CASE
A 21-year-old male with known type 1 diabetes mellitus presented to the emergency department (ED) with two days of vomiting, polyuria, and polydipsia after several days of viral upper respiratory tract infection symptoms. Since his symptom onset, his home capillary blood glucose readings have been higher than usual. On the day of presentation, his glucometer read “high,” and he could not tolerate oral fluids. On examination, his pulse was 110 beats/minute, and his respiratory rate was 24 breaths/minute. He was afebrile, and the remaining vital signs were normal. Other than dry mucous membranes, his cardiopulmonary, abdominal, and neurologic exams were unremarkable. Venous blood gas demonstrated a pH of 7.25 mm Hg, pCO2 of 31 mm Hg, HCO3 of 13 mm Hg, anion gap of 18 mmol/L, and laboratory blood glucose of 40 mmol/L, as well as serum ketones measuring “large.”
CLINICAL QUESTIONS
- 1.
What is the epidemiology of diabetic ketoacidosis?
Diabetic ketoacidosis usually occurs in individuals with type 1 diabetes mellitus, although it can occur in type 2 diabetes mellitus. Its incidence is estimated to be 4.6–8.0 per 1,000 patient-years for those with type 1 diabetes mellitus and 0.32–2.0 per 1,000 patient-years for those with type 2 diabetes mellitus,Reference Goguen and Gilbert1 with even higher rates for young adults aged 18–25 years (100–120 cases per 1,000 persons).Reference Fazeli Farsani, Brodovicz and Soleymanlou2 While inpatient mortality for diabetic ketoacidosis is generally low in developed countries (<1%), recent studies have shown that mortality rates for hospitalized diabetic ketoacidosis cases in some developing countries may be as high as 30% and that 54%–76% of all type 1 diabetes mellitus-related deaths for those aged <30 years can be attributed to diabetic ketoacidosis.Reference Fazeli Farsani, Brodovicz and Soleymanlou2 Diabetic ketoacidosis and other acute hyperglycemic emergencies (e.g., hyperosmolar hyperglycemic state, which is treated similarly) tend to recur in individuals with poorly controlled diabetes mellitus, resulting in frequent, unplanned repeat ED visits (almost 20% within a 30-day period in one recent Canadian study including diabetic ketoacidosis and hyperosmolar hyperglycemic state patients).Reference Yan, Gushulak and Columbus3
- 2.
How is diabetic ketoacidosis diagnosed? Can diabetic ketoacidosis present with normal blood glucose?
As the diagnostic criteria for diabetic ketoacidosis are not well defined, it is important to keep a high index of suspicion.Reference Goguen and Gilbert1 Serum pH and bicarbonate are usually low (≤7.30 and ≤15.0 mmol/L, respectively), and serum or urine ketones are positive. Typically, the anion gap is elevated (>12 mmol/L), serum ketones or beta-hydroxybutyrate are present, and serum blood glucose is increased (>11 mmol/L); however, normal blood glucose does not preclude the diagnosis of diabetic ketoacidosis as euglycemic diabetic ketoacidosis may occur in specific instances (e.g., pregnancy, sodium-glucose co-transporter 2 inhibitor use, food restriction, and alcohol use).Reference Peters, Buschur and Buse4 Furthermore, negative urine ketones should not be used to rule out diabetic ketoacidosis, as urine tests measure the presence of acetoacetate, but not beta-hydroxybutyrate.
- 3.
What are potential precipitants of diabetic ketoacidosis?
The “five I's” are often used as a mnemonic to remember potential diabetic ketoacidosis precipitants: infection, ischemia (e.g., myocardial, cerebral, and mesenteric), insulin omission, intoxication (e.g., alcohol and sympathomimetics), and iatrogenic (e.g., drugs or dextrose-containing infusions). Additional causes include a new diabetes mellitus diagnosis, trauma, thyrotoxicosis, and other metabolic disorders.
- 4.
What investigations should be ordered for this patient?
