Patrick MANSON'S FIRST HELMINTHOLOGIST
There is a long list of eminent parasitologists of Scottish decent active in the 1870–1920 period, who were at the forefront of the great advances made in the battle against parasitic diseases (Barrett et al. Reference Barrett, Innes and Cox2015; Cox, Reference Coxin press). This period has often been described as ‘the golden age of parasitology’ and a most prominent figure throughout was undoubtedly Sir Patrick Manson (1844–1922). Manson is widely acknowledged as ‘The Father of Tropical Medicine’ and was largely responsible for the creation of the London School of Tropical Medicine that opened in 1899 as part of the Seamen's Hospital Society's Branch Hospital at the Albert Dock (Cook, Reference Cook2007). Under his influence many made significant international contributions, for example Ronald Ross (1878–1937) in protozoology, and in the nascent field of medical helminthology, his first appointee, Robert Thomson Leiper (1881–1969), was to be particularly productive (Willmott, Reference Willmott1981). Indeed, Leiper was to have an influential role in all aspects of pure and applied helminthology not only within the London School but also much further afield (Grove, Reference Grove1990).
LEIPER AND THE LONDON SCHOOL
At the age of 24, Leiper joined the London School in 1905 after graduating from the University of Glasgow in medicine and very quickly gained international prominence whilst on an expedition to Accra, Ghana as Carnegie Research Scholar. While in Ghana, he elucidated the life cycle of the Guinea Worm (Dracunculus medinensis) and devised simple measures for its control, still used today (Grove, Reference Grove1990). First introduced to schistosomiasis in Egypt by Arthur Looss (1861–1923) between 1906 and 1907, he also took part in the Egyptian Government's helminthological survey of Uganda. It was not until 8 years later and again in Egypt between 1915 and 1916, that he resolved the controversy behind Bilharzia. Second time around, he clearly described the essentials of life cycles of Schistosoma mansoni and Schistosoma haematobium, deducing key intervention points. This feat did not come ‘out of the blue’ for it was firmly based on formative work in the preceding year with E. L. Atkinson (1881–1929) in China, and guided by Japanese researchers who shared with him their knowledge of the life cycle of Schistosoma japonicum (see below). Other pioneering and seminal studies were conducted during 1912–1913 in Southern Nigeria where he incriminated Tabanid flies of the genus Chrysops as vectors of loiasis, as initially suggested by Manson (Grove, Reference Grove1990).
Shortly before Manson's death, in 1918 Leiper was appointed to the Courtauld Chair in Helminthology, a post subsequently held by J. J. C. Buckley (1904–1972) and then by G. S. Nelson (1923–2008). Buckley and Nelson each had a tremendous influence on the study of parasitology, which built on Leiper's legacy with newer research methods and grounded on meticulous and painstaking observation(s). In 1923, and in the same year that Leiper was elected a Fellow of the Royal Society, he founded the Journal of Helminthology, which continues to this day. He remained its lead editor until 1946 and, by raising substantial funds, Leiper was instrumental in establishing at Keppel Street the new London School of Hygiene & Tropical Medicine, which opened in 1929 (Fig. 1).

Fig. 1. As commissioned upon his 80th birthday, a portrait in oils of Professor R.T. Leiper by Andrew Freeth (Royal Society of Portrait Painters) has been on display in the London School of Hygiene and Tropical Medicine since 1972. There are two rather subtle points to note. First, as Leiper was a chain-smoker his habitual cigarette in his right hand was later removed so as not to offend anti-smoking campaigns. Second, the untitled booklet in his hands clearly has images of Bulinus and Biomphalaria, the freshwater snails involved in transmission of Schistosoma spp.. Despite being the world's eminent helminthologist, he seems happy to be remembered for these two things, a smoker and a pioneer of medical malacology, perhaps a testament to his mischievous humour.
HIS RETIREMENT AND LASTING INFLUENCE
Leiper's association with the London School was very enduring, working there until his retirement in 1947. He still remained active afterwards continuing to work up to 1958, then aged 77, as the Director of the Commonwealth Bureau of Helminthology at St. Albans, Hertfordshire, UK which became later incorporated into the Centre for Agriculture and Biosciences International (CABI). The Bureau had previously evolved from the Imperial Bureau of Agricultural Parasitology and was originally part of the Winches Farm Estate, which Leiper himself had helped the London School to purchase in 1924 (Willmott, Reference Willmott1981). The Winches Farm Research Station was later revitalized by Nelson and directed by G. Webbe (1929–1999) until its closure in 1992.
From 1958 and even in ‘full-retirement’, Leiper still influenced parasitology. As he had a passion for farming, like his father before, he was given a pedigree cow upon retirement from the London School. He continued to enjoy agriculture keeping abreast of new practices in animal husbandry. It was said that a peaceful home life had given him a happy base to secure his endeavours; 3 years after joining the London School, he married Ceinwen Saron Jones, a dentist practicing in Liverpool. They had three children, a son and two daughters, and remained married for 58 years until her death in 1966. At the time of his death in the early hours of 21st May 1969, Leiper owned three farms, two in Scotland and one in Hertfordshire.
