Many people with schizophrenia continue to experience disabling residual and remitted symptoms, impaired functioning and high relapse rates in community care. Practice guidelines Reference Lehman, Lieberman, Dixon, McGlashan, Miller and Perkins1,2 and systematic reviews Reference Rummel-Kluge and Kissling3,Reference Xia, Merinder and Belqamwar4 recommend that psychoeducation in either an individual or group format, on a fortnightly to monthly basis, should be offered to patients with schizophrenia as it is consistently effective in reducing relapse and encouraging adherence to medication. However, as with other models of psychosocial intervention, the effects of psychoeducation on patients’ awareness of and insight into their schizophrenia and other functional outcomes over the longer term are inconclusive. Reference Xia, Merinder and Belqamwar4 This may be because these interventions focused less attention on awareness of and insight into mental illness or its symptoms, and offer limited strategies for motivating and self-empowering patients in their illness management. Reference Rummel-Kluge and Kissling3-Reference Chadwick, Hughes, Russell, Russell and Daqnan5 Other methodological limitations of studies of psychosocial interventions include few multisite trials with diverse health outcomes, small sample sizes and high attrition rates. Reference Bäuml, Froböse, Kraemer, Rentrop and Pitschel-Walz6 Mindfulness-based stress reduction programmes aim, through meditation and discussion, to change patients’ relationships with thoughts and negative feelings - they can experience how mindful observation and acceptance of their illness is empowering and calming. Reference Chadwick, Hughes, Russell, Russell and Daqnan5,Reference Chien and Lee7 These fortnightly ten-session programmes have been shown to empower patients’ personal care, symptom management and control over distressing thoughts in severe depression and anxiety. Reference Ma and Teasdale8 Although a widespread perception, emanating from case studies, exists that mindfulness practices can elicit harmful reactions in individuals with acute psychosis, such as intense suffering from increased awareness of their illness condition, Reference Freeman, Garety, Kuipers, Fowler and Bebbington9 two recent feasibility trials have indicated its benefits for patients with psychosis. Reference Chadwick, Hughes, Russell, Russell and Daqnan5,Reference Chien and Lee7 Our study aimed to evaluate the effect of mindfulness-based psychoeducation on mental state, rate of readmission to hospital, insight into illness, social support and functioning over a 24-month follow-up of Chinese patients with schizophrenia when compared with those receiving either conventional psychoeducation or usual care.
Method
The study was a multicentre randomised controlled trial with a repeated-measures design to compare the intervention outcomes in three groups of patients with schizophrenia (ClinicalTrials.gov: trial registration NCT01667601). The study was undertaken in Hong Kong between August 2010 and March 2013. Analysis of data was on an intention-to-treat basis and all participants were followed up over 24 months, irrespective of whether the intervention was completed or not.
Participants and study settings
Of approximately 1085 eligible patients with schizophrenia (15% of this patient population) attending three out-patient clinics in the largest geographical region (New Territories) of Hong Kong, 515 (48%) were successfully contacted. Of these, 450 (87%) agreed to participate and 107 (24%) were then randomly selected. Chinese out-patients with schizophrenia from the three clinics were eligible to participate if they: (a) had a diagnosis of schizophrenia according to DSM-IV criteria; 10 (b) had a history of ⩽5 years of illness at recruitment; (c) were aged 18 years or over; and (d) were able to understand Chinese/Mandarin. Patients were excluded if there was comorbidity with another mental illness such as affective and organic brain disorders. From each clinic, those eligible patients who agreed to participate were listed in alphabetical order and then selected randomly from the list (n = 35-36 per clinic), using a computer-generated random numbers table.
Sample size was estimated on the basis of previous clinical trials of psychoeducation for Chinese patients with schizophrenia, in which symptom severity and relapse rate were the main outcomes. Reference Chien and Lee7,Reference Chan, Yip, Tso, Cheng and Tam11,Reference Li and Arthur12 Sample size calculation indicated that 108 participants (n = 36 per group) were required to detect any statistically significant differences in psychiatric symptom severity and rates of readmission to hospital between three groups with effect sizes of 0.50 and 0.48 respectively, an alpha of 0.05 and a power of 0.80, allowing for 20% potential attrition. Reference Stevens13 With informed written consent and baseline measurement taken at recruitment, 107 patients were randomly assigned to either mindfulness-based psychoeducation (n = 36), conventional psychoeducation (n = 36) or usual care (n = 35, 1 withdrew before the intervention). Another 65 patients were approached but refused because of a lack of interest in participating (n = 28), an unwillingness to be known as having a mental illness (n = 20) and/or an inconvenient time for group meetings (n = 17).
Procedure
This trial was approved by the Human Subject Research Ethics Committee of the university and the study clinics and a flow diagram summarises the study procedures according to the revised version of the CONSORT statement (Fig. 1). Reference Schultz, Altman and Moher14 After giving their written consent, patients were asked to draw a sealed opaque envelope, in which a labelled number card indicated the group to which they were assigned. An independent trained research nurse performed the outcome measurements using a set of questionnaires before treatment allocation (Time 1), at 1 week (Time 2), 12 months (Time 3) and 24 months (Time 4) following the 6-month interventions. Both the assessor and clinic staff were masked to treatment allocation.
