Introduction
Vocal fold leukoplakia refers to white plaques or patchy lesions on the surface of the vocal folds that are not easily removed. It is a descriptive clinical diagnosis with different pathological manifestations, including inflammatory changes or squamous hyperplasia, dysplasia of different grades, carcinoma in situ, or even carcinogenesis.Reference Park, Altman, Prasad, Broadhurst and Akst1
Vocal fold leukoplakia is a key precancerous lesion observed in laryngeal carcinoma. Weller et al. Reference Weller, Nankivell, McConkey, Paleri and Mehanna2 performed a meta-analysis on the risk for the transformation of laryngeal dysplasia into a malignant laryngeal tumour; they found that the malignant transformation rate of laryngeal dysplasia was 14 per cent, and the mean malignant transformation time was 5.8 years. The malignant transformation rate of mild to moderate dysplasia was 10.6 per cent, and that of severe dysplasia or carcinoma in situ was 30.4 per cent. Therefore, the distinction between benign and malignant vocal fold leukoplakia is of substantial clinical significance, guiding the correct formulation of treatment strategies. Making this distinction can help avoid the excessive treatment of benign lesions, and the misdiagnosis and mistreatment of lesions with high malignant potential.
Vocal fold leukoplakia often causes hoarseness, and patients usually visit a doctor early in the course of the disease. Some studies have shown that narrow-band imaging laryngoscopy and strobolaryngoscopy are helpful for the differential diagnosis of benign and malignant vocal fold leukoplakia.Reference Rzepakowska, Sobol, Sielska-Badurek, Niemczyk and Osuch-Wójcikiewicz3 Nevertheless, white-light imaging laryngoscopy, which allows the observation of morphological characteristics of the vocal fold surface, remains the most common method of examination used for vocal fold leukoplakia diagnosis.
Although some studies have attempted to scoreReference Fang, Lin, Lee, Young, Lee and Chang4 and classifyReference Zhang, Cheng, Chen, Chen, Yang and Xie5 vocal fold leukoplakia using white-light imaging, these studies have limitations and do not include all the morphological characteristics related to malignant transformation. Therefore, there are still deficiencies in the differential diagnosis of benign and malignant vocal fold leukoplakia.
The current study was designed to comprehensively summarise the morphological characteristics associated with malignant leukoplakia, and to propose a new, simple and effective leukoplakia finding score for the diagnosis of vocal fold leukoplakia, in order to improve the accuracy of the preliminary judgement by white-light imaging laryngoscopy before treatment and to provide a basis for correct management.
Materials and methods
Study subjects
Patients with hoarseness as their chief complaint undergoing laryngoscopy at the Department of Endoscopy, Cancer Hospital, Chinese Academy of Medical Sciences, from January 2009 to December 2020, were identified. Those with vocal fold leukoplakia were included in this study; all patients had a definite pathological diagnosis.
The exclusion criteria were as follows: (1) patients with obvious cauliflower or ulcerative masses, polyps, cysts, Reinke's oedema, and papilloma on the surface of the vocal folds; (2) lesions without a definite pathological diagnosis; (3) patients with a history of vocal fold surgery within the last six months; (4) patients with low-quality laryngoscopic images that did not meet the requirements for morphological assessment; and (5) patients with lidocaine allergy, severe uncontrolled dyspnoea, unstable angina, uncontrolled haemorrhagic disease, or an inability to provide informed consent.
This study was approved by the medical ethics committee of the hospital. All patients provided written informed consent prior to examination.
Vocal fold leukoplakia examination
In this study, the Evis Lucera 260 endoscopy system and BF-260 flexible video endoscope by Olympus were used to observe vocal fold leukoplakia. All patients were examined by one experienced laryngologist who did not participate in the subsequent evaluation.
Patients were examined whilst in the supine position. The laryngoscope was inserted through the nasal cavity to observe the nasopharynx, oropharynx, hypopharynx and larynx. When vocal fold leukoplakia was identified, the laryngeal mucosa was sprayed with 2 per cent lidocaine for surface anaesthesia. Representative images were collected before biopsy of the vocal fold leukoplakia. The biopsy specimens were preserved in 10 per cent formalin and submitted for pathological examination.
Image analysis
The laryngoscopic images of vocal fold leukoplakia were independently evaluated by two experienced laryngologists who were not informed of the pathological diagnosis or other clinically relevant information. The two laryngologists recorded the characteristics of the vocal fold leukoplakia by laryngoscopy, including size, thickness, texture, hyperaemia, boundary, and whether the anterior commissure and bilateral vocal folds were involved. Their consensus was used as the final diagnosis result.
