Recent ideas based on social ranking theory and power from evolutionary psychology (Reference GilbertGilbert, 1992) argue that certain life situations are likely to be depressogenic, particularly if they encapsulate feelings of loss, humiliation and entrapment (or defeat). We have argued that placing the individual at the centre of our thinking locates psychosis as a major life event whose appraisal may involve all of these elements and can limit activity in the interpersonal and achievement domains, leading to loss of valued roles or goals and the individual being unable to assert an identity (Reference Rooke and BirchwoodRooke & Birchwood, 1998). The archetypal factor that is highly congruent with the course of depression is self-esteem (Reference Brown, Bifulco and AndrewsBrown et al, 1990). Blatt et al (Reference Blatt, D'Afflitti and Quinlan1976) argue that depression vulnerability is associated with greater self-criticism, the need for autonomy or dependence on others (‘sociotropy’), all highly stable factors accessing feelings of social inferiority and poor sense of agency. Zuroff et al (Reference Zuroff, Moskowitz and Cote1999) have embedded these characteristics within the socio-evolutionary framework, arguing that depression-prone individuals suffer from insecurities regarding attachment and social acceptance. In addition, the developmental nature of self-representations is argued to be a significant factor in the recovery of individuals with severe mental illness (Reference Davidson and StraussDavidson & Strauss, 1992). They suggest that reconstruction of the self can only occur following acceptance of the disorder, allowing individuals to focus on their sense of self and ‘move forward’ in life. But individuals then fall short of their preferred or aspired-to self, resulting in a sense of entrapment and loss (Reference Birchwood, Iqbal, Wykes, Tarrier and LewisBirchwood & Iqbal, 1998). In this paper appraisals about psychosis (loss, humiliation and entrapment), awareness of illness, depression vulnerability and appraisals of self are hypothesised to distinguish patients developing postpsychotic depression (PPD) from those without PPD. Given that a number of individuals relapsed during the course of the follow-up, we reasoned that factors disposing to relapse and to PPD will be qualitatively different, and that these beliefs will also distinguish those developing PPD from those who relapse. Furthermore, it is hypothesised that participants developing PPD will have a greater propensity to see their future selves as low-status self-representations (‘possible selves’), whereas those not developing PPD will report a lesser inclination to believe that low-status roles will describe them in the future.
METHOD
Methodology, case identification, assessment criteria and the definitions of PPD, non-PPD and relapse are described in the preceding companion paper (Reference Birchwood, Iqbal and ChadwickBirchwood et al, 2000b , this issue).
Hypotheses
-
(a) Patients will, immediately prior to and during PPD onset, show more negative appraisals of psychosis, cognitive vulnerability and more insight in comparison to non-PPD patients.
-
(b) Relapsing patients will not differ in beliefs about psychosis, insight or cognitive vulnerability in comparison to patients without relapse or without PPD.
-
(c) Patients developing PPD will show a greater propensity to describe their possible future selves in terms of lowstatus roles rather than high-status roles in comparison to those not developing PPD.
Measures
Appraisal of psychosis
Participants' cognitive appraisal of their illness was evaluated using the Personal Beliefs about Illness Questionnaire (PBIQ; Reference Birchwood, Mason and MacmillanBirchwood et al, 1993). The PBIQ is comprised of 16 items rated on a four-point scale and assesses patients' beliefs in five domains: loss, humiliation, shame, attribution of behaviour to self or to illness and entrapment in psychosis. The scale has been shown to have a good level of reliability and validity with schizophrenia.
The Insight Scale (Reference Birchwood, Smith and DruryBirchwood et al, 1994) is a rapid self-report measure, specifically developed for psychotic populations, consisting of eight statements to which the subject responds in one of three ways: agree, disagree and unsure. The scale provides three insight factors (relabelling of symptoms, awareness of illness and need for treatment) in addition to a total insight score. The scale has been shown to have excellent reliability and both concurrent and criterion validity.
