Introduction
Non-purulent skin and soft tissue infections (SSTIs), cellulitis or erysipelas, are common emergency department (ED) presentations.Reference Phoenix, Das and Joshi 1 , Reference Dong, Kelly and Oland 2 Emergency physicians must decide on the type of antibiotic, the duration of therapy, the route to administer it (either oral or intravenous), and the time to reassessment. There are studies that make the case for the use of “simple” oral antibiotics for the treatment of “uncomplicated” SSTIs.Reference Powers 3 A recent ED study found that even a single dose of broad-spectrum intravenous antibiotics prior to discharge was associated with antibiotic-associated diarrhea and Clostridium difficile infection.Reference Haran, Hayward and Skinner 4 Despite this, practice patterns are highly variable.Reference May, Harter and Yadav 5 , Reference Murray, Stiell and Wells 6 Treatment decisions have been complicated further by the increasing prevalence of community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA).Reference Wallin, Hern and Frazee 7 - Reference Moran, Krishnadasan and Gorwitz 9 There is a lack of consensus on the appropriate route of delivery of antibiotics. Disadvantages to employing the intravenous route may include cost, required repeat visits to the ED, utilization of home nursing resources to deliver intravenous antibiotics, and patient inconvenience and discomfort.
Current guidelines regarding the optimal route of antibiotic delivery are primarily based on expert opinion.Reference Stevens, Bisno and Chambers 10 - 12 Interestingly, a recent prospective cohort study found that 43% of patients were overtreated with parenteral therapy (according to the Clinical Resource Efficiency Support Team [CREST] guidelines), with the authors suggesting that many of these cases could have been managed as outpatients with oral antibiotic therapy.Reference Marwick, Broomhall and McCowan 13 Although studies have been conducted in an effort to identify predictors of admission or prolonged hospital stay,Reference Perello-Alzamora, Santos-Duran and Sanchez-Barba 14 - Reference Talan, Salhi and Moran 16 published clinical trials aiming to predict failure with oral antibiotics for SSTIs are currently lacking. In fact, a recent Cochrane systematic review on the management of cellulitis identified 25 randomized trials, but no two trials compared the same antibiotics.Reference Kilburn, Featherstone and Higgins 17 The key clinical question is: what are the risk factors that predict failure with oral antibiotics for SSTIs? In other words, when is it appropriate to select the intravenous route?
To our knowledge, no studies have specifically addressed how physicians decide when a patient is likely to fail oral antibiotic therapy (and thus require intravenous therapy). The objective of this study was to survey Canadian emergency physicians to determine how management of SSTIs is approached. Furthermore, we sought to gauge physician opinion on which factors are considered to be most important in predicting failure with oral antibiotic therapy.
Methods
Survey
Study design and population
We conducted a self-administered electronic survey of physician members of the Canadian Association of Emergency Physicians (CAEP). In addition, we surveyed physician members of the Association of Medical Microbiology and Infectious Disease Canada (AMMI; see Appendix). Residents and medical students were excluded from the survey population.
Survey content and administration
Development of the 61-question survey (see Appendix) was overseen by a researcher (IS) with extensive experience in survey design and implementation.Reference Calder, Arnason and Vaillancourt 18 - Reference Perry, Goindi and Symington 21 For the survey creation, we also sought feedback from several emergency medicine and infectious disease physicians from our institution. We conducted cognitive building exercises for generating appropriate questions. This involved meeting with individual staff physicians and asking them to suggest risk factors that they felt were important in predicting failure with oral antibiotic therapy for SSTIs. This process was repeated until question saturation was reached. Selected emergency medicine and infectious disease specialists then participated in a pilot survey to assess for content and face validity. The survey was created using SurveyMonkey software (SurveyMonkey Inc., Palo Alto, CA). The initial part of the survey was related to physician approach to the management of SSTIs. The latter portion focused on physician opinion of risk factors important in predicting failure with oral antibiotics for SSTIs, and this was assessed using a 7-point Likert scale.
A pre-notification email was sent out prior to the survey using the modified Dillman method. Non-responders were sent three and two reminders at 2-week intervals to CAEP and AMMI members, respectively.
Data analysis
Data were analysed using descriptive statistics. In addition, comparisons between the CAEP and AMMI responses were evaluated by unpaired two-tailed t-tests (see the supplementary appendix). The study was approved by the research ethics board at our institution.
Results
Overall, 391 of 1060 emergency physicians responded to the survey (a response rate of 37%). By region, the majority of respondents were from Western and Central Canada. Physician demographics are presented in Table 1.
Table 1 Demographics of the survey respondents

CAEP = Canadian Association of Emergency Physicians.
Physicians were asked what factors they considered for patients with SSTIs to help determine the need for administering at least one dose of intravenous antibiotics (Table 2). Emergency physician respondents relied heavily on both clinical impression (97.4%) and patient comorbidities (87.7%). Only a minority of physicians reports using guidelines or classification tools in their decision-making.
Table 2 Factors physicians consider to determine whether to give IV antibiotics for skin and soft tissue infections (SSTIs)
CAEP=Canadian Association of Emergency Physicians; IDSA=Infectious Disease Society of America.
Results for physician approach to management of SSTIs are presented in Table 3. Cephalexin and cefazolin are the preferred oral and intravenous antibiotics to manage SSTIs, respectively. A significant proportion of emergency physician respondents suggested ceftriaxone as a first choice for parenteral therapy (18.9%). Most respondents selected 7 days of therapy with oral antibiotics. The majority of respondents suggested that 48 hours was an appropriate time to consider treatment failure with oral antibiotics (55.8%). Although most respondents indicated that they would switch to parenteral therapy in the event of treatment failure with oral antibiotics, 13% of respondents indicated that they would select another oral antibiotic rather than switch to parenteral therapy. There was a lack of clear consensus for the appropriate time to reassess patients following the first dose of intravenous antibiotics; 44% of emergency physician respondents favored reassessment at 24 hours. Finally, emergency physician respondents were asked to identify the most common setting for subsequent intravenous antibiotic doses. Although the majority indicated a return to the ED (40.9%), there were significant responses indicating home or community administration (36.6%) or an infectious disease clinic (16.4%).
Table 3 Approach to management of skin and soft tissue infections (SSTIs)