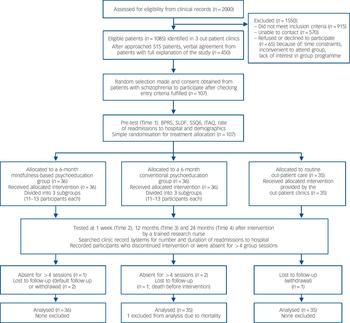
Fig. 1 Flow diagram of clinical trial for psychoeducation and usual care groups.
BPRS, Brief Psychiatric Rating Scale; SLOF, Specific Levels of Functioning Scale; SSQ6, 6-item Social Support Questionnaire; ITAQ, Insight and Treatment Attitudes Questionnaire.
Measures
At Times 1-4, the research nurse asked the participants to complete four questionnaires: the Brief Psychiatric Rating Scale (BPRS), Reference Overall and Gorham15 Specific Levels of Functioning Scale (SLOF), Reference Schneider and Struening16 6-item Social Support Questionnaire (SSQ6) Reference Sarason, Sarason, Shearin and Pierce17 and Insight and Treatment Attitudes Questionnaire (ITAQ). Reference McEvoy, Apperson, Appelbaum, Ortlip, Brecosky and Hammill18 Frequency and duration of readmissions to psychiatric hospital over the previous 6 or 12 months at Times 1-4 were collected from clinic records.
The 18-item BPRS has been used globally in clinical assessment and research to assess the severity of psychiatric symptoms. Reference Overall and Gorham15 Items were rated on a seven-point Likert scale (0, not assessed; 1, not present; 6, extremely severe). The BPRS indicated satisfactory content validity, interrater reliability (intraclass correlation (ICC) = 0.89), and internal consistency (Cronbach’s α = 0.85) in Chinese patients with psychosis. Reference Chien, Chan and Thompson19
The 43-item SLOF measures the levels of patients’ psychosocial functioning and comprises three functional domains for patients with schizophrenia: self-maintenance (12 items); social functioning (14 items); and community living skills (17 items). Reference Schneider and Struening16 The Chinese version used in this study showed satisfactory content validity, test-retest reliability (Pearson’s r = 0.79), and internal consistency (Cronbach’s α = 0.90-0.96 for subscales) in Chinese patients with schizophrenia. Reference Li and Arthur12,Reference Chien, Chan and Thompson19
The SSQ6 was used to measure each patient’s satisfaction with the social support available in his/her immediate social environment. Reference Sarason, Sarason, Shearin and Pierce17 The items are rated on a six-point Likert scale, with a higher total score (range 0-6) indicating more satisfaction with the available social support. The translated Chinese version indicated satisfactory content validity and internal consistency (Cronbach’s α = 0.89-0.93) in Chinese patients with psychosis. Reference Chan, Yip, Tso, Cheng and Tam11,Reference Chien, Chan and Thompson19
The 11-item ITAQ Reference McEvoy, Apperson, Appelbaum, Ortlip, Brecosky and Hammill18 measures patients’ awareness of and insight into illness and need for treatment in schizophrenia. Its items are rated on a three-point Likert scale (0, no insight; 1, partial insight; and 2, good insight). The higher the score, the better is the patient’s insight regarding recognition of illness-related problems and willingness to receive treatment. The Chinese version indicated satisfactory internal consistency (Cronbach’s α = 0.82), interrater reliability (ICC = 0.82) and correlation (Pearson’s r = 0.56 and 0.60, P = 0.001) for symptom severity and psychopathology. Reference Chien and Leung20
Patients’ demographic and clinical data (for example age, gender, education and duration of illness) were also collected at baseline. Dosages of antipsychotic medication examined from patients’ out-patient progress sheets were converted into haloperidol equivalents for comparison. Reference Bezchlibnyk-Butler, Jeffries and Virani21
Mindfulness-based psychoeducation programme
Participants (n = 36) received 12 fortnightly, 2 h sessions of the mindfulness-based psychoeducation programme (MBPP group) (i.e. over 24 weeks), with 11-13 patients per group, in addition to usual psychiatric out-patient care (as described below). The programme was developed in accordance with recent psychoeducation programmes. Reference Chan, Yip, Tso, Cheng and Tam11,Reference Kreyenbuhl, Buchanan, Dickerson and Dixon22 as well as a mindfulness-based stress reduction programme tested in Chinese patients with depression. Reference Ma and Teasdale8 One nurse therapist led and facilitated patients to become more aware of and relate differently to their thoughts, feelings and sensations such as hallucinations and delusions, rather than identifying with them as accurate readouts on reality. The programme consisted of seven components in three phases (see online supplement):
-
(a) phase 1: orientation and engagement, empowerment and focused awareness of experiences, bodily sensations/thoughts and guided awareness exercises and homework practices;
-
(b) phase 2: education about schizophrenia care, intentionally exploring and dealing with difficulties regarding symptoms and problem-solving practices; and
-
(c) phase 3: behavioural rehearsals of relapse prevention strategies, accessible community support resources and future plans.