A good example of his exceptional influence on parasitology can be found in the festschrift in honour of his 80th birthday in 1961 in the Journal of Helminthology. In the preface, there is a long list of signatures from very distinguished attendees, including from H.A. Baylis (1889–1972) Head of Parasitic Worms at the British Museum (Natural History). This was no small testament to the respect he commanded even in those he may have once unsettled (see below). His longstanding colleague at the London School P.C.C. Garnham (1901–1994) described him “He has a very decisive manner of speech and is a good lecturer. Those who argue with him or come to cross purposes usually get the worst of the argument. He is not to be deviated from his course” (Garnham, Reference Garnham1970). Other insights from P. Manson-Bahr (1891–1966), Sir Patrick Manson's son-in-law, include “He is kind, charming and helpful to the worthy, but withering to the insincere or make-believe” (Manson-Bahr, Reference Manson-Bahr1961). A former student who was later Reader in Medical Helminthology at the London School, Philippus L. LeRoux (1897–1962) commented “he has contributed much, by training and encouraging helminthologists, to alleviate pain, miseries, losses and mortality from helminthiasis in man and man's domesticated animals” (LeRoux, Reference LeRoux1961). In the context of today's OneHealth, Leiper should be recognized as a seminal pioneer exploring these concepts.
Leiper maintained regular contact with the London School until shortly before his death. In life he had obtained numerous awards including the Mary Kingsley Medal of the Liverpool School of Tropical Medicine and the Bernhard Nocht Medal from the Tropeninstitut in Hamburg, Companionship of the Order of Saint Michael and Saint George (CMG) and an Honorary LLD from the University of Glasgow and had more than 180 scientific papers to his credit, the vast majority as senior or sole author (Nelson, Reference Nelson1977) (Fig. 2).

Fig. 2. In celebration of Leiper's work on schistosomiasis. (A) Cartoon sketch by Joy Gordon of his 1915 work in Egypt as part of his 1961 festscrift in Journal of Helminthology. (B) Black and White photograph of Leiper's collectors working in the small irrigation canals in Egypt foraging for snails where one might infer how arduous field-collecting can be in the midday sun.
LEIPER'S EARLY CAREER
Aged 24 and writing from Glasgow, on 28th December 1904 Leiper submitted his application to the London School of Tropical Medicine with testominals from R. Stockman (1861–1946), Robert Muir (1864–1959) and J. F. Gemmill (1867–1926). By his own admission he was more interested in the biological side of medicine and had taken full advantage of facilities at the Marine Biological Station at Millport, on the Isle of Cumbrae in Scotland. There he had pursued the study of parasitic worms, notwithstanding being the honorary librarian. Even as a keen student, he was particularly productive. He published his first paper in 1902 in Nature, a description of a parasitic flatworm (Avagina unicolor) found in the accessory canal of a sea-urchin. In his application, he was especially proud to report that as a Carnegie Medical Research Scholar and University Research Student in Embryology, he had been entrusted to conduct the examination of various trematodes, turbellarians and polychaetes brought back from the Scottish National Antarctic Expedition (SNAE) 1902–1904. The SNAE was led by W. S. Bruce (1867–1921) but was largely overshadowed by the concurrent Discovery Expedition 1901–1904 led R. F. Scott (1868–1912). By another helminthological twist of fate, the lives of Leiper and Scott were to be later intertwined with the lives of two others.
It was a good choice, perhaps, to have Stockman, Muir and Gemmill as referees and while Muir and Gemmill took much pleasure in their appraisals of him, Stockman commented “I can testify from personal knowledge that he is a competent clinician and pathologist. He has, however, devoted his time and energies chiefly to the study of Zoology and Embryology, and more particularly to the morphology and life-history of worms”. This might be lukewarm praise to some but to Manson it must have been just the ticket to appoint an ambitious, resourceful young man. On a more personal note, Leiper was reluctant to pursue a career in clinical medicine (Willmott, Reference Willmott1981). This was forged by the unhappy memory of his late father who had long suffered and died with tuberculosis which, at that time, had little in the way of prevention yet alone cure.
LEIPER'S FIRST EXPEDITIONS AND ACHIEVEMENTS
Whilst at the London School, Leiper did not disappoint. As teaching was delivered in discrete subject blocks there was ample time for travels abroad. Visiting the Gold Coast in 1905, he conducted experimental infections of primates to show how ingestion of infected Cyclops, the water flea harbouring Dracunculus medinensis, led to dracunculiasis and the transmission of Guinea Worm (Grove, Reference Grove1990). After proving this, he devised basic measures of prevention involving simple filtration of drinking water through cotton gauze. Largely as a result of this measure, Guinea Worm is now on the verge of eradication albeit new concerns of zoonotic transmission in Chad within a hitherto unknown infection reservoir in dogs (Callaway, Reference Callaway2016). Typical of Leiper he was often prophetic, in 1910 for example, he wrote a seminal paper discussing the role of domesticated animals in dracunculiasis transmission concluding that domestic dogs and horses were permissive hosts (Leiper, Reference Leiper1910).
