The association of the Mediterranean diet (MedDiet) with health and longevity has been consistently demonstrated in a large number of observational studies, as well as in some randomised clinical trials (RCT)( Reference Martínez-González and Bes-Rastrollo 1 – Reference Gay, Rao and Vaccarino 3 ). Comprehensive meta-analyses have reported a substantial decrease in the incidence of, and mortality from, various chronic diseases associated with higher adherence to the MedDiet( Reference Sofi, Macchi and Abbate 4 , Reference Schwingshackl, Schwedhelm and Galbete 5 ). Recently, an umbrella review classified the accumulated evidence as ‘robust’ regarding the protective role of the MedDiet in reducing the risk of total mortality, CVD overall, CHD, myocardial infarction, cancer, neurodegenerative diseases and diabetes mellitus( Reference Dinu, Pagliai and Casini 6 ).
Despite a general consensus on the beneficial influence of this diet on health, several issues remain unsolved. First, quantification of this diet has been carried out through indices and scores, which are different from each other with respect to the constructing algorithms, range of values, as well as food groups/nutrients that are included as components in these indices. Second, the relative role of the individual components of the MedDiet in the association with health outcomes of the MedDiet in toto has not been fully evaluated, except for a small number of studies( Reference Schwingshackl, Schwedhelm and Galbete 5 , Reference Trichopoulou, Bamia and Trichopoulos 7 , Reference Martínez-González, Guillén-Grima and De Irala 8 ). Third, in the vast majority of the studies, the cut-offs that are used to define high v. low adherence to the components of the MedDiet are population-specific; that is, they vary across populations according to the amount of consumption of each food group/nutrient composing the score. Recently, Sofi et al.( Reference Sofi, Macchi and Abbate 4 ) attempted to define common cut-offs by constructing a literature-based MedDiet score, which has been tested so far in a few studies( Reference Tong, Wareham and Khaw 9 , Reference Stefler, Malyutina and Kubinova 10 ).
The most recent meta-analysis on the association of the MedDiet with all-cause mortality( Reference Sofi, Macchi and Abbate 4 ) included investigations published up to June 2013. We have therefore performed an updated meta-analysis of prospective cohort studies aiming to (1) quantify the association of the MedDiet with all-cause mortality among adults using all available data up to January 2018, (2) to explore the heterogeneity across studies and (3) to evaluate the relative contribution of the individual components of this diet in the overall association of the MedDiet with mortality.
Methods
Search strategy
As a starting set, we used those studies published up to June 2013, which were included in the latest meta-analysis by Sofi et al.( Reference Sofi, Macchi and Abbate 4 ). Furthermore, in December 2017, we carried out a literature search in the PubMed database using the following keywords: (Mediterranean diet [Title/Abstract]) AND ((mortality[Title/Abstract]) OR (survival [Title/Abstract]) OR (longevity[Title/Abstract]) OR (death[Title/Abstract])) AND (‘2013/07/01’[Date - Publication]:‘2017/12/31’[Date - Publication]). Studies were included if they (i) had a cohort design or were case–control studies nested within cohorts, (ii) used a MedDiet index/score (labelled as MDS hereafter) defined a priori, (iii) investigated all-cause mortality and examined associations with MDS and (iv) provided the RR estimate (i.e. risk or rate ratios (RRa) hazard ratios (HR) or OR) and the corresponding 95 % CI, or sufficient information for their calculation. In all, three authors (C. B., D. E. and V. B.) independently screened the search results against these criteria to identify eligible articles, and checked the reference list of the publications retrieved to identify additional publications. Discrepancies were discussed and resolved in consensus. If additional data were requested from the identified publications, contact with authors was realised.
Study selection
The flow chart for the selection procedure, undertaken by our group in December 2017, is shown in Fig. 1. The corresponding information for studies published up to June 2013 has been published( Reference Sofi, Macchi and Abbate 4 ). This search identified 264 articles, with all abstracts published in English, included in the PubMed database, which were fully examined. From these, 236 were excluded because (a) they examined a different outcome and/or exposure, (b) there were reviews or discussions on the possible effects of the MedDiet on health or other related issues and (c) the association of the MedDiet with various end points including all-cause mortality was assessed among specific populations (e.g. people with CVD, diabetes mellitus, cancer and so on). From the remaining twenty-eight papers, the following were further excluded: one systematic review and meta-analysis evaluating the health effects of the MedDiet with various health outcomes( Reference Bloomfield, Koeller and Greer 11 ) because it did not provide the respective HR for the included cohort studies; three studies( Reference Zazpe, Sanchez-Tainta and Toledo 12 – Reference Menotti, Puddu and Maiani 14 ) because the so-called MedDiet patterns were derived from a posteriori factor analyses and not a priori; one study( Reference Kouris-Blazos and Itsiopoulos 15 ) because it was a discussion of previously reported findings that are included in the current meta-analysis( Reference Kouris-Blazos, Gnardellis and Wahlqvist 16 ); one study( Reference Sotos-Prieto, Bhupathiraju and Mattei 17 ) because the association with all-cause mortality was examined for changes in MedDiet scores from baseline to follow-up, and therefore could not match the rest of the studies that reported associations of baseline MedDiet with subsequent mortality; one study because it did not report the HR for the association of the MedDiet with total mortality but only for CVD incidence/mortality( Reference Panagiotakos, Georgousopoulou and Pitsavos 18 ); the study of Guasch-Ferré et al.( Reference Guasch-Ferré, Salas-Salvadó and Ros 19 ) because it referred to a discussion on findings of the PREvención con DIeta MEDiterránea (PREDIMED) RCT; the study by Ebell & Grad( Reference Ebell and Grad 20 ) in which the MedDiet was examined as a potential factor for recommendation among primary care physicians; and the study by Rautiainen et al.( Reference Rautiainen, Gaziano and Christen 21 ) in which the MedDiet was examined as a modifier of the effect of multivitamin use on total mortality (among other outcomes) in the Physicians’ Health Study II RCT. Furthermore, the study by Harmon et al. ( Reference Harmon, Boushey and Shvetsov 22 ) was also excluded as the subsequent study by Shvetsov et al.( Reference Shvetsov, Harmon and Ettienne 23 ) used the same study population and was more informative. Similarly, the study by Liese et al.( Reference Liese, Krebs-Smith and Subar 24 ) was excluded because the HR of the MedDiet with all-cause mortality were only graphically displayed and it was not possible to derive the actual values – nonetheless, the cohorts analysed in the indicated publication were the same as in three other studies( Reference Shvetsov, Harmon and Ettienne 23 , Reference George, Ballard-Barbash and Manson 25 , Reference Reedy, Krebs-Smith and Miller 26 ) that reported the respective HR and were included in our meta-analysis.