Depression (cognitive) vulnerability
Depression vulnerability was assessed using the Depressive Experiences Questionnaire (DEQ; Reference Blatt, D'Afflitti and QuinlanBlatt et al, 1976) and the Crown Self-Esteem Scale (Reference Crown, Lucas and StringerCrown et al, 1977). The DEQ is a self-report measure consisting of 66 items rated for conviction of belief for each item on a seven-point scale: from ‘strongly disagree’ to ‘strongly agree’. The reliability of the DEQ is well established with both adult and adolescent depressive populations and three highly stable factors can be calculated: sociotropy, self-criticism and self-efficacy (Reference Blatt, D'Afflitti and QuinlanBlatt et al, 1976).
The Crown scale is a variant of Rosenberg's original self-esteem measure (Reference RosenbergRosenberg, 1965) and consists of ten items. It is a self-report inventory that provides a rapid evaluation of patient's self-esteem. Each item is rated on a four-point scale: from ‘strongly agree’ to ‘strongly disagree’. Item directionality and scoring is such that a lower score depicts higher levels of self-esteem. Extensive use of the scale by both Rosenberg (Reference Rosenberg1965) and Crown et al (Reference Crown, Lucas and Stringer1977) suggests good levels of reliability across a range of populations (see Table 1).
Table 1 Mean BDI, PBIQ, Insight Scale and Crown scores for post-psychotic depression (PPD), non-PPD and relapse groups prior to and during PPD

| Group | Measure | Pre-PPD (s.d.) | PPD (s.d.) |
|---|---|---|---|
| PPD (n=28) | BDI | 9.5 (3.8) | 21.4 (7.7) |
| Entrapment | 8.8 (3.0) | 10.1 (2.5) | |
| Self v. illness | 8.2 (1.9) | 8.2 (2.0) | |
| Loss | 6.9 (2.6) | 7.4 (2.4) | |
| Shame | 5.6 (1.8) | 6.3 (2.1) | |
| Humiliation (social) | 3.8 (1.0) | 3.8 (0.8) | |
| Awareness | 2.2 (1.6) | 3.0 (1.3) | |
| Relabel | 3.2 (1.3) | 3.5 (1.0) | |
| Treatment | 2.3 (1.6) | 3.2 (1.2) | |
| Insight | 7.7 (4.1) | 9.7 (3.0) | |
| Self-esteem | 21.0 (5.8) | 26.3 (5.4) | |
| Non-PPD (n=31) | BDI | 7.1 (4.6) | 7.5 (4.9) |
| Entrapment | 7.5 (2.4) | 6.9 (2.1) | |
| Self v. illness | 7.2 (1.9) | 6.7 (1.8) | |
| Loss | 5.6 (2.0) | 5.3 (2.1) | |
| Shame | 5.5 (1.9) | 4.8 (1.5) | |
| Humiliation (social) | 3.3 (1.0) | 3.1 (1.0) | |
| Awareness | 1.5 (1.3) | 1.6 (1.2) | |
| Relabel | 2.5 (1.6) | 2.5 (1.7) | |
| Treatment | 2.6 (1.4) | 2.4 (1.7) | |
| Insight | 6.6 (3.9) | 6.6 (4.3) | |
| Self-esteem | 17.1 (4.6) | 16.1 (4.7) | |
| Relapse (n=11) | BDI | 7.4 (4.1) | 25.6 (10.0) |
| Entrapment | 8.3 (2.9) | 11.4 (2.3) | |
| Self v. illness | 8.4 (2.1) | 8.5 (1.9) | |
| Loss | 6.0 (1.7) | 7.9 (1.7) | |
| Shame | 6.1 (1.1) | 6.4 (1.8) | |
| Humiliation (social) | 3.6 (1.0) | 4.3 (1.0) | |
| Awareness | 1.6 (1.2) | 3.2 (1.3) | |
| Relabel | 2.5 (1.6) | 3.4 (0.9) | |
| Treatment | 2.4 (1.7) | 3.4 (1.3) | |
| Insight | 6.5 (3.9) | 10.1 (3.0) | |
| Self-esteem | 18.8 (4.9) | 27.81 (7.0) |
The working self-concept
The short (80-item) form of the Possible Selves Questionnaire (PosSq; Reference Marcus and NuriusMarcus & Nurius, 1986) is a self-rated measure of self-knowledge that provides representations of the self in the past, present and future. The 80 items are personality descriptors with an equal number of items covering five areas: general abilities, lifestyle possibilities, general descriptions, physical characteristics and possibilities tied to the opinion of others. Half of the items are high-status or ‘positive’ selves and the other half are low-status or ‘negative’ selves.
