Increasing the number of doctors choosing to enter and remain in psychiatry has been a key health policy priority in the UK over the past 3 years.1,2
The proportion of graduates from each medical school entering immediately into psychiatry post-foundation training varies widely, from 0.1 to 0.4%.3 Overall, approximately 5% of foundation year 2 (F2) doctors who enter directly into specialty training are appointed to core psychiatry training each year.3,4 However, increasingly large numbers of junior doctors are delaying their progression into specialty training, for multiple complex reasons.3,4 Although recruitment to core training has improved more recently, almost 10% of core and consultant posts still remained unfilled in 2019.5,6
Recruiting and retaining sufficient doctors to fill these gaps requires multifaceted, long-term approaches. As well as increasing the number of doctors entering medical school, policy has recently focused on improving the exposure and experience of psychiatry training at undergraduate level.7 Prior research has demonstrated that regular early undergraduate exposure to psychiatry (through the Psychiatry Early Experience Programme, PEEP) can sustain positive attitudes towards psychiatry and challenge preconceptions about the specialty.Reference Holt, Mirvis, Bao, Cross, Hussain and Hutchings8 However, little is known about the value of mentorship for medical students interested in psychiatry, despite this demonstrating clear value for students and doctors in other specialties and the broader literature.Reference Ramanan, Phillips, Davis, Silen and Reede9–Reference Frei, Stamm and Buddeberg-Fischer12
This paper describes and evaluates the establishment of an undergraduate enrichment programme that combines opportunities for mentorship with additional clinical exposure to psychiatry. To our knowledge, this is the first paper to explore the potential role of undergraduate mentorship in improving recruitment to the profession. We also evaluate the potential utility of mentoring for supporting, and promoting the development of, the future psychiatric workforce.
Method
PsychStart, a career-based mentoring scheme for medical students interested in psychiatry, was co-founded by two of the authors (T.H. and N.T.) at the University of Nottingham in January 2018.
Medical students from all year groups were recruited to the scheme via communication through the student-led psychiatry society Mind Matters, social media advertising (Facebook and Twitter) and signposting during lectures and psychiatry teaching.
There are approximately 280 students in undergraduate years 1 and 2 of the Nottingham medical course, and 100 students in graduate-entry years 1 and 2. The undergraduate and graduate students merge during year 3, with approximately 380 students in years 3–5 of the medical programme. The psychiatry module is taught in year 4, and approximately 45 students complete this module at any one time.
Mentors were recruited from three local healthcare trusts that provide clinical psychiatry placements, as well as from the University of Nottingham and the university's Institute of Mental Health, facilitating the involvement of both academic and clinical psychiatrists. Mentor recruitment was limited to registrars (specialty trainee year 4 and above, ST4+) and consultant psychiatrists across a wide range of psychiatric subspecialties.
Places on the scheme were allocated on a first-come-first-served basis when appropriate mentors became available. Medical students were matched 1:1 or 2:1 to registrar or consultant psychiatrist mentors according to three main criteria: subspecialty interests, geographical location of mentors’ workplaces and students’ placements locations, and other career interests (e.g. in research, management or education).
All mentors and mentees were invited to attend a 2 h training session, with scheduled time incorporated for the initial ‘meet and greet’ between mentors and mentees. The mentor training was led by a consultant psychiatrist with experience of medical education and the Nottingham psychiatry module (N.T.), with input from the Director of Student Wellbeing. Mentor training topics covered the role of a mentor, theories of mentoring, characteristics of positive and negative mentorship, the structure and scope of the PsychStart scheme, the context of psychiatry at Nottingham medical school, and student welfare and support. Mentee training was coordinated by a junior doctor (T.H.) and/or the President of the student-led PsychStart committee, with oversight from a consultant psychiatrist (N.T.). Mentee training topics included the role of a mentee, characteristics of positive and negative mentoring interactions, the structure and scope of the PsychStart scheme, and career pathways and opportunities in psychiatry.
No minimum or maximum restrictions were placed on the frequency of mentor–mentee contact, but monthly email contact was recommended initially to promote engagement.
A generic email account was created for general communication and administrative queries. A separate email account monitored by a consultant psychiatrist (N.T.) was used for communication of any mentoring difficulties or issues requiring senior input.
Regular surveys were distributed to mentees to evaluate the different mentoring relationships and identify any requiring extra support. Any failing or inactive mentoring relationships, as identified by survey data and communication with the scheme's co-founders, were discussed with the concerned mentors and mentees. Where appropriate, some mentoring relationships were subject to reallocation.