Individual participants were requested to regularly (daily) practice intentional and focused awareness of body sensations, thoughts and feelings and mindful walking in the early phases, and in later stages, select self-empowering and constructive perspectives for working with negative/distressing thoughts and feelings.
As mindfulness training served to increase patients’ acceptance and management of their individual thoughts and emotional responses within their cultural context, the programme adopted a few strategies to address traditional Chinese cultural tenets. For instance, the first phase focused on understanding strong interdependence and inviting more mutual support and problem-solving among group members. In the second/third phases, patients were encouraged to cultivate an open, accepting mode of their responses to problems/stimuli and develop a ‘decentred’ attitude (recognising that the established beliefs and practices constitute only one of several possible interpretations) on their thoughts/feelings. Reference Ma and Teasdale8 Resolution around strong self-centeredness (for example, saving face and reconstruction of self-image) was reinforced.
Conventional psychoeducation programme
In addition to usual out-patient care, participants in the conventional psychoeducation programme group (CPEP group, n = 36) received a 6-month programme of conventional psychological support and education conducted by a trained psychiatric nurse experienced in leading psychiatric rehabilitation and education groups. Similar to the mindfulness-based psychoeducation programme, this group programme consisted of 12 fortnightly, 2 h sessions (11-13 participants per group). Its content was modified from other similar programmes Reference Chien and Leung20,Reference Macpherson, Jerrom and Hughes23 and comprised four stages: engaging and empowering individual patients (two sessions on orientation and engagement of participants and discussion about goals); education and survival skills workshop (four sessions covering basic facts on schizophrenia and stressful life situations and coping strategies); preventing relapse through problem-solving training (four sessions); and evaluation of knowledge and skills learnt, and preparation for the future (two sessions).
The psychiatric nurses in both the psychoeducation programmes were trained by the research team and a psychotherapist with a 3-day workshop and supervised practice within all group sessions. Progress monitoring of the two programmes was conducted between group sessions and consisted of regular reviews of audiotapes of each session by the research team, together with the nurse therapists, and clarification of any problems encountered.
Usual out-patient care
Participants in the usual care group (n = 35) received usual psychiatric out-patient services, which were similar across the three clinics. These services included monthly medical consultation and treatment by psychiatrists, advice and brief education on medication and community care services by psychiatric nurses, social welfare and financial assistance by medical social workers, and individual and family counselling by clinical psychologists whenever necessary.
Data analyses
All quantitative data collected were analysed on an intention-to-treat basis using SPSS version 19.0 for Windows. Differences in demographic characteristics and the outcome measures (BPRS, SLOF, SSQ6, ITAQ and readmission to hospital rates) at Time 1 between the three study groups and between the three clinics under study within each of the three groups were assessed by analysis of variance (ANOVA) or the Kruskal-Wallis test (H statistic) as appropriate. Without any violation of assumptions of normality, linearity and homogeneity of variance-covariance and multicollinearity, Reference Stevens13 multivariate analysis of variance (MANOVA) was performed for the dependent (outcome) variables to determine the treatment effects over time (group×time interactive effects), followed by univariate analyses (repeated-measures ANOVA) of the variables if the MANOVA test results were significant. Bonferroni’s multistage procedure was used to adjust the significance level for the multiple ANOVA analyses (adjusted P = 0.01). Reference Tabachnick and Fidell24 The Helmert contrast codes were set to test any significant differences between groups on those measures that indicated a significant interactive effect of time×group in the repeated-measures ANOVA tests. Reference Stevens13 Except for the repeated-measures ANOVA test, the level of statistical significance was set at 0.05.
Results
Sample characteristics
Demographic and clinical characteristics of the three study groups and non-participants were similar (Table 1, see online Table DS1 for a more detailed version of this table), with no statistically significant differences (P>0.15). More than half of the patients (56-60%) were taking medium dosages of oral or intramuscular antipsychotic medications (haloperidol equivalent mean values Reference Bezchlibnyk-Butler, Jeffries and Virani21 were between 8.5 mg/day (s.d.= 5.1) and 11.3 mg/day (s.d.= 6.3)). The mean duration of the illness was 2.6 years (range 3-60 months).
