Introduction
Major depressive disorder (MDD) is the leading cause of disability in the world and is associated with personal, family, and social burdens (WHO, 2017). In psychiatry, treatment is prescribed on an empirical basis based on clinical profile. Pharmacological and non-pharmacological treatments are available; however, antidepressants are used more frequently than psychological interventions because of inadequate resources (Cipriani et al., Reference Cipriani, Furukawa, Salanti, Chaimani, Atkinson, Ogawa and Geddes2018). When considering the risk-benefit profile of antidepressants in the acute treatment of MDD, these drugs do not seem to offer a clear advantage for young populations (Cipriani et al., Reference Cipriani, Zhou, Del Giovane, Hetrick, Qin, Whittington and Xie2016). Moreover, antidepressants entail side effects and complications, highlighting the importance of alternative therapeutic strategies. Thus, emerging evidence encourages a more integrative approach for MDD and suggests that lifestyle factors such as diet, exercise, and sleep also play a significant mediating role in the development, progression, and treatment of MDD (Jacka et al., Reference Jacka, Kremer, Leslie, Berk, Patton, Toumbourou and Williams2010; Jacka et al., Reference Jacka, Pasco, Williams, Leslie, Dodd, Nicholson and Berk2011; Lopresti, Hood, & Drummond, Reference Lopresti, Hood and Drummond2013; Opie et al., Reference Opie, Itsiopoulos, Parletta, Sanchez-Villegas, Akbaraly, Ruusunen and Jacka2017). Accordingly, lifestyle modification should serve as a routine part of treatment and preventative efforts (Sarris, O'Neil, Coulson, Schweitzer, & Berk, Reference Sarris, O'Neil, Coulson, Schweitzer and Berk2014). In this context, there is increasing recognition of the importance of some nutritional components in MDD (Libuda, Antel, Hebebrand, & Focker, Reference Libuda, Antel, Hebebrand and Focker2017). For example, it is evident that vitamin D might influence risk, pathogenesis, persistence, and treatment of MDD (Bersani et al., Reference Bersani, Ghezzi, Maraone, Vicinanza, Cavaggioni, Biondi and Pasquini2019).
Vitamin D has long been recognized as important for bone health. In recent years, there is also growing interest in its role as a risk factor for mental health. It is quite apparent that vitamin D acts as hormone and fat-soluble vitamin, regulating the expression of more than 900 genes involved in a wide array of physiological functions (Kongsbak, Levring, Geisler, & von Essen, Reference Kongsbak, Levring, Geisler and von Essen2013; Pike et al., Reference Pike, Meyer, Martowicz, Bishop, Lee, Nerenz and Goetsch2010). In addition, vitamin D is engaged in various neural processes, such as the growth and development of neurons as well as the synthesis, release, and regulation of neurotransmitters (Kesby et al., Reference Kesby, Turner, Alexander, Eyles, McGrath and Burne2017; Patrick & Ames, Reference Patrick and Ames2015). Moreover, metabolites of vitamin D can cross the blood-brain barrier and bind to vitamin D receptors (Ryan, Anderson, & Morris, Reference Ryan, Anderson and Morris2015), which are broadly distributed in the brain (e.g. the prefrontal cortex and limbic system) (Eyles, Smith, Kinobe, Hewison, & McGrath, Reference Eyles, Smith, Kinobe, Hewison and McGrath2005), providing a mechanistic account for the role of vitamin D in emotion, cognition, and neuropsychiatric disorders (Di Somma et al., Reference Di Somma, Scarano, Barrea, Zhukouskaya, Savastano, Mele and Marzullo2017; Eyles, Burne, & McGrath, Reference Eyles, Burne and McGrath2013; Schlogl & Holick, Reference Schlogl and Holick2014). Crucially, a large number of clinical studies have provided strong evidence for an association between low vitamin D and MDD (Aghajafari, Letourneau, Mahinpey, Cosic, & Giesbrecht, Reference Aghajafari, Letourneau, Mahinpey, Cosic and Giesbrecht2018; Anglin, Samaan, Walter, & McDonald, Reference Anglin, Samaan, Walter and McDonald2013; Briggs et al., Reference Briggs, McCarroll, O'Halloran, Healy, Kenny and Laird2019; Ju, Lee, & Jeong, Reference Ju, Lee and Jeong2013; Milaneschi et al., Reference Milaneschi, Hoogendijk, Lips, Heijboer, Schoevers, van Hemert and Penninx2014; Parker, Brotchie, & Graham, Reference Parker, Brotchie and Graham2017; Wong, Chin, & Ima-Nirwana, Reference Wong, Chin and Ima-Nirwana2018), suggesting that hypovitaminosis D may represent an underlying vulnerability for depression. Several possible mechanisms that may be responsible for the link between low vitamin D and MDD have been proposed: (1) elevation in both Ca2+ and reactive oxygen species levels in neuronal cells (Berridge, Reference Berridge2015, Reference Berridge2017; Kalueff, Eremin, & Tuohimaa, Reference Kalueff, Eremin and Tuohimaa2004), (2) epigenetic alterations including the hypermethylation of gene promotors (Berridge, Reference Berridge2017; Guidotti et al., Reference Guidotti, Auta, Chen, Davis, Dong, Gavin and Tueting2011; Saavedra, Molina-Marquez, Saavedra, Zambrano, & Salazar, Reference