To celebrate successes on the scheme and support the network, annual awards evenings were established where mentoring achievements were formally recognised. Awards were selected using information from regular feedback surveys, and mentors and mentees were also given the opportunity to submit nominations.
The data presented in this paper are from the 12- and 18-month evaluation surveys in January and June 2019 (Appendix 1 in the supplementary material, available at https://doi.org/10.1192/bjb.2020.107) and other feedback, including nominations for the annual scheme awards. All participants gave informed consent for their anonymised data to be included in future research and promotional materials. As this was a service evaluation to help improve a novel mentoring scheme, ethical approval was not required.
Results
In mid-2020, there are currently 66 active mentoring relationships participating in the PsychStart scheme at Nottingham University. Of these, 36 are 1:1; the remaining 30 students are matched 2:1 to mentors. There are also 20 medical students on the reserve list awaiting mentor allocation.
Mentee demographics
Of the current mentees, in mid-2020, 50 (75.8%) are women and 16 (24.2%) are men. Just under half (29; 43.9%) are in the pre-clinical phase of the medical course, with the rest in years 3 and above (37; 56.1%) (Table 1). The scheme is most popular among fourth year students (14; 21.2%) (Table 1).
Table 1 Year groups of medical students on the PsychStart scheme across the East Midlands in mid-2020
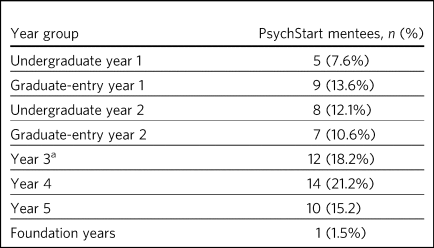
a. The graduate-entry medicine (GEM) students merge with the undergraduate students from year 3 onwards.
Psychiatric subspecialties
In mid-2020, there are 51 registrar and consultant psychiatrists participating in the PsychStart scheme across the East Midlands. The mentors span a range of specialties, from forensic to perinatal psychiatry, with most mentors in general adult and child and adolescent mental health services (Fig. 1).
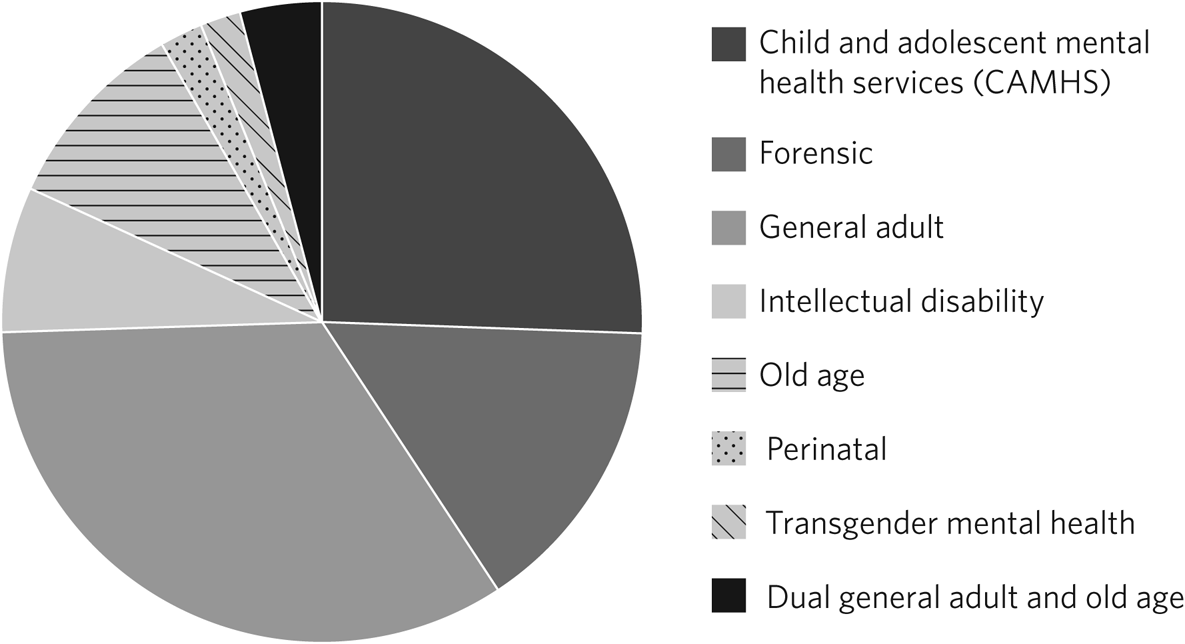
Fig. 1 Specialty distribution of mentors on the PsychStart scheme across the East Midlands in mid-2020.