In 1906 Leiper made his first visit to Egypt and performed studies on parasites, including schistosomes, in the Cairo School of Medicine within the laboratory of the eminent parasitologist Arthur Looss. It is worthy to note that in his later 1915 return, Leiper's ensconced himself within Looss's vacant laboratory, for Looss being German had to vacate Cairo at the start of WWI (Nelson, Reference Nelson1977). Whilst schistosomiasis was formally described decades before by T. M. Bilharz (1825–1862), the disease was firmly engrained in Egypt and had no known cure (Grove, Reference Grove1990). Moreover, its transmission was enigmatic and particularly puzzling and controversy raged concerning the significance of lateral and terminal spined eggs and how miracidia, the ciliated larval stage released from eggs, either infected people directly or was indirectly transmitted by an intermediate host (Farley, Reference Farley1991). Both opinions were complete conjecture but the latter would imply additional larval stages of unknown form and function (Cook, Reference Cook2007). Leiper's studies with Looss were inconclusive but they no doubt focused his mind on this biological conundrum, likely whetting his ambition to be the only man to solve it. There were of course several others pursuing similar investigations, such as the Brazilian M. A. Parajá da Silva (1873–1961) who had hotly debated the ‘second species’ with Looss and with whom he and Manson were in correspondence with (Katz, Reference Katz2008).
The following year Leiper had a more productive time as medical officer for the Egyptian Government Railway Survey operating between Lake Victoria and Lake Albert Uganda. There he was employed to look after the health of the survey teams but was much more interested in parasites of wildlife, finding a new species of liver fluke, Fasciola nyanzae, Leiper Reference Leiper1910, in a hippopotamus near Murchison Falls. He collected and described various other helminthological curiosities from elephants, on return to Egypt by way of the Nile.
Subsequently he fostered his interests in parasites in wildlife but now at home in the UK, where he was helminthologist to the Grouse Diseases Enquiry Committee (GDEC). Since the turn of the century there had been several mass die-offs of grouse, and other game birds, of sufficient calamity to warrant a national intensive investigation of its aetiology (Campbell, Reference Campbell1988). To this end, Leiper worked with E. A. Wilson (1872–1912) who was the field observer for the GDEC. Wilson was a medical doctor as well as a very talented natural historian and illustrator. Several years earlier, Wilson had accompanied Scott on the Discovery Expedition and was to continue with this strong Antarctic association in years to come. Concerning the epizooty in grouse, Wilson and Leiper were able to show, by experimental infections, that the nematode Trichostrongylus pergracilis was responsible for the periodic decimations (Nelson, Reference Nelson1977; Campbell, Reference Campbell1988).
ANTARCTIC PARASITES AND ASIAN SCHISTOSOMIASIS
Perhaps it was fate that Leiper would again study Antarctic parasites for Wilson was requested by Scott to act as his Chief Scientific Officer for the British Antarctic Expedition (BAE) 1910–1913. The BAE was informally known as the Terra Nova Expedition after the name of their ship, a coal-fired steam whaler. Woefully, both Scott and Wilson were to later perish, along with three others, on their ill-fated march to the South Pole. Once the details of their heroism became widely known, their demise was to subsequently inspire a tremendous future heritage of scientific exploration (Campbell, Reference Campbell1988).
A significant member of Scott's Terra Nova team was the Navy Surgeon E. L. Atkinson (1881–1929). Although younger than Leiper, only by several months, he and Leiper were known to have completely different and ill-fitting demeanours. ‘Atch’ as he was affectionately known by BAE staff, was employed both as expedition medical officer and parasitologist. It is outside the scope of this paper to describe Atkinson's unique talents, having been done admirably before (Nelson, Reference Nelson1977; Campbell, Reference Campbell1988), but suffice to say that after Scott's failure to return, he held the BAE together with remarkable fortitude and courage.
The BAE was foremost a scientific endeavour and thus Atkinson subsequently worked with Leiper at the London School to characterize the parasitic helminths he had collected, which resulted in an outstanding academic monograph recording 38 species (Leiper and Atkinson, Reference Leiper and Atkinson1915a ). Many of these species were novel and named in honour of their BAE colleagues (and their wives) (Campbell, Reference Campbell1988; Campbell and Overstreet, Reference Campbell and Overstreet1994). The history and associations with these names is particularly interesting and been previously discussed by William C. Campbell (the 2015 Nobel Laureate) and Robin M. Overstreet (Campbell and Overstreet, Reference Campbell and Overstreet1994). For example, unbeknownst to them the nematode Terranova antarctica, Leiper and Atkinson, which Atkinson had encountered from a gummy shark, was later shown to be a significant cause of anisakiasis in Japan (Campbell, Reference Campbell1988).
Although researching the parasitology of fishes the puzzle of Bilharzia was still in Leiper's mind as it was with other influential people at that time, such as Lord Horatio Kitchner (1850–1916), the British Administrator in Egypt. Lord Kitchner was to later put it “It was high time that serious steps should be taken to prevent the continuity of infection that has been going on so long in the country”. Bilharzia was also known to occur in China where it was a considerable problem within the British Navy, oddly enough in officers and not ordinary seamen, on their gunboats patrolling the Yangtze River (Hamilton Fairley, Reference Hamilton Fairley1951). By obtaining a grant from the Colonial Office through its Tropical Diseases Research Fund, Leiper and Atkinson were able to proceed to the Far East and investigate the mode of spread of Bilharziasis and, if possible, collect experimental evidence on this subject (Atkinson, Reference Atkinson1916).