The development of the low- and high-status items for the PosSQ involved asking a community sample to “tell us what is possible for you” and generated 150 distinct possibilities for the self, utilised in the long version of the questionnaire, which also included a sixth domain of personality descriptors: possibilities reflecting various occupational alternatives (Reference Marcus and NuriusMarcus & Nurius, 1986). An equal number of items judged as positive, negative and neutral were employed within each of these six categories. The short form of the PosSQ used here omits all neutral items and also the category of ‘occupational’ possible selves.
Each descriptor or possible self is rated on a five-point scale from ‘not at all’ to ‘very much’ on four questions:
-
(a) How much does this describe you now?
-
(b) How much would you like this to describe you in the future?
-
(c) How probable is it that this will describe you in the future?
-
(d) How important is it to you to be this?
The short form of the PosSQ provides three weighted variables for both the high-status and low-status self-representations: the ‘now self’, the ‘probable self’ and the ‘like-to-be self’. Prior to calculating the variables, each item's ‘importance to self’ rating (i.e. from question (d)) was employed as a cutoff, so that only descriptors rated as ‘somewhat’, ‘quite a bit’ or ‘very much’ important are included in calculating the possible selves variables. This procedure accounted for the individual differences between participants' self-representations (i.e. certain possible selves will be more important to some participants than others and therefore, the ratings for ‘now’, ‘probable’ and ‘ideal’ selves would be affected by this subjectivity). A mean score for high- and low-status ‘now’, ‘probable’ and ‘ideal’ selves was then obtained.
The PosSQ is a valid and reliable measure of self-knowledge and, in addition, is highly correlated with self-esteem measures (Reference Marcus and NuriusMarcus & Nurius, 1986).
RESULTS
Post-psychotic depression and group membership criteria
The definition of PPD and group membership criteria is described in the preceding companion paper. To recap, pre-PPD refers to the follow-up point immediately prior to PPD where the patient is not depressed. In the following analyses we compare the groups of patients with PPD with those without PPD on appraisal and vulnerability factors (patients' beliefs about their psychosis, cognitive vulnerability and insight) at the pre-PPD stage when neither group was depressed.
Comparison of PPD with non-PPD groups
Beliefs about psychosis
Figure 1 shows the course of the five beliefs about psychosis measured in the PBIQ in the PPD and non-PPD groups. The factors measure patients' beliefs about their psychosis and its implications for the self as described in Rooke & Birchwood (Reference Rooke and Birchwood1998): entrapment (control over illness); shame; loss of autonomy and valued social role; humiliation and loss of rank, arising from a belief in the social segregation of those with mental illness; and attribution (self v. illness as responsible for behaviour/experience).

Fig. 1 Graphs depicting stability and change in key appraisals across post-psychotic depression (PPD, [UNK]), non-PPD ([UNK]) and relapse ([UNK]) groups. A higher score depicts greater perceived negativity for each variable.
The first hypothesis was tested using a MANOVA model with factors of group (PPD v. non-PPD), time (pre-PPD and PPD) and their interaction. The dependent variables were entrapment, shame, social humiliation, loss and attribution of illness to the self. A significant group effect (F=3.4, d.f.=5, 53, P <0.01) and group × time interaction (F=2.5, d.f.=5, 53, P <0.05) emerged.
The main test of the hypothesis is the difference between groups at the pre-PPD stage. At this stage (i.e. when neither group was depressed), the PPD group was significantly more likely than non-PPD participants to attribute the cause of psychosis to the self rather than an ‘externalised’ illness (F=4.3, P <0.05), to perceive greater loss of autonomy and valued role (F=4.9, P <0.05) and to perceive themselves to be humiliated (F=4.0, P=0.05) and entrapped by their illness (F=3.5, P=0.07). No difference was observed between the two groups for shame (F<1, NS).
