Perinatal depression is known to occur during pregnancy or the postpartum period and can affect one in seven women(1,2) . In addition, postpartum depression can occur within 4 weeks after childbirth and is characterised by depressive mood and loss of interest or pleasure in daily activities(Reference First3). Several systematic reviews and meta-analyses have indicated that postpartum depression negatively impacts infant cognitive development and bonding between mothers and infants(Reference Oyetunji and Chandra4). A recent cohort study has reported that women who experienced childbirth with postpartum depression had a higher rate of suicide and took a shorter time to suicide than those without postpartum depression during approximately 10 years of follow-up(Reference Lee, Tien and Bai5). Therefore, preventing postpartum depression is crucial for improving child and maternal health.
Several lifestyle factors may contribute to the development of postpartum depression. Countermeasures against lifestyle factors in pregnant and postnatal women may be an important strategy for improving postpartum depression(Reference Ghaedrahmati, Kazemi and Kheirabadi6). A scoping review of interventional studies has reported that nutritional and physical activity interventions may improve postpartum depression(Reference Yahya, Teng and Das7). According to a systematic review of systematic reviews and meta-analyses, several dietary factors, including high consumption of seafood, healthy dietary patterns, and multivitamin supplementation, may afford protection against postpartum depression(Reference Zhao and Zhang8).
Recently, reports on the association between the use of ready-made meals (RMM) or eating out (EO) and health-related outcomes have increased worldwide. Previous studies have defined RMM as prepackaged or takeout prepared meals available at grocery stores and fast-food restaurants(Reference Alkerwi, Crichton and Hébert9–Reference Profeta, Siddiqui and Smetana11) and EO as eating at restaurants, fast-food restaurants, and cafeterias(Reference Gesteiro, García-Carro and Aparicio-Ugarriza12). In addition, the Japan National Health and Nutrition Survey (NHNS) defines RMM as the use of takeaway food from supermarkets or convenience stores, while EO is defined as meals prepared at a restaurant or café(13). Previous studies have suggested that the consumption of RMM is related to the risk of obesity(Reference Alkerwi, Crichton and Hébert9) and that the frequency of EO is related to being overweight and other components of metabolic syndrome(Reference Gesteiro, García-Carro and Aparicio-Ugarriza12). Additionally, a higher frequency of RMM and EO use has been associated with lower vegetable and fruit intake(Reference Sweetman, McGowan and Croker10–Reference Gesteiro, García-Carro and Aparicio-Ugarriza12). Notably, RMM contain more Na(Reference Allemandi, Tiscornia and Ponce14) and lack protein(Reference Borkent, Beelen and Linschooten15). The Dietary Guidelines for Americans recommend paying attention to portion sizes and ingredients present in RMM to achieve a healthy dietary pattern and avoid excessive energy intake(16). Owing to changes in physical condition and lifestyle during pregnancy, pregnant women may face challenges in preparing meals. One cross-sectional study has suggested that pregnant women tend to use RMM high frequently (Reference Garnweidner-Holme, Torheim and Henriksen17). Thus, it is crucial to investigate the potential implications of RMM and EO in pregnant women to better clarify their associations with maternal health and well-being. Two cross-sectional studies have suggested that the frequency of EO is related to depressive symptoms among adults(Reference Yun, Kim and Lee18,Reference Zhang, Xie and Li19) . However, these studies lacked a longitudinal design, leaving the directionality of the association uncertain. Furthermore, no study has examined the association between the frequency of RMM or EO use and postpartum depression.
In 2019, the NHNS reported that the rate of eating a homemade meal among Japanese adults was 75·3 % for breakfast, 58·2 % for lunch and 73·6 % for dinner(13). Moreover, the NHNS 2019 reported that the frequency of using RMM once weekly was 47·2 and 44·3 % among males and females, respectively, while the frequency of EO once weekly was 41·6 and 26·7 % among males and females, respectively(13). Therefore, most Japanese adults consume homemade meals daily, although the use of RMM and EO is also common.
In the current novel study, we aimed to explore the association between the frequency of using RMM or EO and the incidence of postpartum depression after childbirth among community-dwelling pregnant women. In addition, we focused on the relationship between the frequency of using RMM or EO and food group intake.