What subsequently happened on this expedition to China and Japan is best told by George Nelson for he considers Leiper and Atkinson's (Reference Leiper and Atkinson1915 Reference Leiper and Atkinson b ) publication entitled “Observations on the spread of Asiatic schistosomiasis” a milestone in helminthology (Leiper and Atkinson, Reference Leiper and Atkinson1915b ); never in the whole history of parasitology have two men of such contrasting backgrounds and personalities collaborated to produce a paper that attracted so much attention (Nelson, Reference Nelson1977). In essence their time in the field did not go well and after suffering the company of Leiper, Atkinson who incidentally was once a champion boxer in the Navy, wanted to “…give him (Leiper) a sound thrashing and tell him what he is for the good of his soul and then leave him” for Leiper had typically everyone “by-the-ears” (Goodwin, Reference Goodwin and Cox1996). The poignancy should be measured by the gravity of which Atkinson had suffered in the Antarctic and was likely exhausted by always having to clear things up.
On a more positive note, they were able to follow the life cycle of S. japonicum linking miracidia to intermediate host (the snail Katayama nosophora), the internal sporocyst stages then to cercariae. It is this highly motile larvae stage, which is shed by snails into water and has a radically different morphology to miracidia, which is the infectious form to humans (Leiper and Atkinson, Reference Leiper and Atkinson1915b ). Thus it was the cercaria, not the miracidium, which was able to infect mammals by per-cutaneous transmission, or to cross the oral mucosa, which then went onto mature as an adult worm (male or female) within the bloodstream. Notably, they were only able to conduct these observations after Leiper made two short visits to Japan to seek advice from A. Fujinama (1870–1934). It was Fujinama who alerted him to the significant steps Japanese co-workers had already undertaken in elucidating the life cycle of S. japonicum publishing their work in Japanese journals (Goodwin, Reference Goodwin and Cox1996). These reports were largely outside the notice of the English speaking world (Tanaka and Tsuji, Reference Tanaka and Tsuji1997) and being clearly scooped, Leiper was understandably irate (Fig. 3).
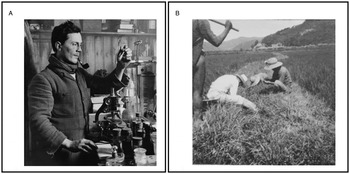
Fig. 3. Leiper's initial studies on Asian schistosomiasis with Atkinson. (A) Black and White photograph of Edward Atkinson in 1911 taken by Herbert Ponting (1870–1935) during his research on the Terra Nova expedition. Atkinson had recently suffered severe frost-bite on his hands and face, the remnants can be seen by his cheek scars and swollen right index finger. Upon his return to the UK, he worked with Leiper on his collection of parasitic worms from the Antarctic. (B) Black and White photograph of snail collecting in China along the marshes surrounding rice paddies.
AGAIN IN EGYPT AND ON A BREVET COMMISSION
With the outbreak of the first World War in 1914 and returning from China, Atkinson and Leiper went their separate ways with little further interactions; Atkinson to Gallipoli and later the Western Front while Leiper went again to Egypt. However, Leiper was now armed with knowledge of the S. japonicum life cycle. To fund his trip, The British War Office was immediately receptive to Leiper's application to resource this trip and appointed him as brevet Lieutenant-Colonel in the Royal Army Medical Corps to “Investigate Bilharzia disease in that country and advise as to the preventive measures to be adopted in connection with the troops”. As an aside, a good example of his diligence and the Leiper-effect on others is evidenced by his visit to the British Museum (Natural History). Before leaving for Egypt, he needed to seek confirmation of certain measurements of the Antarctic worms before their corrected monograph proof could be published. This was very much to the consternation of Baylis who was also very clearly had ‘by-the-ears’ (Fig. 4).
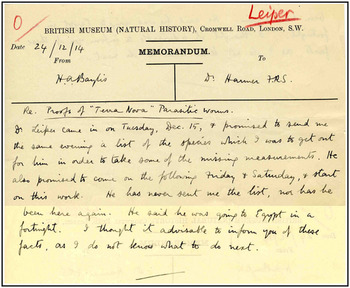
Fig. 4. Leiper unsettles Harold Baylis, for it was exceptional practice for British Museum (Natural History) staff to work on Saturdays. This note from Baylis to S.F. Harmer RFS (1862–1950) the Keeper of Zoology at the B.M.(N.H.) clearly shows how active Leiper could be pushing ahead the Terra Nova manuscript and how on Christmas Eve 1914 and Baylis was worried about the fuss Leiper might create if unsatisfied. Nevertheless, nearly half a century later Baylis was happy to sign Leiper's festscrift.
On this mission to Egypt Leiper, as Wandsworth Scholar, was accompanied by two other London School staff, J. G. Thompson (1878–1937), who was given a captaincy, and the London School's administrator R. P. Cockin (1889–1918). They arrived in Egypt on 8th February 1915 but soon encountered problems. These were reported back to Ronald Ross at the London School by Leiper who later wrote “Within a week of our arrival Dr Cockin had fallen sick and was invalided home. Three weeks earlier I had been admitted to hospital with scarlet fever. It was not until the beginning of April foregoing my convalescence, I was able to start field investigations at Marg. Early in May the opening of the Gallipoli campaign, with its rush of wounded and the attendant excitement in Cairo, brought pressing local suggestions for foreclosing of my mission”.
