Acardiac twin or twin reversed arterial perfusion (TRAP) sequence is a rare complication of monochorionic twinning. It is a special form of twin-to-twin transfusion syndrome. When one twin is dead or acardiac, there is an anomalous reversal of umbilical arterial flow from the pump twin to the acardiac twin, via a placental arterio-arterial anastomosis.
The acardiac twin acts as a parasite that is hemodynamically dependent on the pump twin, and it is usually amorphous and hydropic. This threatens the survival of the pump twin by stealing blood, finally leading to heart failure, fetal death, polyhydramnios and preterm birth. While the acardiac twin is unable to survive, the pump twin is associated with a high mortality rate, as many as 50% in case of no therapeutic intervention (Moore et al., Reference Moore, Gale and Benirschke1990). To improve the survival rate of the pump twin, many interventions to interrupt arterial flow to the acardiac twin have been used, with a high success rate, such as alcoholization (Sepulveda et al., Reference Sepulveda, Sfeir, Reyes and Martinez2000; Tongsong et al., Reference Tongsong, Wanapirak, Sirichotiyakul and Chanprapaph2002), radiofrequency ablation (Hirose et al., Reference Hirose, Murata, Kita, Aotani, Takebayashi and Noda2004; Lee et al., Reference Lee, Wagner, Sy, Ball, Feldstein, Goldstein and Farmer2007), detachable coils (Tanawattanacharoen et al., Reference Tanawattanacharoen, Manotaya, Wacharaprechanont, Uerpairojkit, Tannirandorn and Charoenvidhya2004) and glue occlusion. Such techniques have the same principle of arterial occlusion of intrafetal arterial flow. The occlusion certainly gets rid of the parasitic reservoir, eventually leading to a decrease in volume load or cardiac load. However, the occlusion can also have a negative impact on hemodynamics of the pump twin, possibly resulting in fetal loss. Theoretically, hemodynamic changes after the procedure are as follows: (1) Acute pressure load: once the artery of the acardiac twin is occluded, fetal hypertension or an increase in afterload develops acutely, resulting in pressure load to the heart. (2) Acute volume load: venous return from the acardiac twin occurs but cannot flow back because of the occlusion; the acardiac twin is no longer a blood reservoir, resulting in hypervolemia in the surviving twin. The twin encounters both pressure and volume load acutely. The pump twin has to adapt itself to pass through this critical time without residual insults. Theoretically, the fetus takes a high risk for decompensation or heart failure, and it is unclear whether the occlusive procedures are truly safe or not. Also, acardiac twin pregnancies are a fascinating model for fetal hemodynamic flow study, and how the fetal heart can cope with the emergent situation has never been explored. Therefore, in this study, we aimed to comprehensively assess the fetal hemodynamic adaptions to the occlusive procedures.
Methods
A prospective descriptive (case series) study was conducted on monochorionic twin pregnancies complicated with an acardiac twin, attending the Maternal-Fetal Medicine (MFM) unit at Maharaj Nakorn Chiang Mai Hospital (a tertiary center and teaching school) between January 2010 and December 2020. The study was carried out with ethical approval by the Institutional Review Boards of the Faculty of Medicine, Chiang Mai University, and the patients provided written informed consent. Inclusion criteria were (1) monochorionic twin pregnancies diagnosed with acardiac twin, (2) gestational age in the second trimester, (3) demonstration of fetal hydropic signs (fluid collections in the third space) in the surviving twin and (4) consent from the couples to have occlusive procedures. Four techniques of occlusive procedures were available, including alcoholization, radiofrequency ablation, Guglielmi detachable coil embolization and n-butyl cyanoacrylate occlusive glue. The details of these techniques are described elsewhere (Hirose et al., Reference Hirose, Murata, Kita, Aotani, Takebayashi and Noda2004; Lee et al., Reference Lee, Wagner, Sy, Ball, Feldstein, Goldstein and Farmer2007; Tan & Sepulveda, Reference Tan and Sepulveda2003; Tanawattanacharoen et al., Reference Tanawattanacharoen, Manotaya, Wacharaprechanont, Uerpairojkit, Tannirandorn and Charoenvidhya2004; Tongsong et al., Reference Tongsong, Wanapirak, Sirichotiyakul and Chanprapaph2002).