Saavedra, Molina-Marquez, Saavedra, Zambrano and Salazar2016), (3) abnormal serotonin synthesis (Geng et al., Reference Geng, Shaikh, Han, Chen, Guo and Jiang2019), (4) excessive activation of the immune system (Geng et al., Reference Geng, Shaikh, Han, Chen, Guo and Jiang2019), and (5) dysfunctional inflammatory pathways (Alroy, Towers, & Freedman, Reference Alroy, Towers and Freedman1995; Beurel, Toups, & Nemeroff, Reference Beurel, Toups and Nemeroff2020; McCann & Ames, Reference McCann and Ames2008; Sun et al., Reference Sun, Kong, Duan, Szeto, Liao, Madara and Li2006). Moreover, a previous review concludes that vitamin D deficiency is associated with an increased risk of depression and vitamin D supplementation is of benefit for depressed individuals who are vitamin D deficient (Parker et al., Reference Parker, Brotchie and Graham2017). Another recent systematic review and meta-analysis of randomized controlled trial (RCT) suggests that vitamin D supplementation can reduce negative emotions, with patients with MDD and individuals with vitamin D deficiency most likely to benefit from supplementation (Cheng, Huang, & Huang, Reference Cheng, Huang and Huang2020). However, there are prior RCT indicating no effect of vitamin D supplementation on depression (Gowda, Mutowo, Smith, Wluka, & Renzaho, Reference Gowda, Mutowo, Smith, Wluka and Renzaho2015), or no differences in depression outcomes between vitamin D supplementation and placebo (Okereke et al., Reference Okereke, Reynolds, Mischoulon, Chang, Vyas, Cook and Manson2020; Okereke & Singh, Reference Okereke and Singh2016). The heterogeneity in these findings may be due to differences in the samples or the dosage and duration of vitamin D supplementation. Although several attempts have been made to identify the neural substrates underlying the association between low vitamin D and depression (Zhao et al., Reference Zhao, Zhu, Li, Xu, Zhang, Zhang and Yu2023; Zhao et al., Reference Zhao, Zhu, Li, Cui, Jiang, Wang and Yu2022; Zhu et al., Reference Zhu, Zhao, Zhang, Zhang, Yang, Zhang and Yu2019; Zhu et al., Reference Zhu, Zhao, Cui, Jiang, Zhang, Zhang and Yu2022), there is a paucity of longitudinal research investigating the effects of vitamin D supplementation on the brain of MDD patients.
The notion that specific cognitive and emotional processes arise from functionally distinct brain regions has lately shifted toward a connectivity-based approach that emphasizes the role of network-mediated integration across regions. Likewise, the clinical neuroscience has shifted from predominantly lesion-based approach to a connectomic paradigm, framing mental disorders including MDD as dysconnectivity syndromes. Magnetic resonance imaging (MRI) has provided a safe, non-invasive, and easily repeated neuroimaging tool to investigate the underlying neuropathology of MDD (Luo, You, DelBello, Gong, & Li, Reference Luo, You, DelBello, Gong and Li2022). Structural and functional connections of brain networks can be characterized by white matter integrity measured by diffusion tensor imaging (DTI) (Alexander, Lee, Lazar, & Field, Reference Alexander, Lee, Lazar and Field2007) and functional network connectivity measured by resting-state functional MRI (fMRI) (Fox & Raichle, Reference Fox and Raichle2007), respectively. These approaches have been widely applied to examine impairments in white matter integrity (Chen et al., Reference Chen, Guo, Zhu, Kuang, Bi, Ai and Gong2017; Chen et al., Reference Chen, Hu, Li, Huang, Lui, Kuang and Gong2016; Jiang et al., Reference Jiang, Zhao, Hu, Du, Chen, Wu and Gong2017; Yang et al., Reference Yang, Zhu, Zhang, Zhang, Wang, Zhang and Yu2020; Zhang et al., Reference Zhang, Yang, Zhu, Zhao, Zhang, Zhang and Yu2020) and functional network connectivity (Albert, Potter, Boyd, Kang, & Taylor, Reference Albert, Potter, Boyd, Kang and Taylor2019; Chen et al., Reference Chen, Liu, Zhang, Zhang, Xue, Lin and Deng2019; Jiao et al., Reference Jiao, Xu, Teng, Song, Xiao, Fox and Zhong2020; Liu et al., Reference Liu, Jiao, Zhong, Hao, Wang, Xu and Zhang2021; Liu et al., Reference Liu, Xu, Zhang, Jiang, Li and Luo2019; Liu et al., Reference Liu, Chen, Liang, Li, Zheng, Zhang and Qiu2020; Sacchet et al., Reference Sacchet, Ho, Connolly, Tymofiyeva, Lewinn, Han and Yang2016; Wu et al., Reference Wu, Zeng, Shen, Yuan, Qin, Zhang and Hu2017; Yu et al., Reference Yu, Linn, Shinohara, Oathes, Cook, Duprat and Sheline2019; Zhu et al., Reference Zhu, Zhao, Cui, Jiang, Zhang, Zhang and Yu2022) in MDD. Remarkably, using a combination of DTI and resting-state fMRI techniques, investigators have found abnormal brain structural and functional connectivity in MDD (de Kwaasteniet et al., Reference de Kwaasteniet, Ruhe, Caan, Rive, Olabarriaga, Groefsema and Denys2013; Li et al., Reference Li, Lin, Liu, Su, Zhu, Zheng and Sun2020; Yin et al., Reference Yin, He, Xu, Hou, Song, Sui and Yuan2016), pointing to the potential utility of a combined analysis of multimodal imaging data in achieving a more complete investigation of disease mechanisms.