Methods
Study population
Community-dwelling pregnant women in Ebetsu, Hokkaido, Japan, recruited between July 2019 and July 2022 were included in this study on baseline survey. The participants received a self-administered questionnaire along with a maternal handbook issued by a city health center or city government and were requested to complete the questionnaire during pregnancy and return it via mail. The participants were followed up from the baseline survey to after childbirth. Data on postpartum depression assessments were collected during a health check-up conducted at a medical institution from 2 weeks to 1 month post-childbirth. Data were confirmed by a public health nurse in the city health centre. This study was conducted in accordance with the guidelines of the Declaration of Helsinki, and the study protocol was approved by the Ethics Committee of Rakuno Gakuen University (2019, No. 19-1). Written informed consent was obtained from all the participants.
Data collection and measures
The frequency of RMM or EO use was determined based on single questions using the NHNS(13). RMM was defined as the use of takeaway meals obtained at supermarkets or convenience stores, and EO was defined as eating meals prepared at restaurants or cafés. The RMM and EO status have been determined using the NHNS since 2001; thus, the definitions of RMM and EO are well established among the Japanese population. Data on the frequency of eating RMM and EO were collected by asking participants to indicate their category (<1 time/week, 1–2 times/week, 3–4 times/week and almost every day) using self-administered questionnaires. Socio-demographic and socio-economic factors recorded were education (lower than high school, high school or above or unknown), marital status (married, divorced or unmarried) and current employment status (employed, maternity leave, unemployed or unknown). Data on household income were collected by asking participants to indicate the category of their estimated household income (<2 million JPY, 2–3·99 million JPY, 4–5·99 million JPY or ≥6 million JPY). Lifestyle factors included sleep duration, physical activity before pregnancy (>30 min of exercise twice a week or more: yes, no or unknown) and smoking status (current smoker, former smoker or never smoked). Information on sleep duration was obtained as a self-reported continuous variable and recorded as hours and minutes per day. The recorded results were converted into three categorical value ranges: <7 h/d, 7–8 h/d, >8 h/d or unknown. Participants provided information on receiving support for housework or childcare from partners or other family members using four possible responses: always supported, occasionally supported, hardly supported and never supported. The participants were then classified into two categories based on their responses: adequate support (always supported) and inadequate support (the other three responses). Dietary intake over the previous 1 month was assessed using a validated brief self-administered diet history questionnaire regarding the frequency of consumption of fifty-eight foods and beverages commonly consumed by the Japanese population. Total daily energy intake was calculated based on daily food intake information and the Japanese food composition table(Reference Kobayashi, Murakami and Sasaki20).
Depressive symptoms during pregnancy were assessed using the Japanese version of the Kessler 6 Scale (K6)(Reference Furukawa, Kawakami and Saitoh21). The K6 comprises six items on the symptoms of psychological distress, which are assessed on a five-point scale (0 = none of the time; 1 = a little of the time; 2 = some of the time; 3 = most of the time and 4 = all of the time). The total scores range from 0 to 24, with higher scores indicating a greater level of psychological distress(Reference Kessler, Andrews and Colpe22). The K6 has been administered to a representative nationwide cohort study conducted among Japanese women in the perinatal period(Reference Susukida, Usuda and Hamazaki23). The K6 score of 10 points or more indicates severe depressive symptoms in the Japanese population(Reference Sakurai, Nishi and Kondo24).
Outcomes
Postpartum depression was assessed using the Japanese version of the Edinburgh Postnatal Depression Scale (EPDS)(Reference Okano, Murata and Masuji25). The EPDS comprises ten items on maternal psychological distress, which are assessed on a four-point scale (0–3) for each item of questions(Reference Cox, Holden and Sagovsky26). The Japanese version of the EPDS is a valid measure for screening postpartum depression, and a cut-off point of 8/9 has a sensitivity of 0·75, specificity of 0·93, and detection of postpartum depression(Reference Okano, Murata and Masuji25).