Thus nearly all of the early snail collecting therefore had fallen on the shoulders of Thompson who also wrote back to Ross saying that looking for snails in the canals and ponds “…was very exhausting work here in the sun especially travelling distances to search but it is extremely interesting”. Nonetheless, they were advantaged to focus on those snails that shed cercariae with characteristic bifurcate tails. Furthermore, with these cercariae it was possible to establish experimental infections in laboratory rodents and to follow the maturation of schistosomes within the vasculature system. Using the ova shed from these animals allowed experimental challenge and infection of laboratory-bred freshwater snails in order to identify clearly, which species were and were not permissive hosts (Cook, Reference Cook2007). Without doubt their progress was rapid and once sufficient field and experimental evidence had been accrued, Leiper left Egypt on 15th July 1915 to return to the London School. There he assembled all the information, and authored a clutch of sequential papers in the Journal of the Royal Army Medical Corps, which forms the backbone to our understanding of schistosomiasis today (Cook, Reference Cook2007).
ADOPTING SIMPLE MEASURES OF PREVENTION AND CONTROL
To his credit, Leiper had clarified beyond doubt that there were two species of African schistosome, S. haematobium and S. mansoni (Farley, Reference Farley1991). Each could now be clearly recognized by their characteristic egg-spine morphology in the excreta of infected hosts, which could also denote co-infection correcting Bilharz's original oversight. Although the species shared many commonalities in their life cycle, crucially they were each restricted in their development in Bulinus and Biomphalaria, respectively. This detail had much broader significance for the endemic zone of each species of schistosome was firmly tied to the distribution of their permissive snail host. Furthermore, from a public health perspective, destruction or removal of these intermediate hosts from the waterways could form an environmental intervention strategy of tremendous importance both in Egypt and China (Jordan, Reference Jordan2000). His seminal study also helped to develop a new field of medical malacology with key scientists such as C. A. Wright (1928–1983), G. D. Mandahl-Barth (1910–1994) and D. S. Brown (1935–2004) describing even greater complexities in the snail-schistosome relationship than he could have ever imagined (Lockyer et al. Reference Lockyer, Jones, Noble and Rollinson2004).
From a military perspective, knowing the life cycle and experimenting with ways to render water safe, Leiper made a variety of significant observations upon which camp standing orders were raised (Farley, Reference Farley1991). Adhering to these would ensure that troops would not be infected. Like his work on Guinea Worm, the water hygiene measures were based upon simple filtration, boiling water and use of disinfectants. Most importantly, knowing that cercariae are an ephemeral, short-lived larval stage, resting water for at least 24 h was sufficient to make it safe for bathing. These measures could be implemented without need for expensive equipment; all that was required was a little behavioural change prohibiting troops to swim or bathe in environmental water or to introduce simple hygiene measures when freshly drawn water was to be used (Farley, Reference Farley1991). Brilliantly, all that was needed to control schistosomiasis was to introduce a modicum of patience along with adequate temporary water storage.
With better knowledge of the life cycle and features of transmission the early clinical significance of the disease in soldiers could be more accurately described. For example, the eminent military physician Sir Neil Hamilton Fairley (1891–1966) helped to develop diagnostic tests based on complement fixation and later pioneered individual treatment with tartar emetic. Like the discovery of the life cycle, the first clinician to use intravenous tartar emetic successfully as an anti-schistosomal drug is controversial, ascribed in the UK to J. E. R. McDonagh (1881–1965) or in Egypt to J. B. Chistopherson (1868–1955). Nonetheless with Manson-Bahr, Fairley confirmed Leiper's experimental observations in rodents but now repeated in monkeys and his new descriptive pathology helped to shed fresh light on symptoms including: fever, urticarial, abdominal pain, enlargement of the spleen and liver, emaciation, bronchitis and diarrhoea (Hamilton Fairley, Reference Hamilton Fairley1951). From then on, the burden and fear within the British Army of schistosomiasis was greatly diminished (Farley, Reference Farley1991).
In local communities, however, schistosomiasis continued to flourish although future outbreaks within military settings did occur. An influential outbreak of acute schistosomiasis, or Katayama fever, in tens of thousands of the People's Liberation Army took place in 1949. By incapacitation, the Chinese amphibious assault on Taiwan (Formosa) was delayed sufficiently long enough to allow the US Seventh Fleet enter the Strait of Formosa and abort the communist takeover (Hotez, Reference Hotez2013). This made a deep impression on Chairman Mao, galvanizing a need to eliminate this disease in China. Despite a suite of interventions beginning in 1955, schistosomiasis has proven difficult to eliminate owing to its continued persistence involving zoonotic reservoirs (Zou and Ruan, Reference Zou and Ruan2015), as Leiper knew well (Nelson, Reference Nelson1990).
In 1951 Hamilton Fairley commented on the occurrence of schistosomiasis during WWII in Allied Forces when more than 1500 American Officers and 174 army personnel from the Royal Australian Air Force contracted S. japonicum. In his Presidential Address to the Royal Society of Tropical Medicine at Portland Place, London, and by all odds Leiper would have been in attendance, Hamilton Fairley surmised that it has taken another world war to make evident the difficulty of finding ova in the feces in mild and atypical schistosome infections and that the extent of subclinical army cases was still unknown (Hamilton Fairley, Reference Hamilton Fairley1951). More broadly, this summation is very relevant today. There is still a dearth of sensitive diagnostics, which has largely downplayed the clinical significance of disease, especially in children and women, when eggs are seemingly absent in the excreta (Stothard et al. Reference Stothard, Stanton, Bustinduy, Sousa-Figueiredo, Van Dam, Betson, Waterhouse, Ward, Allan, Hassan, Al-Helal, Memish and Rollinson2014b ).