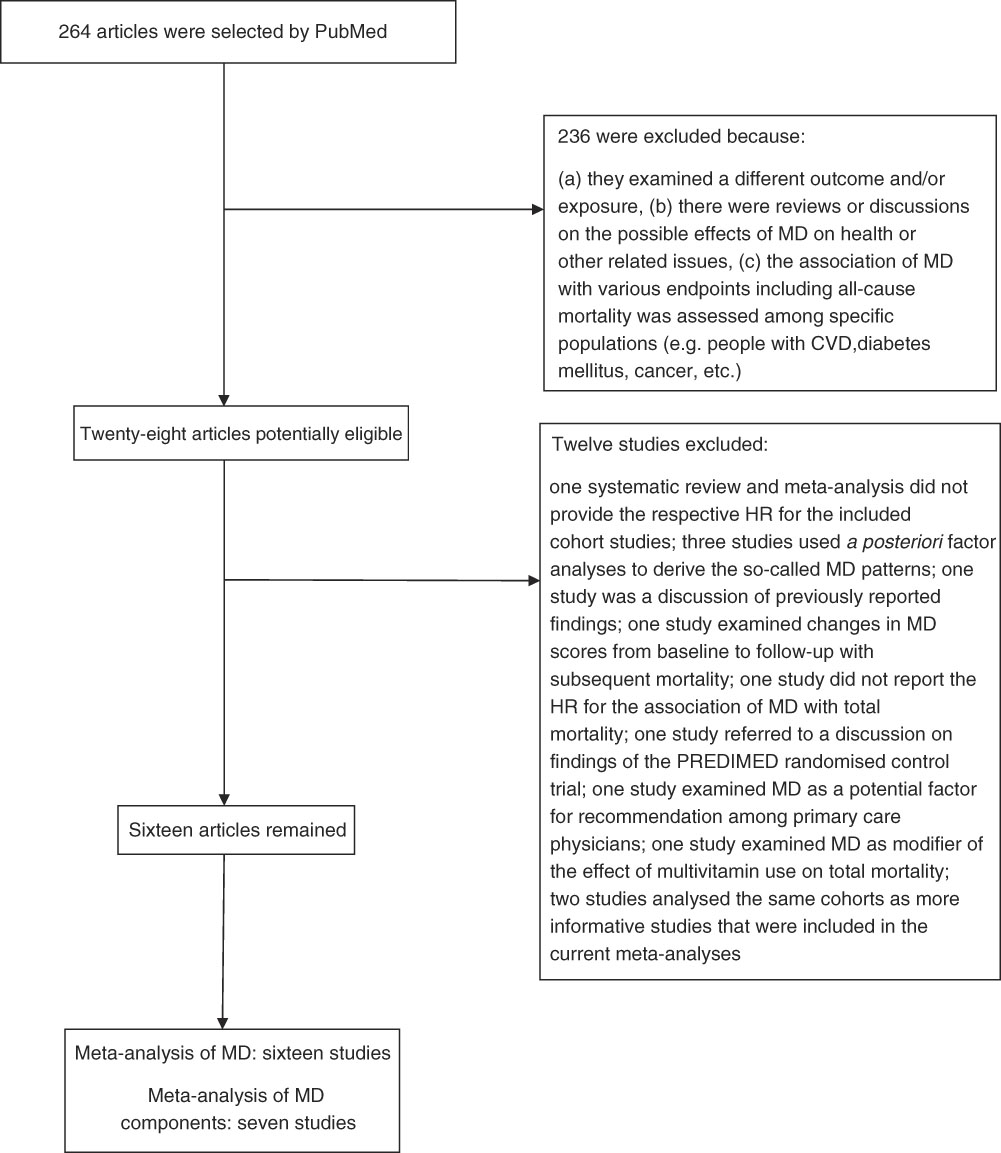
Fig. 1 Selection strategy to identify studies that were published from 1 July 2013 to 31 December 2017 and were included in the meta-analysis of the Mediterranean diet (MD) and overall mortality. HR, hazard ratio; PREDIMED, PREvención con DIeta MEDiterránea.
A total of sixteen articles were finally identified through the above process. One further study( Reference Lassale, Gunter and Romaguera 27 ) was identified upon examination of the references of these studies; this was an update of the study conducted by Trichopoulou et al.( Reference Trichopoulou, Orfanos and Norat 28 ) using the European Prospective Investigation into Cancer and Nutrition (EPIC) multi-centre cohort. However, as the study by Trichopoulou et al.( Reference Trichopoulou, Orfanos and Norat 28 ) contained more information relevant to the current meta-analysis (RR for each of the included cohorts and RR for each of the components of the MedDiet), we decided to keep the earlier study. Nonetheless, the summary RR of the overall meta-analysis remained the same when the most recent study by Lassale et al.( Reference Lassale, Gunter and Romaguera 27 ) was included instead of the Trichopoulou et al.( Reference Trichopoulou, Orfanos and Norat 28 ) study.
The studies analysed by Sofi et al.( Reference Sofi, Macchi and Abbate 4 ) were also included in the current meta-analysis, except for the study by Martínez-González et al.( Reference Martínez-González, Guillén-Grima and De Irala 8 ), as the most recent publication by Alvarez-Alvarez et al.( Reference Alvarez-Alvarez, Zazpe and Pérez de Rojas 29 ) used the same cohort and was more informative. Therefore, thirty articles were finally included in the meta-analyses of the MedDiet with all-cause mortality: fourteen published before( Reference Trichopoulou, Bamia and Trichopoulos 7 , Reference Kouris-Blazos, Gnardellis and Wahlqvist 16 , Reference Trichopoulou, Orfanos and Norat 28 , Reference Trichopoulou, Kouris-Blazos and Wahlqvist 30 – Reference Tognon, Nilsson and Lissner 40 ) and sixteen published after June 2013 (up to 31 December 2017)( Reference Tong, Wareham and Khaw 9 , Reference Stefler, Malyutina and Kubinova 10 , Reference Shvetsov, Harmon and Ettienne 23 , Reference George, Ballard-Barbash and Manson 25 , Reference Reedy, Krebs-Smith and Miller 26 , Reference Alvarez-Alvarez, Zazpe and Pérez de Rojas 29 , Reference Cuenca-García, Artero and Sui 41 – Reference Shah, Leonard and Finley 50 ). Detailed characteristics of these studies are shown in Table 1. In eighteen of these publications, RR of all-cause mortality associated with at least one of the components of the MedDiet were reported.
Table 1 Main characteristics of prospective studies included in the meta-analyses reporting on the association of the Mediterranean diet (MedDiet) and of its components and overall mortality
MDS, Mediterranean diet score; HALE, Healthy Ageing: a Longitudinal Study in Europe; EPIC, European Prospective Investigation into Cancer and Nutrition elderly study; NIH-AARP, National Institutes of Health – AARP (formerly known as the American Association of Retired Persons); M, men; W, women; MET, metabolic equivalents; NA, non-applicable; NLCS, Netherlands Cohort Study; VIP, Vasterbotten Intervention Program; MONICA, MONItoring trends and determinants of CVD; NRP1A, National Research Program 1A; TV, television; COSM, Cohort of Swedish Men; SMC, Swedish Mammography Cohort; ILSA, Italian Longitudinal Study on Aging; MMSE, Mini Mental State Examination; GDS, Geriatric Depression Scale; HAPPIE, Health Alcohol and Psychosocial Factors in Eastern Europe; REGARDS: REasons for Geographic and Racial Differences in Stroke Study; HRT, hormone replacement therapy; ULSAM, Uppsala Longitudinal Study of Adult Men; SUN, Sequimenta Universidad de Navarra.
* The MedDiet indices from each study that were used in the current analysis are shown in this column, labelled for simplicity as MDS. The labels of these indices may be different in the original publications.
†Associations of (at least one) MedDiet components with mortality were reported in this study.
Data extraction
For each study, data were extracted on study design, country, duration of follow-up, enrolment period, number of subjects or person(time)-at-risk, number of deceased, age of the study population, estimates of RR (e.g. HR) and their corresponding 95 % CI, construction rule of adherence to the MedDiet and range of MDS and covariates adjusted for in the analysis. If a study used more than one MedDiet index to measure the adherence to the MedDiet( Reference Tong, Wareham and Khaw 9 , Reference Shvetsov, Harmon and Ettienne 23 , Reference Alvarez-Alvarez, Zazpe and Pérez de Rojas 29 , Reference Mitrou, Kipnis and Thiébaut 34 , Reference Tognon, Rothenberg and Eiben 36 , Reference Tognon, Nilsson and Lissner 40 ) the one more closely resembling the first, original MedDiet index that appeared in the literature( Reference Trichopoulou, Kouris-Blazos and Wahlqvist 30 , Reference Trichopoulou, Costacou and Bamia 51 ) was used. From each study, we selected RR estimates adjusted for the largest number of potential confounders.