At the PPD stage (i.e. while depressed) all five PBIQ appraisals were significantly more negative in those participants with PPD (entrapment: F=27.5, P <0.001; shame: F=10.3, P <0.01; social humiliation: F=8.0, P <0.01; illness attributed to self: F=9.4, P <0.01, loss of autonomy/ role: F=12.8, P <0.01).
Ideal versus probable self
Table 2 depicts the mean scores for ratings of ‘now’, ‘probable’ and ‘like-to-be’ (ideal) possible selves in both low-status and high-status domains for the PPD and non-PPD groups. In line with the hypothesis, participants developing PPD were more likely to evaluate their future (i.e. ‘probable’) roles as ‘low status’ than those who did not become depressed (t=2.7, P <0.01). This held even when controlling for depression at the time of testing. As anticipated, no difference was evident for low-status roles for ‘now’ and ‘like-to-be’ selves (t<2, NS). However, for the high-status roles, no difference was observed between the two groups for ‘now’, ‘probable’ and ‘like-to-be’ selves (t<1, NS).
Table 2 Mean post-psychotic depression (PPD) and non-PPD group ratings for propensity to high- and low-status roles by the individual: now, probable and like-to-be

| High-status roles | Low-status roles | |||||
|---|---|---|---|---|---|---|
| Now | Probable | Like-to-be | Now | Probable | Like-to-be | |
| PPD (n=24) | 1.13 (0.15) | 1.18 (0.19) | 1.26 (0.25) | 2.00 (0.42) | 1.89 (0.45) | 1.27 (0.32) |
| Non-PPD (n=26) | 1.11 (0.11) | 1.14 (0.11) | 1.20 (0.17) | 1.85 (0.33) | 1.58 (0.31) | 1.23 (0.20) |
| P | NS | NS | NS | NS | <0.01 | NS |
In other words, both PPD and non-PPD patients' evaluation of their aspired-to (and current) roles were identical; however, patients developing PPD anticipated lower status future roles, whereas those not developing PPD were less likely to see their future as being of a lower status. The converse does not apply: PPD patients did not invest less in higher status roles.
Depression vulnerability
Self-esteem. Figure 2 depicts the course of mean self-esteem for both PPD and non-PPD groups (increasing score depicting greater negativity of esteem). To test the first hypothesis, a similar MANOVA model, with factors of group and time as outlined above, was employed and revealed a significant time effect (F=7.9, d.f.=1, 54, P <0.01) and group × time interaction (F=16.5, d.f.=1, 57, P <0.01).
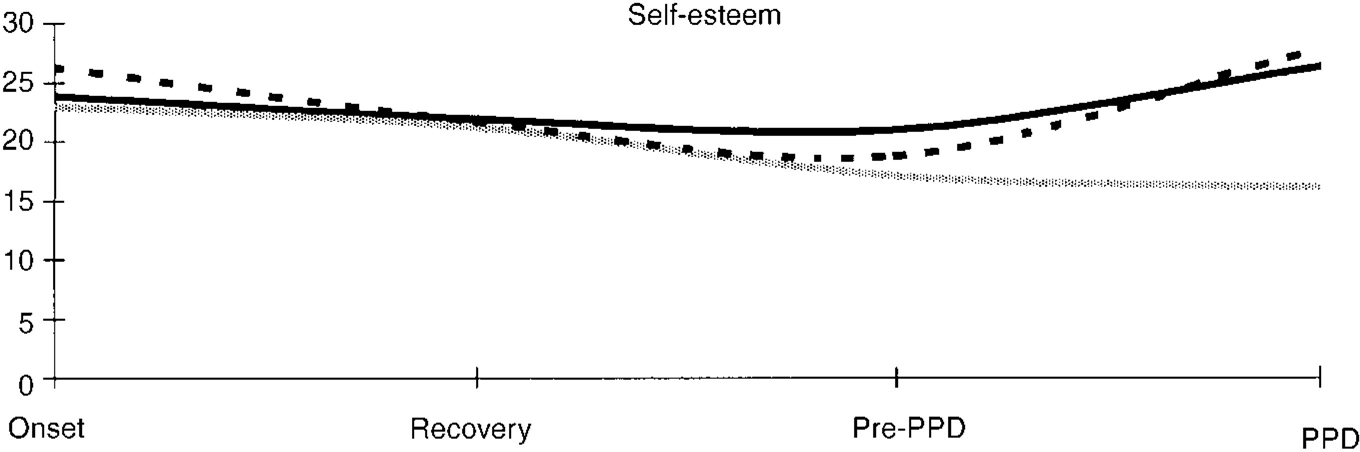
Fig. 2 Graph depicting stability and change in mean self-esteem across post-psychotic depression (PPD, [UNK]), non-PPD ([UNK]) and relapse ([UNK]) groups. A higher score depicts greater perceived negativity for each variable.