SCHISTOSOMIASIS IN UGANDA TODAY
Perhaps Leiper would have been interested to learn how in areas where he once worked, in Uganda with the Egyptian Government Railway Survey, the disease is still causing havoc. On the Lake Albert shoreline, Butiaba and Pakwach, once essential ferry ports linking rail and road systems, are hyper-endemic foci for intestinal schistosomiasis. Since Leiper's visit, Butiaba and Pakwach have been the locations of numerous clinical epidemiological surveys for intestinal schistosomiasis (Nelson, Reference Nelson1958; Ongom and Bradley, Reference Ongom and Bradley1972; Kabatereine et al. Reference Kabatereine, Ariho and Christensen1992, Reference Kabatereine, OdongoAginya and Lakwo1996). Throughout this time efforts to control the disease have evolved being contingent with the changing emphasis of global strategies chiefly guided by the WHO and with available resources from international and national donors and agencies (Loewenberg, Reference Loewenberg2014). With the drive towards mass drug administration with praziquantel, the National Control Programme (NCP) for Control of Bilharzia and Intestinal Worms was launched in Pakwach in 2003 (Fenwick et al. Reference Fenwick, Webster, Bosque-Oliva, Blair, Fleming, Zhang, Garba, Stothard, Gabrielli, Clements, Kabatereine, Toure, Dembele, Nyandindi, Mwansa and Koukounari2009). The main intention of the NCP was to distribute and administer praziquantel annually to all children attending Universal Primary Education (UPE) schools in endemic areas (Stothard et al. Reference Stothard, Bustinduy and Montresor2014a ). At that time, Uganda was the first country to benefit from the support of the Schistosomiasis Control Initiative, using funds from the Bill & Melinda Gates Foundation, which purchased and donated praziquantel to the Ugandan Ministry of Health with its Vector Control Division as the lead agency overseeing the programme within country (Fenwick et al. Reference Fenwick, Webster, Bosque-Oliva, Blair, Fleming, Zhang, Garba, Stothard, Gabrielli, Clements, Kabatereine, Toure, Dembele, Nyandindi, Mwansa and Koukounari2009; Fleming et al. Reference Fleming, Fenwick, Tukahebwa, Lubanga, Namwangye, Zaramba and Kabatereine2009). The programme was also seminal for it helped to spearhead a new appraisal of this disease within this country by starting baseline surveys in 2002 with annual follow-ups that recorded a variety of disease-specific information and associated changes with treatment (Kabatereine et al. Reference Kabatereine, Brooker, Koukounari, Kazibwe, Tukahebwa, Fleming, Zhang, Webster, Stothard and Fenwick2007).
Since 2002, there has been a rich variety of research studies undertaken on the shoreline of Lake Albert and Victoria, inclusive of socio-demographic studies (Dunne et al. Reference Dunne, Vennervald, Booth, Joseph, Fitzsimmons, Cahen, Sturrock, Ouma, Mwatha, Kimani, Kariuki, Kazibwe, Tukahebwa and Kabatereine2006; de Moira et al. Reference de Moira, Kabatereine, Dunne and Booth2011; Stothard et al. Reference Stothard, Sousa-Figueiredo, Betson, Green, Seto, Garba, Sacko, Mutapi, Nery, Amin, Mutumba-Nakalembe, Navaratnam, Fenwick, Kabatereine, Gabrielli and Montresor2011) and medical malacology (Jorgensen et al. Reference Jorgensen, Kristensen and Stothard2007; Adriko et al. Reference Adriko, Standley, Tinkitina, Mwesigwa, Kristensen, Stothard and Kabatereine2013; Levitz et al. Reference Levitz, Standley, Adriko, Kabatereine and Stothard2013; Rowel et al. Reference Rowel, Fred, Betson, Sousa-Figueiredo, Kabatereine and Stothard2015). Collectively it is clear that control of schistosomiasis in these lacustrine environments is particularly challenging. Today, intestinal schistosomiasis is very firmly engrained in school-aged children, as well as pre-school children and the more obvious high-risk occupational groups such as adult fisherfolk (Seto et al. Reference Seto, Sousa-Figueiredo, Betson, Byalero, Kabatereine and Stothard2012). Domestic water supplies are typically contaminated with schistosome cercariae contributing to the failure of any viable alternative long term. This freshly drawn water is daily collected from the lake itself and used by all household members in their daily chores and ablutions, oblivious or contravening Leiper's advice (Stothard et al. Reference Stothard, Sousa-Figueiredo, Betson, Green, Seto, Garba, Sacko, Mutapi, Nery, Amin, Mutumba-Nakalembe, Navaratnam, Fenwick, Kabatereine, Gabrielli and Montresor2011; Seto et al. Reference Seto, Sousa-Figueiredo, Betson, Byalero, Kabatereine and Stothard2012).