The MedDiet was assessed in the vast majority of the studies through FFQ (quantitative or semi-quantitative) enquiring usual dietary intakes over a period preceding enrolment (e.g. previous year). Dietary history( Reference Knoops, de Groot and Kromhout 32 , Reference Tognon, Rothenberg and Eiben 36 , Reference Buckland, Agudo and Travier 37 ), dietary records or weighted food records( Reference Sjögren, Becker and Warensjö 35 , Reference McNaughton, Bates and Mishra 39 , Reference Cuenca-García, Artero and Sui 41 , Reference Tognon, Lissner and Sæbye 42 ) and 24-h dietary recall( Reference Vormund, Braun and Rohrmann 43 ) were also used. Most FFQ had been validated for (at least some) dietary intakes of the MedDiet components.
RR for all-cause mortality were reported: (a) only for continuous increments of MDS (e.g. one or two units) in nine studies( Reference Trichopoulou, Bamia and Trichopoulos 7 , Reference Tong, Wareham and Khaw 9 , Reference Kouris-Blazos, Gnardellis and Wahlqvist 16 , Reference Trichopoulou, Kouris-Blazos and Wahlqvist 30 – Reference Knoops, de Groot and Kromhout 32 , Reference Tognon, Nilsson and Lissner 40 , Reference Tognon, Lissner and Sæbye 42 , Reference Shah, Leonard and Finley 50 ), (b) only as a comparison of different categories of MDS in ten studies( Reference Shvetsov, Harmon and Ettienne 23 , Reference George, Ballard-Barbash and Manson 25 , Reference Reedy, Krebs-Smith and Miller 26 , Reference Alvarez-Alvarez, Zazpe and Pérez de Rojas 29 , Reference Mitrou, Kipnis and Thiébaut 34 , Reference McNaughton, Bates and Mishra 39 , Reference Cuenca-García, Artero and Sui 41 , Reference Limongi, Noale and Gesmundo 47 – Reference Franzon, Byberg and Sjögren 49 ) and (c) for both (a) and (b) in eleven studies( Reference Stefler, Malyutina and Kubinova 10 , Reference Trichopoulou, Orfanos and Norat 28 , Reference Lagiou, Trichopoulos and Sandin 33 , Reference Sjögren, Becker and Warensjö 35 – Reference van den Brandt 38 , Reference Vormund, Braun and Rohrmann 43 – Reference Bo, Ponzo and Goitre 46 ). Categories of MDS were defined arbitrarily or were based on percentiles.
Statistical analysis
Mediterranean diet score
To estimate more closely the association of the MedDiet with all-cause mortality, we considered separately studies that reported RR for contrasting categories of upper to lowest MDS (thus assuming a non-linear association) and studies that estimated RR for continuous increments of MDS (thus assuming a log linear shape of the association). For the former studies, RR for the highest v. lowest study-specific categories of MDS were analysed. For the latter studies, RR were re-estimated (if needed) to correspond to 1sd increment in MDS, in order to account for differences in the range of MDS values.
For studies that did not report sd for the MDS, we assumed the same sd as those reported in other studies that used the same MDS. In the study by Tong et al.( Reference Tong, Wareham and Khaw 9 ), the respective sd was obtained by personal communication with the authors. For the study of Prinelli et al.( Reference Prinelli, Yannakoulia and Anastasiou 44 ), the sd of the MDS was obtained by the study of Georgousopoulou et al.( Reference Georgousopoulou, Kastorini and Milionis 52 ), which used the same score and reported its sd.
Mediterranean diet components
Intakes of the following nine major MedDiet components were examined: vegetables, legumes, fruit/nuts, cereals, fish and shellfish, meat and meat products, milk and dairy products, alcohol and lipid ratio in any way this was defined (e.g. monounsaturated-to-saturated, mono+polyunsaturated-to-saturated and so on). We also considered RR reported for olive oil or wine intakes as these are the main sources of MUFA and alcohol intake, respectively, in the typical MedDiet.
Similarly to the analysis of MDS, mortality RR for each of the indicated food groups/nutrients were estimated in some studies for continuous increments in the intake of the MDS component or as comparisons of categories of the component intake. For continuous increments, we re-estimated mortality RR for one study-specific sd increment in order to account for differences in the intakes of the MedDiet components across different populations. Among studies reporting mortality RR for different categories of MedDiet components, the vast majority contrasted the above/below-median study-specific consumptions. For studies that used other categories of comparison, we considered in our meta-analysis the comparison that resembled more the above/below-median comparison.
Meta-analysis of Mediterranean diet score and Mediterranean diet score components
Summary RR were estimated by combining the study-specific RR (considered as explained above) using random-effects models to take into account the between-study heterogeneity( Reference DerSimonian and Laird 53 ). Each study’s ln (RR) was weighted by the inverse of its variance plus the between-study variance component τ 2 computed by the moment estimator( Reference DerSimonian and Laird 53 ). Heterogeneity among studies was evaluated with χ 2 test and I 2 statistic( Reference Greenland 54 , Reference Higgins and Thompson 55 ). Publication bias was evaluated through funnel plots( Reference Stuck, Rubenstein and Wieland 56 ) and with the Egger’s test( Reference Macaskill, Walter and Irwig 57 ).
We also conducted meta-analyses in strata of geographical area (USA, Australia, Europe (Northern, Central/Eastern, Western, Mediterranean)), range of MDS scale (0–9, >9), in order to account for the different spread of the distribution of the MedDiet indices used in each study, and year of publication (<2010, 2010–2014, >2014). RR estimated from the multi-centre EPIC study( Reference Trichopoulou, Orfanos and Norat 28 ) were considered both overall and cohort-specific in meta-analyses stratified by country.
Sensitivity analyses were also conducted by omitting one study at a time from the analyses and assessing its effect on the overall summary RR.
The significance threshold was set at 0·05, whereas all statistical analyses were conducted using R statistical software version 3.4.2.
Results
In Table 1 the main characteristics of the thirty articles (including a total of 225 600 deaths) considering a quantitative relation between MDS and all-cause mortality are shown. Out of these, seven were conducted in North America, twenty-two in Europe and one in Australia. Most studies used a 9- or 10-scale MedDiet index, except for the studies conducted by Buckland et al.( Reference Buckland, Agudo and Travier 37 ), Prinelli et al.( Reference Prinelli, Yannakoulia and Anastasiou 44 ), Limongi et al.( Reference Limongi, Noale and Gesmundo 47 ), Stefler et al.( Reference Stefler, Malyutina and Kubinova 10 ) and Whalen et al.( Reference Whalen, Judd and McCullough 48 ), which used indices of broader ranges. Studies by Mitrou et al.( Reference Mitrou, Kipnis and Thiébaut 34 ), Tognon et al.( Reference Tognon, Rothenberg and Eiben 36 ), Tognon et al.( Reference Tognon, Nilsson and Lissner 40 ), Shvetsov et al.( Reference Shvetsov, Harmon and Ettienne 23 ), Tong et al.( Reference Tong, Wareham and Khaw 9 ) and Alvarez-Alvarez et al.( Reference Alvarez-Alvarez, Zazpe and Pérez de Rojas 29 ) used more than one MedDiet index; from these the traditional MDS, the refined version of the modified Mediterranean diet score (refined mMDS), the alternate MDS without energy adjustment in each of the MedDiet components, the MDS based on cohort-specific medians (mMDS) and the MDS proposed by Trichopoulou et al.( Reference Trichopoulou, Costacou and Bamia 51 ), respectively, were considered in the current meta-analyses, all labelled as MDS for reasons of simplicity.