Table 1 Sociodemographic characteristics of patients receiving the mindfulness-based psychoeducation programme (MBPP), the conventional psychoeducation programme (CPEP) or usual care and non-participants at baseline measurementFootnote a
| Group | ||||||
|---|---|---|---|---|---|---|
| Characteristics | MBPP (n = 36) |
CPEP (n = 36) |
Usual care (n = 35) |
Non-participants (n = 343) |
Test valueFootnote b |
P |
| Gender, n (%) | 1.21 | 0.34 | ||||
| Male | 20 (55.6) | 21 (58.3) | 20 (57.1) | 198 (57.7) | ||
| Female | 16 (44.4) | 15 (41.7) | 15 (42.9) | 145 (42.3) | ||
| Age, mean (s.d.) | 25.1 (6.8) | 25.8 (7.9) | 26.0 (8.5) | 25.9 (12.8) | 1.58 | 0.16 |
| Education level, n (%) | 1.38 | 0.19 | ||||
| Primary school or below | 8 (22.2) | 8 (22.2) | 8 (22.9) | 75 (21.9) | ||
| Secondary school | 20 (55.6) | 19 (52.8) | 19 (54.3) | 185 (53.9) | ||
| University or above | 8 (22.2) | 9 (25.0) | 8 (22.9) | 83 (24.2) | ||
| Monthly household income, HK$Footnote c : mean (s.d.) | 13 240 (1714) | 13 010 (1805) | 12 805 (1980) | 13 345 (2965) | 1.45 | 0.15 |
| Duration of illness, years: mean (s.d.) | 2.6 (1.7) | 2.5 (1.8) | 2.7 (1.8) | 2.5 (2.1) | 1.32 | 0.26 |
| Number of family members living with patient, n (%) | 1.10 | 0.38 | ||||
| 0-1 | 13 (36.1) | 14 (38.9) | 13 (37.1) | 130 (37.9) | ||
| 2-3 | 18 (50.0) | 18 (50.0) | 17 (48.6) | 165 (48.1) | ||
| 4-5 | 5 (13.9) | 4 (11.1) | 5 (14.3) | 48 (14.0) | ||
| Type of medication, n (%) | 1.32 | 0.24 | ||||
| Conventional antipsychotics (e.g. haloperidol) | 9 (25.0) | 8 (22.2) | 8 (22.9) | 76 (22.2) | ||
| Atypical antipsychotics (e.g. risperidone) | 17 (47.2) | 18 (50.0) | 16 (45.7) | 170 (49.6) | ||
| Antidepressants (e.g. fluoxetine) | 5 (13.8) | 4 (11.1) | 4 (11.4) | 40 (11.7) | ||
| Blended modeFootnote d | 5 (13.8) | 6 (16.7) | 7 (20.0) | 57 (16.6) | ||
| Dosage of medication,Footnote e n (%) | 1.18 | 0.32 | ||||
| High | 9 (25.0) | 10 (27.8) | 9 (25.7) | 83 (24.2) | ||
| Medium | 20 (55.6) | 20 (55.6) | 21 (60.0) | 198 (57.7) | ||
| Low | 7 (19.4) | 6 (16.7) | 5 (14.3) | 62 (18.1) | ||
a. See online Table DS1 for a more detailed version of this table.
b. Analysis of variance (F-test, d.f. = 448) or the Kruskal-Wallis test by ranks (H statistic, d.f. = 3) was used to compare the sociodemographic variables of patients among the three study groups and the non-participants.
c. US$1 = HK$7.8.
d. Patients were taking more than one type of psychotropic medication such as the use of either conventional and atypical antipsychotic or atypical antipsychotic together with one antidepressant.
e. Dosage levels of antipsychotic medication were compared with the average dosage of medication taken by schizophrenic patients in haloperidol-equivalent mean values. Reference Chien, Chan and Thompson19
Three participants (8.3%) in each of the MBPP and CPEP groups and one (2.9%) in the usual care group either dropped out or were absent for more than 4 of the 12 group sessions. Reasons were similar, including lack of time/interest to attend, unstable mental state, and/or limited family encouragement and support. One CPEP participant died before the intervention and their data were excluded from the outcome analysis.
Homogeneity of study groups
There were no statistically significant differences in the amount and types of atypical v. conventional antipsychotics at Times 1-4 (ANOVA or χ2 tests, P>0.10) between the three groups (Table 1) nor in the baseline mean scores of the outcome measures (F(5,104) = 1.35, P>0.20) and between the three clinics within each of the study groups (H statistic: 1.2-1.8, P>0.1), or significant correlations (r<0.20) between demographic characteristics and all of the outcome measures (BPRS, SLOF, SSQ6, ITAQ and frequency and duration of readmissions to hospital), indicating no covariate effects.
Effects of interventions
The multivariate analysis of the dependent variables (group×time) indicated a statistically significant difference between the three groups, F(5,104) = 5.98, P= 0.001 (Wilks’ λ= 0.92, partial η2 = 0.28). With this significant multivariate test result, repeated-measures ANOVAs of each of the outcome variables were performed. Results (Table 2 and Fig. 2) indicated that there were statistically significant differences between the three groups: a reduction in the BPRS score (F(2,104) = 4.36, P<0.005) and duration of readmissions to hospital (F(2,104) = 4.80, P<0.004), and an increase in the SLOF (F(2,104) = 4.98, P<0.004) and ITAQ scores (F(2,104) = 6.52, P<0.001) using a Bonferroni adjusted alpha level of 0.01. An examination of the adjusted mean scores at Times 1-4 (Fig. 2) indicated that the MBPP group reported more consistently positive improvements in ITAQ, SLOF and BPRS scores and duration of readmissions to hospital than the CPEP group. The usual care group reported mainly progressive mild negative changes of scores in all outcomes over the 2-year follow-up and a significant reduction in the SLOF and BPRS scores at Time 3.