Statistical analyses
We categorised the distribution of socio-demographic factors, lifestyle factors and food group consumption based on the frequency of using RMM or EO into three groups: <1 time/week, 1–2 times/week and ≥3 times/week. A logistic regression model was used to calculate the OR and 95 % CI of postpartum depression based on the frequency of using RMM or EO after adjusting for potential confounding factors. We selected confounding factors using an analytical framework for a directed acyclic graph(Reference Textor, van der Zander and Gilthorpe27), which applied a minimum adjustment model (online Supplementary Fig. 1). The multivariable-adjusted model included gestational week, marital status, household income and receipt of support from a partner at the baseline survey. A sensitivity analysis was conducted, excluding participants with severe depression with a K6 score of 10 or higher during pregnancy. All analyses were performed using the JMP Pro 12·1·0 software (SAS Institute Inc.). The level of significance was set at P < 0·05.
Results
A total of 2154 individuals were eligible for study participation. Among the 933 participants who returned the questionnaire, twelve participants who answered the questionnaire after giving birth were excluded. The remaining 921 female participants (42·8 %) were enrolled. Among these, participants who provided duplicate responses twice or more (n 29), those with missing data on the brief self-administered diet history questionnaire (n 1), those with less than 600 kcal or 4000 kcal, or more of total energy intake (n 18), those with a history of depression or other mental health illnesses (n 67), those who did not provide information on the frequency of using RMM (n 1) and those without an EPDS assessment during the post-birth checkup (n 166) were excluded from this study. Therefore, 639 participants were included in the final analysis.
The characteristics of the study participants, grouped based on the frequency of using RMM or EO during pregnancy, are presented in Table 1. Regarding the frequency of using RMM, 65·3, 28·0, and 6·7 % of participants were categorised into the none, 1–2 times/week and ≥3 times/week groups, respectively. Concerning the frequency of EO, 61·7, 36·0 and 2·3 % of the participants were in the none, 1–2 times/week and ≥3 times/week groups, respectively. Thus, the sample size of the group EO ≥ 3 times/week was the smallest. Participants who had a higher frequency of using RMM were currently employed than those with a lower frequency of using RMM. Additionally, participants with no EO use had a higher proportion of birth experience than those with a 1 time/week or more frequency of using EO.
Table 1. Characteristics of the participants grouped according to frequency of using ready-made meals or eating out during pregnancy

Data are presented as the mean and standard deviation or n (%).
Table 2 presents the total energy intake (kcal) and energy-adjusted food group consumption (g/1000 kcal) based on the frequency of using RMM or EO during pregnancy. Participants with an RMM frequency of ≥3 times/week had a lower intake of pulses, other vegetables, fish and eggs than those with an RMM frequency of <1 time/week and 1–2 times/week. Participants with an RMM frequency of 1–2 times/week and ≥3 times/week had a higher intake of fruits and confectioneries than those who had an RMM frequency of <1 time/week. Participants with an EO frequency of 1–2 times/week and ≥3 times/week had a higher fruit intake than those with an EO frequency of <1 time/week.
Table 2. Total energy intake and a consumption of food groups (g/1,000 kcal) according to frequency of using ready-made meals or eating out during pregnancy
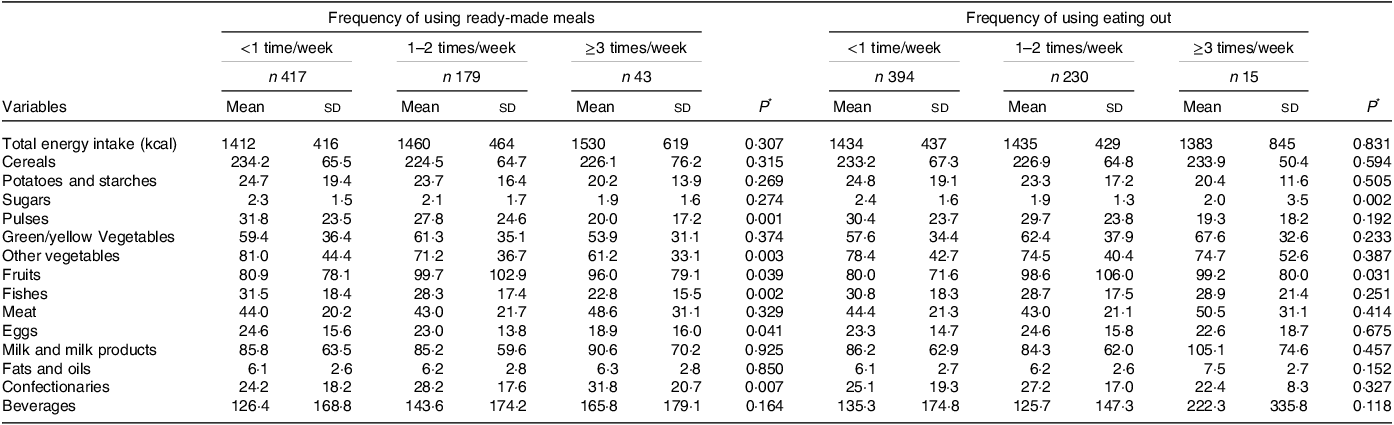
Data are mean and standard deviation.