Highest v. lowest level of adherence to the Mediterranean diet in relation to all-cause mortality
Fig. 2 shows the RR of all-cause mortality for the study-specific highest v. lowest MDS levels of adherence among the twenty-one studies, which reported such associations. In most studies that used an MDS ranging from 0 to 8/9, the highest/lowest level of adherence was 6–8 or 6–9 v. 0–2 or 0–3, respectively, except for the studies by Tognon et al.( Reference Tognon, Rothenberg and Eiben 36 ) (6–9 v. 0–5), van den Brandt( Reference van den Brandt 38 ) (5–9 v. 0–4) and Vormund et al.( Reference Vormund, Braun and Rohrmann 43 ) (6–9 v. <4). Buckland et al.( Reference Buckland, Agudo and Travier 37 ) contrasted 11–18 v. 0–6 scores of their 0–18 MDS scale, Prinelli et al.( Reference Prinelli, Yannakoulia and Anastasiou 44 ) the Q3 v. Q1 of their 46-point MedDiet index, Limongi et al.( Reference Limongi, Noale and Gesmundo 47 ) the Q3: >24 v. Q1: <20 of their MDS ranging from 0 to 44, Stefler et al.( Reference Stefler, Malyutina and Kubinova 10 ) 11–17 v. 0–7 scores of a 0–18 point MDS and Whalen et al.( Reference Whalen, Judd and McCullough 48 ) the Q5: (36–50) v. Q1 (14–26) of their 0–55 MDS.
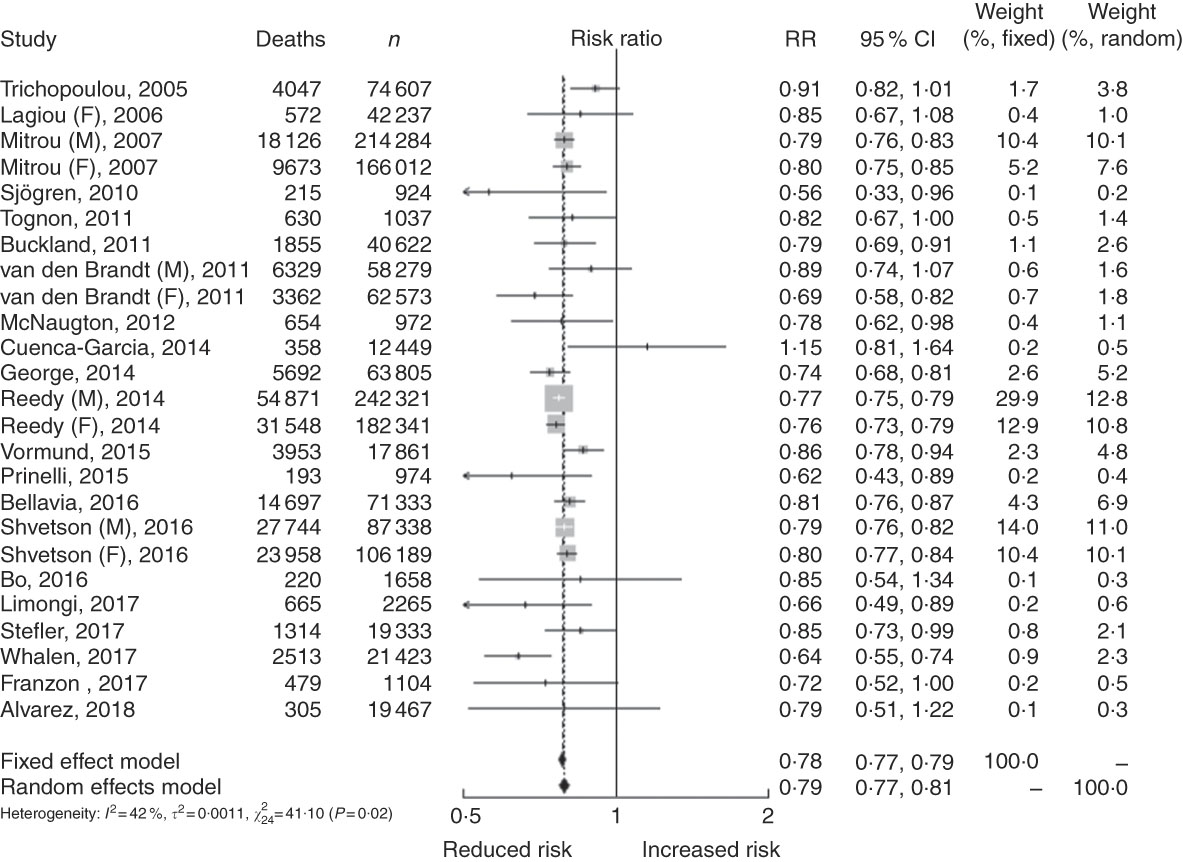
Fig. 2 Relative risks (RR) and 95 % CI of mortality associated with the highest v. the lowest level of Mediterranean diet score from all studies included. The combined hazard ratio and 95 % CI were calculated using the random-effects models. F, female; M, male.
All studies reported inverse associations, which were statistically significant in sixteen of them. Only one study( Reference Cuenca-García, Artero and Sui 41 ) reported an increased (non significant) mortality risk (RR: 1·15, 95 % CI, 0·81, 1·64) with increased MDS.
The summary mortality ratio for the highest v. lowest MDS level indicates an inverse and significant association: RR 0·79 (95 % CI 0·77, 0·81). Heterogeneity was moderate overall (I 2=42 %; P-heterogeneity 0·02).
All-cause mortality in relation to 1sd increase in adherence to the Mediterranean diet
In Fig. 3, RR of all-cause mortality per one study-specific sd increase in MDS are shown for the twenty studies with available information. Study-specific sd ranged from 1·4( Reference Trichopoulou, Orfanos and Norat 28 ) to 5( Reference Prinelli, Yannakoulia and Anastasiou 44 ) units in MDS. Inverse associations, statistically significant in fifteen studies, were reported in all publications, except for the study by Lasheras et al.( Reference Lasheras, Fernandez and Patterson 31 ), which reported increased albeit not significant mortality among eighty-seven Spanish people ≥80 years of age for a 1·7-unit increase in MDS.