Survey responses
We received responses from 31 out of 44 mentees (70.5%) in the 18-month survey and 47 out of 68 (69.1%) in the 1-year survey, creating a cumulative total of 78 responses from 68 mentees; 18 students completed both surveys.
Most students had participated in the PsychStart scheme for over a year at the time of survey completion (46; 59.0%); 14 students (17.9%) had participated in the scheme for 6–12 months; and 18 (23.1%) for less than 6 months.
Subjective ratings of scheme experiences and mentoring relationships
Including all 78 survey responses, over 90% of students described their overall scheme experience as ‘good’ or ‘excellent’ (Table 2). The organisation of, and support available on, the PsychStart scheme were also rated as ‘good’ or ‘excellent’ by 93.6 and 89.8% of mentees respectively, with no student rating these as ‘poor’ or ‘very poor’ (Table 2).
Table 2 Subjective mentee ratings of their experiences on the PsychStart scheme
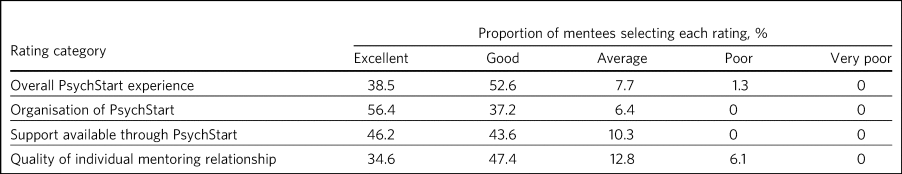
Over 80% of students subjectively rated the quality of their mentoring relationships as ‘good’ or ‘excellent’ (Table 2). Only 6.1% of students reported poor mentoring relationships (Table 2).
Over 80% of mentees ‘agreed’ (48.2%) or ‘strongly agreed’ (35.7%) that they had been well-matched to their mentors; 14.3% of responses were neutral and 1.8% disagreed.
