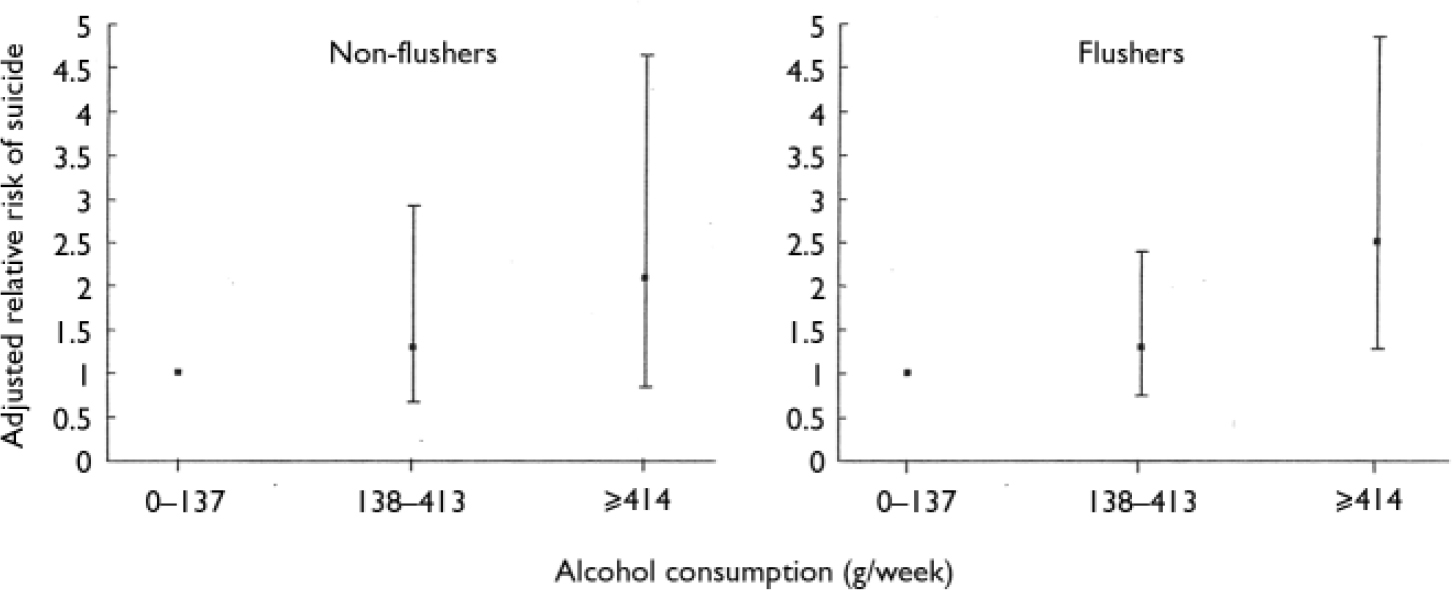
Fig. 2 Relative risk of suicide after adjustment for age, area, living alone and employment status according to alcohol consumption in flushers and non-flushers. Bars represent 95% confidence intervals.
To exclude effects of other potential confounders, the RRs were further adjusted for medication, past history of any chronic diseases, self-reported stress, smoking status, body mass index, and sports and physical exercise in leisure time. However, the results did not substantially change after adjustment (data not shown). To eliminate effects of preclinical diseases, we performed analyses that excluded the first 2 years of follow-up. The pooled RR in non-drinkers was attenuated and the statistical significance of the association disappeared (pooled multivariate RR=1.8, 95% CI 0.9–3.7). In Cohort II, the RRs were attenuated in both never drinkers (multivariate RR=1.2, 95% CI 0.3–4.4) and ex-drinkers (multivariate RR=6.0, 95% CI 1.6–22.7) but the statistical significance was still observed in the ex-drinkers. To account for the possible under-reporting of suicide cases, the association of alcohol consumption with suicide was examined including deaths from undetermined causes (ICD–10 code Y10–Y34, n=19) as suicide cases. However, we observed a similar U-shaped association (data not shown).
DISCUSSION
Association between alcohol consumption and suicide
This is the first study to show a U-shaped association between alcohol consumption and subsequent death by suicide on the basis of validated measurement of alcohol consumption in two large Japanese population-based middle-aged male cohorts.
To the best of our knowledge, only five cohort studies have investigated the association between alcohol consumption and subsequent suicide (Reference Paffenbarger, King and WingPaffenbarger et al, 1969; Reference Ross, Bernstein and TrendRoss et al, 1990; Reference Andreasson, Romelsjo and AllebeckAndreasson et al, 1991; Reference Klatsky and ArmstrongKlatsky & Armstrong, 1993; Reference Turvey, Conwell and JonesTurvey et al, 2002) but their findings were inconsistent. Three of these reports indicated that individuals consuming large amounts of alcohol were more likely to die by suicide than those who never drank or consumed moderate amounts (Reference Ross, Bernstein and TrendRoss et al, 1990; Reference Andreasson, Romelsjo and AllebeckAndreasson et al, 1991; Reference Klatsky and ArmstrongKlatsky & Armstrong, 1993). The other two studies found no significant association (Reference Paffenbarger, King and WingPaffenbarger et al, 1969; Reference Turvey, Conwell and JonesTurvey et al, 2002). Our present findings indicate that heavy drinkers among middle-aged Japanese men, who constitute the majority of Japanese suicide victims, are not the only group vulnerable to subsequent death by suicide. Non-drinkers are also at risk. The increased risk for death by suicide among non-drinkers was an unexpected finding, and there are several possible explanations.