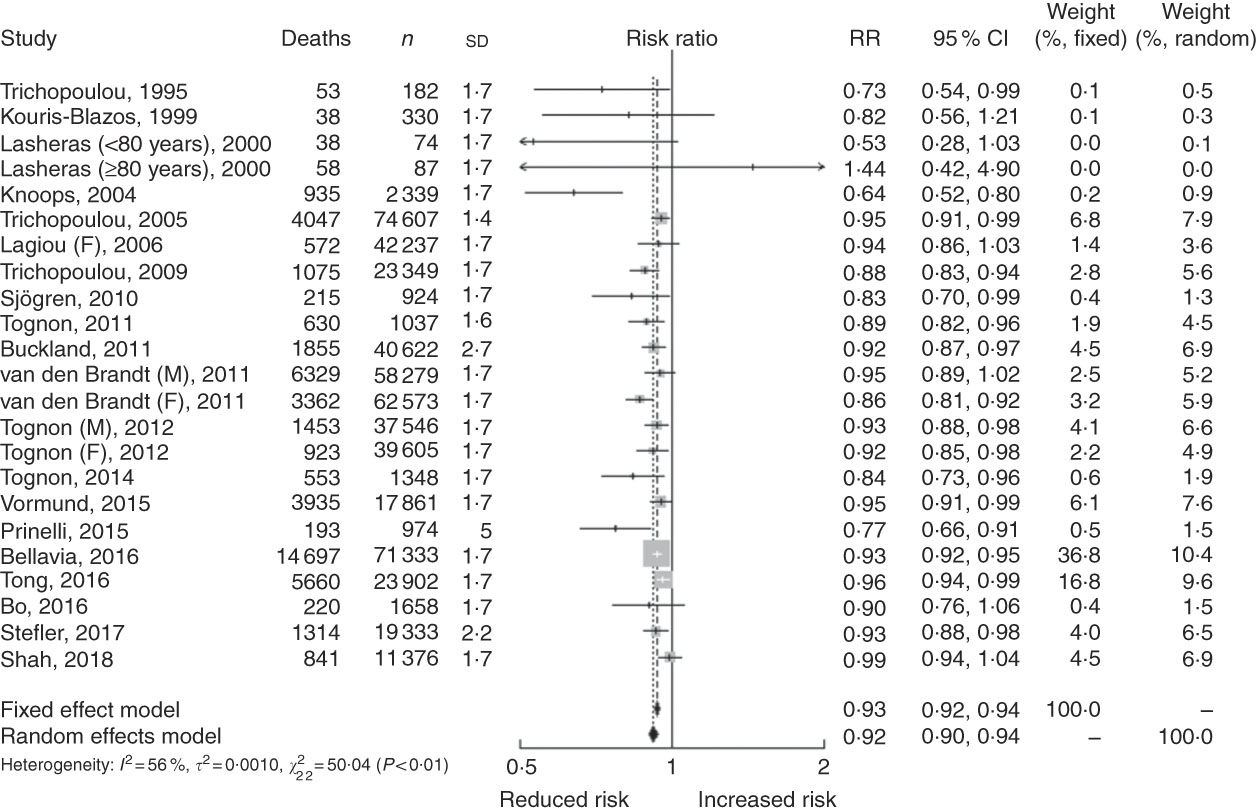
Fig. 3 Relative risks (RR) and 95 % CI of mortality per one study-specific standard deviation increment in Mediterranean diet score from all studies included. The combined hazard ratio and 95 % CI were calculated using the random-effects models. F, female; M, male.
The summary mortality RR per 1sd MDS increment was 0·92 (95 % CI 0·90, 0·94), with moderate-to-high heterogeneity (I 2=56 %; P-heterogeneity <0·01).
Subgroup analysis
Summary RR (95 % CI) for the highest v. lowest MDS level of adherence, as well as per 1sd MDS increment in strata of selected covariates, are shown in Table 2. As only two of the studies reporting RR for continuous increments of MDS were conducted outside Europe (one in USA and one in Australia), stratified meta-analysis of RR per 1sd increment in MDS by geographical location was undertaken only among European studies.
Table 2 Summary relative risks (RR) and 95 % CI of all-cause mortality for the highest v. the lowest and per 1sd increment in the adherence to the Mediterranean diet (MedDiet) in strata of selected covariates
MDS, Mediterranean diet score; NA, non-applicable.
* Only two studies were undertaken outside Europe: one in the USA and one in Australia.
† In analysis among European countries, the nine cohort-specific RR reported in the study by Trichopoulou et al. (2005) were considered instead of the overall-cohorts RR, whereas the multi-centre European study by Knoops et al. (2004) was excluded as it did not report cohort-specific RR. Total number of studies in this meta-analysis: twenty-three for highest v. lowest MDS and twenty-five for per sd MDS increments.
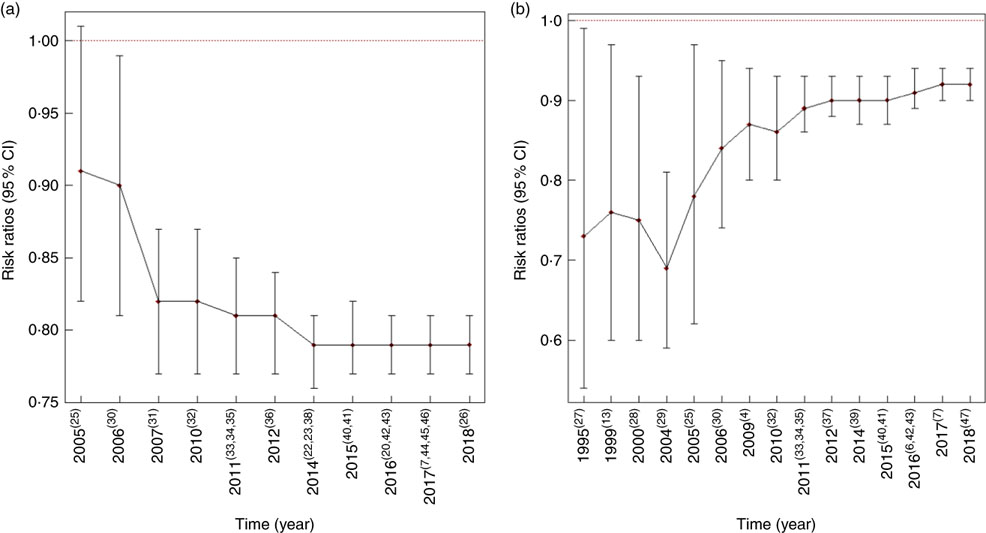
RR of highest v. lowest MDS among studies undertaken in USA and Europe were 0·78 (95 % CI 0·76, 0·80) and 0·82 (95 % CI 0·78, 0·88), respectively, with higher heterogeneity observed among the US (I 2=55 %, P-heterogeneity 0·02) rather than European studies (I 2=10 %, P-heterogeneity 0·33). In analysis confined to European studies, stratification by geographical location revealed stronger summary RR among Mediterranean populations, and weakest ones among the fewer studies conducted in central/eastern Europe for both the highest/lowest or the per sd increment in MDS. Similar summary RR were estimated among studies with different spread of distribution of MDS – that is, those that used MDS scales of 0–9 or greater. Stratification by publication year revealed high consistency in RR after 2011, when the majority of the studies were published (Fig. 6(a) and (b)).
Heterogeneity was evident by country location. Across European studies heterogeneity was evident for RR corresponding to 1sd increment in MDS, but not for studies contrasting highest/lowest level of adherence to the MedDiet.
Sensitivity analysis and publication bias
In sensitivity analysis, the summary mortality RR in association with MDS adherence (highest v. lowest or per sd increment) did not change appreciably when each study was excluded in turn, and the RR was estimated from the remaining studies (mortality RR of highest v. lowest MDS ranged from 0·78 to 0·79; mortality RR per sd increment ranged from 0·92 to 0·93). The funnel plots of individual RR for the highest v. lowest MDS, and for the per sd MDS increment are shown in Figs. 4 and 5, respectively. There was no indication of publication bias for studies reporting RR for the highest v. lowest MDS adherence (P-value 0·67), but there was evidence for publication bias for studies reporting RR for 1sd increment in MDS (P<0·01), probably owing to the absence of studies reporting less precise RR showing increased mortality with continuous increments of MedDiet adherence. Nevertheless, when we used the trim-and-fill method including the missing studies, the estimated association between the per- MDS increment and mortality did not change appreciably and retained its statistical significance.