The characteristics of vocal fold leukoplakia were defined as follows: (1) size – unilateral vocal fold leukoplakia covering more than half of the total area of the vocal fold was defined as large leukoplakia; otherwise, the definition was small leukoplakia; (2) thickness – leukoplakia was considered thick if obviously exceeding the height of the vocal fold surface and the blood vessels beneath the lesion were not visible; otherwise, it was considered thin; (3) texture – leukoplakia with a rough and uneven surface, which may manifest as papillary, verrucous, granular or scattered nodules, was defined as irregular; if the surface of the lesion was flat and smooth, and the thickness of each part was almost equal, it was judged to be regular; (4) hyperaemia – mucosal erythema or dilated blood vessels seen on or around the leukoplakia were considered hyperaemia; (5) boundary – if the boundary between the lesion and the surrounding normal mucosa was clear, neat and sharp, the lesion boundary was considered clear; if the boundary was disordered, fuzzy and rough, the lesion boundary was deemed unclear; (6) anterior commissure involvement was determined; (7) bilateral vocal fold involvement was ascertained; and (8) the vocal fold leukoplakia underwent general classification using a laryngoscope, as proposed by Zhang et al. Reference Zhang, Cheng, Chen, Chen, Yang and Xie5
According to the Zhang et al. Reference Zhang, Cheng, Chen, Chen, Yang and Xie5 classification system, vocal fold leukoplakia was categorised as: (1) flat and smooth type (localised white plaque lesion with a uniform thin, smooth homogeneous surface, or a slightly raised white patch with an edge continuous with the surrounding mucosa); (2) bulge and smooth type (white patches obviously higher than the mucosal surface, with edges discontinuous with the surrounding mucosa, but the thickened white patches are homogeneous and smooth); and (3) bulge and rough type (rough leukoplakia that is uneven or nodular, verrucous, papillary or granular).
Pathological classification
The pathological results obtained after biopsy or surgery are the ‘gold standard’ for the final diagnosis of vocal fold leukoplakia. According to the World Health Organization classification criteria (2005),Reference Gale, Pilch, Sidransky, Naggar, Westra, Califano, Barnes, Eveson, Reichart and Sidransky6 vocal fold leukoplakia is classified into benign and malignant types. Benign leukoplakia includes inflammation, simple hyperplasia, mild dysplasia and moderate dysplasia. Malignant leukoplakia includes severe dysplasia, carcinoma in situ and invasive carcinoma.
Statistical analysis
The statistical software SPSS version 20.0 was employed for statistical analyses. The chi-square test was utilised for univariate analysis. Multivariate logistic regression analysis was used for multivariate analysis. Based on the results of the univariate and multivariate analyses, characteristics with statistically significant differences were compiled to establish the leukoplakia finding score system. The best critical score was determined in combination with the receiver operating characteristic curve and clinical practice. The kappa statistic was calculated to evaluate the reading consistency between the two laryngologists (kappa < 0.2 indicates poor consistency; kappa = 0.2–0.4, fair consistency; kappa = 0.4–0.6, moderate consistency; kappa = 0.6–0.8, relatively strong consistency; and kappa = 0.8–1.0, very strong consistency). Differences were considered statistically significant at p < 0.05.
Results
Clinical and pathological characteristics
Of the 163 patients with vocal fold leukoplakia included in this study, 158 (96.9 per cent) were male and 5 (3.1 per cent) were female, and the median age was 59 years (range, 26–86 years). There were 126 cases of unilateral onset of vocal fold leukoplakia and 37 cases of bilateral onset, totalling 200 lateral lesions. Among the 200 lateral lesions (Table 1), there were 152 (76.0 per cent) cases of benign leukoplakia and 48 (24.0 per cent) cases of malignant leukoplakia (Table 1).
Benign and malignant laryngoscopic differences
Vocal fold leukoplakia was examined by laryngoscopy to assess the differences in the morphological characteristics between its benign and malignant presentation. The univariate analysis showed significant differences between benign and malignant vocal fold leukoplakia in terms of size, thickness, texture, hyperaemia, anterior commissure involvement and Zhang classification (p < 0.05). The results of the multivariate regression analysis showed that thickness, hyperaemia and anterior commissure involvement were independent risk factors for malignancy (p < 0.05) (Table 2).
Table 2. Comparison of laryngoscopic characteristics between benign and malignant vocal fold leukoplakia

OR = odds ratio; CI = confidence interval
Leukoplakia finding score system
This section concerns the establishment of the leukoplakia finding score system based on laryngoscopic characteristics, with comparison with other methods. According to the regression analysis, the effect of hyperaemia was most obvious (odds ratio = 38.278), followed by the involvement of the anterior commissure (odds ratio = 5.314) and the presence of thick leukoplakia (odds ratio = 4.556).