Fig. 2 Mean scores of study outcomes at baseline (Time 1) to 24-month follow-up (Time 4).
Mean scores on the (a) Insight and Treatment Attitudes Questionnaire (ITAQ); (b) Specific Levels of Functioning Scale (SLOF); (c) Brief Psychiatric Rating Scale (BPRS); (d) Six-item Social Support Questionnaire (SSQ6); (e) number of readmissions to hospital; (f) duration of readmissions to hospitals (days). Mindfulness-based psychoeducation programme (MBPP) group (n = 36); conventional psychoeducation programme (CPEP) group (n = 35); routine care group (n = 35). Time 2, 1-week follow-up; Time 3, 12-month follow-up.
Table 2 Outcome measure scores at Times 1-4 and results of MANOVA (group×time) for the three study groups
| Group, mean (s.d.) | Effect size (partial η) |
|||||
|---|---|---|---|---|---|---|
| Measure (range)Footnote a | MBPP (n = 36) | CPEP (n = 35)Footnote b | Usual care (n = 35) | F(2,104) | P | |
| Insight and Treatment Attitudes Questionnaire (0-33) | 6.52 | 0.001 | 0.28 | |||
| Time 1 | 14.3 (2.5) | 14.0 (2.6) | 14.5 (2.0) | |||
| Time 2 | 16.5 (2.7) | 15.8 (2.6) | 14.8 (2.9) | |||
| Time 3 | 19.9 (3.1) | 16.9 (3.1) | 15.0 (3.5) | |||
| Time 4 | 21.3 (3.3) | 16.3 (3.3) | 14.8 (3.8) | |||
| Specific Level of Functioning (43-215) | 4.98 | 0.004 | 0.19 | |||
| Time 1 | 138.1 (13.8) | 135.9 (18.3) | 133.8 (16.1) | |||
| Time 2 | 155.0 (20.1) | 143.0 (20.5) | 128.8 (21.1) | |||
| Time 3 | 168.2 (20.0) | 145.5 (21.4) | 120.9 (22.3) | |||
| Time 4 | 176.9 (22.1) | 146.1 (20.4) | 119.1 (22.8) | |||
| Brief Psychiatric Rating Scale (0-108) | 4.36 | 0.005 | 0.16 | |||
| Time 1 | 30.6 (7.5) | 32.0 (6.7) | 31.6 (5.2) | |||
| Time 2 | 24.8 (6.0) | 28.9 (5.1) | 30.9 (6.8) | |||
| Time 3 | 20.1 (5.9) | 26.8 (8.1) | 34.0 (6.9) | |||
| Time 4 | 17.0 (4.9) | 28.1 (7.0) | 35.8 (7.8) | |||
| Six-item Social Support Questionnaire (0-30) | 1.98 | 0.132 | 0.05 | |||
| Time 1 | 4.0 (1.1) | 4.1 (1.1) | 4.0 (0.9) | |||
| Time 2 | 4.1 (1.3) | 4.2 (1.5) | 4.0 (1.3) | |||
| Time 3 | 3.8 (1.6) | 3.7 (1.1) | 3.6 (1.8) | |||
| Time 4 | 3.6 (1.6) | 3.9 (1.0) | 3.9 (1.5) | |||
| Number of readmissions to hospitalFootnote c | 2.78 | 0.096 | 0.09 | |||
| Time 1 | 2.8 (1.6) | 2.5 (0.9) | 2.7 (1.0) | |||
| Time 2 | 2.4 (1.3) | 2.3 (1.1) | 2.6 (1.2) | |||
| Time 3 | 2.1 (0.9) | 2.5 (1.0) | 2.9 (1.2) | |||
| Time 4 | 1.8 (1.3) | 2.3 (1.1) | 3.0 (1.3) | |||
| Duration of readmissions to hospitalFootnote d | 4.80 | 0.004 | 0.16 | |||
| Time 1 | 19.0 (4.3) | 18.5 (4.7) | 19.2 (4.1) | |||
| Time 2 | 15.7 (4.1) | 16.2 (4.1) | 19.8 (4.8) | |||
| Time 3 | 13.0 (3.6) | 16.5 (5.0) | 20.2 (5.2) | |||
| Time 4 | 11.0 (4.0) | 16.1 (6.0) | 21.0 (6.9) | |||
MBPP, mindfulness-based psychoeducation programme; CPEP, conventional psychoeducation programme; Time 1, baseline measurement at the start of intervention; Time 2, 1 week after intervention; Time 3, 12 months after intervention; Time 4, 24 months after intervention.