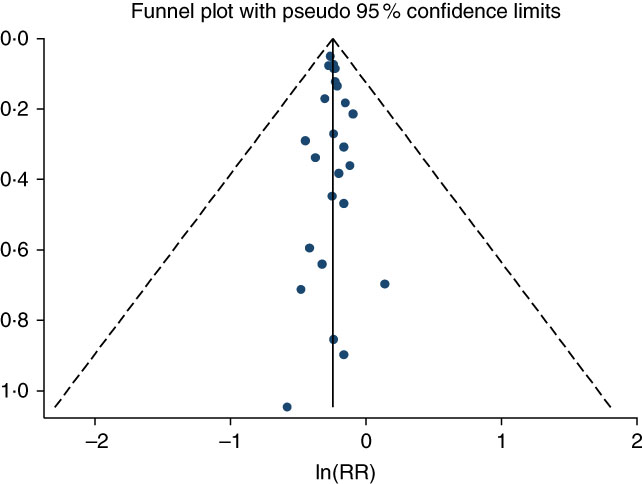
Fig. 4 Funnel plot for the assessment of publication bias in the studies included in the meta-analysis of mortality in association with the highest v. the lowest level of Mediterranean diet score (P for Egger test 0·67; P for Begg’s test 0·83). Dashed diagonal lines indicate 95 % CI.
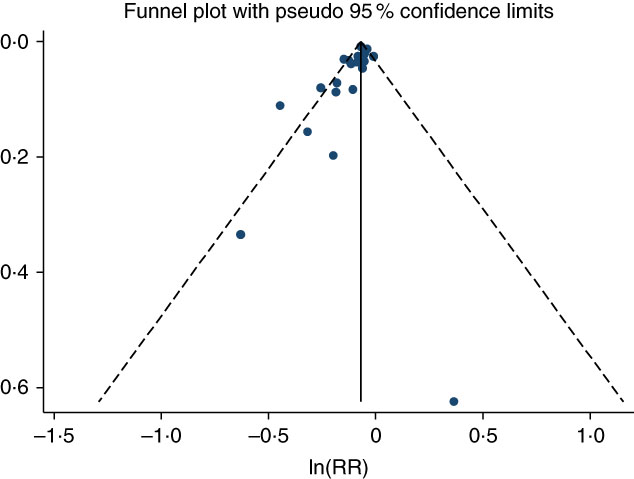
Fig. 5 Funnel plot for the assessment of publication bias in the studies included in the meta-analysis of mortality per one study-specific standard deviation increment in Mediterranean diet score (P for Egger test <0·01; P for Begg’s test 0·01). Dashed diagonal lines indicate 95 % CI).
All-cause mortality in relation to intakes of components of the Mediterranean diet
In all, eighteen studies reported associations of at least one component of the MedDiet with all-cause mortality( Reference Trichopoulou, Bamia and Trichopoulos 7 , Reference Stefler, Malyutina and Kubinova 10 , Reference Kouris-Blazos, Gnardellis and Wahlqvist 16 , Reference Trichopoulou, Orfanos and Norat 28 – Reference Lagiou, Trichopoulos and Sandin 33 , Reference Tognon, Rothenberg and Eiben 36 – Reference van den Brandt 38 , Reference Tognon, Nilsson and Lissner 40 , Reference Tognon, Lissner and Sæbye 42 – Reference Prinelli, Yannakoulia and Anastasiou 44 , Reference Limongi, Noale and Gesmundo 47 , Reference Shah, Leonard and Finley 50 ). The studies by Knoops et al.( Reference Knoops, de Groot and Kromhout 32 ) and Lagiou et al.( Reference Lagiou, Trichopoulos and Sandin 33 ) reported RR only for alcohol intake; however, the latter study reported mortality RR contrasting high v. moderate ethanol consumption, which was incompatible with the contrasting categories of alcohol intake reported in the rest of the studies (mostly above/below median or moderate v. other). Therefore, that article was not included in the meta-analysis of alcohol intake. Moreover, the study by Vormund et al.( Reference Vormund, Braun and Rohrmann 43 ) reported mortality ratios contrasting consumers v. non-consumers for each of the MedDiet components; these categories of comparison were incompatible with those used in the rest of the studies (above/below median or per specific MDS increment). Thus, the indicated publication was also not included in the meta-analysis of MedDiet components in relation to mortality.
In Table 3, the summary RR of mortality (from random effects models) corresponding to the above/below median intake comparison, as well as to moderate intake v. other for alcohol consumption, are shown for each of the nine components of the MDS. Results from the meta-analyses of mortality RR per sd increment were in the same direction. Summary RR were based on different number of studies for each component, as some studies reported associations for a few components only.
Table 3 Summary relative risks (RR) and 95 % CI of all-cause mortality for the above v. below the study-specific median intake in each of the components of the Mediterranean diet (MedDiet)
* Moderate v. none/excess consumption.
† Above v. below study specific median.
Table 3 reveals those MedDiet components that showed a significant association with all-cause mortality either inverse – (a) fruit/nuts, (b) vegetables, (c) alcohol (moderate v. other) – or positive – meat. With respect to the rest of the components, null associations were estimated for legumes and fish intake, weak/minimal inverse associations for cereal and lipid ratio intakes, respectively, and a weak positive association for dairy intakes.
Olive oil in relation to mortality was investigated in four studies( Reference Stefler, Malyutina and Kubinova 10 , Reference Buckland, Agudo and Travier 37 , Reference Prinelli, Yannakoulia and Anastasiou 44 , Reference Limongi, Noale and Gesmundo 47 ), with RR reflecting the above v. below median intake comparison in all of them except for the study by Buckland et al.( Reference Buckland, Agudo and Travier 37 ) who reported RR for the highest (>24·7 g/d) v. lowest (<13·7 g/d) consumption. No detailed information of the type of olive oil was given in these four studies. The summary RR of these studies was 0·97 (95 % CI 0·82, 1·15). Similarly, RR for wine intake in association with all-cause mortality were reported in two studies( Reference Tognon, Nilsson and Lissner 40 , Reference Tognon, Lissner and Sæbye 42 ) comparing the above/below median intakes. The summary RR based on these two studies was 0·87 (95 % CI 0·78, 0·97).
In Fig. 7, the excess relative risk (ERR) associated with each of the MedDiet components is depicted as estimated from the summary RR. The ERR was highest for moderate alcohol intake (−14 %), followed by above-the-median intakes: fruit (−12 %), meat (7 %) and vegetable (−6 %) intakes, cereals (−5 %), dairy (5 %) and lipid ratio (−2 %) intakes. The ERR for fish and legume intake were close to zero.