For patients with suspected diabetic ketoacidosis, the following bloodwork should be ordered: serum electrolytes including bicarbonate and anion gap, glucose, serum ketones or beta-hydroxybutyrate, creatinine, serum osmolality, complete blood count (CBC), venous blood gas, lactate, and beta-hCG (as appropriate). Ancillary tests to investigate precipitants of diabetic ketoacidosis depending on clinical suspicion include urinalysis, electrocardiogram, urine and/or blood cultures, imaging (e.g., chest x-ray and neuroimaging), and cardiac troponin.
- 5.
What treatment should be initiated?
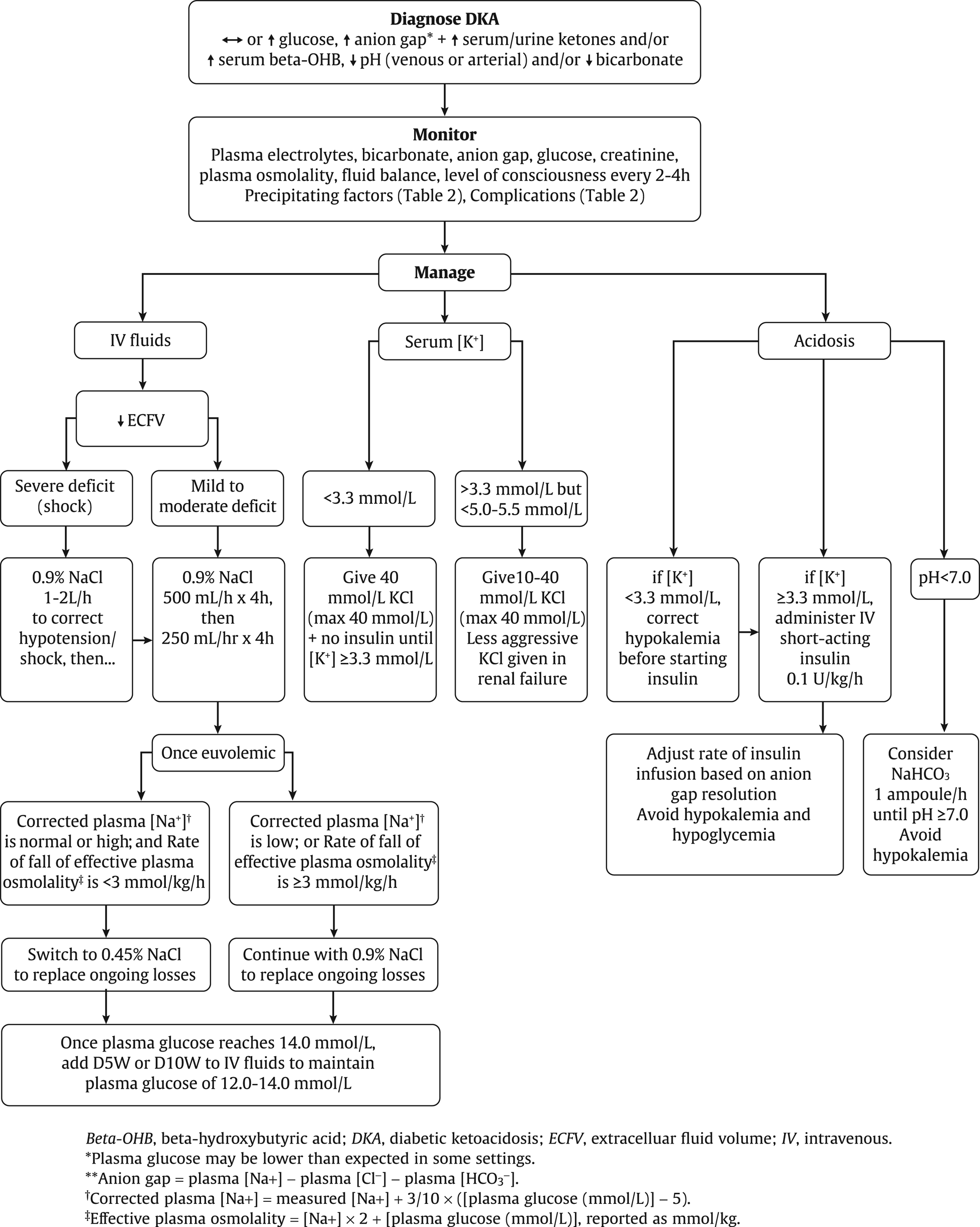
In addition to symptomatic management and treatment of the underlying precipitant, the goals of initial diabetic ketoacidosis treatment are to: 1) correct fluid deficits; 2) replace potassium; and 3) treat acidosis and hyperglycemia. Hypotension/hypovolemic shock is treated with aggressive fluid resuscitation (1–2 L/h until shock is corrected); for non-shock patients, intravenous (IV) normal saline boluses of 500 mL/h should be initiated and may be repeated until euvolemic (usually for at least four hours) and then continued at 250 mL/h for four hours. If serum potassium is <3.3 mmol/L, 40 mmol/L of potassium chloride should be administered, and insulin should be withheld until levels are ≥3.3 mmol/L; if serum potassium is normal, 10–40 mmol/L potassium chloride should be given in the IV fluid. If the patient is hyperkalemic, potassium should be withheld until less than 5.0–5.5 mmol/L and diuresis occurs. Potassium chloride should also be administered less aggressively to those with renal failure. IV short-acting insulin therapy should begin at 0.1 units/kg/hour and adjusted based on the anion gap resolution while avoiding hypoglycemia or hypokalemia. Because of limited evidence, insulin