We established a vocal fold leukoplakia finding score system (Table 3) with a possible range of 0–10 points. In order to facilitate calculation (and for ease of memorability of scoring), according to the regression co-efficients, 4 points were assigned for hyperaemia, 2 points for anterior commissure involvement, 2 points for thickness, 1 point for size and 1 point for texture, whereby more points correlate with malignant (as opposed to benign) leukoplakia.
Table 3. Vocal fold leukoplakia finding score based on laryngoscopic characteristics

The total scores of the benign and malignant vocal fold leukoplakia groups were calculated according to the above scoring system, and the receiver operating characteristic curve was generated. The area under the receiver operating characteristic curve for the diagnosis of benign and malignant vocal fold leukoplakia by the scoring system was 0.946 (95 per cent confidence interval (CI) = 0.916–0.976, p < 0.0001). According to the calculation formula (score = 0.060 × age + 2.609 × texture + 1.307 × hyperaemia) for assessing benign and malignant vocal fold leukoplakia reported by Fang et al.,Reference Fang, Lin, Lee, Young, Lee and Chang4 the area under the curve was 0.880 (95 per cent CI = 0.821–0.939, p < 0.0001). The area under the curve according to the classification of leukoplakia reported by Zhang et al.Reference Zhang, Cheng, Chen, Chen, Yang and Xie5 was 0.742 (95 per cent CI = 0.664–0.820, p = 0.0001). Hence, the area under the curve of the leukoplakia finding score was significantly better than that of the Fang score (p = 0.0143) and Zhang classification (p < 0.0001) (Figure 1).

Figure 1. Receiver operating characteristic curve of laryngoscopic characteristics in the diagnosis of vocal fold leukoplakia. LFS = leukoplakia finding scores
Diagnostic efficiency of scoring system
Five indicators were included in the leukoplakia finding score system designed in this study. The total scores assigned to the 200 vocal fold leukoplakia cases included in this study were within the range of 0–10 points. The Youden index of all scores was calculated according to the sensitivity and specificity of each cut-off score determined by the receiver operating characteristic curve, and the maximum Youden index (score of ≥6 points) was taken as the reference cut-off value (Table 4). The lesion tended to be malignant when the score was 6 or more points, while the lesion tended to be benign when the score was less than 6 points (Figure 2). A cut-off value of 6 points or more was most efficient for the diagnosis of benign and malignant vocal fold leukoplakia. The sensitivity, specificity, positive predictive value, negative predictive value and accuracy rates were 93.8 per cent, 83.6 per cent, 64.3 per cent, 97.7 per cent and 86.0 per cent, respectively.
Table 4. Diagnostic efficacy of different leukoplakia finding scores
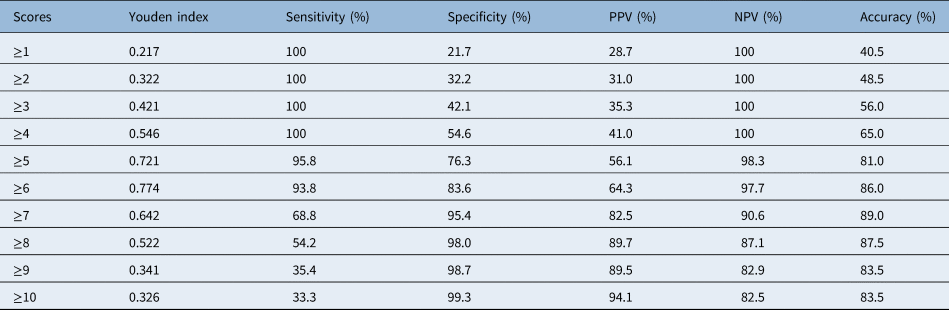
PPV = positive predictive value; NPV = negative predictive value

Figure 2. Diagnostic efficiency of the leukoplakia finding score system based on laryngoscopic characteristics. (a–c) Benign leukoplakia; (d–f) malignant leukoplakia. (a) Leukoplakia finding score = no erythema (0 points) + anterior commissure no invasion (0 points) + thick leukoplakia (2 points) + large size (1 points) + irregular texture (1 point) = 4 points; the pathological diagnosis is mild dysplasia. (b) Leukoplakia finding score = no erythema (0 points) + anterior commissure invasion (2 points) + thick leukoplakia (2 points) + large size (1 point) + regular texture (0 points) = 5 points; the pathological diagnosis is simple hyperplasia. (c) Leukoplakia finding score = no erythema (0 points) + anterior commissure no invasion (0 points) + thick leukoplakia (2 points) + large size (1 point) + irregular texture (1 point) = 4 points; the pathological diagnosis is mild dysplasia. (d) Leukoplakia finding score = erythema (4 points) + anterior commissure invasion (2 points) + thick leukoplakia (2 points) + large size (1 point) + irregular texture (1 point) = 10 points; the pathological diagnosis is squamous cell carcinoma. (e) Leukoplakia finding score = erythema (4 points) + anterior commissure no invasion (0 points) + thick leukoplakia (2 points) + large size (1 point) + regular texture (0 points) = 7 points; the pathological diagnosis is carcinoma in situ. (f) Leukoplakia finding score = erythema (4 points) + anterior commissure invasion (2 points) + thick leukoplakia (2 points) + small size (0 points) + irregular texture (1 point) = 9 points; the pathological diagnosis is squamous cell carcinoma.