First, because the findings were somewhat attenuated after excluding the first 2 years of follow-up, non-drinkers might have several underlying physical diseases, which could be risk factors for later suicide. Second, one epidemiological study investigating drinking habits and depression among middle-aged and elderly Japanese males revealed a significantly higher degree of depression among non-drinkers than among moderate and even problem drinkers (Reference Sato, Shouji and SenohSato et al, 1990). Underlying depression in non-drinkers may contribute to the higher risk for suicide. Third, non-drinkers in Cohort II perceived less social support, for example, in the form of close friends and confidants, and this might contribute to the increased risk of subsequent suicide (Reference Heikkinen, Aro and LonnqvistHeikkinen et al, 1993). There might also be other factors associated with a non-drinking lifestyle, such as specific personality traits, coping strategies, religious beliefs and a past history of alcohol dependence, although we do not have clear empirical data supporting the association. Finally, the difference between never drinkers and ex-drinkers which are both classed as non-drinkers in the present study, should be considered more carefully because each showed different RR compared with occasional drinkers in Cohort II. An increased risk of suicide might be observed only in exdrinkers but not in never drinkers. Our findings, like those of other health outcomes (Reference de Lorimierde Lorimier, 2000), suggest a U-shaped association between alcohol consumption and suicide. However, further research is needed to determine why non-drinkers are more likely to die by suicide than moderate drinkers.
Alcohol-related flushing and suicide
The dose–response effect of alcohol consumption on death by suicide was significant in regular drinkers with alcohol-related flushing, although a borderline significance was also observed among non-flushers and the interaction test for facial flushing did not yield statistically significant results. Several recent studies have demonstrated potential roles for genetic factors, including polymorphisms, in psychiatric disorders that are associated with suicide behaviours (Reference Hasegawa, Higuchi and MatsushitaHasegawa et al, 2002; Reference Huang, Oquendo and FriedmanHuang et al, 2003) but the current findings do not suggest any clearly different effect of alcohol consumption on suicide among non-flushers (active ALDH2) and flushers (inactive ALDH2).
Methodological advantages of this study
Our study had several methodological advantages. First, the prospective design made it possible to avoid recall bias. Most epidemiological studies of alcohol consumption and suicide have used a retrospective design with proxy respondents. Second, this study included a large population-based sample with a high response rate (approximately 80%) and a very low rate of loss to follow-up. Third, we measured alcohol consumption using a validated questionnaire, whereas most previous cohort studies did not use a validated measurement for alcohol consumption (Reference Paffenbarger, King and WingPaffenbarger et al, 1969; Reference Ross, Bernstein and TrendRoss et al, 1990; Reference Andreasson, Romelsjo and AllebeckAndreasson et al, 1991; Reference Turvey, Conwell and JonesTurvey et al, 2002). Fourth, the similar findings in the two cohorts strengthens the results.
Limitations
Our study had some limitations. First, several important items of data were not available because the primary aims of the cohort (JPHC Study) did not include provision of evidence for suicide. In particular, the lack of any data on psychiatric disorders such as depression and alcohol misuse/dependence is the most important limitation. Second, because the numbers of suicides are small in each alcohol consumption group, the results might be overinterpreted. Third, ICD–10 suicide statistics might not be reliable because under-reporting and misclassification of suicide can occur (such as accidental drowning and poisonings) and any event in the undetermined intent category can be misclassified as suicide (Reference Rockett and SmithRockett & Smith, 1993). However, this type of misclassification would be unlikely to have influenced the results because we observed similar results after taking deaths from undetermined causes into account. Fourth, there may be measurement errors in the alcohol consumption and other lifestyle factors resulting from the use of the questionnaire. In addition, the influence of modification of drinking habits during the follow-up period cannot be ignored. A reduction or increase of alcohol consumption might lead to attenuation of the true association. Fifth, since two of the metropolitan areas were excluded because of different definitions of the study population, our findings may not be directly generalisable to the entire Japanese urban population. However, our findings can at least be generalised to middle-aged and elderly Japanese men in rural areas. Finally, because the participants were middle-aged Japanese men, the findings may not be applicable to those from different generations and/or to women.
Further research
Although there are several limitations, the observed association between alcohol consumption and suicide is still important, and future studies, particularly of the cooccurrence of alcohol dependence and mood disorders, should yield interesting results.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ There is a U-shaped association between alcohol consumption and subsequent suicide in middle-aged Japanese males.