In this study, we conducted a double-blind RCT to investigate the effects of vitamin D supplementation on brain structural and functional connectivity in MDD patients using a combination of DTI and resting-state fMRI. We hypothesized that adjuvant vitamin D supplementation therapy would help to preserve white matter integrity and functional network connectivity in addition to better ameliorating clinical symptoms.
Materials and methods
Participants
Patients were recruited consecutively from Affiliated Psychological Hospital of Anhui Medical University. Healthy controls (HC) were enrolled from the local community via poster advertisements. A total of 98 right-handed subjects were enrolled, including 72 MDD patients and 26 matched HC. Two well-trained clinical psychiatrists confirmed the diagnosis of depression using the MINI-International Neuropsychiatric Interview (M.I.N.I.) following the International Classification of Diseases (ICD-10) criteria. HC were carefully screened to confirm the absence of any psychiatric illness using the M.I.N.I. Right handedness was determined by the Edinburgh handedness inventory (Oldfield, Reference Oldfield1971). The exclusion criteria for all participants included: (1) the presence of other psychiatric disorders such as substance-induced (e.g. drug and alcohol) mood disorder, bipolar disorders, anxiety disorders, schizophrenia, substance abuse, or addiction; (2) a history of significant physical or neurological disease; (3) a history of head injury with loss of consciousness; and (4) contraindications for MRI such as pregnancy. Additional exclusion criterion for HC was a family history of major neurological or psychiatric illnesses among their first-degree relatives. For all patients, we used the 24-item Hamilton Rating Scale for Depression (HAMD) (Williams, Reference Williams1988) and the 14-item Hamilton Rating Scale for Anxiety (HAMA) (Thompson, Reference Thompson2015) to assess the severity of depression and anxiety symptoms. Notably, we used the Chinese versions of HAMD and HAMA, which have been documented to show great reliability and validity (Zheng et al., Reference Zheng, Zhao, Phillips, Liu, Cai, Sun and Huang1988) and have been widely applied in the Chinese population (Guo et al., Reference Guo, Xiang, Xiao, Hu, Chiu, Ungvari and Wang2015; Lai et al., Reference Lai, Deng, Xu, Zhao, Xu, Liu and Rong2021; Shen et al., Reference Shen, Wei, Yang, Zhang, Du, Jia and Zhang2020; Tong et al., Reference Tong, Bo, Shi, Dong, Sun, Gao and Yang2021). This study was approved by the ethics committee of The First Affiliated Hospital of Anhui Medical University. Written informed consent was obtained from all participants after being given a complete description of the study. This study was registered in the Chinese Clinical Trial Registry (ChiCTR) (Registration No: ChiCTR2100054570) at http://www.chictr.org.cn.
Study design
Following successful completion of screening, MDD patients entered a double-blind randomized controlled phase II trial. The 72 patients were randomly allocated into either VD (antidepressant medication + vitamin D supplementation; n = 36) or NVD (antidepressant medication + placebos; n = 36) groups. Both groups of patients received their regular antidepressant medication as prescribed by the attending psychiatrists, including selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), or noradrenergic and specific serotonergic antidepressants (NaSSA). VD group received vitamin D3 supplements (1600 IU/day), while NVD group received placebos of similar appearance and packaging. The adherence assessment was done based on supplement/placebo count and patient self-report. Notably, the dose of vitamin D used in this study was safe considering the upper tolerable intake level of vitamin D for adults (4000 IU/day) (Patrick & Ames, Reference Patrick and Ames2015). Both groups of patients completed two study visits: baseline (before intervention) and follow-up (after an average of 7 months of intervention). This period was selected as the follow-up visit since it is the conventional time frame for determining recovery from a depressive episode and is thus appropriate for evaluating clinical and psychosocial outcomes. MDD patients underwent serum concentration of vitamin D (SCVD) measurement, MRI examination, and clinical assessment at each visit. HC underwent SCVD measurement, MRI examination, and clinical assessment at baseline.
Serum concentration of vitamin D measurement
After an overnight fasting period, peripheral venous blood samples (2 ml) were collected from all participants in the morning of MRI scanning. Samples were sent to the Department of Clinical Laboratory, Affiliated Psychological Hospital of Anhui Medical University immediately for centrifugation and serum was separated. Vitamin D [25(OH)D] was measured in serum using a chemiluminescence immunoassay (CLIA) technique in a fully automated Maglumi 1000 analyzer (SNIBE Co., Ltd., China). Internal quality control provided by the manufacturer was used to assure quality. SCVD was stratified as follows: 30–100 ng/ml (75–250 nmol/L) as sufficiency, 20–30 ng/ml (50–75 nmol/L) as insufficiency, and <20 ng/ml (50 nmol/L) as deficiency (Ringe & Kipshoven, Reference Ringe and Kipshoven2012).
Image acquisition
MRI data were obtained on a 3.0-Tesla MR system (Discovery MR750w, General Electric, Milwaukee, WI, USA). Details regarding the image acquisition are presented in the Supplemental Materials.