* ANCOVA was performed to compare continuous variables and adjusted for gestation period, marital status, household income and support from partners and during pregnancy.
The OR and 95 % CI for the incidence of postpartum depression based on the frequency of RMM or EO are presented in Table 3. After adjusting for all related variables, there was limited evidence suggesting an association between consuming RMM 3 times/week or more and the likelihood of experiencing postpartum depression. The OR of postpartum depression in those who consumed RMM ≥ 3 times/week was the highest (4·16; 95 % CI: 1·68, 10·27, P for trend = 0·017) compared with those who consumed RMM < 1 time/week. In addition, there was no association between participants with EO use ≥ 3 times/week and postpartum depression, with an OR of 1·20 (95 % CI: 0·14, 10·04, P for trend = 0·283), compared with EO < 1 time/week. Upon repeating the sensitivity analysis by excluding participants with depression (K6 score ≥10) during pregnancy, the results were unaltered (online Supplementary Table 1).
Table 3. Odds ratio and 95 % confidence interval for postpartum depression according to frequency of using ready-made meals or eating out during pregnancy

* Participants with Edinburgh Postnatal Depression Scale score of ≥9.
** Adjusted for gestation period, marital status, household income and support from partners during pregnancy.
Discussion
In the current study, we analysed the risk of postpartum depression after childbirth among community-dwelling pregnant women grouped based on their frequency of using RMM or EO during pregnancy. We observed that participants consuming RMM ≥ 3 times/ week exhibited a higher incidence of postpartum depression than those consuming RMM < 1 time/week. Sensitivity analyses limited to participants without depression during pregnancy showed similar associations. To the best of our knowledge, this is the first study to suggest an association between the frequency of RMM use during pregnancy and the incidence of postpartum depression.
Herein, we detected a postpartum depression incidence of 6·3 % using the Japanese version of the EPDS, and the value during each survey year from 2019 to 2022 was 7·6, 7·2, 4·9, and 5·9 %, respectively (online Supplementary Table 2). The incidence of postpartum depression among our participants was less than the 9·0 % value observed 1 month after childbirth among another cohort of Japanese women(Reference Honjo, Kimura and Baba28). The lower incidence of postpartum depression in our cohort could be attributed to the lack of EPDS data for all participants and potential selection bias, such as participants being limited to healthy pregnant women.
Participants who frequently used RMM ≥ 3 times/week had a lower intake of pulses, other vegetables, fish and eggs, which was nearly consistent with that reported previously(Reference Sweetman, McGowan and Croker10–Reference Gesteiro, García-Carro and Aparicio-Ugarriza12). A systematic review has reported that healthy dietary patterns, such as those characterised by vegetables, fruit, nuts, fish and seafood, eggs and whole grains, may exert a protective effect against postpartum depression(Reference Silva, Cobucci and Gonçalves29), and a nationwide cohort study in Japan indicated that pregnant women with higher fish intake showed a lower incidence of postpartum depression(Reference Hamazaki, Matsumura and Tsuchida30). Furthermore, multivitamin supplementation, fish and PUFA intake, Ca, vitamin D and Zn may exert protective effects against postpartum depression(Reference Sparling, Henschke and Nesbitt31). These results support the findings of the current study. A recent large-scale prospective cohort study has indicated that women with postpartum depression have lower plasma anti-inflammatory cytokine levels than those without postpartum depression(Reference Ono, Yu and Obara32). Moreover, a meta-analysis reported that various anti-inflammatory foods, such as vegetables, fruits, and fish, may prevent depression(Reference Li, Chen and Yao33). Although the mechanisms underlying dietary inflammation and the incidence of depression are not completely clarified, the frequent use of RMM may be related to the occurrence of inflammation with a subsequent higher risk of postpartum depression.
