Introduction
The coronavirus disease 2019 (COVID-19) pandemic has stressed the health system in such a way that it has been necessary to reorganize part of its structure, human resources, and clinical approach.Reference Klein, Cheng and Lii1 In disaster medicine, there is a widely used concept, “surge capacity,” that could be defined as the capacity of the health system to expand its response capacity to needs that exceed normal demand. The COVID-19 pandemic has affected the entire integrity of the health system, which has led to talking about surge capacity for the entire health care system. This has led to the design of out-of-hospital structures, newly built following the classic concept of the World Health Organization (WHO; Geneva, Switzerland) “field hospital,”2 or adapting civil facilities to be used as a hospital. Different guidelines define the fundamental aspects of their design and clinical operation. The US Federal Emergency Management Agency (FEMA; Washington, DC USA) developed the “Alternate Care Site [ACS] Toolkit.” These ACS are defined in the US by FEMA and the Center for Disease Control and Prevention (CDC; Atlanta, Georgia USA) as “a building or structure of opportunity that is temporarily converted for health care use during a public health emergency to provide additional health capacity and capability for an affected community, outside the walls of a traditional established health care institution.”3 Also, the WHO established recommendations for the design of temporary COVID-19 facilities4 and for the management of acute respiratory infections.5
Different types of structures were designed world-wide with different approaches regarding location (existing building or open areas) and design.Reference Candel, Canora and Zapatero6,Reference Sacchetto, Raviolo, Beltrando and Tommasoni7 The H144 Hospital of the Health Service of the Principality of Asturias, Spain (Sespa) was built in the central pavilion of an exhibition hall. Gregg S. Meyer has described three interesting models of care in relation to temporary COVID-19 hospitals:Reference Meyer, Blanchfield, Bohmer, Mountford and Vanderwagen8 (1) Acute Care Model, complex by focusing on intensive care, requiring highly specialized staff that could be needed from other intensive care units (ICUs); (2) Hospital Care Model, with a certain capacity for intensive care, wide availability of disciplines, and that tend to support an inadequate hospital network, also requiring a large number of staff in terms of their profiles; and (3) Non-Acute Care Model, for mild or recovering patients from other hospitals, allowing them to focus on moderate to severe COVID-19 patients and to increase their capacity to care for non-COVID-19 patients. This third model was adopted by the H144, and as Gregg S. Meyer points out, its strengths are low execution time and being easier to staff as it does not require high specialization, doesn’t “absorb” specialized staff from other health centers, it improves the transition of hospitals to a non-pandemic phase, and can have a positive effect on the control of epidemic outbreaks in nursing homes.Reference Bouza, Pérez-Granda and Escribano9
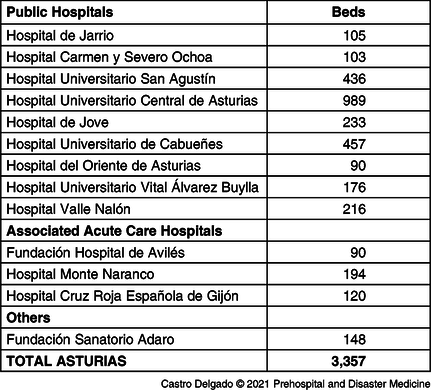
The Principality of Asturias is located in the north of Spain. It has 1,011,560 inhabitants with an elderly population and negative natural growth in recent years. The health system is organized in eight health areas, each with its reference hospital (Table 1).10
Table 1. Hospital Network of the Principality of Asturias
The aim of this article is to define the main challenges in the design, implementation, and operational aspects of ACS for COVID-19 patients following the experience of the H144 Hospital of the Health Service of the Principality of Asturias (Sespa), and describes the clinical activity during its operational time.
Report
Time Frame
Health systems managers in Asturias, on March 24, 2020, decided to create a new and temporary health facility to support the health care network in anticipation of a health care over-demand due to COVID-19 patients. The design was developed by the architect of the Health Department. On March 27, the first meeting of the medical direction with the architect took place to adapt the initial design to health care needs and organization. On March 28, the execution of the project began, ending on April 8. Medical direction approved its use to receive patients on April 9. Different fields of knowledge related to health worked on the project: medicine, nursing, hospital engineering, and hospital architecture (Figure 1). From July 1-10, the hospital was dismantled without having received patients.