White matter integrity analysis
For DTI data, standard processing steps were performed by using the FMRIB Software Library (FSL, www.fmrib.ox.ac.uk/fsl). Eddy currents in the gradient coils induce stretches and shears in the diffusion weighted images. These distortions are different for different gradient directions. Eddy current correction implemented in the FSL was adopted to correct for these distortions and simple head motions by registering the diffusion weighted images to a reference volume (i.e. the first b0 image) using affine transformations. Correspondingly, the diffusion gradient direction of each diffusion weighted image was rotated according to the resultant affine transformation information (Leemans & Jones, Reference Leemans and Jones2009). Brain tissues were extracted using FSL's brain extraction tool (http://www.fmrib.ox.ac.uk/fsl/bet2). Next, the three-dimensional maps of the diffusion tensor and fractional anisotropy (FA) were calculated by using the DTIFIT toolbox. Then, the tract-based spatial statistics (TBSS) pipeline was conducted (Smith et al., Reference Smith, Jenkinson, Johansen-Berg, Rueckert, Nichols, Mackay and Behrens2006). Briefly, individual FA images were initially non-linearly registered to the Montreal Neurological Institute (MNI) space, with a mean FA image created and thinned to generate a mean FA skeleton. Next, each subject's FA image was projected onto the skeleton via filling the mean FA skeleton with FA values from the nearest relevant tract center by searching perpendicular to the local skeleton structure for maximum FA value. Finally, the Johns Hopkins University (JHU) probabilistic white matter atlas was used to define 50 white matter tracts in the whole brain (Hua et al., Reference Hua, Zhang, Wakana, Jiang, Li, Reich and Mori2008). Mean FA within each white matter tract were extracted from the skeletonized FA images for subsequent analysis.
fMRI data preprocessing
Resting-state fMRI data were preprocessed using Statistical Parametric Mapping software (SPM12, http://www.fil.ion.ucl.ac.uk/spm) and Data Processing & Analysis for Brain Imaging (DPABI, http://rfmri.org/dpabi) (Yan, Wang, Zuo, & Zang, Reference Yan, Wang, Zuo and Zang2016). The first 10 volumes for each subject were discarded and the remaining volumes were corrected for the acquisition time delay between slices. Realignment was then performed to correct the motion between time points. Head motion parameters were computed by estimating the translation in each direction and the angular rotation on each axis for each volume. All participants' BOLD data were within the defined motion thresholds (i.e. maximum translational or rotational motion parameters less than 2.5 mm or 2.5°). We also calculated frame-wise displacement (FD), which indexes the volume-to-volume changes in head position. In the normalization step, individual structural images were firstly co-registered with the mean functional images; the transformed structural images were then segmented and normalized to the MNI space using a high-level nonlinear warping algorithm, i.e. the diffeomorphic anatomical registration through exponentiated Lie algebra (DARTEL) technique (Ashburner, Reference Ashburner2007). Finally, each functional volume was spatially normalized to the MNI space using the deformation parameters estimated during the above step and resampled into a 3-mm isotropic voxel. After spatial normalization, all datasets were smoothed with a 6 mm full-width at half-maximum (FWHM) Gaussian kernel.
Independent component analysis
ICA was conducted to parcellate the preprocessed fMRI data with the GIFT toolbox (mialab.mrn.org/software/gift/) and the number of independent components (N = 24) was estimated automatically by the software using the minimum description length criteria. Spatial ICA decomposes the participant data into linear mixtures of spatially independent components that exhibit a unique time course profile. This was achieved by using two data reduction steps. First, principal component analysis was applied to reduce the subject-specific data into 36 principle components. Next, reduced data of all subjects were concatenated across time and decomposed into 24 independent components using the infomax algorithm. To ensure estimation stability, the infomax algorithm was repeated 20 times in ICASSO (Luo et al., Reference Luo, Li, Wang, He, Wang, You and Li2023b) (http://research.ics.tkk.fi/ica/icasso/), and the most central run was selected and analyzed further. Finally, participant specific spatial maps and time courses were obtained using the GICA back reconstruction approach.
We identified as functional networks several independent components that had peak activations in gray matter, showed low spatial overlap with known vascular, ventricular, motion, and susceptibility artifacts, and exhibited primarily low-frequency power. This selection procedure resulted in 11 functional networks out of the 24 independent components obtained (online Supplementary Figure S1): anterior and posterior default mode networks (aDMN and pDMN), dorsal and ventral attention networks (DAN and VAN), posterior and medial visual networks (pVN and mVN), left and right frontoparietal networks (lFPN and rFPN), sensorimotor network (SMN), and salience network (SN), and auditory network (AN).
Before internetwork functional connectivity calculation, the following additional postprocessing steps were performed on the time courses of the selected functional networks: (1) detrending linear, quadratic, and cubic trends; (2) despiking detected outliers; and (3) low-pass filtering with a cut-off frequency of 0.15 Hz. Then, internetwork functional connectivity was estimated as the Pearson's correlation coefficients between pairs of time courses of the functional networks, resulting in a symmetric 11 × 11 correlation matrix for each subject. Finally, correlations were transformed into Fisher's Z-scores to improve normality.
Statistical analysis
The statistical analyses of demographic and clinical data were performed using the SPSS 23.0 software package (SPSS, Chicago, IL, USA). For cross-sectional analyses of baseline data, we compared age, education, body mass index (BMI), SCVD and FD among VD, NVD, and control groups using one-way analyses of variance (ANOVA). Pearson Chi-square test was used to examine group difference in gender. Two-sample t tests were utilized to compare HAMD, HAMA, illness duration, and intervention duration between VD and NVD groups. For longitudinal analyses of SCVD, HAMD and HAMA, we adopted two-way repeated-measures ANOVA that included the between-subject factor group (VD v. NVD) and the within-subject factor time (baseline v. follow-up). Potential main effects of group and time as well as group-by-time interactions were followed by appropriate two-sample t-tests for comparing groups and paired t-tests for comparing time points. In addition, we calculated longitudinal changes (follow-up - baseline) in SCVD and clinical symptoms (HAMD and HAMA), followed by Pearson's correlation analyses to test their associations within each group. A threshold of p < 0.05 was considered to indicate statistical significance.