Consistent analysis of scores
Table 5 shows the independent leukoplakia finding score results of the two laryngologists for the 200 vocal fold leukoplakia cases. The kappa co-efficient value between their scores was 0.809, showing very strong consistency (Figure 3).
Table 5. Leukoplakia finding scores of 200 vocal fold leukoplakia cases assigned by two doctors

LFS = leukoplakia finding scores

Figure 3. Consistency analysis of leukoplakia finding score (LFS) between two laryngologists.
Discussion
The incidence of vocal fold leukoplakia is mostly correlated with long-term chronic stimulation of laryngeal mucosa, such as that resulting from smoking, drinking alcohol and laryngopharyngeal reflux. Leukoplakia is a common precancerous lesion that is most likely to progress to glottic cancer.Reference Ali, Smith and Hogikyan7 Laryngoscopy is the main means to diagnose vocal fold leukoplakia. Exploring the relationship between the appearance of vocal fold leukoplakia and the degree of vocal fold leukoplakia dysplasia observed by laryngoscopy is key to determining treatment strategies, prognosis and follow-up approaches. The accurate diagnosis of potentially malignant vocal fold leukoplakia is closely related to laryngologists’ clinical experience.
We have previously reported that narrow-band imaging laryngoscopy helps to improve the accuracy of the diagnosis of benign and malignant vocal fold leukoplakia, by aiding observation of the morphology of microvessels on the mucosal surface.Reference Ni, Zhu, Zhang, Zhang and Wang8 However, as the narrow-band imaging laryngoscopy has not been fully popularised clinically, mastering its use and making accurate judgements of observations require training.Reference Ni, Wang, Hu, Xu, Xu and Liu9 Most laryngologists observe vocal fold leukoplakia by white-light imaging laryngoscopy. Therefore, it is of greater clinical significance to improve the diagnostic accuracy of vocal fold leukoplakia under white-light imaging laryngoscopy, which is worthy of further study.
Although the gross appearance of vocal fold leukoplakia with different pathological properties is sometimes approximately similar, some researchers have tried to use white-light imaging laryngoscopy for the scoring and classification of vocal fold leukoplakia, to evaluate the possibility of malignancy and guide treatment. Representative scoring systems are the leukoplakia scoring system proposed by Fang et al. Reference Fang, Lin, Lee, Young, Lee and Chang4 and the classification proposed by Zhang et al. Reference Zhang, Cheng, Chen, Chen, Yang and Xie5
Fang et al.Reference Fang, Lin, Lee, Young, Lee and Chang4 observed the colour, texture, size, hyperaemia, thickness and symmetry of vocal fold leukoplakia under laryngoscopy. The regression analysis showed that age, lesion heterogeneity and hyperaemia were independent factors for predicting malignant vocal fold leukoplakia. The formula for the diagnosis of vocal fold leukoplakia (score = 0.060 × age + 2.609 × texture + 1.307 × hyperaemia) was proposed on the basis of the regression co-efficient. This score has some clinical value for predicting the malignancy of vocal fold leukoplakia (area under the curve = 0.86).