Comprehensive hemodynamic assessments were performed at six points on a timeline: just before the procedures, shortly after the procedures (1−4 h), then 12, 24, 48 h and 1 week after the occlusive procedures. The results of assessments, which were prospectively recorded, included fetal heart rate, Tei index of the left ventricle together with isovolumic contraction time (ICT) and isovolumic relaxation time (IRT), fetal middle cerebral arterial−peak systolic velocity (MCA-PSV), ductus venosus Doppler including preload index (S-a/S), umbilical artery Doppler (pulsatility index and systolic/diastolic [S/D] ratio), the presence of umbilical venous pulsations, cardio-thoracic diameter ratio (CTR) and shortening fraction of the left and right ventricle. The procedures were performed under ultrasound guidance. All ultrasound scans were performed by the MFM specialists, using Voluson E8 and Voluson E10 machine (GE Healthcare Ultrasound, Milwaukee, WI), equipped with transabdominal 2–4 MHz curvilinear transducers.
Baseline characteristics or demographic data were recorded on the day of diagnosis or intervention. All attended standard antenatal care clinics, and follow-up ultrasound scans were also performed every 2−4 weeks. Pregnancy outcomes were prospectively collected.
The main outcomes to be evaluated were hemodynamic parameter changes after the procedures.
Results
Baseline data of the patients are presented in Table 1. The median (range) gestational age of intervention was 21 (17−26) weeks of gestation. The interventions to interrupt the circulation of acardiac twins included alcoholization in four cases (median procedural time 9.0 min; range 7.0−11.0 min), radiofrequency, helical coils and glue in one case each (procedural time 35, 26, and 12 min, respectively). Instantaneous complete occlusion was observed in two cases (no. 1 and no. 7; Figure 1), which were occluded with alcholization and glue, respectively.
Table 1. Baseline characteristics and outcomes of pregnancies
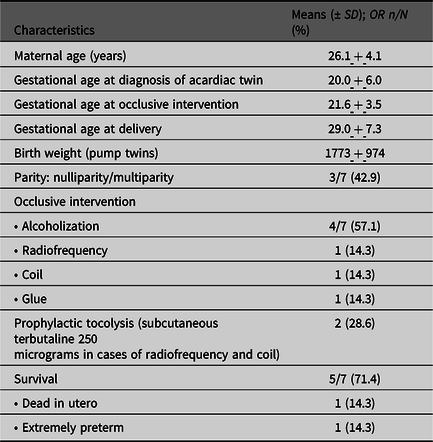

Fig. 1. Hemodynamic parameters at various points of time lines (0: before the procedures, 1: shortly after procedure; 2:12 h; 3:24 h; 4:48 h; 5: 1 week after procedure)
Prior to the occlusive procedures, although all were hydropic, cardiac function of the pump twins (Tei index, shortening fraction, and afterload) was within normal limits. However, blood volume and cardiac output were higher than 95th percentile, and MCA-PSV showed some degree of anemia (median: 1.4 multiples of median [MoMs]; 1.23−1.74 MoMs). The preload index was within a normal limit in most cases except for cases no. 2 and no. 7, which had a preload index of greater than the 95th percentile (Figure 1). Cases no. 2 and no. 7 also had a relatively high Tei index but within normal limits (Figure 1).
After occlusive procedures, hemodynamic changes were as follows:
-
Afterload reflected by UA-S/D ratio was significantly increased (p < .05) shortly after occlusion, but the change was temporary. The afterload after 24 h after occlusion was not significantly different from that before the procedures (excluding cases no. 2 and no. 7).
-
The Tei index tended to be temporarily increased. Nevertheless, the two cases (cases no. 2 and no. 7) with preexisting increased preload had a persistently increased Tei index of greater than 95th percentile values.
-
IRT was significantly prolonged and more pronounced than ICT. In the cases of successful outcomes, IRT and Tei index return to preocclusion levels in 24−48 h. However, cases no. 2 and no. 7 had a persistent high Tei index and were followed by prolonged bradycardia, with recovery in case no. 2 and death in case no. 7.
-
Shortening fraction between 6 and 24 h was significantly decreased in only two cases whereas the remainder had no significant change. The two cases also showed a Tei index greater than the 95th percentile and a high preload index. They were diagnosed with heart failure; case no. 2 had a spontaneous recovery with some residual insults ending with fetal distress but survived, while case no. 7 progressively ran down until death in utero.
-
Preload index in ductus venosus Doppler and shortening fraction was not significantly changed in all cases except the two cases of heart failure as mentioned earlier.
-
One week after the procedures, anemia represented by MCA-PSV tended to improve without blood transfusion but was not statistically significant (0.88−1.23 MoM compared to 1.23−1.74 MoMs before occlusion).