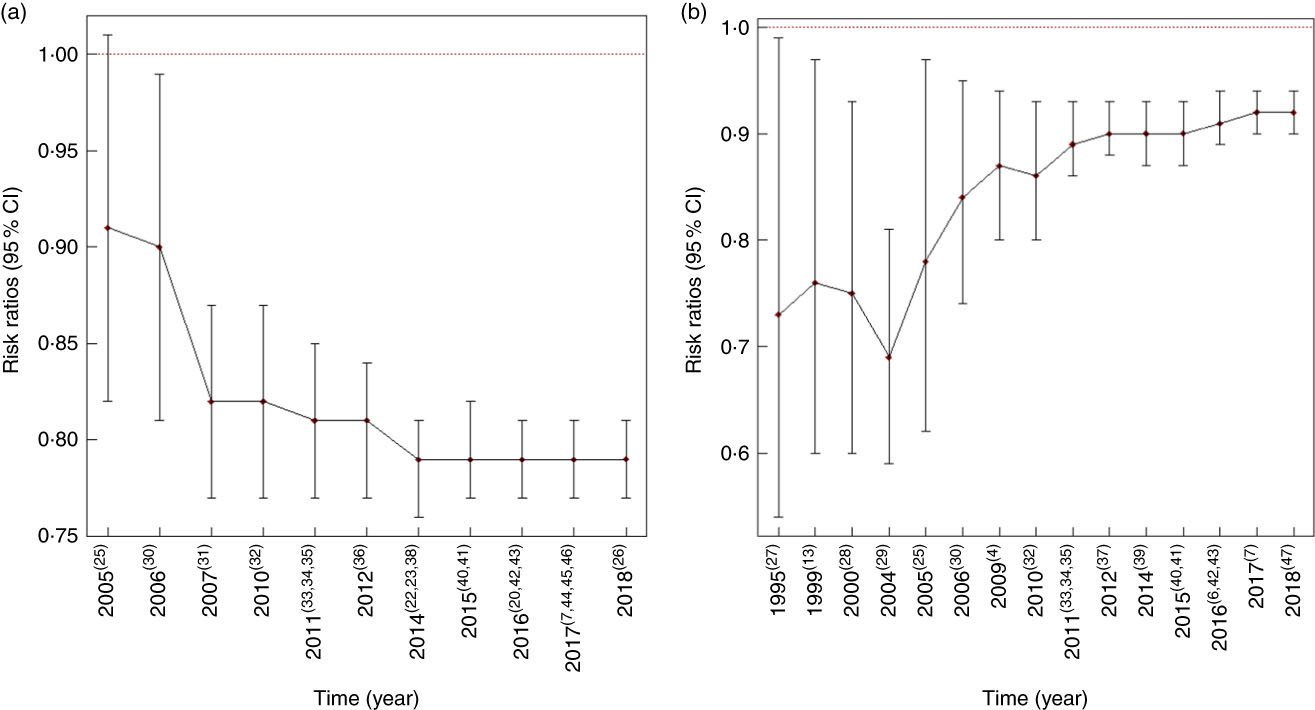
Fig. 6 (a) Cumulative meta-analysis of cohort studies on the Mediterranean Diet (MedDiet) (highest v. lowest category in each study) and mortality. (b) Cumulative meta-analysis of cohort studies on the MedDiet (per one study-specific standard deviation increment) and mortality. Diamonds are the estimated summary relative risks and error bars are the associated 95 % CI, by year of publication. References of studies included in the cumulative meta-analyses are shown in parentheses.
Discussion
In the present meta-analyses of all published prospective investigations up to 31 December 2017, including thirty studies and 225 600 deaths, we found an inverse, significant association between conformity to the MedDiet and all-cause mortality. We also estimated summary mortality ratios for each of the nine components of the MedDiet. In these analyses, relatively stronger and statistically significant associations were highlighted for moderate alcohol (RR=0·86) consumption, as well as for above-the-median intakes of fruit (RR=0·88), meat (RR=1·07) and vegetables (RR=0·94).
Our findings are in agreement with recently published studies( Reference Sofi, Macchi and Abbate 4 , Reference Dinu, Pagliai and Casini 6 ). In the last meta-analysis of observational studies published up to June 2013, Sofi et al. ( Reference Sofi, Macchi and Abbate 4 ) estimated a summary RR of 0·91 (95 % CI 0·89, 0·93) associated with a 2-point increment in MDS with moderate heterogeneity. Although previous studies have estimated RR for either continuous increments or categorical comparisons of MDS, we have chosen to provide RR separately for the two approaches, avoiding making any assumptions for transforming the reported RR (i.e. from expressing continuous increments to reflecting categorical comparisons of MDS and vice versa). Our approach adds to interpreting and communicating the results regarding the health benefits associated with the MedDiet: realistic increments of the adherence to the MedDiet result in a reduction of 8 % in all-cause mortality, whereas this survival benefit achieves its maximum (21 % reduction in mortality rates) among adherers at the highest as compared with those in the lowest percentiles of MDS.
In our meta-analysis, we observed moderate heterogeneity across studies, similarly to previous meta-analyses( Reference Sofi, Macchi and Abbate 4 ). When exploring this heterogeneity in strata of pre-defined covariates, none of the stratification variables had any appreciable influence on the summary RR, which were always indicative of inverse and significant associations of the MedDiet with mortality. Heterogeneity, however, was decreased, in a significant manner, among European as compared with US studies. Studies across USA and Europe may differ in definitions and components of MDS, intakes of foods included in MDS, correlations between components of MDS and so on. No appreciable heterogeneity across European studies was observed in our investigation, similarly to previous meta-analyses( Reference Sofi, Abbate and Gensini 58 ), even though the reported associations were somewhat stronger in Mediterranean rather than in western and northern European countries. This is expected, as Mediterranean populations are likely to have greater adherence to MedDiet scores. The constructing algorithm underlying MedDiet indices, which usually results in different MDS ranges of scales, did not seem to influence the results of our meta-analysis. Studies published before 2011 were fewer and smaller with more imprecise RR as compared with the large body of studies published after 2011. Nevertheless, heterogeneity by year of publication (before/after 2011) was not statistically significant.
The beneficial effect of the MedDiet on several health outcomes has been often attributed to constituents such as vitamins, minerals, fibre and antioxidants abundant in foods of plant origin, ethanol and polyphenols in wine (the most frequent type of alcoholic beverage consumed in the traditional MedDiet) and antioxidative and anti-oncogenic effects of oleic acid abundant in olive oil, highly consumed in the MedDiet( Reference Menendez and Lupu 59 Reference Dedoussis, Kanoni and Mariani – Reference Pelucchi, Bosetti and Negri 61 ). In our study, we attempted to evaluate the contribution of each component on the association with mortality of the MedDiet in toto, by performing suitable meta-analyses. Examination of the summary mortality ratios revealed inverse or null associations for higher intakes of all MedDiet components except for meat and dairy intakes, for which the associations were positive, as reflected in the scores. Moreover, our results indicated highest protection for moderate (v. excessive or minimal) alcohol consumption (14 %), followed by above (v. below)-the-median consumption of fruit (12 %). Low (below-the-median) consumption of meat and dairy products and high (above-the-median) consumption of vegetables and cereals were associated with lower mortality rates of about 5–6 %. The association with mortality of the lipid ratio was minimal (2 %), whereas consumption of fish and seafood, as well as of legumes, was not associated with mortality. The importance of alcohol in the association of MDS with mortality may be partly owing to the more valid, as compared with the rest of the MedDiet components, reporting of habitual intake of alcoholic beverages. On the other hand, fruit and vegetables, as well as meat and meat products, are foods widely consumed in the countries included in this meta-analysis and therefore a ‘true’ association with mortality may be more easily detected as compared with other non-frequently consumed foods in the non-Mediterranean countries, such as legumes and olive oil (included in the lipid ratio).
A few studies have investigated the contribution of the MedDiet components in the association of this diet with mortality. An empirical investigation by Trichopoulou et al. ( Reference Trichopoulou, Bamia and Trichopoulos 7 ) (included in the current meta-analysis) based on the Greek EPIC also highlighted the high importance of moderate (v. excessive or minimal) alcohol intake and the neutral contribution of fish intake to the association of the MedDiet with mortality. Although the magnitudes of the RR in that study were, naturally, different from our summary RR, the order of the relative importance of the different components was quite similar in their study and ours.