boluses are no longer recommended. Sodium bicarbonate is not routinely recommended but may be considered for cases with severe acidemia (serum pH <7.0) or shock. For ongoing care, point-of-care glucose should be checked hourly, electrolytes and blood gases checked every 2–4 hours, and insulin should be continued until acidosis and anion gap resolve. For further reference, the 2018 Clinical Practice Guidelines can be found in Figure 1.Reference Goguen and Gilbert1
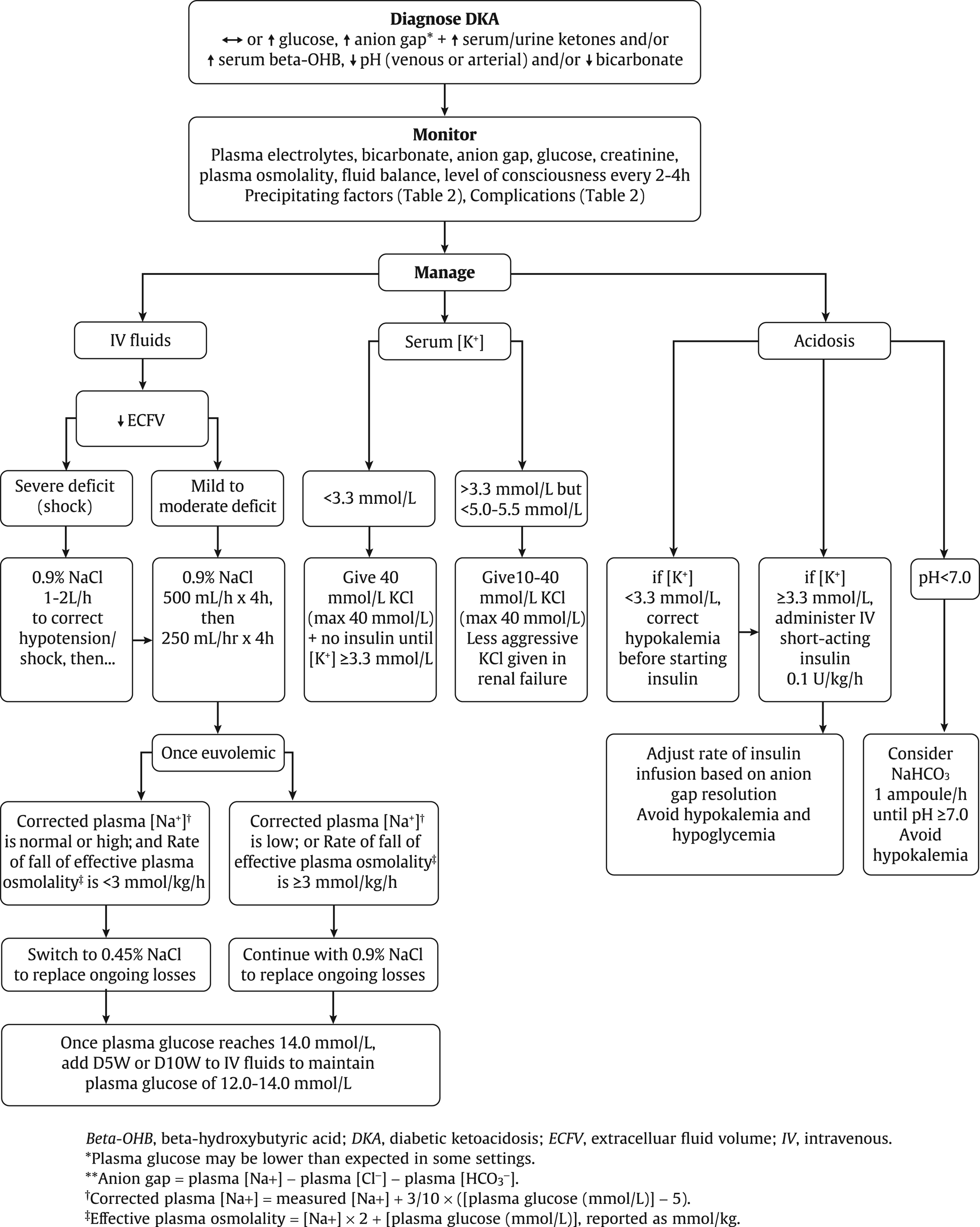
Figure 1. Management of diabetic ketoacidosis in adults.
From: Goguen J, et al. Hyperglycemic emergencies in adults: 2018 Clinical Practice Guidelines. Canadian Journal of Diabetes, 42:S109-S114. [Used with permission]
- 6.
What factors might predict adverse outcomes in ED patients presenting with hyperglycemia, diabetic ketoacidosis, and hyperosmolar hyperglycemic state?
A recent systematic review of eight observational studies (96,970 patients) identified factors associated with adverse outcomes (unplanned return ED visit, hospital admission, or death) involving ED patients presenting with hyperglycemia.Reference Siddiqi, Van Aarsen, Iansavitchene and Yan5 Risk factors included age, lowest income quintile, urban dwellers, presence of comorbidities, coexisting hyperlactatemia, having a family physician, elevated serum creatinine, on insulin, ED hyperglycemia visit in the past month, and high blood glucose level on presentation. Systolic blood pressure of 90–150 mm Hg and tachycardia were protective. However, this review highlighted that there are few high-quality studies examining hyperglycemia in ED, particularly in Canada. Furthermore, limited conclusions can be drawn as studies were retrospective (thus, prone to bias), focused on selected patient populations, or were not able to quantify the risk of adverse outcomes.