Frequency of mentee–mentor contact
Two-thirds of survey responses indicated a frequency of mentee–mentor contact of every 3 months or more often (52; 66.7%), of which just under a quarter (18; 23.1%) reported monthly contact with mentors (Fig. 2). Over 80% (66; 84.6%) were in contact with their mentors every 6 months or more often (Fig. 2).
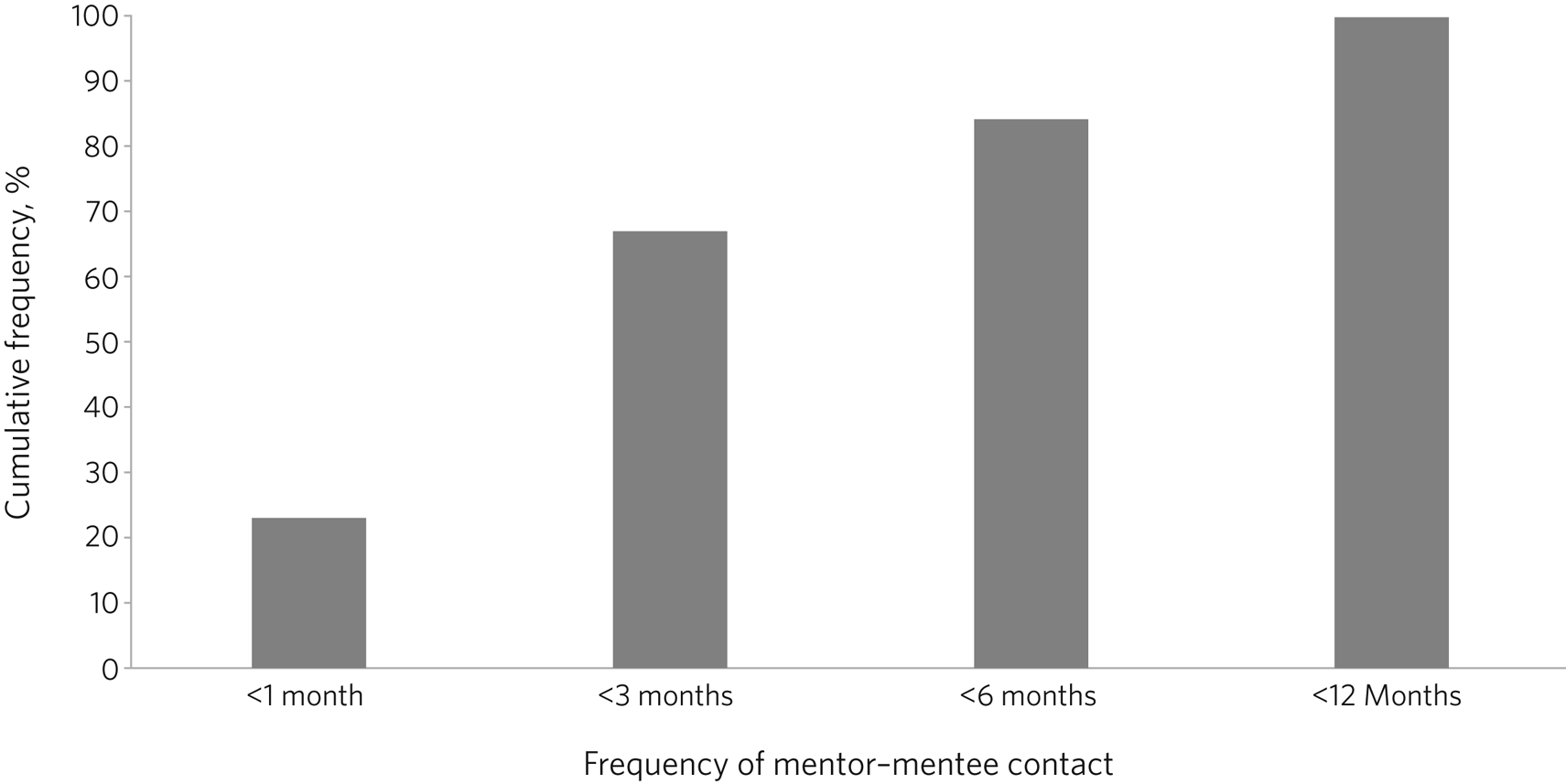
Fig. 2 Frequency of mentor contact reported by mentees on the PsychStart scheme.
Mentoring activities
Students reported a range of mentoring activities on the PsychStart scheme. The most popular activities were receiving careers or medical school advice, engaging in clinical shadowing, discussing psychiatry topics with mentors and being signposted to opportunities in the specialty (Fig. 3). Some students reported attending events, such as conferences, with their mentors, arranging clinical psychiatry electives, and engaging in audit or quality improvement projects and research (Fig. 3).
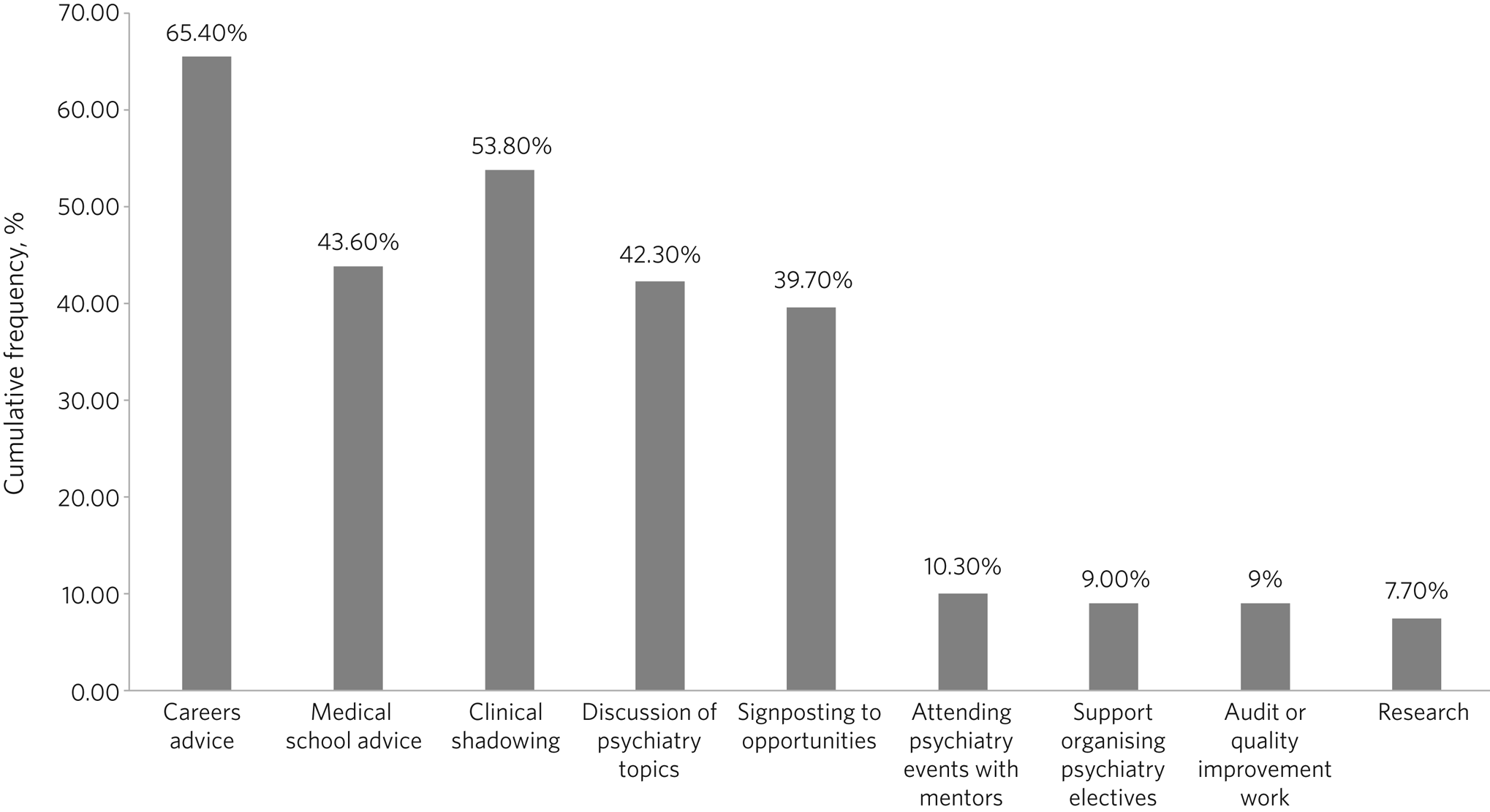
Fig. 3 Frequency of mentoring activities reported by mentees on the PsychStart scheme.
Effects of mentoring and the PsychStart scheme
A majority of mentees reported improved personal (71.4%) and professional (75%) development, clinical knowledge about psychiatry (60%) and knowledge about careers in the specialty (83.6%) (Table 3).
Table 3 Reported effects of the PsychStart mentoring scheme