For neuroimaging data, we initially tested differences in baseline FA of 50 white matter tracts across VD, NVD, and control groups using one-way ANOVA. Then, we used the above-described two-way repeated-measures ANOVA to assess the main effects and interactions on FA, followed by post hoc two-sample and paired t-tests. Notably, in case of a significant group-by-time interaction on FA of a white matter tract, we further adopted the same analytic strategy (i.e. a combination of two-way repeated-measures ANOVA and post hoc t-tests) to examine functional connectivity between the functional networks connected by that white matter tract. For completeness, we also carried out an exploratory investigation of other functional network connectivity. Moreover, we conducted within-group correlations between changes in neuroimaging measures (FA and functional connectivity) and clinical variables (SCVD, HAMD, and HAMA). For these analyses, multiple comparison correction was performed using the false discovery rate (FDR) method with a corrected significance level of p < 0.05.
Sensitivity analysis
To test the possible effects of antidepressants and illness duration on our results, we included antidepressant types (SSRIs, SNRIs, and NaSSA) and illness duration as nuisance covariates in our analyses.
Results
Demographic and clinical characteristics at baseline
Eligibility, examinations, randomization, and follow-up of the participants are illustrated in Fig. 1. 20 participants were lost to follow-up and six were excluded due to poor MRI quality. Ultimately, a total of 72 participants completed the study, including 20 patients in VD group, 26 patients in NVD group, and 26 HC. Out of the 26 patients in NVD group, 2 were excluded from fMRI analysis due to excessive head motion during scanning. Demographic and clinical characteristics of the participants at baseline are shown in Table 1. The three groups did not diverge on demographic variables including gender, age, education, BMI, and FD. VD and NVD groups did not differ in clinical variables including HAMD, HAMA, illness duration, and intervention duration. With respect to baseline SCVD, there was a significant difference among the three groups, with post hoc t-tests demonstrating lower SCVD in VD and NVD groups relative to HC, but no difference between VD and NVD groups (Fig. 2).

Figure 1. Flowchart of the study design. Abbreviations: HC, healthy controls; MDD, major depressive disorder; MRI, magnetic resonance imaging; SCVD, serum concentration of vitamin D; VD, vitamin D supplementation; NVD, no vitamin D supplementation; DTI, diffusion tensor imaging; fMRI, functional magnetic resonance imaging.
Table 1. Demographic and clinical characteristics of the participants at baseline

Except for gender designation, data are expressed as mean ± standard deviation.
Abbreviations: VD, vitamin D supplementation; NVD, no vitamin D supplementation; HC, healthy controls; BMI, body mass index; SCVD, serum concentration of vitamin D; FD, frame-wise displacement; HAMD, Hamilton Rating Scale for Depression; HAMA, Hamilton Rating Scale for Anxiety; SSRIs, selective serotonin reuptake inhibitors; SNRIs, serotonin norepinephrine reuptake inhibitors; NaSSA, noradrenergic and specific serotonergic antidepressant.
a The data are available for 24 of 26 patients in NVD group.
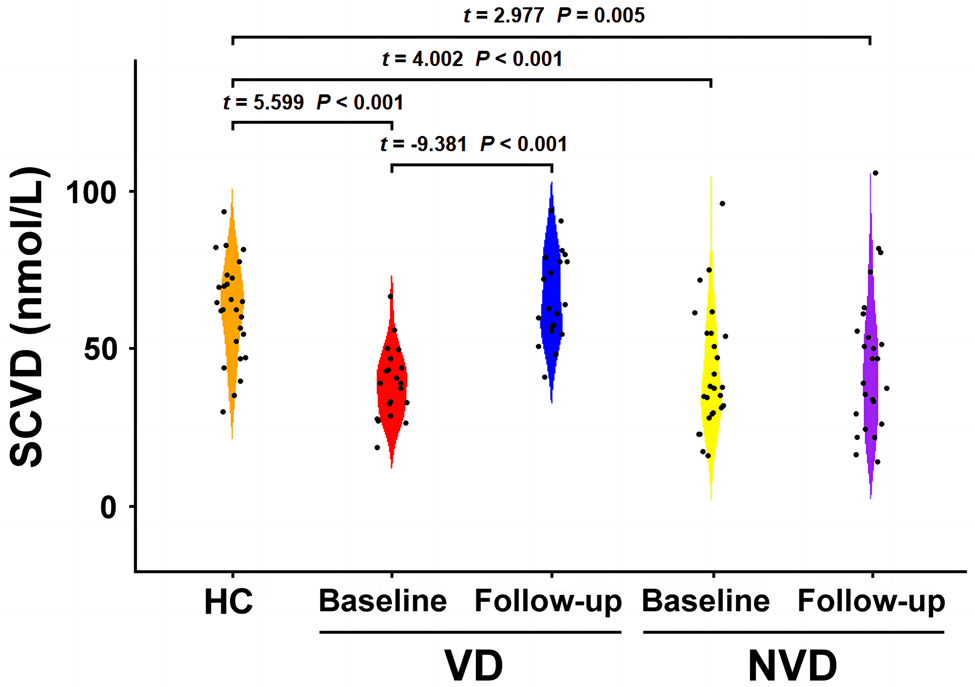
Figure 2. SCVD at baseline and follow-up. Abbreviations: HC, healthy controls; VD, vitamin D supplementation; NVD, no vitamin D supplementation; SCVD, serum concentration of vitamin D.