Results in bold are significant.
a. Possible range of scores of each scale.
b. One of the 36 participants in the CPEP group died before the intervention and was therefore excluded from data analysis.
c. Average number of readmissions to a psychiatric in-patient unit over 6 or 12 months at Times 1 to 4.
d. Average duration of readmissions to a psychiatric in-patient unit (average number of days stay) over 6 or 12 months at Times 1 to 4.
There were also significant statistical differences on the mean scores of the three SLOF subscales between the three groups at Times 2-4. (Fig. 3). The MBPP group reported significantly greater improvements in self-maintenance (F(2,104) = 4.83), social functioning, (F(2,104) = 4.28) and community living skills (F(2,104) = 4.32) and all of their P-values were <0.005 and with effect sizes (η2) of 0.17 to 0.20 (large effects). Reference Tabachnick and Fidell24
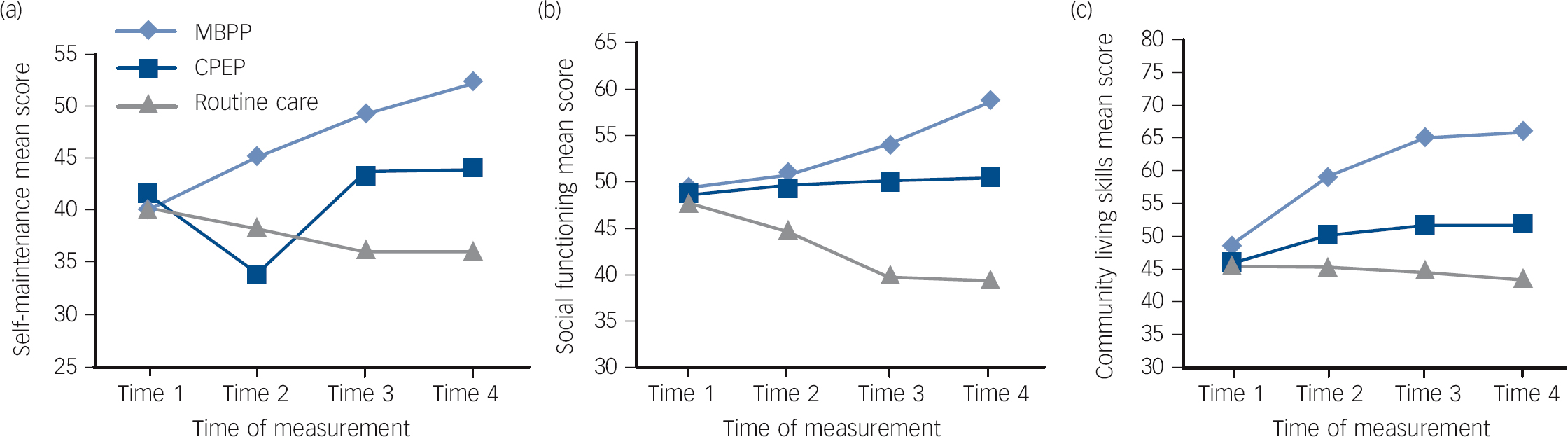
Fig. 3 Mean scores on three subscales of the Specific Level of Functioning (SLOF) scale at baseline (Time 1) to 24-month follow-up (Time 4).
(a) Self-maintenance; (b) social function; and (c) community living skills subscales. Mindfulness-based psychoeducation programme (MBPP) group (n = 36); conventional psychoeducation programme (CPEP) group (n = 35); routine care group (n = 35). Time 2, 1-week follow-up; Time 3, 12-month follow-up.
Helmert’s contrasts indicated that the mean differences between groups at two time-points on the following outcomes were significant at 0.05, and contributed to the overall multivariate significance.
-
(a) The ITAQ score of the MBPP group increased more significantly from Times 1 to 4 than in the other two groups (MBPP v. CPEP group, mean differences were 0.7, 3.0 and 5.0 (s.e. = 0.3-1.9) and MBPP v. usual care group, mean differences were 1.7, 4.9 and 6.5 (s.e. = 0.6-2.4) at Times 2-4, respectively), whereas for the CPEP group it increased slightly over time.
-
(b) The SLOF score of the MBPP group increased more significantly from Times 1 to 4 (MBPP v. CPEP group, mean differences were 12.0, 22.7 and 30.8 (s.e. = 3.0-4.9) and MBPP v. usual care group, mean differences were 26.2, 47.3 and 57.8 (s.e. = 4.8-7.6) at Times 2-4, respectively). For the CPEP group it also increased and differed significantly from the usual care group, which showed a consistent reduction over time.