With the increasing availability of donated praziquantel and the international drive towards reaching WHO 2020 targets, such as sustained treatment coverage of 75% in school-aged children, there is an expectation that schistosomiasis will significantly decline (Stothard et al. Reference Stothard, Bustinduy and Montresor2014a ; Savioli et al. Reference Savioli, Fenwick, Rollinson, Albonico and Ame2015). Our recent parasitological survey of school children across 5 primary schools in Buliisa and Hoima (Fig. 5), has little to foster such optimism. The fecal egg-patent prevalence and arithmetic mean intensity (eggs per gram [epg]) of intestinal schistosomiasis in three primary schools Runga, Walakuba and Biiso in 2003 was: 95·2% (631 epg); 90·4% (1026 epg) and 17·2% 52 (epg) while in 2015 was: 86·7% (1723 epg); 80·3% (814 epg) and 19·6% 198 (epg). Despite best efforts after a decade of control with school-based delivery of praziquantel treatment, there has been an intangible decline in egg-patent prevalence or intensity. Moreover, there are still many children with very heavy infections (>3000 epg). As treatment with praziquantel does not guard against reinfection, this is firm evidence that annual administration is insufficient and that short treatment cycles, given out twice or even three times a year, are needed.

Fig. 5. Malacological and parasitological studies in Uganda on the Lake Albert shoreline. (A) Sketch map of 10 collection points for Biomphalaria and associated location of 5 primary schools (Bugoigo, Walakuba, Runga, Biiso & Busingiro) examined for intestinal schistosomiasis in May 2015. Whilst Pakwach is located at the northern end of Lake Albert, the settlement of Butiaba occupies much of the peninsula indicated at snail collection site 4. The table denotes the number of snails collected and occurrence of snails shedding S. mansoni. (B) Ongoing water contact, contradictory to Leiper's advice, such as collecting water in yellow plastic jerry cans and washing clothes [inset] at Itutwe is still a common occurrence along the Lake Albert shoreline. While Bulinus and Lymnaea have been regularly collected from Itutwe since 2002, it was not until May 2015 that Biomphalaria has been encountered making this a possible transmission site away from the lakeshore and in need of further surveillance.
We are also still far from having a complete understanding of its full spectrum of morbidity and the consequences of associated vascular remodelling (Andrade, Reference Andrade2008). For example, in those with advancing hepatosplenic disease, progressive fibrotic sequelae in other organs and abdominal hypertension can occur and was recently discussed in connection with right ventricular endomyocardial fibrosis detected in a child at Walakuba (Bustinduy et al. Reference Bustinduy, Luzinda, Mpoya, Gothard, Stone, Wright and Stothard2014). This simply points towards the need for better clinical surveillance of the disease, in all its manifestations, at the periphery of primary health care else we will continue to observe only the tip of the iceberg (Stothard et al. Reference Stothard, Stanton, Bustinduy, Sousa-Figueiredo, Van Dam, Betson, Waterhouse, Ward, Allan, Hassan, Al-Helal, Memish and Rollinson2014b ). A potential solution is to expand access and administration of praziquantel to children younger than school-age who are currently not targeted for treatment. This is very firmly in line with the ethos of preventive chemotherapy, which aims to avert or stall the development of any morbidity but in the pre-school setting there are several impediments and bottlenecks to consider (Stothard et al. Reference Stothard, Bustinduy and Montresor2014a ). Only time will tell if this key treatment gap will be sufficiently rectified when an appropriate paediatric formulation of the drug is developed and deployed (Stothard et al. Reference Stothard, Sousa-Figueiredo, Betson, Bustinduy and Reinhard-Rupp2013).
INTRODUCING COUNTDOWN
The practical translation of many of Leiper's findings into tangible improvements in the health of neglected and impoverished populations of the world has been a long time coming (WHO, 2013). Effective control of schistosomiasis in sub-Saharan Africa is problematic and challenging (Southgate et al. Reference Southgate, Rollinson, Tchuente and Hagan2005; Rollinson, Reference Rollinson2009; Rollinson et al. Reference Rollinson, Knopp, Levitz, Stothard, Tchuente, Garba, Mohammed, Schur, Person, Colley and Utzinger2013). It clearly exposes several weaknesses in the health system as well as many deficits in our ability to respond comprehensively (Southgate et al. Reference Southgate, Rollinson, Tchuente and Hagan2005; WHO, 2015). The global response is being tracked as best possible by the neglected tropical disease score card, which seeks to measure progress in commitments and pledges made at the London Declaration on Tropical Diseases (WHO, 2015). Currently the score card places progress on schistosomiasis in red (see http://unitingtocombatntds.org/). Why is this? Put simply, the scale-up of access to praziquantel treatment has been much slower than expected. Currently those that are living in need of treatment are simply not receiving it and those that have access to treatment sometimes refuse to take it in fear of complications or side-effects for they have an incomplete understanding and awareness of the benefit of treatment (Parker et al. Reference Parker, Allen and Hastings2008; Parker and Allen, Reference Parker and Allen2011). There have been insufficient biosocial science studies undertaken to rectify this problem and enhance and sustain the performance of NCPs (Allen and Parker, Reference Allen and Parker2011; Rollinson et al. Reference Rollinson, Knopp, Levitz, Stothard, Tchuente, Garba, Mohammed, Schur, Person, Colley and Utzinger2013).