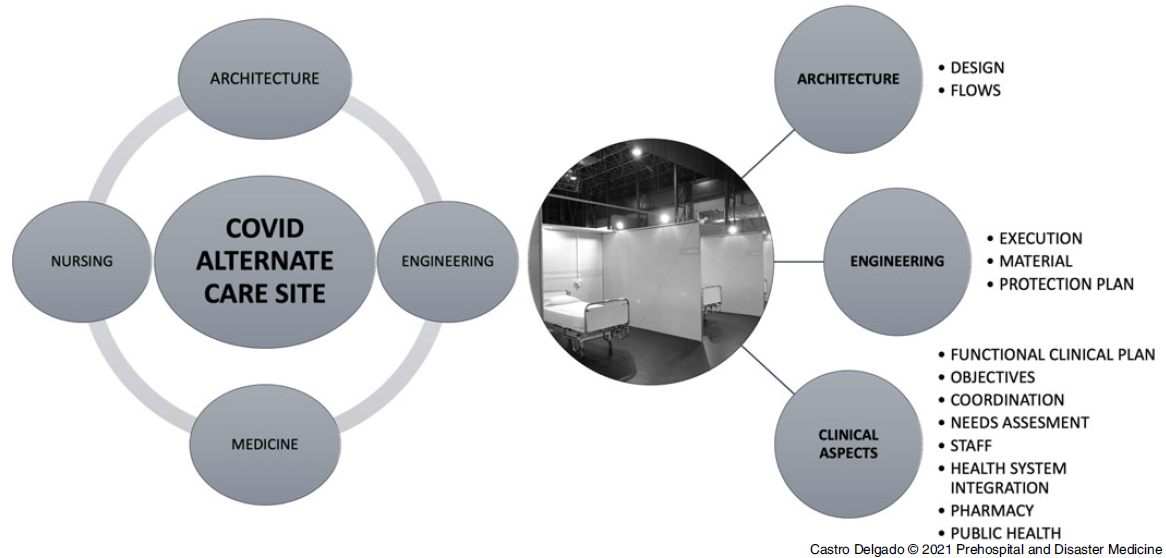
Figure 1. Different Fields of Knowledge Related to Health that Worked on the Project.
In the beginning of a second wave, the Health Department decided to replicate the model again, with slight structural improvements, and construction began again on November 4. On November 11, it was approved by the medical direction, and the first patient was received on November 12, 2020. On March 5, 2021, the last patient was discharged from H144 after 113 days of operation during the second and third wave, with 334 admitted patients and 3,149 hospital stays.
Design, Construction, and Implementation of the H144
The H144 hospital was placed in the central pavilion of Gijón Chamber of Commerce, located in the center of Gijón, Spain, with easy access control. The pavilion is an open-plan construction measuring approximately 89.70 x 58.72 meters and a height of almost 12 meters, with 5,398.78m2. A H144 management area was established in an annexed pavilion, where it was also placed the monitoring system for the hospital’s environmental conditions (humidity, temperature, and CO2). From an architectural design point of view,Reference Pernas Gali11 some aspects that were taken into consideration were: (1) the feasibility of the chosen venue; (2) adaptation of the design to an existing structure; (3) the definition of spaces and work areas; (4) coordination between design and clinical aspects; and (5) comfort for patients and workers. The execution of the work was quite a logistical challenge, especially in the first wave, where the breakdown of stocks at the international level increased efforts in searching for material and companies that could carry out the work with certain standards of hospital quality.12 Among the many aspects that affected the implementation of the project were: (1) feasibility of the structural design; (2) patient and staff comfort and environmental safety; (3) market competitiveness, especially oxygen therapy; (4) coordination with clinical functional plan and availability of electromedicine; (5) the establishment of an adequate communications network; (6) waste management; (7) the management and availability of adequate supplies and flows (ie, energy, water, food, and linen); and (8) the implementation of a biosecurity plan.