Scores for PPD and non-PPD groups were compared at both pre-PPD (not depressed) and PPD observation points: participants developing PPD were more likely to have significantly lower self-esteem at both observation points, including the point at which neither group was depressed (i.e. pre-PPD; P <0.01).
Sociotropy, self-efficacy and self-criticism. The PPD group participants were significantly more self-critical than those who remained non-depressed, implying that the depressed group had lower self-esteem (F=14.2, P <0.001). In addition, the DEQ vulnerability factor of sociotropy approached significance (F=3.6, P=0.06) with higher scores in the PPD group. Self-efficacy was not a significant discriminator between the PPD and non-PPD groups.
Insight. The course of insight, specifically the awareness of illness, the relabelling of symptoms and the need for treatment, is depicted as a total insight score for both PPD and non-PPD groups in Fig. 3. The MANOVA model revealed a significant group effect (F=7.0, d.f.=3, 54, P <0.01) and group × time interaction (F=3.0, d.f.=3, 54, P <0.05). The main test of the first hypothesis is the difference between groups at the pre-PPD stage, where no difference was apparent between the PPD and non-PPD groups on any insight variables: awareness (F=2.8, NS); symptom relabelling (F=2.6, NS); treatment need (F=0.5, NS) and total insight (F=0.9, NS).
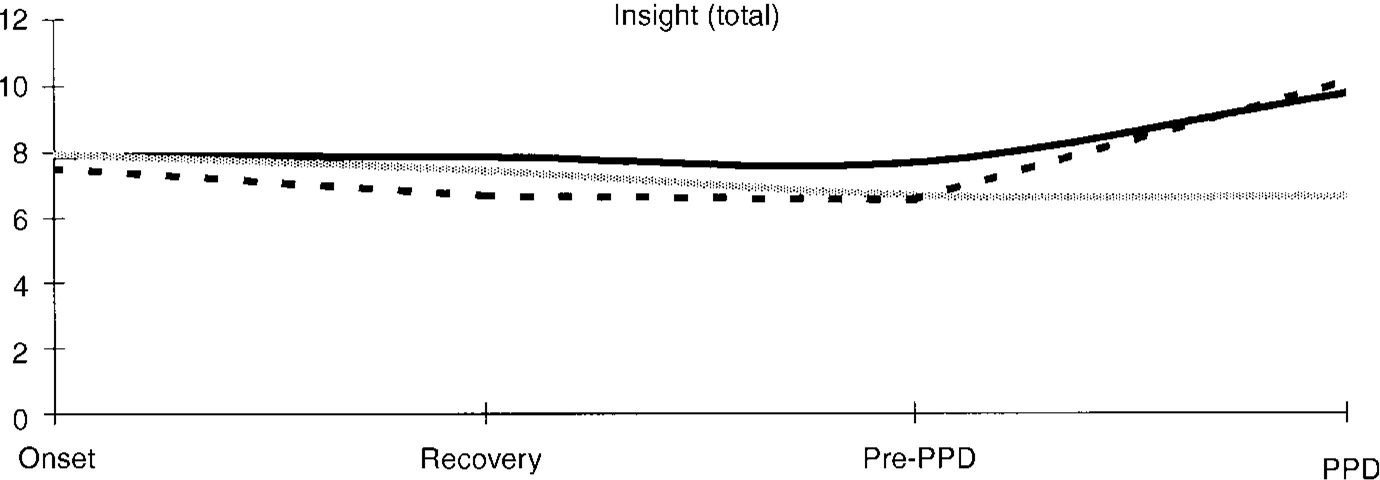
Fig. 3 Graphs depicting stability and change in insight across post-psychotic depression (PPD, [UNK]), non-PPD ([UNK]) and relapse ([UNK]) groups. A higher score depicts greater insight.