-
▪ Non-drinkers are also candidates for suicide prevention efforts.
-
▪ There is no clearly different effect of alcohol consumption on suicide among non-flushers (inactive aldehyde dehydrogenase 2) and flushers (active aldehyde dehydrogenase 2).
LIMITATIONS
-
▪ Potential confounding factors, especially psychiatric disorders and individual characteristics, may remain unaccounted.
-
▪ Suicide statistics may not be reliable because under-reporting and misclassification of suicide can occur.
-
▪ Since two metropolitan areas were excluded and the participants were middle-aged Japanese men, our findings may not be generalisable to the entire Japanese urban population and to different generations and/or women.
Acknowledgements
We thank all staff members in each study area and central offices for their cooperation and technical assistance. We also thank Dr S. Yamamoto of the Statistics and Cancer Control Division, Research Centre for Cancer Prevention and Screening, National Cancer Centre, Tokyo, Japan for hisstatistical advice, and Dr T. Hayashi of the Cellular Pathobiology Unit, Cellular Neurobiology Research Branch, Intramural Research Programme, National Institute on Drug Abuse, National Institute for Health and Dr T. Otani of the Epidemiology and Prevention Division, Research Centre for Cancer Prevention and Screening, National Cancer Centre, Tokyo, Japan for their helpful comments.
This study was supported by a Grant-in-Aid from the Cancer Research and Second-Term Comprehensive Ten-Year Strategy for Cancer Control from the Ministry of Labour, Health and Welfare of Japan.
Members of the JPHC Study Group (principal investigator S.Tsugane):M.Inoue, T.Hanaoka, S. Tsugane): M. Inoue, T. Hanaoka, S. Tsugane, S. Yamamoto and T. Sobue, Research Centre for Cancer Prevention and Screening, National Cancer Centre, Tokyo; J. Ogata, S. Baba, T. Mannami and A. Okayama, National Cardiovascular Centre, Suita; K. Miyakawa, F. Saito, A. Koizumi, Y. Sano and I. Hashimoto, Iwate Prefectural Ninohe Public Health Centre, Ninohe; Y. Miyajima, N. Suzuki, S. Nagasawa and Y. Furusugi, Akita Prefectural Yokote Public Health Centre, Yokote; H. Sanada, Y. Hatayama, F. Kobayashi, H. Uchino, Y. Shirai, T. Kondo, R. Sasaki and Y. Watanabe, Nagano Prefectural Saku Public Health Centre, Saku; Y. Kishimoto, E. Takara, T. Fukuyama, M. Kinjo and M. Irei, Okinawa Prefectural Ishikawa (Chubu) Public Health Centre, Ishikawa; K. Imoto, H. Yazawa, T. Seo, A. Seiko and F. Ito, Katsushika Public Health Centre, Tokyo; A. Murata, K. Minato, K. Motegi and T. Fujieda, Ibaraki Prefectural Kasama (Mito) Public Health Centre, Mito; K. Matsui, T. Abe and M. Katagiri, Niigata Prefectural Kashiwazaki Public Health Centre, Kashiwazaki; M. Doi, A. Terao and Y. Ishikawa; Kochi Prefectural Tosayamada (Chuo-higashi) Public Health Centre, Tosayamada; H. Sueta, H. Doi, M. Urata, N. Okamoto and F. Ide, Nagasaki Prefectural Arikawa (Kamigoto) Public Health Centre, Arikawa; H. Sakiyama, N. Onga and H. Takaesu, Okinawa Prefectural Miyako Public Health Centre, Hirara; F. Horii, I. Asano, H.Yamaguchi, K. Aoki, S. Maruyama and M. Ichii, Osaka Prefectural Suita Public Health Centre, Suita; S. Matsushima and S. Natsukawa, Saku General Hospital, Usuda; S. Watanabe and M. Akabane, Tokyo University of Agriculture, Tokyo; M. Konishi and K. Okada, Ehime University, Matsuyama; H. Iso and Y. Honda, Tsukuba University, Tsukuba; H. Sugimura, Hamamatsu University, Hamamatsu; Y. Tsubono, Tohoku University, Sendai; M. Kabuto, National Institute for Environmental Studies, Tsukuba; S. Tominaga, Aichi Cancer Centre Research Institute, Nagoya; M. Iida and W. Ajiki, Osaka Medical Centre for Cancer and Cardiovascular Disease, Osaka; S. Sato, Osaka Medical Centre for Health Science and Promotion, Osaka; N. Yasuda, Kochi University, Kochi; S. Kono, Kyushu University, Fukuoka; K. Suzuki, Research Institute for Brain and Blood Vessels, Akita; Y. Takashima, Kyorin University, Mitaka; E. Maruyama, Kobe University, Kobe; the late M. Yamaguchi, Y. Matsumura and S. Sasaki, National Institute of Health and Nutrition, Tokyo; T. Kadowaki, Tokyo University, Tokyo, Japan.







eLetters
No eLetters have been published for this article.