In the H144, three main work areas were defined (Figure 2):
-
1. COVID-19 (+) Patient Care Area: Six modules of 24 beds each (144 beds in total), with a nursing station per module. Rooms were individual, separated by panels of 2.7 meters high, and with a surface of nine square meters (3x3m), with a chair, a table, and an individual wardrobe. In this health care area, there was also a toilet and shower area, a reading/TV area, a triage area, a medical work room, and a warehouse area. A special room was also designed for relatives to accompany patients in a very severe condition, prior to death. It had two entrances: one from the inside for the patient and one from the outside for relatives.
-
2. Working Area: Without risk of contamination, with staff dressing rooms with lockers and showers, work area for doctors, and rest area.
-
3. Logistic Area: Without risk of contamination, with a general logistics warehouse, lingerie area, food preparation area, health material store, pharmacy, and management area. Outside, in an annex pavilion, there was a waiting room for relatives.

Figure 2. Main Work Areas Defined in the H144.
Abbreviation: PPE, personal protective equipment.
Health Aspects in the Design and Implementation of the H144
From a health point of view, multiple factors were taken into consideration, which were developed in parallel with the construction of the hospital.
Definition of Health Care Objectives—One of the keys of ACS for COVID-19 patients is a clear definition of their health care objectives, always taking into account the necessary flexibility in a changing reality. The H144 was designed to treat COVID-19 patients without or with moderate symptoms, and that in case of clinical worsening, would not be candidates for ICU admission due to poor functional and cognitive situations (Barthel index prior to acute illness ≤15).13 Only in the event that the regular hospital network could not admit more severe patients, these would be treated at the H144 with prior authorization from health authorities.
Design of a Humanization Plan 14—Parallel to the design of the functional plan, a humanization plan was designed, including aspects such as reception and information plan for patients and relatives, welcome and training plan for staff, and a special approach for comfort care for terminally ill patients, including relatives visits in a specially designed room. In addition, an outdoor space was set up so that patients with a good clinical condition could go for a walk outside, accompanied by specific staff with appropriate use of personal protective equipment (PPE).
Definition of Flows and Work Areas—The first flow to be defined was the admission of patients. The COVID-19 coordinator of each hospital, usually a doctor, contacted the H144 medical direction to provide clinical information and ask for patient transfer. After checking the availability of beds and the adequate profile of the patient, the patient was admitted. Patients from nursing homes or from the primary health care network requiring hospital care or isolation could also be admitted, but always after blood test and thorax x-ray in the emergency department (Figure 3). The H144 received patients until 8:00pm every day of the week.

Figure 3. Locations Where Patients were Admitted From.
Waste Management Plan—Following regional law 22/2011 of waste and contaminated soil15 and the guide for the management of sanitary waste of the Principality of Asturias,16 a simple waste management plan was drawn up, dividing them into two large groups (non-hazardous and hazardous). In the white or green area, the waste would be classified as non-hazardous, with a subsequent division of these as recyclable or not, while all the waste generated in the red area would be classified as hazardous waste and would be sent to the incinerator for disposal.
Management of Human Resources and Training Program—Staff assigned to the H144 were mostly professionals from public health system job-seeker lists, to avoid absorbing health professionals from other centers. Training programs included a training session (operation and general structure of the H144, use of PPE, and the H144 emergency plan were addressed). Simulations were carried out to improve teamwork in emergency care in a contaminated area with PPE and to measure response time from the clean area. For the staff who carried out their entire working day with a PPE, a system of rest shifts was designed to plan 45-60 minutes breaks at least every three hours. Due to changing health care needs over the opening period, a system to open and close modules was designed in which external staff was activated to cover new needs when a new module was opened. Table 2 shows staff organization.