-
(c) The BPRS score of the MBPP group increased more significantly from Times 1 to 4 (MBPP v. CPEP group, mean differences were 4.1, 6.7 and 11.1 (s.e. = 0.9-3.0) and MBPP v. usual care group, mean differences were 6.1, 13.9 and 18.8 (s.e. = 1.9-4.5) at Times 2-4, respectively). For the CPEP group it also increased and differed significantly from the usual care group at Times 2 to 3.
-
(d) The duration of readmissions to hospital in the MBPP group were significantly reduced from Times 1 to 4 (MBPP v. CPEP group, mean differences (days) were 0.5, 3.5 and 5.1 (s.e. = 0.2-1.8) and MBPP v. usual care group, mean differences were 4.1, 7.2 and 10.0 (s.e. = 1.2-4.9) at Times 2-4, respectively). For the CPEP group it was slightly reduced and for the usual care group it consistently increased.
There were progressive mild but non-significant reductions in medication scores among the three groups based on the converted haloperidol equivalents, Reference Bezchlibnyk-Butler, Jeffries and Virani21 from a mean of 11.8-12.1 mg/day (s.d. = 3.8-4.2) at Time 1, a mean of 10.8-11.9 mg/day (s.d. = 4.1-4.8) at Time 2, a mean of 10.6-11.7 mg/day (s.d. = 4.0-4.6) at Time 3, to a mean of 10.2-11.2 mg/day (s.d. = 4.1-4.8) at Time 4. There was also no significant difference in the types/ frequency of participation in other individual/family-based psychological treatments (two-way ANOVA, P>0.1).
Discussion
Benefits of mindfulness-based psychoeducation
The findings from this study strongly suggest that mindfulness-based psychoeducation for schizophrenia appears to be a promising approach to the treatment of this condition. A 6-month programme of this intervention, when compared with conventional psychoeducation or usual care, resulted in better patient outcomes (severity of psychiatric symptoms, level of psychosocial functioning, awareness of and insight into illness and need for treatment and duration of readmissions to hospital) at 2-year follow-up. Interestingly, there were no statistically significant differences between the three groups in terms of satisfaction with social support or frequency of readmissions to hospital. With a paucity of clinical trials reported, these findings suggest that mindfulness-based psychoeducation can be effective not only in patients with recurrent depression, Reference Ma and Teasdale8 but also in people with schizophrenia and probably other psychotic disorders. Reference Chadwick, Hughes, Russell, Russell and Daqnan5
This mindfulness-based psychoeducation programme is one of very few that has attempted to enhance awareness and acceptance among Chinese people with schizophrenia and that addresses their specific cultural needs (such as self-blame about having mental illness and interdependence among co-patients). Reference Chien and Lee7 Similar to mindfulness-based interventions in other clinical trials for depression, anxiety Reference Ma and Teasdale8,Reference Chlesa and Serretti25 and psychotic disorders, Reference Chadwick, Hughes, Russell, Russell and Daqnan5,Reference Freeman, Garety, Kuipers, Fowler and Bebbington9 this programme can enhance psychotic patients’ positive thoughts and relieve their guilty feeling towards the illness and its symptoms. Recent literature on psychiatric treatments cautions against the use of mindfulness meditation training for people with psychosis because of concerns about the potential for exacerbating psychotic symptoms during meditation practice. Reference Bäuml, Froböse, Kraemer, Rentrop and Pitschel-Walz6,Reference Chien and Lee7 Nevertheless, this clinical trial provides evidence attesting to this model of intervention improving these patients’ awareness of and insight into their illness, treatment needs and clinical functioning, supporting the findings of a feasibility trial in the UK of mindfulness groups for patients with distressing voices and paranoia. Reference Chadwick, Hughes, Russell, Russell and Daqnan5 This clinical trial also demonstrates the significant longer-term (2-year) beneficial effects of a mindfulness-based programme. Whether these improvements are a result of a combined effect of mindfulness training and psychoeducation, all of which are considered potential therapeutic factors in different current models of psychosocial intervention, Reference Rummel-Kluge and Kissling3,Reference Chan, Yip, Tso, Cheng and Tam11 remains to be answered. Thus, further research to explore the therapeutic effects of the individual active elements in the programme is recommended. In addition, there is a suggestion that it may be particularly suitable for Chinese people who are self-conscious and internalising their emotions and feelings. Reference Ma and Teasdale8 The mindfulness-based programmes adopted in this trial and a few recent studies are all highly structured and demanding for participants and include work on home assignments using practices such as self-awareness of their body, redirecting and increasing their focus on symptoms and behaviours. Reference Chadwick, Hughes, Russell, Russell and Daqnan5,Reference Ma and Teasdale8,Reference Brown, Davis, LaRocco and Strasburger26 These extensive assignments may not be easily implemented by patients with florid psychotic symptoms and an unstable mental state, or with chronic illness and negative symptoms. Therefore, the flexibility of the approach used should be studied further.
Why a mindfulness-based psychoeducation group?