Zhang et al.Reference Zhang, Cheng, Chen, Chen, Yang and Xie5 classified vocal fold leukoplakia into three types according to roughness: type I is flat and smooth, type II is bulged and smooth, and type III is bulged and rough. Further studies by this team showed that the classification of vocal fold leukoplakia into low-risk and high-risk groups has a certain auxiliary effect (area under the curve = 0.863) and helps to guide the choice of clinical treatment.Reference Li, Zhang, Wang, Cheng, Wu and Chen10,Reference Chen, Li, Yang, Cheng and Wu11 In this classification system, type I mostly suggests low-risk leukoplakia, whereas type III mainly suggests high-risk vocal fold leukoplakia. However, the differential diagnosis of type II leukoplakia is not accurate, mainly because this classification was only based on texture, and ignored other factors, especially hyperaemia, which is an important potential malignant indicator. Some studies have shown that under white-light imaging laryngoscopy, the existence of hyperaemiaReference Young, Lin, Lee, Lee, Hsin and Liao12 and vascular stipplingReference Anis13 are closely related to atypical hyperplasia and malignancy. Although Fang's scoring system considered texture and hyperaemia, it is not widely applied in clinical practice. The main reason is that the formula of this scoring method is difficult to remember; in addition, there is a lack of consideration of other factors associated with malignant vocal fold leukoplakia (such as colour, size and symmetry), which leads to an average diagnostic efficiency (sensitivity of 80.4 per cent and specificity of 81.5 per cent).
In order to improve the accuracy and objectivity of vocal fold leukoplakia evaluations performed by laryngoscopy, all morphological factors associated with benign and malignant leukoplakia were included in this study, by referring to the grading method of reflux finding score in the diagnosis of laryngopharyngeal reflux.Reference Belafsky, Postma and Koufman14 Scores were assigned according to the regression co-efficients. The regression analysis showed that hyperaemia was the most important factor. For easy memorisation, 4 points were assigned for hyperaemia, 2 points each for anterior commissure involvement and thickness, and 1 point each for size and texture. The final range of the score was 0–10 points. This scoring system showed a very strong consistency between two laryngologists (kappa = 0.809). The area under the curve for this leukoplakia finding score in terms of the diagnosis of benign and malignant vocal fold leukoplakia was 0.946, which was higher than that of the Fang score (area under the curve = 0.880) and Zhang classification (area under the curve = 0.742). The reference cut-off score for diagnosing malignant vocal fold leukoplakia was 6 points or more. The sensitivity, specificity and accuracy values of this scoring method were 93.8 per cent, 83.6 per cent and 86.0 per cent, respectively.
• Morphology of vocal fold leukoplakia under conventional laryngoscopy corresponds with pathological properties to some degree
• Five indicators (size, thickness, texture, hyperaemia and anterior commissure involvement) are associated with malignant vocal fold leukoplakia
• Leukoplakia finding score based on laryngoscopic features is helpful for differential diagnosis of benign and malignant vocal fold leukoplakia
In this study, hyperaemia of vocal fold leukoplakia is the most important predictor of malignancy (it has a maximum weight of 4 points in the scoring system); thus, this feature should be a focus of evaluation during laryngoscopy. This characteristic on white-light imaging laryngoscopy, which corresponds to narrow-band imaging laryngoscopy, is observed as tortuous dilated microvessels, and is the main observation point of narrow-band imaging laryngoscopy used to assess the nature of these lesions.Reference Ni, He, Xu, Gao, Lu and Yuan15,Reference Li, Yu, Zhu, Wang, Li and Yang16 In order to accurately assess whether vocal fold leukoplakia is hyperaemic, it is critical to observe the vocal fold surface as closely as possible during laryngoscopy and to pay attention to the edge of the leukoplakia. In addition, anterior commissure involvement is closely related to the malignant transformation of vocal fold leukoplakia (assignment of 2 points in our scoring system), which has not been reported in other studies but is consistent with the aggressiveness of the tumours. The relationship between vocal fold leukoplakia and the anterior commissure can provide accurate clinical information for subsequent minimally invasive surgical treatment.
Conclusion
The differential diagnosis of benign and malignant vocal fold leukoplakia is challenging for laryngologists. The morphology of vocal fold leukoplakia observed under conventional laryngoscopy corresponds with its pathological properties to some degree, but the subjective factors are strong, and there is no clear objective standard.
The establishment of this scoring method was based on the comprehensive consideration of the factors associated with the cancerous transformation of vocal fold leukoplakia. This scoring system was simplified for easy memorisation and is based on objective scoring during clinical laryngoscopy. Hence, vocal fold leukoplakia pathological properties can be evaluated using this scoring system without biopsy, avoiding unnecessary invasive injury and helping to protect vocal fold function. However, whether this scoring system can be well applied clinically needs to be further verified by a multicentre clinical study.
Acknowledgements
This work was financially supported by: the Chinese Academy of Medical Sciences (‘CAMS’) Innovation Fund for Medical Sciences (‘CIFMS’) (grant number: 2022-I2M-C&T-B-059), Beijing Hope Run Special Fund of Cancer Foundation of China (grant number: LC2021A04) and Sanming Project of Medicine in Shenzhen (grant number: SZSM201911008).
Competing interests
None declared