Serum concentration of vitamin D and clinical symptoms
Two-way repeated-measures ANOVA revealed a significant group-by-time interaction effect on SCVD (F = 44.137, p < 0.001) (Fig. 2). Post hoc analyses demonstrated increased SCVD from baseline to follow-up in VD group, but no change in NVD group. At follow-up, there was no difference in SCVD between VD and control groups, but NVD group still showed lower SCVD than HC. In terms of clinical symptoms, both VD and NVD groups exhibited significant reductions in HAMD (Fig. 3a) and HAMA (Fig. 3c) from baseline to follow-up, indicating improvement in depression and anxiety symptoms. However, no significant group-by-time interactions were found for HAMD (F = 1.119, p = 0.296) or HAMA (F = 0.124, p = 0.726). Moreover, we observed significant negative correlations of SCVD change with changes in HAMD (r = −0.539, p = 0.017) (Fig. 3b) and HAMA (r = −0.675, p = 0.002) (Fig. 3d) in VD group but not NVD group (HAMD, r = −0.099, p = 0.637; HAMD, r = −0.055, p = 0.795). None of the patients complained about adverse drug reactions.

Figure 3. Longitudinal changes in clinical symptoms and their associations with SCVD change. Changes in HAMD (a) and their associations with SCVD change in VD group (b). Changes in HAMA (c) and their associations with SCVD change in VD group (d). Abbreviations: HAMD, Hamilton Rating Scale for Depression; HAMA, Hamilton Rating Scale for Anxiety; SCVD, serum concentration of vitamin D; VD, vitamin D supplementation; NVD, no vitamin D supplementation.
White matter integrity and functional network connectivity
At baseline, FA of 50 white matter tracts did not differ among VD, NVD, and control groups (online Supplementary Table S1 in the Supplementary Materials). Two-way repeated-measures ANOVA showed a significant group-by-time interaction effect on FA of right inferior fronto-occipital fasciculus (IFOF) (F = 14.677, p < 0.001) that survived FDR correction (Fig. 4 and online Supplementary Table S2 in the Supplementary Materials). Post hoc analyses demonstrated decreased FA of right IFOF from baseline to follow-up in NVD group, but no change in VD group. At follow-up, NVD group showed lower FA of right IFOF than HC, but there was still no difference between VD group and HC.

Figure 4. FA of right IFOF at baseline and follow-up. Abbreviations: FA, fractional anisotropy; IFOF, inferior fronto-occipital fasciculus; HC, healthy controls; VD, vitamin D supplementation; NVD, no vitamin D supplementation; R, right.
Since right IFOF connects right frontal and occipital cortex, we focused our functional connectivity analyses on functional networks involving right frontal cortex (rFPN, aDMN, and VAN) and right occipital cortex (mVN and pVN). Two-way repeated-measures ANOVA revealed a significant group-by-time interaction effect on functional connectivity between rFPN and mVN (F = 7.875, p = 0.008) that survived FDR correction (Fig. 5). Post hoc analyses demonstrated decreased rFPN-mVN connectivity from baseline to follow-up in NVD group, but no change in VD group. The exploratory investigation did not reveal any significant group-by-time interaction effects on other functional networks connectivity (p > 0.05, FDR corrected) (online Supplementary Table S3 in the Supplementary Materials).

Figure 5. Functional connectivity between rFPN and mVN at baseline and follow-up. Abbreviations: HC, healthy controls; VD, vitamin D supplementation; NVD, no vitamin D supplementation; rFPN, right frontoparietal network; mVN, medial visual network.
No significant correlations between changes in neuroimaging measures (FA and functional connectivity) and clinical variables (SCVD, HAMD, and HAMA) were observed in either group (online Supplementary Table S4 in the Supplementary Materials).
Sensitivity analysis
After controlling for antidepressant types and illness duration, the group-by-time interaction effects on SCVD (F = 45.402, p < 0.001), FA of right IFOF (F = 13.744, p < 0.001), and rFPN-mVN connectivity (F = 7.657, p = 0.009) remained significant. The group-by-time interaction effects on HAMD (F = 1.342, p = 0.253) and HAMA (F = 0.088, p = 0.768) were still not significant. The correlation between changes in SCVD and HAMA remained significant (partial correlation coefficient [pr] = −0.512, p = 0.036), but the correlation between changes in SCVD and HAMD was not significant (pr = −0.357, p = 0.159).
Discussion
This is the first RCT to investigate the effects of vitamin D supplementation on brain structural and functional connectivity in MDD patients using a combination of DTI and resting-state fMRI. After an average of 7 months of intervention, both VD and NVD groups showed significant improvement in depression and anxiety symptoms, but with no significant differences between the two groups. However, a greater SCVD increase was found to be associated with greater improvement in depression and anxiety symptoms in VD group. More importantly, neuroimaging data demonstrated decreased FA of right IFOF along with decreased rFPN-mVN functional connectivity after intervention in NVD group, but no changes in VD group. The novel contribution of these findings is the demonstration that vitamin D supplementation as adjunctive therapy to antidepressants may not only contribute to improvement in clinical symptoms but also help to preserve white matter integrity and functional network connectivity in MDD patients, supporting the neuroprotective and anti-inflammatory role of vitamin D.