Mindfulness meditation training has been found to be effective in empowering patients to manage their distressing and negative thoughts and beliefs across a range of mental and physical health conditions, as well as demonstrating an encouraging prophylactic effect on illness relapse or recurrence in depressive and anxiety disorders. Reference Ma and Teasdale8,Reference Chlesa and Serretti25 However, there are few studies reporting the usefulness of mindfulness meditation (trained voluntary deployment attention) for people with schizophrenia or psychosis to increase patients’ awareness of, and change their relationship with, unwanted thoughts, sensations and negative feelings. Our study reports similar positive outcomes to those found in all 15 participants with schizophrenia interviewed in a pilot study Reference Brown, Davis, LaRocco and Strasburger26 testing a mindfulness-based intervention to reduce anxiety: more awareness of and relief from their psychotic and other psychological symptoms, cognitive changes (such as more acceptance of and higher motivation in illness management) and a focus on the present. The findings from our trial suggest that people with schizophrenia may not be distressed by the occurrence of psychotic symptoms but by the meaning they construct and perceive, as suggested by recent qualitative studies. Reference Chadwick, Hughes, Russell, Russell and Daqnan5,Reference Freeman, Garety, Kuipers, Fowler and Bebbington9,Reference Brown, Davis, LaRocco and Strasburger26 Further study on distress and the related behaviours associated with psychotic symptoms and the meditation role of cognition in driving or combating this distress is recommended. It is also noteworthy that the confounding effects of covariants such as medication adherence and other psychotherapeutic interventions were not examined in our study, thus providing directions for future research.
Limitations of the study
Only Chinese patients were recruited from three psychiatric out-patient clinics in one geographical region in Hong Kong. Although the participants in this study were randomly selected in these three clinics, most were volunteers who may have been highly motivated to participate in the group interventions, thus resulting in very low drop-out rates. These patients, whose schizophrenia was of short duration (mean 2.6 years), might not be representative of those with long-term or chronic schizophrenia, or of those with comorbidities of other mental disorders receiving mental healthcare services. Therefore, such selective sampling should be taken into consideration when comparisons are made between this and other studies of psychoeducation programmes. Unlike the samples in some studies on psychoeducation groups, it is also important to note that more than half of patients recruited in this study were male, taking low/medium dosages of antipsychotics, living with their family, and had a high level of education. In addition, the participants were not masked to the intervention undertaken and any Hawthorne effect among the participants could not be excluded. Also the programme was time-limited to 6 months and used a less standardised format than other psychoeducation programmes; and no booster session was offered.
Implications for further research
As the first pragmatic trial designed to evaluate the effect of a mindfulness-based psychoeducation group for young Chinese people with schizophrenia, these results lend support for further evaluation of this intervention as a treatment in other populations and settings. This may necessitate tailoring the structure and content of the programme to, for example, the cultural tenets of specific patient populations and evaluating its medium- to long-term effect. An exploration of not only individual participants’ perceptions of and satisfaction with the intervention but also the group process, in terms of enablers and barriers and degree of involvement, Reference Schneider and Struening16 is essential to better understand the active ingredients of a mindfulness-based psychoeducation group.
In this study, the mindfulness-based psychoeducation programme had substantial positive effects for patients with schizophrenia in terms of psychiatric symptom severity, psychosocial functioning, awareness of and insight into illness and need for treatment and duration of readmissions to hospital. However, there were no significant effects on patients’ dosage of medication, service utilisation or perceived social support. Other longer-term benefits/outcomes used in psychoeducation studies such as improvement in global functioning, satisfaction with mental health services and quality of life warrant further investigation. Reference Xia, Merinder and Belqamwar4
Finally, in view of this intervention being shown to be effective, it will be interesting to observe whether further studies will replicate these findings and whether the intervention will be adopted more widely. There is a suggestion that it may be particularly suitable for Chinese people and we await with interest to see whether it is found to be so for other populations. Further research is needed to examine issues such as the flexibility of the approach used and whether the duration of the intervention has an impact on medication use. Therefore, it is important to investigate long-term effects, cost-effectiveness, and/or comparative effectiveness with other psychosocial interventions for schizophrenia, in larger representative samples from different socioeconomic and ethnic/ cultural backgrounds with different durations of illness and/or comorbidities of other mental disorders.
Clinical implications
This mindfulness-based psychoeducation programme, when compared with a conventional psychoeducation programme and usual psychiatric out-patient care, appeared to be an effective alternative community-based intervention for Chinese people with schizophrenia. It was found to enhance patients’ awareness of and insight into their illness and treatments and reduce the duration of their readmissions to hospitals and, similar to other psychoeducation groups, can improve patients’ symptoms and functioning. The programme can yield improvements without any increased demand for community mental health services or medication use.
Funding
This research was supported by the Central Research Fund, The Hong Kong Polytechnic University, and Health and Medical Research Fund, Hong Kong SAR, China.
Acknowledgements
Special thanks are given to the patients who participated in this study. The support and cooperation of mental health staff in the clinics under study is gratefully acknowledged.








eLetters
No eLetters have been published for this article.