-
In most cases, as an example, case no. 5 is presented in Figure 2 shortly after occlusion; hemodynamic changes are mainly secondary to increased volume load and pressure load, leading to an overworked heart. However, the overworked state is temporary, and the pump twin can cope with the critical situation without residual insult by an effective compensatory mechanism of fluid balance. Because there was no longer parasitic circulation, the volume load and hydropic changes prior to occlusion finally disappeared.
-
In cases of preexisting compromise, as an example, case no. 7 is presented in Figure 3; the occlusion can aggravate cardiac function and deteriorate the hemodynamics leading to heart failure or even death in utero during the critical period.
-
In summary, the hemodynamic change may be illustrated as presented in Table 2 and Figure 4.

Fig. 2. Case 5 shows mild deterioration of hemodynamics shortly after the occlusive procedure (A: shortening fraction; B: Tei index; C: ductus venosus Doppler; D: umbilical artery Doppler)
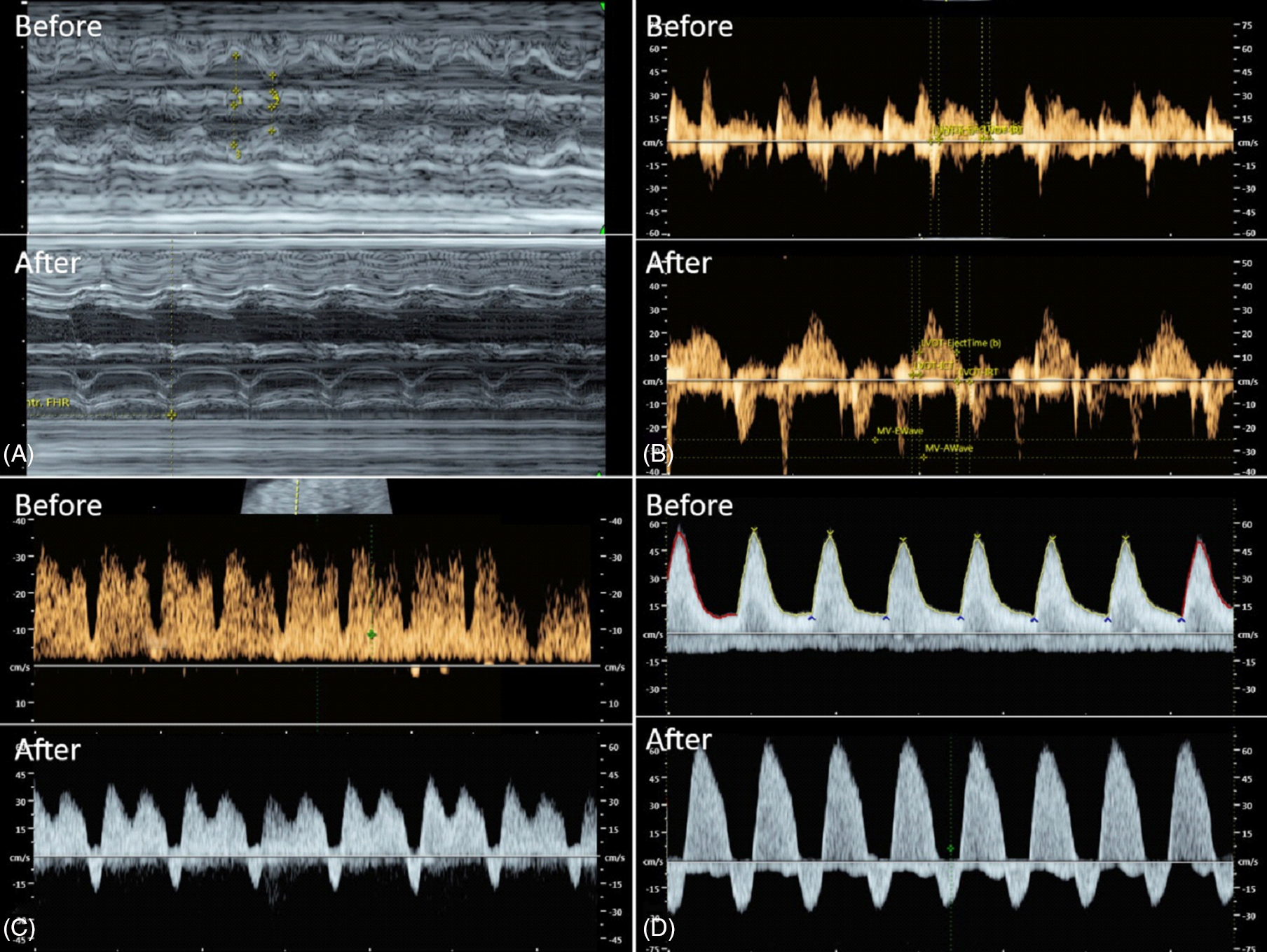
Fig. 3. Case 7 shows marked deterioration of hemodynamics shortly after the occlusive procedure (A: shortening fraction; B: Tei index; C: ductus venosus Doppler; D: umbilical artery Doppler)

Fig. 4. Schematic drawing shows circulation of acardiac twin and effects of occlusion
Table 2. Hemodynamic changes during various time periods
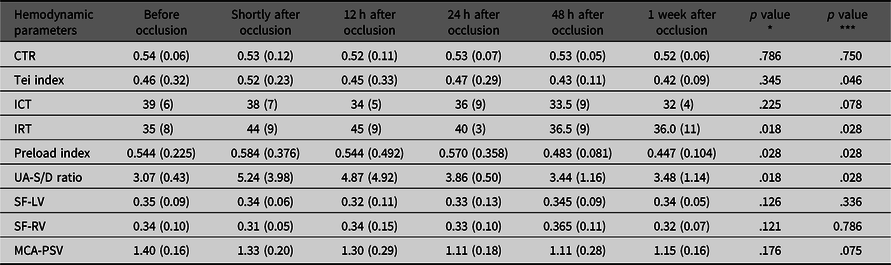
Note: The number presented as medians and interquartile range are in parenthesis; *compared between before occlusion and shortly after occlusion; **compared between shortly after occlusion and 1 week after occlusion.
CTR, cardio-thoracic ratio; ICT, isovolumetric contraction time; IRT, isovolumetric relaxation time; MCA-PSV, middle cerebral artery – peak systolic velocity; SF-LV, shortening fraction of the left ventricle; SF-RV, shortening fraction of the right ventricle; UA-S/D, umbilical artery – systolic/diastolic flow ratio.
Discussion
This is the first report of a comprehensive study of fetal hemodynamics in response to acute increase in pressure load together with volume load, using acardiac twins as a study model.