When patients were depressed, however, the reported greater insight, including awareness of illness (F=16.2, P <0.001), relabelling of symptoms (F=7.3, P <0.01), need for treatment (F=4.2, P <0.05) and total insight score (F=10.1, P <0.01).
Experience of psychosis
The PPD group did not experience most relapse, use of the Mental Health Act or longer duration of illness. Indeed, patients with a first episode of psychosis were more prone to PPD than those with multiple episodes (50% v. 32%; P <0.01). Patients with PPD were no more likely to be unemployed than the non-PPD group.
Comparing relapsing with non-relapsing patients
In the following analyses we are concerned with determining whether the vulnerability to relapse embodies individuals' concerns about the experience of psychosis and its implications for the self. In other words, do the negative appraisals, which seem to confer vulnerability to PPD, also confer vulnerability to relapse? We contrast, therefore, our vulnerability factors between the group of relapsing patients (n=11) and the group of non-relapsing, non-PPD patients (n=31) at the pre-PPD stage.
The relapse group contains those patients whose depressive symptoms at the PPD stage were in fact part of a relapse (see the preceding companion paper), so to test the second hypothesis between-subject comparisons for the aforementioned variables at the pre-PPD stage were conducted. No differences emerged between the non-PPD and relapse groups on beliefs about psychosis (loss, humiliation and entrapment), self-esteem, sociotropy, self-efficacy or self-criticism. Insight did not differentiate between the groups.
In summary, there were no cognitive vulnerability factors for psychotic relapse, in stark contrast to PPD: different processes would seem to be in operation.
DISCUSSION
Vulnerability to PPD
In accordance with the first hypothesis, those who went on to develop PPD felt greater loss, humiliation and entrapment arising from their psychosis and were more likely to attribute the cause of the psychosis to the self; they also had lower self-esteem and were more self-critical than their non-depressed counterparts. Insight did not differentiate between the two groups while participants were not depressed. During PPD, patients reported greater insight into their illness, further lowering of self-esteem and increase in their appraisals of loss, humiliation, entrapment, shame and self-blame. This is a replication of similar comparisons of depressed versus non-depressed participants in our previous studies (Reference Birchwood, Mason and MacmillanBirchwood et al, 1993; Reference Birchwood, Smith and DruryBirchwood et al, 1994; Reference Rooke and BirchwoodRooke & Birchwood, 1998). As hypothesised, a comparison of relapsing patients with non-depressed/non-relapsing patients revealed no differences in appraisal of psychosis, insight or depression (cognitive) vulnerability, underlining the fundamental distinction between these processes.
We conclude that the mechanism underlying PPD is dependent upon the individual's own experience of psychosis and how he/she appraises its implications for the self, specifically in terms of loss, self-blame, humiliation and feelings of entrapment in psychosis.
The application of social ranking theory to depression (Reference GilbertGilbert, 1992) provides an important framework from which PPD may be conceptualised. The effect of powerful and oppressive experiences (or shattering life events, such as psychotic illness) according to this theory initiates an internal defensive mechanism that forces the individual to ‘down-rank’ and yield to others, particularly if escape is blocked (entrapment). This mechanism may be accompanied by cognitions that are ‘self-attacking’, leading to feelings of inferiority and self-blame. This focuses attention on the appraisal of psychosis more than depression vulnerability per se, underlined by the result that those who are depressed are more aware of their psychosis (i.e. insight). Brown et al (Reference Brown, Bifulco and Andrews1990) argue that any individual can become depressed when given the right context and we suggest that the particular ‘context’ required for PPD is provided by the appraisal of psychosis where this embodies loss, humiliation and entrapment and the patient's consequent ‘down-ranking’.