Table 2. H144 Staff

Coordination with Other Structures and Integration into the Public Health Care Network, Including Information Systems—Based on the H144 experience, the key to the success of ACS for COVID-19 patients is their correct integration into the health system network, at an organizational, technical, and “emotional” level. In this sense, it is essential that fixed hospitals feel these facilities as a resource to support their daily activity in caring for COVID-19 patients. This required multiple meetings to inform about the structure and operational aspects of H144, in addition to face-to-face visits by clinical managers before and during its operation. Although patients were received from the entire health system in Asturias, H144 was integrated into the logistics and technological circuits of the Cabueñes University Hospital (HUCAB) in Gijón, which made easy daily operation by using existing logistics circuits (ie, warehouse, pharmacy, kitchen, and lingerie). Sespa’s Infrastructure and Technical Services was in charge of integrating H144 into Sespa’s Electronic Health Record System, called SELENE, as an extension of HUCAB. For this, it was necessary to build up the entire hardware infrastructure in the center itself. In addition, templates, forms, reports, and ad-hoc requests were designed, which made it possible to have a specific software work scenario for H144, but integrated with HUCAB, allowing to request and access to all the necessary tests, as well as to carry out consultations with other services, if necessary. Pharmacological prescriptions were also managed through SELENE, which were received daily in the form of single doses for each patient prepared by the pharmacy service. The integration was such that, when necessary, the presence of physiotherapists and psychologists from HUCAB was required in H144. Furthermore, coordination with the Social Work Unit was essential given the special social circumstances for a significant number of patients.
Biosecurity Plan—Processes were developed for cleaning and environmental disinfection, including surfaces and materials, to provide the highest level of biosafety for patients and professionals. Environmental control of air quality (particles of 0.5 and 5.0 μm, humidity, temperature, and concentration of CO and CO2) was made, as well as count of aerobic flora in the environment in representative areas (analysis of general microbiological contamination and microbiological analysis to identify COVID-19). Also, bio-decontamination of areas, equipment, and material during the activity was performed with Ethylene peroxide, obtaining excellent results.
Clinical Activity
The H144 was opened from November 12, 2020 through March 5, 2021. A total of 334 patients were admitted, generating 3,149 hospital stays. A sequential opening-closing system of modules was established to adapt to the needs, planning human resources according to H144 activity. Maximum occupancy was on February 1, 2021 (74 patients). In Figure 4, it shows the daily number of patients admitted to the H144 compared to the patients admitted for COVID-19 in the Sespa hospital network. Number of patients follows the wave of hospital occupancy in both the second and third waves. Between both waves, a small health care activity was maintained due to the admission of patients from an outbreak in a nursing home.Reference Mas Romero, Avendaño Céspedes and Tabernero Sahuquillo17

Figure 4. Daily Number of Patients Admitted to the H144 Compared to Patients Admitted for COVID-19 in Sespa’s Hospital Network.
There was a total of 334 admissions (66% women; 34% men), with a mean stay of 9.42 days (MD = 3.99; [1-34]), generating a total of 3,149 hospital stays. At discharge, 126 patients (38%) went to a nursing home, 112 (33%) to their home, 40 (12%) were transferred to another hospital, and 56 (17%) died. Of those transferred to the hospital, 31 (77.5%) were admitted and did not return to the H144. The mean age of the admitted patients was 82.79 years (MD = 8.68; [29-104]) and was higher in women (85.09; MD = 7.57; P = .000) than in men (78.28; MD = 9.22), which could explain higher mortality among womenReference Bonanad, García-Blas and Tarazona-Santabalbina18 (19.5% versus 11.5% in men), greater average stay (9.74 versus 8.81 in men), and higher discharge to nursing homes (41% versus 30% in men). Forty-three percent of men were discharged at home (28% in the case of women). In Table 3, these differences are shown.
Table 3. Differences by Gender of the Patients

As mentioned above, the H144 supported Sespa’s health structure. In Figure 5, the origin of the patients is shown.

Figure 5. Origin of Patients.
Abbreviations: HUCAB, Cabueñes University Hospital; HUSA, Hospital Universitario San Agustín; HUCA, Hospital Universitario Central de Asturias; JOVE, Hospital de Jove.