The pump twin is usually anemic, associated with volume overload because of blood reservoir in the parasitic twin. The fetal heart is overworked to maintain tissue oxygen perfusion by increased heart size and cardiac output. The definitive treatment is interruption of the blood flow to feed the acardiac twin. The main purpose of occlusive procedures is to cut the blood reservoir, eventually leading to a decrease in cardiac overload. Nevertheless, just after the occlusion of arterial flow, the volume overload in the pump twin can be even more aggravated by one-way venous return from the acardiac twin. Also, the arterial occlusion causes an increase in afterload and cardiac pressure load. The pressure load is acutely increased, different from a gradual increase, as seen in the case of placental insufficiency in singleton. The elapsed time, from occlusive procedure to the complete clearance of excessive volume, returning to normovolemia, is a critical period due to both volume load and pressure load, which places the heart at a higher risk of failure.
Before the procedures, hydrops fetalis in the pump twin was hypothetically caused by anemia, and hypervolemia leading to extravasation of fluid to interstitial spaces, as well as probable congestive heart failure, was believed to occur, though this might occur at the end stage of the overworked heart. We have noted that they were hydropic, but Tei index, shortening fraction, preload index and cardiac output were within normal limits, in spite of high blood flow in central venous system. Although the heart was overworked, it worked well, without heart failure. However, heart failure may develop after prolonged exposure to volume overload. The most important new knowledge from this study is that just after occlusion, the volume load and pressure load can aggravate the previously overworked heart, which may fail. Note that shortly after intervention, two cases gradually developed poor performance index, shortening fraction, and increased preload in the ductus venosus.
Notably, the case with heart failure and death in utero had complete occlusion and immediate absence of blood flow in the acardiac twin. This might be associated with acute pressure load, leading to cardiac decompensation as well as increased preload, and a decrease in shortening fraction and increased Tei index. Another new insight is that hydrops is not the predictor of success rate, but preexisting hemodynamic impairment plays a major role in prognosis. In other words, preload index, Tei index and shortening fraction can be prognostic factors. The two cases with heart failure had abnormal preload together with a relatively high Tei index prior to the procedures, and just after the procedures they had progressive change to absent or reversed DV a-wave, ending with heart failure. All of the five cases with normal preload resulted in good outcomes, though all already had hydropic signs before the procedures.