Methodological issues
In hindsight the utilisation of the DEQ at only one of the follow-up points after the psychotic episode may have resulted, in the case of dependency and self-efficacy variables, in an increase of any difference between PPD and non-PPD patients, because the timing of PPD varied across participants; that is, it would have been preferable to administer the DEQ at the pre-PPD stage (when no participants are depressed). However, two arguments can be made to support the validity of these particular results. First, Blatt et al (Reference Blatt, D'Afflitti and Quinlan1976) and Zuroff et al (Reference Zuroff, Moskowitz and Cote1999) have demonstrated that the DEQ variables are indeed vulnerability factors for depression and are stable. Second, the high correlation between self-esteem (assessed at all follow-up points) and self-criticism, both of which discriminated between PPD and non-PPD patients, does suggest that utilising the DEQ at one follow-up point did provide accurate data. Owing to the relatively low numbers in the relapsing group (n=11), the results of the between-group analyses lacked power and should be interpreted with a degree of caution.
Is psychological vulnerability cause or effect?
These results show that it may be possible prospectively to determine who will develop PPD by reference to our vulnerability variables. The issue arises: is this vulnerability cause or effect? There are two possibilities. First, the vulnerabilities that we have identified may be simply markers or epiphenomena of past depressive episodes, with no causal value. The high level of PPD in first episodes seen in this and other studies (Reference Addington, Addington and PattenAddington et al, 1998) suggests, on the contrary, that they can be primary. It is highly likely, however, that repeated depressive episodes will leave their mark on self-esteem. What is clear is that the study has identified a group of individuals, when well, who later develop PPD and this largely revolves around how they perceive the implications of psychosis for their identity and social status. What is remarkable is how patients' awareness of their illness (‘insight’) increased during PPD, supporting our belief that psychosis is indeed what patients are depressed about (Reference Birchwood, Iqbal, Wykes, Tarrier and LewisBirchwood & Iqbal, 1998).
The second possibility is that the vulnerabilities that we have identified are a direct result of particularly adverse experiences of psychosis. In fact, no difference was found between the PPD groups in duration of psychosis, number of episodes, etc.; indeed, patients with a first episode of psychosis were more likely to develop PPD. Thus, although we are arguing that a degree of ‘depressive realism’ about psychosis underpins the appraisals, they do seem to go beyond patients' direct experience and engage the individual's personal interpretation. What was not measured, however, was individuals' premorbid aspirations and functioning and thus the limits that the illness may have ‘objectively’ placed on functioning. We attempted to examine this by directly focusing upon discrepancies between individuals' ‘ideal’ and ‘probable’ self. The hypothesis was partly upheld in that the participants who developed PPD believed that it was significantly more likely that their future selves would include low-status roles than those who were not depressed (i.e. non-PPD). However, no difference was observed between the two groups for their affinity to high-status roles.
It is to be noted that both depressed and non-depressed participants display certain similarities (at the time of testing, similar self-representations were held for both low- and high-status roles: ‘now’ selves) and that both groups also estimate that they would, in an ideal situation, see themselves as acquiring the same-status roles (‘like-to-be’ selves). Indeed, the distinguishing variable appears to be the belief by patients who become depressed (i.e. the PPD group) that their future selves are more likely to be defined by low-status roles.
Our hypothesis is that the implications of psychotic illness force the individual to ‘down-rank’ and accept a less-valued social role/goal, and that the appraisals underpinning this oppressive ‘mechanism of change’ for the self result in depression (Reference GilbertGilbert, 1995). We propose that patients who did develop PPD may foresee lower status roles and these may lead to the ‘inner conflict’ manifested by cognitions of loss, humiliation and entrapment.
The justification for employing the PosSQ as a one-off measure comes from literature supporting the stability of the self-concept in the short term (i.e. the working self-concept) (Reference Marcus and WurfMarcus & Wurf, 1987). This is defined as the ‘self-concept of the moment’ and suggests that individuals are heavily influenced in all aspects of judgement, memory and behaviour by their currently accessible thoughts, attitudes and beliefs. Indeed, this definition implies that there is no fixed or static self, but an evolving self-concept influenced by the individual's ongoing social experiences. However, this approach also allows for the self-concept to be viewed as a dynamic and static entity: dynamic owing to the changes in the individual's motivational and social state, and static because core aspects of the self may be unresponsive to such changes (Reference Marcus and NuriusMarcus & Nurius, 1986). This limitation in the methodology would therefore require further replication of the findings, and ideally include an evaluation of the self-concept at more than one follow-up point after the psychotic episode. We would emphasise, however, that this result held even when controlling for depression at the time of testing.