Addressing these deficits and needs requires implementation research that is able to provide evidence to expand, strengthen and sustain the delivery of treatment alongside complementary efforts that foster interventions against well-known attack points in the schistosome life cycle (Southgate et al. Reference Southgate, Rollinson, Tchuente and Hagan2005; Rollinson et al. Reference Rollinson, Knopp, Levitz, Stothard, Tchuente, Garba, Mohammed, Schur, Person, Colley and Utzinger2013). Traditionally this needs effective intersectoral dialogue and coordination of resources between, amongst others, the Ministries of Health, Education, Sanitation, Agriculture and Hydroelectricity (WHO, 2013). Responding to this need a 5-year implementation research consortium entitled COUNTDOWN was formed in November 2014 and funded by DFID, UK. The rationale of COUNTDOWN was to conduct research that would attempt to identify and alleviate bottlenecks in interventions and accelerate progress towards WHO 2020 targets for those neglected tropical diseases amenable to preventive chemotherapy (i.e. trachoma, lymphatic filariasis, onchocerciasis, soil-transmitted helminthiasis and schistosomiasis).
There are five overarching research themes within COUNTDOWN, three of which, the mass drug scale-up themes, operate across the four supported countries Liberia, Ghana, Nigeria and Cameroon and are focused on (1) evidence synthesis and Cochrane review, (2) applied social science and health system analysis studies and (3) health economics and financial forecasting. Two other research themes on integrated complementary strategies are specifically undertaken in Ghana and Cameroon and each address disease-specific aspects. For schistosomiasis this includes assessing the cost and impact of biannual praziquantel treatment, expanded access to groups, which are inadequately served (i.e. pregnant women and girls of reproductive age) and implementation of more sensitive diagnostics such as DNA detection methods to better describe the burden of schistosomiasis in those who otherwise do not have egg-patent infections (Stothard et al. Reference Stothard, Stanton, Bustinduy, Sousa-Figueiredo, Van Dam, Betson, Waterhouse, Ward, Allan, Hassan, Al-Helal, Memish and Rollinson2014b ).
A key deficit, which has immediately come to light is a fundamental disconnect and lacking dialogue within the health system linking women's reproductive health and sexual well-being with the prevention and management of female genital schistosomiasis (FGS) (Gyapong et al. Reference Gyapong, Marfo, Theobold, Hawking, Page, Osei-Atweneboanaa and Stothard2015). This has a wider significance as there is good evidence that FGS is a risk factor for sexually transmitted viruses such as HIV and HPV (Norseth et al. Reference Norseth, Ndhlovu, Kleppa, Randrianasolo, Jourdan, Roald, Holmen, Gundersen, Bagratee, Onsrud and Kjetland2014; Christinet et al. Reference Christinet, Calmy, Odermatt and O'Brien2015). Within COUNTDOWN, this is starting to be addressed with a comprehensive literature review on FGS (Christinet et al. Reference Christinet, Lazdins-Helds, Stothard and Reinhard-Rupp2016) and developing a social science research agenda, which will give increased voice to women's experiences of this manifestation of the disease linked with better epidemiological surveillance with modern diagnostic methods (Christinet et al. Reference Christinet, Lazdins-Helds, Stothard and Reinhard-Rupp2016).
ON LEIPER'S LASTING LEGACY
What would Leiper, the founder of modern helminthology, make of today's situation on schistosomiasis? Leiper was no stranger to raising international funds, so he would appreciate the tremendous effort and difficulty needed to mobilize and sustain control interventions by philanthropy. He would of course be saddened to see the links between schistosomiasis and agriculture decline, largely coincident with the demise of the Commonwealth Bureau of Helminthology but would be heartened to see the Centre for Agriculture and Biosciences International (CABI) and Journal of Helminthology still vibrant. He would be pleased to see the interdisciplinary nature of COUNTDOWN with an agenda determined in partnership with researchers from endemic countries but would be astonished to learn of the complexity behind the schistosome-snail relationship and that after a century, the world is still far from implementing his simple measures of prevention with total reliance on a single anthelminthic drug. As Leiper once put it to Buckley when asked for his advice, and to close, perhaps it was high time for him “to take another closer look”.
ACKNOWLEDGEMENTS
This manuscript results from a presentation on 8th January 2016 at the University of Glasgow held by the Wellcome Trust Centre for Molecular Parasitology (WTCMP) to celebrate ‘Glasgow Encounters with Tropical Diseases’. We thank several colleagues in the WTCMP, Professor Mike Barrett in particular, staff in the archives of the London School of Hygiene and Tropical Medicine, the Natural History Museum and the University of Glasgow for their help and access to materials concerning Robert Leiper's life. In addition, we acknowledge the help of several co-workers in Vector Control Division, Kampala who have assisted in research in Uganda over the years, as well as, general advice and support from colleagues within the COUNTDOWN consortium in particular Mark Taylor, Rachael Thomson, Sally Theobald, Nana Kwadwo-Biritwum, Mike Osei-Atweneboana, Ifeoma Anagbogu, Anthony Bettee and Karsor Kollie. J. R. S. would like to thank helpful colleagues over the year whilst based in the Natural History Museum, Vaughan Southgate, David Rollinson and David Gibson, especially the late David Brown, for sharing their humorous stories which have given flavour, impetus and desire to write this narrative on schistosomiasis and Leiper's contribution.
FINANCIAL SUPPORT
This work received no specific grant from any funding agency, commercial or not-for-profit sectors.
DECLARATION OF INTERESTS
J. R. S. is Director of the COUNTDOWN consortium and together with L. A. T. T. and M. G. received funding from DFID, UK to conduct implementation research on neglected tropical diseases.