Previous studies examining the effects of vitamin D supplementation on MDD have produced mixed findings, with some demonstrating that vitamin D supplementation is beneficial for depression treatment and prevention (Alavi, Khademalhoseini, Vakili, & Assarian, Reference Alavi, Khademalhoseini, Vakili and Assarian2019; Alghamdi et al., Reference Alghamdi, Alsulami, Khoja, Alsufiani, Tayeb and Tarazi2020; Casseb, Kaster, & Rodrigues, Reference Casseb, Kaster and Rodrigues2019; Cheng et al., Reference Cheng, Huang and Huang2020; de Koning et al., Reference de Koning, van Schoor, Penninx, Elders, Heijboer, Smit and Lips2015; Kaviani, Nikooyeh, Zand, Yaghmaei, & Neyestani, Reference Kaviani, Nikooyeh, Zand, Yaghmaei and Neyestani2020; Khoraminya, Tehrani-Doost, Jazayeri, Hosseini, & Djazayery, Reference Khoraminya, Tehrani-Doost, Jazayeri, Hosseini and Djazayery2013; Parker et al., Reference Parker, Brotchie and Graham2017) and others showing no effects (Gowda et al., Reference Gowda, Mutowo, Smith, Wluka and Renzaho2015; Okereke et al., Reference Okereke, Reynolds, Mischoulon, Chang, Vyas, Cook and Manson2020; Okereke & Singh, Reference Okereke and Singh2016). These heterogeneous results may be attributed to differences in the samples or the dosage and duration of vitamin D supplementation. In our RCT, the antidepressants plus vitamin D supplements combination was not superior to the antidepressants plus placebos combination in controlling depression and anxiety symptoms after an average of 7 months of intervention, which may be due to the small sample size. However, we found that a greater SCVD increase was associated with greater improvement in depression and anxiety symptoms in VD group, giving indirect support for the view that adjuvant vitamin D supplementation therapy could contribute to better clinical improvement in MDD patients. The underlying biological mechanisms are not completely understood but there are several hypotheses. First, the active form of vitamin D can be produced by the brain and vitamin D receptors are widely distributed across distinct brain systems (e.g. the prefrontal cortex and limbic system) (Eyles et al., Reference Eyles, Smith, Kinobe, Hewison and McGrath2005). Vitamin D in the brain can regulate production of serotonin, which is one of the key neurotransmitters involved in mood regulation (Kesby et al., Reference Kesby, Turner, Alexander, Eyles, McGrath and Burne2017; Patrick & Ames, Reference Patrick and Ames2015). Second, converging evidence indicates that an imbalance between the glutamatergic excitatory and GABAergic inhibitory pathways is implicated in the pathophysiology of MDD (Croarkin, Levinson, & Daskalakis, Reference Croarkin, Levinson and Daskalakis2011; Hasler et al., Reference Hasler, van der Veen, Tumonis, Meyers, Shen and Drevets2007). This imbalance can lead to increased neuronal levels of Ca2+ that may contribute to depression; vitamin D can reduce Ca2+ levels via its function to maintain the expression of the Ca2+ pumps and buffers, which may explain how it acts to ameliorate depressive symptoms (Berridge, Reference Berridge2017). Third, vitamin D may play a neuroimmunological role by regulating the activity and expression of P2X7 receptors, thus preventing the excessive activation of the immune system that is caused by long-term stress, protecting nerve cells, and producing antidepressant effects (Geng et al., Reference Geng, Shaikh, Han, Chen, Guo and Jiang2019).
Multimodal brain imaging data demonstrated that MDD patients, after antidepressants + placebos intervention, showed decreased FA of right IFOF and decreased functional connectivity between rFPN and mVN connected by right IFOF. The present observation of concurrent structural and functional connectivity alterations is consistent with the hypothesis that brain network function is shaped and constrained by underlying structure (Honey, Kotter, Breakspear, & Sporns, Reference Honey, Kotter, Breakspear and Sporns2007; Honey et al., Reference Honey, Sporns, Cammoun, Gigandet, Thiran, Meuli and Hagmann2009). The FPN is responsible for implementing cognitive control and consists of flexible hubs that regulate distributed systems (e.g. visual, limbic, and motor), thereby playing a central role in mental health (Cole, Repovs, & Anticevic, Reference Cole, Repovs and Anticevic2014). The mVN is implicated in detecting and processing visual stimuli. Extensive research has established the presence of abnormal functional connectivity of FPN and mVN in MDD patients (Kaiser, Andrews-Hanna, Wager, & Pizzagalli, Reference Kaiser, Andrews-Hanna, Wager and Pizzagalli2015; Li et al., Reference Li, Lin, Liu, Su, Zhu, Zheng and Sun2020; Luo et al., Reference Luo, Wu, Xu, Chen, Wu, Wang and Wang2021; Yu et al., Reference Yu, Linn, Shinohara, Oathes, Cook, Duprat and Sheline2019; Zhong et al., Reference Zhong, Shi, Ming, Dong, Zhang, Zeng and Yao2017; Zhu et al., Reference Zhu, Yuan, Zhou, Nie, Wang, Hu and Liao2021). The observed brain structural and functional connectivity changes in NVD group may be trait brain abnormalities of MDD, a detrimental consequence of antidepressant medication, or a combination of both. Of note, we did not find such brain changes in VD group, that is, white matter integrity and functional network connectivity were preserved in MDD patients receiving both antidepressant medication and vitamin D supplementation. This finding suggests that adjuvant vitamin D supplementation therapy might have a protective effect on the brain of MDD patients.