Ogilvie's (Reference Ogilvie1987) suggestion that individuals' appraisal of their well-being is based upon their perception of how close (or distant) they are from their most negative images of themselves (i.e. ‘the undesired self’) may well inform the mechanism underlying PPD onset. Such a mechanism may be sensitive to the chronicity of the patient sample in that a greater conflict between ‘like to be’ and ‘probable/future’ self may be observable during the early episodes of psychosis and less evident after a number of relapses (i.e. where the more chronic patients, through acceptance and adaptation to the experience of their illness, have lowered their expectations and have a lesser discrepancy between how they are at present and how they wish to be). Hence, a greater conflict in early psychosis may be a likely factor in the reported high incidence of depression and suicide in such cases (Reference Addington, Addington and PattenAddington et al, 1998). Indeed, 9/18 (50%) first-onset cases in the present study developed PPD in comparison to 19/60 (32%) in the remaining ‘multiple-episode’ sample (t=3.14, P <0.01). We maintain that the mechanisms of ‘down-ranking’ and the entrapping effect of psychosis may be comparable to other catastrophic life events (such as major physical disability, which requires the individual to readjust and reformulate the self) and are preceded by initial stages where feelings of anger, dis-belief and negative affect are commonplace (Reference Lazarus and FolkmanLazarus & Folkman, 1984). The individual's experience of psychosis and patienthood is just such a debilitating psychological and social assault on the self-concept, especially following first onset, and he/she may display similar reactions.
Therapeutic implications
The social ranking perspective outlined here offers a different emphasis in the application of cognitive therapy to PPD (Reference Birchwood, Iqbal, Wykes, Tarrier and LewisBirchwood & Iqbal, 1998). Fundamentally, cognitive therapy bases its therapeutic approach on the assumption that cognitions are irrational and may be focused upon when almost blind to context. Our approach firmly roots the depression in the realities of psychosis, and lays emphasis on shifting negative appraisals of psychosis and encouraging practical means of avoiding entrapment by promoting control, for example, of relapse (Reference Birchwood, Spencer and McGovernBirchwood et al, 2000a ) or voices (Reference Chadwick, Birchwood and TrowerChadwick et al, 1996). At a service level the experience of compulsory detention may be viewed as ‘hard evidence’ for entrapment that can further entrench this appraisal (Reference Rooke and BirchwoodRooke & Birchwood, 1998). Thus, minimising coercive approaches to care offers a very tangible way of minimising this most pernicious of appraisals. Work is a highly valued social role, particularly among the young (who are particularly prone to PPD), and should be a legitimate focus for mental health services. The timing of PPD some months after the acute episode is of particular concern. It is a time when, for most patients, positive symptoms have remitted and surveillance is lowered. This seems to be the very time when risk for PPD rises. The vulnerability factors, including a feeling of loss and a perceived inability to escape, offer guidance to identify those at risk. We are currently evaluating interventions informed by this model.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Patients, particularly those experiencing first-episode psychosis, need to be monitored for post-psychotic depression (PPD)/hopelessness/suicide risk some weeks after the acute episode.
-
▪ Patients' aspirations and perceived losses need to be assessed and subject to therapy.
-
▪ Developing a sense of control over psychosis may prevent feelings of entrapment and later PPD.
LIMITATIONS
-
▪ The study is a prospective snapshot of PPD following an acute episode.
-
▪ It is difficult to be certain whether the vulnerabilities were markers or risk factors.
-
▪ The inner-city provides the context for study.
ACKNOWLEDGEMENTS
We thank Professor Paul Gilbert for reviewing earlier drafts of the papers.








eLetters
No eLetters have been published for this article.