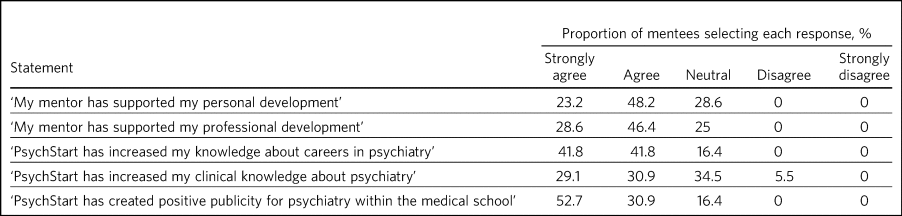
Over 80% of mentees felt that PsychStart had created positive publicity for psychiatry within the medical school, with over half of students strongly agreeing with this statement (Table 3).
Potential links to recruitment
Approximately one-third of mentee responses (21; 32.3%) reported that PsychStart had increased their interest in psychiatry as a career. All but one of the remaining responses (43; 66.2%) reported that PsychStart had maintained their interest in a career in the specialty.
The one mentee who reported that PsychStart had decreased their interest in psychiatry as a career rated their overall scheme experience as excellent. On further clarification, this mentee had been deciding between careers in general practice and psychiatry, and through further experiences of both specialties had decided to pursue primary care. They claimed that PsychStart had helped them to make an ‘informed decision’ and that they were hoping to complete a foundation post in psychiatry.
Qualitative feedback
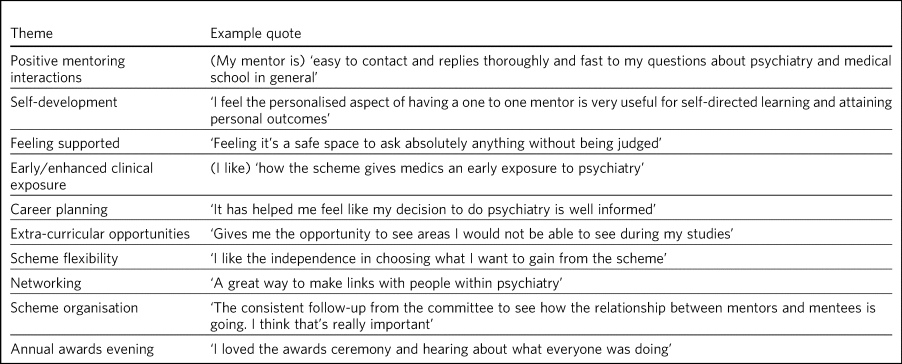
In total, 57 participants provided comments on their favourite aspects of the PsychStart scheme, from which 10 key themes were identified (Table 4). Most commonly, respondents cited their individual mentoring interactions and relationships as their favourite scheme component.