We observed that before occlusion, all fetuses tended to have anemia, based on MCA-PSV of 1.23–1.74 MoM, consistent with low hematocrit levels. Nevertheless, all of the surviving fetuses no longer had anemia after a period of adaptation at 1 week after occlusion (MCA-PSV: 0.88–1.23 MoM). The finding suggests that after interrupting parasitic circulation, volume load gradually improved with increasing hemoglobin levels, together with the disappearance of hydropic signs associated with gradual clearance of excessive fluid.
Of note, case no. 2 developed heart failure after occlusion, but hemodynamic adaptation after passing the critical period (first 24 h) resulted in clearance of the excessive volume load and decreased afterload, leading to the disappearance of the hydropic signs and restoration of cardiac function, whereas the other one with heart failure was progressive to death.
Prior to occlusive intervention, in the pump twin, ICT seems to be greater than IRT, suggesting increased systolic function secondary to anemia, in agreement with relatively high MCA-PSV. Interestingly, shortly after the procedure, IRT was prolonged, possibly reflective of diastolic function secondary to pressure load. IRT was the main component causing an increase in Tei index after occlusion. At follow-up scan 1 week after the procedure, anemia spontaneously improved and IRT seemed to be normal.
This study suggests that prognostic factors of cardiac failure after occlusion might be the impending heart failure prior to occlusion, increased preload and abnormally high Tei index. However, if the fetus can get through the most critical period, 24 h after procedures, good outcomes may be expected. Clinically, evaluation of cardiac function before occlusion is informative for counseling and predicting the outcomes. This study suggests that occlusive procedures should be performed before deterioration of cardiac function, and is more important than the presence or absence of hydrops fetalis.
The weaknesses of this series are as follows: (1) the sample size was small; (2) baseline characteristics (cardiac function, gestational age of the procedures) were heterogeneous; (3) different techniques of obstructive procedures were used; (4) there was no a long-term follow-up.
The strengths include: (1) prospective and longitudinal monitoring after the procedures; (2) comprehensive hemodynamic parameters were assessed.
Certainly, no solid conclusion can be drawn from this small series. Several observations from this series enable us to form a reasonable hypothesis concerning fetal hemodynamics, and these observations suggest ideas or directions for further studies to explore.
Clinical Impact
When an acardiac twin is detected, serial ultrasound should be closely followed up. Hypothetically, conservative treatment can be provided as long as no sign of cardiac compromise is identified. It must be emphasized that the occlusion could aggravate the compromised heart to failure.
Conclusion
Responses to occlusive procedures are as follows: (1) Tei index tends to be temporarily increased, mainly caused by prolonged IRT rather than ICT. (2) The severity is varied, probably depending on several factors, especially cardiac compromise prior to occlusion and degree of acute obstruction (complete or partially). (3) The occlusion can aggravate the overworked heart, leading to heart failure (poor shortening fraction, abnormally increased Tei index, low cardiac output) and death. (4) Most cases could successfully cope with increased volume load and pressure load, which was most pronounced in the first 6−24 h. (5) Shortly after the procedure, IRT seems to be prolonged, possibly reflective of diastolic dysfunction secondary to pressure load. At the follow-up scan 1 week after the procedure, anemia spontaneously improved and IRT seemed to be normal. (6) Prior to occlusion, ICT was likely greater than IRT, suggesting increased systolic function secondary to anemia, in agreement with relatively high MCA-PSV. (7) Volume and pressure load can be completely corrected by fluid balance mechanism after cutting the parasitic circulation, though this process may take some time period after occlusion. (8) Clinically, an occlusive procedure should be offered before impairment of cardiac function. Finally, normal fetal Tei index cannot exclude subtle cardiomyopathy. Fetal cardiomyopathy has increasingly been recognizable as an important prognostic factor for complicated monochorionic twins (twin-to-twin transfusion syndrome, twin anemic-polycystic syndrome) undergoing in-utero treatment.
Acknowledgments
We would like to express our gratitude to MFM team who helped us in patient recruitment and collecting data.
Author contributions
KT: Conceptualization, obstetric management, manuscript draft, final approval; SL: fetal echocardiography, obstetric management, final approval; FT: fetal echocardiography obstetric management, final approval; KS: Fetal echocardiography, obstetric management, final approval; TT: Conceptualization, fetal echocardiography, manuscript revising, final approval.
Financial support
The Thailand Research Fund (DPG6280003), Chiang Mai University Research Fund (CMU-2564).
Conflict of interest
None.
Ethical standards
This study received ethnical approval from the institute review boards of Faculty of Medicine, Chiang Mai University (Ethics Committee 4; Study Code: OBG-2564-08013 / Research ID: 8013).