CAEP = Canadian Association of Emergency Physicians; ED = emergency department; ID = infectious disease; IV = intravenous.
Of emergency physician respondents, 94.4% indicated that they would consider employing a clinical decision rule to predict failure with oral antibiotics for SSTIs. The majority of respondents who indicated that they would use a clinical decision rule felt that a 10% or 5% miss rate would be acceptable (Figure 1).

Figure 1 Acceptable Miss Rate for a Proposed Clinical Decision Rule According to CAEP Physician Respondents
Individual risk factors were defined as high risk for treatment failure if the median score was 6 or 7 (out of 7). Of 42 potential risk factors, emergency physicians endorsed 14 risk factors as high risk for predicting treatment failure (Figure 2). Six risk factors (immune compromise, poorly controlled diabetes mellitus, indwelling peripheral intravenous line at the infection site, elevated venous lactate, tachypnea, and cat bite) were not considered to be high risk by the infectious disease specialists (AMMI) group.
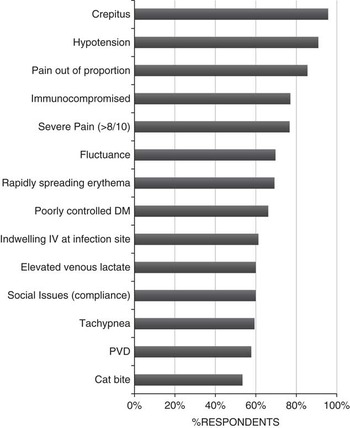
Figure 2 CAEP Respondents Endorsing Risk Factors for Oral Antibiotic Treatment Failure (Median Score ≥6/7) CAEP=Canadian Association of Emergency Physicians
Discussion
Following the participation of 391 emergency physicians and 72 infectious disease specialists, our survey showed a clear lack of consensus for the approach to management of SSTIs. Although the majority of emergency physician respondents rely on clinical impression and comorbidities to guide the decision to treat with parenteral therapy, there is significant variability concerning important management decisions for SSTIs amongst emergency physician respondents. Examples include optimal time to clinical reassessment following oral and intravenous therapy, duration of therapy with oral antibiotics, and the time point at which treatment failure with oral therapy should be considered. Furthermore, the respondents have endorsed many risk factors felt to predict failure with oral antibiotics for SSTIs. Of these risk factors, items such as the patient reporting severe pain, poor compliance due to social issues, and tachypnea are likely not considered by a majority of physicians when considering potential treatment failure with oral antibiotics. A recent study by Peterson et al. identified five risk factors that were independently associated with treatment failure, although the authors did not discriminate between oral and parenteral therapies.Reference Peterson, McLeod and Woolfrey 22 An overwhelming majority of emergency physicians indicated that they would use a clinical decision rule to predict failure with oral antibiotics, and most respondents would accept a 10% or 5% miss rate. Although attempts to derive a clinical decision rule to predict the need for admission for patients with SSTIs have been unsuccessful to date,Reference Sabbaj, Jensen and Browning 23 no studies have attempted to derive a decision rule to predict failure with oral antibiotic therapy. This study has demonstrated that there is a lack of consensus regarding the approach to managing non-purulent SSTIs and has identified several risk factors felt to predict treatment failure, which merit further investigation to improve physician approach to this common clinical presentation.
To our knowledge, this survey is the first to assess how Canadian emergency physicians manage patients with SSTIs, and the first to gauge emergency physician opinion on which risk factors are felt to predict treatment failure with oral antibiotics. Furthermore, emergency clinicians identified several perceived “high risk” factors for treatment failure with oral antibiotic therapy. This study has ultimately shown that there lacks agreement on how to best manage this common clinical problem, and that perhaps we should consider specific risk factors when determining the appropriate route of antibiotic therapy.
This study has several potential limitations. One limitation is that members of CAEP may not be fully representative of emergency physicians, reflecting a sampling bias. However, this group is the only national Canadian organization of emergency physicians that is also involved in the development of practice guidelines. There is also the chance that the responses of non-responders may have differed significantly from those who did participate in the survey (non-response bias). Physician approach to management of non-purulent SSTIs may be affected by variations in local resistance patterns and rates of MRSA. Finally, the comparison of physician groups (see the supplementary appendix) may be open to criticism, as one might argue that each group sees a different disease spectrum concerning SSTIs.
Our findings reveal important clinical implications, having demonstrated a scarcity of existing evidence combined with a lack of consensus on the optimal approach to managing SSTIs. Furthermore, respondents have highlighted several risk factors felt to predict treatment failure with oral therapy. We feel that many of these identified risk factors may not be considered by a majority of emergency physicians when deciding on oral versus parenteral therapy. Ultimately, our findings strengthen the argument for further investigations regarding the management of SSTIs.
The survey demonstrates significant variability regarding physician management of SSTIs, and we have identified several perceived risk factors for treatment failure with oral antibiotics that should be assessed in future studies.
Acknowledgements: The authors would like to thank Angela Marcantonio, My-Linh Tran, and Risa Shorr for their assistance in this study.
Competing interests: None declared.
Supplementary materials
For supplementary material/s referred to in this article, please visit http://dx.doi.org/doi:10.1017/cem.2016.347