Table 4 Major themes identified from qualitative analysis of mentees’ reported favourite aspects of the PsychStart scheme
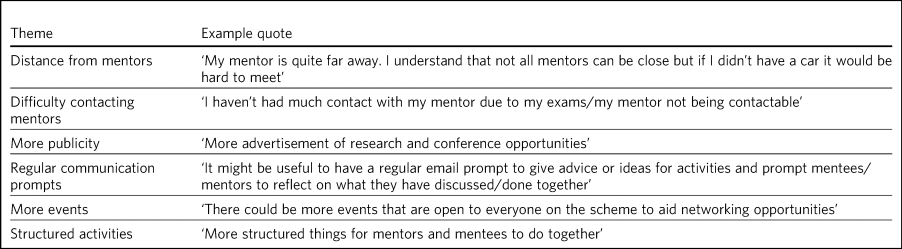
Six key themes were identified from the answers of 39 respondents who offered suggestions for scheme improvement (Table 5). The most popular suggestions included greater provision of locally available mentors, more scheme publicity/advertisement and more communication prompts to mentors/mentees.
Table 5 Major themes identified from qualitative analysis of mentees’ suggested areas of improvement for the PsychStart scheme
Leaving the scheme
In total, 40 mentees have left the scheme since it began, most commonly because they graduated medical school or moved location (22; 55%). Other reasons have included other commitments 3 (7.5%), wanting to explore other specialties (2; 5%) and taking a year out of medical school (1; 2.5%); 7 mentees (17.5%) left the scheme without any specific reason and 5 (12.5%) left because of poor engagement.
Of the mentors, 9 have left the scheme since its inception for various reasons: moving geographical location (3; 33.3%), other commitments (3; 33.3%), difficulty meeting their mentees owing to travel distance (2; 22.2%) and retirement (1; 11.1%).
Discussion
The General Medical Council (GMC) mandates that all medical students must have access to educational and pastoral support and career guidance.13 Medical schools provide extensive educational networks for students to support academic progress, career development and well-being.
In the medical literature, the most frequently cited definition of mentoring is that provided by the Standing Committee on Postgraduate Medical and Dental Education (SCOPME), who describe it as: ‘A process whereby an experienced, highly regarded, empathetic person (the mentor) guides another (usually younger) individual (the mentee) in the development and re-examination of their own ideas, learning, and personal and professional development’.14 The role of a mentor is sometimes confused, and occasionally overlaps, with that of several others, including a tutor, supervisor, counsellor, advisor and role model.Reference Ramanan, Phillips, Davis, Silen and Reede15–Reference Healy, Cantillon, Malone and Kerin17 The main distinctions are the highly personal and active nature of the mentoring interaction and the focus on the individual mentee's personal and career goals, instead of professional skills.Reference Ramanan, Phillips, Davis, Silen and Reede15–Reference Coates, Crooks, Slavin, Guiton and Wilkerson18
Over 90% of medical students perceive mentoring to be important and are keen to engage in mentoring relationships.Reference Aagaard and Hauer19,Reference Gail, Rukstalis and Schuckit20 Despite this, only one-third of medical students report having a mentor.Reference Aagaard and Hauer19,Reference Gail, Rukstalis and Schuckit20 Furthermore, there is a lack of mentoring schemes in most countries’ medical schools, including the UK.Reference Frei, Stamm and Buddeberg-Fischer21,Reference Buddeberg-Fischer and Herta22 This lack is surprising given the evidenced widespread benefits,Reference Ramanan, Phillips, Davis, Silen and Reede15,Reference Frei, Stamm and Buddeberg-Fischer21 although it could be argued that there has been uneven support and guidance for potential mentors to enable them to adopt such roles.Reference Gonçalves and Bellodi23
Mentors provide strong role modelling for careers and can have a significant impact on specialty choice.Reference Frei, Stamm and Buddeberg-Fischer21,Reference Steele, Fisman and Davidson24 In a study including over 9000 medical students, mentors and role models were identified as the most or second-most influential factor in determining specialty selection; for ‘controllable lifestyle’ specialties, of which psychiatry was included, their influence was exceeded only by ‘lifestyle factors’.Reference Boyd, Clyne, Reinert and Zink25
Potential student gains from PsychStart
Our project has demonstrated that a mentoring scheme for medical students interested in psychiatry can be delivered alongside the standard curriculum and is popular among students at a large UK medical school. Participants reported several benefits from mentoring, including enhanced personal and professional development, improved careers and clinical knowledge, and feeling well supported. These benefits could apply to all students and to mentoring in other specialties, with the broader literature demonstrating similar benefits from other mentoring schemes.Reference Frei, Stamm and Buddeberg-Fischer21
It is interesting that many of the qualitative comments by students highlighted generic aspects of the mentoring relationship, such as receiving personalised support, careers advice and assistance in their personal and professional development, as their favourite components of the PsychStart scheme. All students already have a personal tutor throughout the medical course, and clinical supervisors for each placement, who are also able to deliver these functions. It may be that students particularly enjoy receiving such support in the context of their desired specialty or accessing this from somebody to whom they have been closely matched on the basis of shared interests.