CASE RESOLUTION
The patient was treated with IV normal saline boluses and given symptomatic management for his vomiting. After confirming a normal serum potassium level (4.8 mmol/L), IV insulin at 0.1 units/kg/h was started. The patient was admitted for ongoing therapy and serial monitoring of glucose, blood gases, and electrolytes. Ancillary tests including electrocardiogram, chest x-ray, urine and blood cultures, and troponin were all negative. The patient was discharged home two days later in good condition, with follow-up arranged at the Diabetes Education Centre.
KEY POINTS
• Diabetic ketoacidosis is a common complication of diabetes and is associated with significant patient morbidity and mortality.
• The classic presentation of diabetic ketoacidosis includes hyperglycemia, positive serum/urine ketones, and acidemia. However, clinicians should be aware of euglycemic diabetic ketoacidosis as a less common presentation in specific instances (e.g., pregnancy, sodium-glucose co-transporter 2 inhibitor use, food restriction, and alcohol use).
• Patients with suspected diabetic ketoacidosis should be investigated with tests that not only confirm the diagnosis but also search for common precipitants including the “five I's.”
• Treatment of diabetic ketoacidosis includes IV fluids, potassium replacement, insulin infusion, and treating precipitants.
• Risk factors and protective factors for adverse outcomes should be considered while dispositioning ED patients with hyperglycemia.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/cem.2019.428.
Acknowledgements
The authors wish to acknowledge Kristine Van Aarsen, Dimah Azzam, Debra Eagles, Krishan Yadav, and Robert Ohle for their contributions to the writing of and critical review and feedback provided for this manuscript.
Competing interests
None to declare.