A previous cross-sectional study has suggested that pregnant women tend to consume more RMM(Reference Garnweidner-Holme, Torheim and Henriksen17). Moreover, participants who frequently used RMM ≥ 3 times/week had higher rates of employment than those who consumed RMM < 1 time/week and 1–2 times/week. Therefore, it may be important to select RMM comprising healthy and diverse foods and pay attention to social lifestyles during pregnancy to improve dietary habits among pregnant women. Recently, the Japanese nutrition policy has been implemented to improve healthy food environments through restaurants and other settings(Reference Mochizuki, Kushida and Akamatsu34). Furthermore, research on 338 member companies of the Japan Ready-Made Meals Association reported that RMM suppliers in Japan developed menus referred to as Dietary Reference Intakes for Japanese, the Japanese Food Guide, and/or Healthy Japan 21(Reference Sakata35). However, companies should develop menus for RMM containing healthy and diverse foods and provide more publicity for pregnant women to select healthy menus. Previous systematic reviews have reported that healthy dietary patterns during pregnancy are associated with a lower risk of preterm birth(Reference Chia, Chen and Lai36). Consuming the Mediterranean diet, which is characterised by a high intake of fruits, vegetables, whole grain cereals, legumes, fish and nuts, during pregnancy has been associated with a lower risk of gestational diabetes in mothers and congenital defects in offspring(Reference Amati, Hassounah and Swaka37). Therefore, a healthy diet during pregnancy can contribute to both maternal and infant health outcomes.
In the present study, the frequency of EO was not significantly associated with postpartum depression. The sample size of the group using EO ≥ 3 times/week was small, and the data were inadequate to examine the association between the frequency of EO and postpartum depression. Therefore, the association between the frequency of EO and postpartum depression warrants further investigation.
The present study has several strengths. First, this study was undertaken to explore the association between the frequency of RMM or EO and postpartum depression in pregnant women using the data of community-dwelling pregnant women. Second, the survey had a longitudinal design, which aided in considering the direction of the association between the frequency of RMM or EO during pregnancy and postpartum depression. Third, sensitivity analysis was conducted to exclude participants with depression during pregnancy, which reinforced the validity of our results.
Nevertheless, the limitations of the current study need to be addressed. First, we only collected data on the frequency of RMM and EO; quantitative data on the types of foods containing RMM and EO were not obtained. However, we assessed dietary intake using a validated brief self-administered diet history questionnaire and estimated the effect of food group consumption based on the frequency of RMM or EO on postpartum depression. Second, the present study limited EPDS assessment from 2 weeks to 1 month after childbirth, and we did not clarify the long-term effect of the frequency of using RMM on postpartum depression. Third, the frequency of eating RMM and EO may have been affected by the COVID-19 pandemic. Several previous studies have reported that people have increased(Reference Profeta, Siddiqui and Smetana11) or decreased(Reference Scarmozzino and Visioli38) their frequency of using ready-to-use meals during the COVID-19 pandemic. However, in the present study, the frequency of RMM and EO did not differ significantly in each survey year (online Supplementary Table 2). Finally, the relatively small sample size and low response rates could have limited the incidence of postpartum depression, potentially impacting the statistical power of the analysis. Therefore, further studies with larger sample sizes and longer-term observational designs are warranted.
In conclusion, the current study demonstrated that the frequent use of RMM during pregnancy is related to an increased risk of postpartum depression. This study sample was limited to Japanese pregnant women, necessitating further studies in large and diverse samples to overcome potential selection bias.
Acknowledgements
We thank the staff of the Health Center and Department of Health and Welfare of Ebetsu City for their cooperation and assistance during the course of this study.
This study was supported by a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan (grant number JP19K19465).
T. K. conceived the research and designed a project. T. K. drafted the manuscript, and R. K. and E. O. reviewed and edited the manuscript. T. K. conducted data curation and an analyses. All authors have read and approved the final manuscript.
There are no conflicts of interest.
Supplementary material
For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S0007114524001545