Many of the observed mentoring activities fulfil several selection criteria for core psychiatry training applications.32 For example, involvement in audit and quality improvement, completion of research, and demonstration of commitment to the specialty through arranging further clinical exposure and clinical electives with mentors. Hence, mentoring opportunities may increase employability and help students to maximise their chances of successful future training applications. This is likely to be an important attraction to the scheme as recruitment to core training becomes more competitive.
Potential specialty gains from PsychStart
Mentoring may also facilitate increased and broadened clinical exposure to a specialty, with many students arranging shadowing opportunities with their mentors and accessing subspecialties that are less established within the standard curriculum. This is particularly useful within psychiatry, where many subspecialties, such as forensic and perinatal psychiatry, are optional or seldom taught in medical school. The Psychiatry Early Experience Programme (PEEP) has previously demonstrated the benefits of increased psychiatry exposure for young medical students, including sustained positive attitudes towards the specialty.Reference Holt, Mirvis, Bao, Cross, Hussain and Hutchings8 It is unclear whether such positive attitudes extend beyond those students who engage in psychiatry enrichment programmes, but over 80% of mentees felt that PsychStart had created positive publicity for the specialty within the wider medical school, suggesting that these may permeate throughout the student body. Ajaz et al previously reported that medical students often experience ‘badmouthing’ or ‘bashing’ of psychiatry,Reference Ajaz, David, Brown, Smuk and Korszun26 which can deter them from entering the specialty; this highlights the importance of fostering positive attitudes and prompted the Ban the Bash campaign by the RCPsych, which aimed to identify and discourage disparaging comments about psychiatry.27 More recently, the College has focused on emphasising positive ‘pull factors’ that promote selection of psychiatric careers.
The most common year for students to sign up to PsychStart is year 4, which coincides with the clinical psychiatry module; hence, clinical exposure to a specialty may prompt involvement in extra-curricular opportunities. The mentoring scheme was much more popular among women students, with 75.8% of mentees being women. This is considerably larger than the approximately 55% women on the Nottingham medical course (This information was obtained by T.H. through contact with Dr Pamela Hagan at the University of Nottingham Medical School. Permission was granted from the University of Nottingham Dean of Medical Education Professor Gill Doody). It is not clear why this discrepancy exists. Prior research has associated female gender with preferential selection of psychiatry at undergraduate level;Reference Farooq, Lydall, Malik, Ndetei and Bhugra28 however, women have historically been less likely to receive mentorship, and to become mentors, in medical fields.Reference Butkus, Serchen, Moyer, Bornstein and Hingle29,Reference Osborn, Ernster and Martin30
Our scheme data provide further evidence to support the utility of mentoring in improving specialty recruitment, with over one-third of students reporting an increased interest in psychiatric careers. Our data also suggest that mentoring may help to retain, as well as promote, students’ interests in particular specialties, with just under two-thirds of students reporting a sustained interest in psychiatry on the PsychStart scheme. This is particularly important given that 22% of medical students who exhibit an early interest in psychiatry lose this interest throughout their studies.Reference Farooq, Lydall, Malik, Ndetei and Bhugra28 There is evidence that these benefits also exist outside of psychiatry; for example, Dorrance et al reported that a mentoring and research initiative showcasing a career as an internist in primary care settings resulted in a higher proportion of graduates opting for internal medicine training.Reference Dorrance, Denton, Proemba, La Rochelle, Nasir and Argyros31 Furthermore, mentoring has been found to increase interest in academic careers.Reference Sambunjak, Straus and Marsuic10,Reference Frei, Stamm and Buddeberg-Fischer21 Holt et al reported no significant difference in specialty choice at baseline and at their 3-year follow-up for students participating in the Psychiatry Early Experience Programme;Reference Holt, Mirvis, Bao, Cross, Hussain and Hutchings8 this may suggest that, although clinical shadowing may be useful, other opportunities provided by mentorship may have a greater influence on career selection. However, further follow-up and evaluation is required to determine the long-term effects of mentoring and early clinical exposure on decisions to pursue psychiatry.