There has been increasing recognition of the neuroprotective and neurotrophic actions of vitamin D. FA represents white matter integrity that is related to many factors including axonal count and density, degree of myelination, and fiber organization (Winston, Reference Winston2012). Changes in FA may reflect multiple white matter micro-structural alterations, such as altered axonal density or diameter, abnormal myelination, or altered coherence of fiber tracts. Vitamin D is a potent neuromodulatory compound that can potentiate axon regeneration; in addition, vitamin D could play a protective role by restricting Wallerian degeneration, i.e. degeneration of the distal part to the injury (Chabas et al., Reference Chabas, Alluin, Rao, Garcia, Lavaut, Risso and Feron2008). There is also empirical evidence that vitamin D can enhance neural stem cell proliferation and oligodendrocyte differentiation (Shirazi, Rasouli, Ciric, Rostami, & Zhang, Reference Shirazi, Rasouli, Ciric, Rostami and Zhang2015). Neurotransmitter dysfunction has been suggested to be involved in the pathophysiology of MDD. For instance, past studies have reported reduced histamine H1 receptor binding (Yanai & Tashiro, Reference Yanai and Tashiro2007), reduced GABA levels (Croarkin et al., Reference Croarkin, Levinson and Daskalakis2011), and reduced muscarinic acetylcholine receptor binding (Nikolaus, Hautzel, Heinzel, & Muller, Reference Nikolaus, Hautzel, Heinzel and Muller2012) in the frontal and occipital cortex in MDD patients. It is generally accepted that vitamin D implicates the synthesis, release, and regulation of neurotransmitters (Kesby et al., Reference Kesby, Turner, Alexander, Eyles, McGrath and Burne2017; Patrick & Ames, Reference Patrick and Ames2015). This has led to some speculation that vitamin D supplements help preserve structural and functional connectivity through their beneficial effects on neurotransmitter systems. In addition, depression is associated with elevated biomarkers of inflammation (e.g. cytokines and C-reactive protein), which have been linked to decreased brain connectivity (Felger et al., Reference Felger, Li, Haroon, Woolwine, Jung, Hu and Miller2016). Intense research indicates that vitamin D, a regulator of key components of the immune system, can inhibit abnormal activation of the immune system and thereby has anti-inflammatory activity (Wei & Christakos, Reference Wei and Christakos2015). Despite this growing evidence, the exact mechanisms underlying the neuroprotective effect of vitamin D in MDD are rather complex and need further investigation.
Some limitations of our work should be noted. First, although our small sample size is common for longitudinal neuroimaging studies, it limits the statistical power and the generalizability of our findings. In the future, a larger sample is needed to validate these preliminary findings. Second, most of the MDD patients were antidepressant-medicated and chronic, which may introduce confounds of antidepressant medication and illness duration. Although our results held even after controlling for antidepressant types and illness duration, future studies in drug-naïve first-episode patients with MDD are warranted to further eliminate these confounding factors. Third, the neuroprotective effect of vitamin D in MDD patients is a preliminary finding that needs to be validated in future animal studies. Fourth, it should be noted that patients with anxiety disorders were excluded. Since anxiety is frequently comorbid with MDD, this reduces the generalizability of the findings to the general population with MDD. Fifth, we focused our analysis on static functional network connectivity rather than dynamic connectivity. Since the brain connectome is time-varying and dynamic in ways that are themselves clinically relevant (Luo et al., Reference Luo, Chen, Wang, Li, He, Li and Li2023a; You et al., Reference You, Luo, Yao, Zhao, Li, Wang and Li2022), examination of dynamic functional network connectivity alterations will be part of our future investigations. Finally, we failed to collect more relevant information about participants' lifestyle profiles. Further analysis of these data may facilitate the interpretation of our findings.
In conclusion, our RCT demonstrated that a greater SCVD increase was associated with greater improvement in depression and anxiety symptoms in MDD patients who received a combined intervention of antidepressants and vitamin D. More importantly, multimodal neuroimaging data showed that vitamin D supplementation was able to preserve structural and functional connectivity between the frontal and occipital cortex in MDD patients. Our results suggest that vitamin D supplementation as adjunctive therapy to antidepressants may not only contribute to improvement in clinical symptoms but also have a protective effect on the brain of MDD patients. More broadly, these findings might hold high translational value in informing future MDD intervention in clinical settings.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291724000539.
Data availability statement
Data that support the findings of this study are publicly available in the study's Open Science Framework repository (https://osf.io/j9fc2/).
Acknowledgements
The authors are grateful to study participants for volunteering their time. We greatly appreciate the Chinese psychiatrists and psychologists who have developed the Chinese versions of the HAMD and HAMA.
Funding statement
The study was supported by the STI2030-Major Projects (grant number: 2022ZD0205200), the National Natural Science Foundation of China (grant numbers: 82371928 and 82071905), the Anhui Provincial Natural Science Foundation (grant number: 2308085MH277), the Outstanding Youth Support Project of Anhui Province Universities (grant number: gxyqZD2022026), the Scientific Research Key Project of Anhui Province Universities (grant number: 2022AH051135), the Scientific Research Foundation of Anhui Medical University (grant number: 2022xkj143), the Anhui University Collaborative Innovation Project (grant number: GXXT-2021-065), and the Natural Science Research Project of Anhui Province Universities (grant number: KJ2021ZD0037).
Competing interests
All the authors declare that they have no conflict of interest.