Our results regarding the contribution of the individual components to the overall association of the MedDiet with mortality should be interpreted with caution as (1) intakes of the indicated foods/nutrients have been collected with different methods and differ (on average) across studies included in the meta-analysis, (2) different number of studies are used in the meta-analysis of each of the individual components and (3) definitions of the foods comprising the MedDiet components are different across studies (e.g. only whole-grain cereals are used in the alternate MDS, but all types of cereals are included in the original MDS). Nevertheless, the summary RR for the nine MedDiet components are generally in agreement with the current literature. Several studies have reported the survival benefit of moderate alcohol intake( Reference Di Castelnuovo, Costanzo and Bagnardi 62 ), of higher intakes of vegetables, fruit and nuts( Reference Wang, Ouyang and Liu 63 , Reference Grosso, Yang and Marventano 64 ) and of low/no intake of meat (especially red meat) and meat products( Reference Abete, Romaguera and Vieira 65 , Reference Wang, Lin and Ouyang 66 ). For dairy products, a recent meta-analysis( Reference Schwingshackl, Schwedhelm and Galbete 5 ) did not find an association with mortality. For cereals, results are controversial, as they include whole-grain cereals that have been found to be inversely associated with mortality( Reference Schwingshackl, Schwedhelm and Galbete 5 , Reference Aune, Keum and Giovannucci 67 ), as well as refined grains for which no or a moderate direct association was found in previous meta-analyses( Reference Schwingshackl, Schwedhelm and Galbete 5 , Reference Hajishafiee, Saneei and Benisi-Kohansal 68 ). Fish and legume intakes have been inversely associated with mortality( Reference Schwingshackl, Schwedhelm and Galbete 5 , Reference Zhao, Sun and Yang 69 , Reference Marventano, Izquierdo Pulido and Sánchez-González 70 ). In our study, we did not detect an association with mortality for these two food groups, probably owing to their low intakes evident in the studies included in the component-specific meta-analyses. We did not find an appreciable influence in mortality of the lipid ratio intake, either. Although this ratio was proposed originally to reflect a high monounsaturated (mainly owing to high consumption of olive oil in the MedDiet) as opposed to saturated lipid intake, this is not always the case: in many studies undertaken in countries that culturally do not consume olive oil, monounsaturated lipid intake can be of animal origin, whereas polyunsaturated lipid intakes are usually added in the nominator in order to reflect lipid intake from plant origin. In a meta-analysis of Schwingshackl & Hoffmann( Reference Schwingshackl and Hoffmann 71 ) examining the role of MUFA (from plant and animal origin) and olive oil on mortality, the most consistent findings for reduced mortality were for olive oil intake.
Major strengths of our study are the thorough systematic review, allowing us to estimate the association of the MedDiet with all-cause mortality by comparing the extremes of adherence with this diet, as well as for smaller, more easily achievable changes in habitual intakes for those who wish to follow this diet. To our knowledge, this is the first study evaluating the relative merit of the individual components in the overall association of the MedDiet with mortality( Reference Schwingshackl, Schwedhelm and Galbete 5 ). In all, two other meta-analyses have also looked at the individual components of the MedDiet in relation to incidence of, and mortality from, CVD( Reference Grosso, Marventano and Yang 72 ) and cancer( Reference Schwingshackl, Schwedhelm and Galbete 5 ). It is difficult to compare the results of these investigations with ours owing to differences in the studies included, the end points used and the different contrasting categories used for each component. Nevertheless, the aforementioned investigations also found inverse associations for the incidence of/mortality from CVD and cancer with respect to higher intake of vegetables and fruit, and a positive association with respect to higher meat intake (albeit not statistically significant). Schwingshackl et al.( Reference Schwingshackl, Schwedhelm and Galbete 5 ) also found moderate ethanol consumption being associated with a reduction in cancer incidence/mortality. On the other hand, Grosso et al.( Reference Grosso, Marventano and Yang 72 ) found a neutral effect of alcohol on cardiovascular incidence/mortality (0·97, 95 % CI 0·88 1·07) but they have combined RR, which refer both to high v. low and moderate v. other consumptions of alcohol, and therefore their results are not directly comparable to ours.
However, some limitations should also be acknowledged. The studies included in our meta-analysis may have various sources of bias. Misclassification of consumption of the MedDiet components owing to self-reported assessment is likely in the original studies, but this would be non-differential among cohort studies where information is collected long time before mortality. Another limitation is that adherence to the MedDiet has been evaluated only at recruitment, and individual diet may change over time especially in prospective studies with long follow-up. Nevertheless, a recent study, with a substantial sample size, that used a superior design with repeated measurements of diet and examined changes in adherence to the MedDiet during a very long follow-up also showed a benefit in mortality( Reference Kouris-Blazos and Itsiopoulos 15 ).
Heterogeneity among RR associated with MDS was not negligible; however, the consistency of our findings with those reported in other meta-analyses of the MedDiet in relation to various health outcomes( Reference Dinu, Pagliai and Casini 6 ) reassures the accuracy of our results. With respect to confounding, the well-accepted risk factors for mortality were controlled for in many studies, especially the most recent ones, and we used multivariate RR adjusted for all available covariates in our meta-analyses. Finally, the estimated RR referring to the individual components of the MedDiet were based on country-specific medians, which differ across countries, although the use of random-effects models may overcome this problem up to a certain point.
In conclusion, in our systematic meta-analyses of cohort studies, we confirmed the inverse association of the MedDiet with mortality among adults and we provided evidence regarding the contribution of the components of this diet in the overall association. Although the survival benefits of the MedDiet in toto are important from a holistic and public health point of view, understanding which components most influence the protective role of this diet seems also important in order to better promote the MedDiet as a healthy dietary pattern, as well as to propose changes in the intakes of the components of this diet that can most effectively lower mortality.
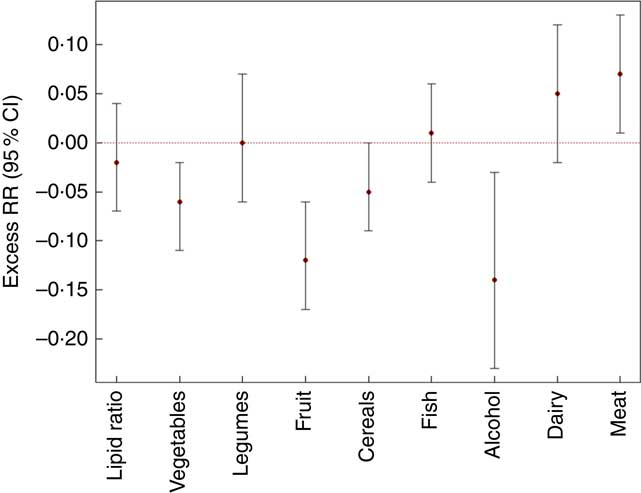
Fig. 7 Summary excess relative risk (RR) and 95 % CI of mortality associated with each of the components of the Mediterranean diet being above v. below the study-specific median intake (lipid ratio, vegetables, fruit, legumes, cereals, dairy products, meat and products, fish) or for moderate v. none/excess consumption (alcohol). The combined hazard ratio and 95 % CI were calculated using the random-effects models.
Acknowledgements
This research received no grant from any funding agency or from commercial or not-for-profit sectors.
C. B. was responsible for formulating the research questions and designing of the study. D. E., V. B. and C. B. carried out the literature search and critically reviewed the selected publications. D. E. performed the statistical analysis. D. E., V. B. and C. B. were responsible for writing the paper. D. E., V. B., A. T., C. L. V. and C. B. critically reviewed the manuscript. All authors have read and approved the final manuscript.
The authors declare that there are no conflicts of interest.