Strengths and limitations
Our scheme data have several strengths. First, to our knowledge, this is the first published report to evaluate a formal mentoring scheme for UK medical students interested in psychiatry. Second, the high response rates to the two surveys (69.1 and 70.5%) assures us that we have gained a representative sample of students on the PsychStart programme. Third, the broad range of survey responses covering all year groups at Nottingham medical school gives strength to the generalisability of our findings.
However, we recognise that these data have the following limitations. First, they are subjective, based on students’ written reports and ratings of their mentoring relationships. The nature of the design of the evaluation did not allow for further probing about the students’ perceptions and experiences of the scheme. Furthermore, students’ stated interests may not necessarily predict future actions and result in core psychiatry training applications. Second, our data were derived from a self-selecting sample of students participating in the PsychStart scheme. We were therefore unable to draw any comparisons between students who do and do not receive mentoring in psychiatry and determine whether the scheme ‘adds value’ for those already interested in a career in the specialty. Finally, the maximum duration of mentoring relationships at the time of survey completion was just over 18 months; hence, we are unable to comment on the long-term effects of mentoring for this cohort.
Research recommendations
We recommend that future research should examine the long-term effects of mentoring and its impact on the quantity and quality of applications to core psychiatry training. Given prior research associating mentoring with improved medical school performance and training outcomes,Reference Frei, Stamm and Buddeberg-Fischer21,Reference Ong, Swift, Magill, Ong, Day and Al-Naeeb33 it would additionally be useful to examine the effects of mentoring in psychiatry on exam performance in the specialty. Delineating what motivates students who do and do not sign up to such mentoring schemes, and potential logistical barriers to taking part, could provide useful insights into factors both promoting and hindering engagement with psychiatry and mentoring. Further attention should be given to the experience of mentors, especially given that the concept of ‘reverse-mentoring’ is becoming increasingly recognised in the medical literature; this describes a process whereby junior medical professionals can mentor their senior colleagues, providing benefits such as enhanced understanding of digital technologies and online platforms, and improved workplace culture.Reference Clarke, Burgess, Van Diggele and Mellis34 Critically, it important to understand whether receiving mentoring from a psychiatrist rather than other doctors positively influences later career choice. Comparison of the impact of mentoring with other medical student enrichment activities, such as shadowingReference Holt, Mirvis, Bao, Cross, Hussain and Hutchings8 or participating in Balint groupsReference Monk, Hind and Crimlisk35 or medical student psychotherapy schemes,Reference Yakeley, Shoenberg and Heady36 needs further evaluation.
About the authors
Thomas Hewson, BMBS, BMedSci, is an Academic Clinical Fellow in Psychiatry with Pennine Care NHS Foundation Trust, UK. Nikki Thomas, MBChB, MRCPsych, PGCME, FHEA, is a consultant psychiatrist and undergraduate clinical tutor at Cambridgeshire and Peterborough NHS Foundation Trust, and an honorary consultant psychiatrist at Nottinghamshire Healthcare NHS Foundation Trust, UK. Kate Lovett, BSc, MBChB, MSc, FRCPsych, Cert Clin Ed (Dist), is a consultant psychiatrist with Livewell Southwest, Plymouth, and Dean of the Royal College of Psychiatrists, London, UK. Helen Bruce, MBBS, BSc, MA, FRCPsych, SFHEA, is a consultant child and adolescent psychiatrist at East London NHS Foundation Trust, Professorial Teaching Fellow at the Great Ormond Street Institute of Child Health, University College London, and Associate Dean for Recruitment into Psychiatry at the Royal College of Psychiatrists, London, UK. Derek K. Tracy, MBBCh, BAO, MSc, FHEA, FRSA, FFFMLM, FRCPsych, is a consultant psychiatrist and clinical director with Oxleas NHS Foundation Trust, and senior lecturer at the Department of Psychosis Studies, Institute of Psychiatry, Psychology and Neuroscience, King's College London, UK.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjb.2020.107.
Acknowledgements
We thank the following organisations and groups for their support in establishing the PsychStart mentoring scheme: University of Nottingham School of Medicine, University of Nottingham Students As Change Agents Programme, Nottinghamshire Healthcare NHS Foundation Trust, University of Nottingham Institute of Mental Health, Lincolnshire Partnership NHS Foundation Trust, Mind Matters Society, and the PsychStart student committee.
Author contributions
All authors were involved in data interpretation, manuscript preparation and proof-reading of the final article.
Declaration of interest
None.
ICMJE forms are in the supplementary material, available online at https://doi.org/10.1192/bjb.2020.107.












eLetters
No eLetters have been published for this article.