From the medical point of view, patients were basically grouped into two categories: mild COVID-19 patients awaiting for recovery on one side, and on the other hand, moderate patients not candidates to intensive care measures in case of clinical worsening. Many of the first group of patients came from nursing homes.Reference Gallego, Codorniu and Cabrero19 As they needed a negative COVID-19 polymerase chain reaction (PCR) test prior to be discharged to their nursing home, medical treatment tended to be simple, trying to prevent further complications (thrombosis, delirium, nosocomial infection, physical deconditioning, and malnutrition associated with hospitalization).20,Reference Inouye, Bogardus and Charpentier21 For patients in the second category, symptomatic treatment, humanization of the stay, and palliative care were focused on.Reference Fadul, Elsayem and Bruera22 In all the patients, the main problem was the tendency to delirium and disorientation typical of hospital stay, increased due to a lack of circadian references for being in a facility without windows, and for prolonged stays in patients with preserved cognitive status with persistently positive PCRs.Reference Guilcher, Everall, Cadel, Li and Kuluski23 In future similar experiences, it is suggested to be flexible with family visits, walks outside the hospital, and other measures to avoid delirium and physical deconditioning due to activity limitation.Reference Zisberg, Shadmi, Sinoff, Gur-Yaish, Srulovici and Admi24,Reference Hoyer, Friedman and Lavezza25 The physical structure of the hospital would be maintained and the distribution of staff in direct contact with the patient, as well as good coordination and teamwork among staff from diverse origins.
Discussion
From the H144 experience, the design, execution, and implementation of an ACS for COVID-19 patients is a challenge in which the participation of different areas of knowledge is essential. Among the aspects to consider for future ACS based on this experience, the following could be highlighted:
-
1. The concept of “temporary hospital” should not imply a decrease in hospital technical requirements or in terms of quality of care.
-
2. A multidisciplinary team, well cohesive and motivated, with common objectives and the ability to adapt to changing environments is one of the critical aspects, probably for any complex project.
-
3. The team that designs the facility and its functional plan must be the same as the one in charge of the facility during its activity.
-
4. Support and acceptance of the rest of the health care network is essential for the success of the project. All must work in coordination with the rest of the health care structures, accept external suggestions for improvement, and work with the clear conviction that it is a health facility to serve the rest of the health care system and, lastly, the citizens. Communication must be fluid and permanent throughout the entire period of operation.
-
5. Permanent adaptability of all equipment and structure is necessary. During the operation period, various scenarios, not foreseen in the initial functional plan, were contemplated (ie, possibility of admitting asymptomatic patients for isolation, and use of non-invasive ventilation not considered initially). The architectural and functional design of the H144 allowed for the contemplation of multiple organizational and health care approaches.
-
6. The fact of opening and closing modules sequentially according to needs was a challenge from the point of view of staff organization, and even so, maintaining the staff ratios initially designed was managed. The main difficulty was precisely this: get staff under the premise of not reducing resources in other health care facilities.
-
7. Team building activities must be developed from the very beginning of the project, facilitating two-way communication with the management team and allowing the implementation of improvement proposals.Reference Miller, Kim, Silverman and Bauer26
-
8. The success of H144 would not have been possible without its Humanization Plan. Only an approach from the humanization of care could relieve the fears of patients, relatives, and workers facing an unknown situation. In the same way, accompaniment in the dying process facilitates mourning. Communication with the relatives was essential, providing permanent communication with them. Probably, H144 patients were the only COVID-19 patients admitted to a hospital who had the possibility to walk outside.
Limitations
As a main limitation of this report, this experience was developed in a country with a well-develop public health care system, so the aspects proposed to consider for future experiences must be taken into consideration for similar contexts, or in some cases, adapted to different ones. Also, clinical follow-up of the patients after discharge was not made, as it was beyond the objectives of this report, but could be of interest for future research.
Conclusion
Alternate care sites for COVID-19 patients can be valuable health care structures to improve surge capacity of the health system when overwhelmed with COVID-19 patients. For that purpose, they need to be well-designed and integrated into the health care network. Focusing ACS on mild patients allows hospitals to focus on more severe patients, avoiding that these structures “absorbed” specialized staff from other more complex hospitals, and may also have positive effects on the control of epidemic outbreaks in nursing homes. The results and experience of use of the H144 Hospital of the Health Service of the Principality of Asturias was satisfactory for the patients and the health system.
Acknowledgments
The authors wish to acknowledge: Jesús Menéndez, architect of the Health Authority in charge of the architectural project; All Health Authority departments involved in the design and implementation of the H144 hospital; All H144 health care and non-health care workers who were somehow linked to this project; The families, for their enormous understanding of everything that could be improved; and of course, The patients, to those alive and to those who left, for teaching all to be better professionals.
Conflicts of interest/funding
None declared. The authors have no financial or other interest that should be known to readers related to this document.











