CLINICIAN’S CAPSULE
What is known about the topic?
A majority of syncope patients are transported to the emergency department by emergency medical services (EMS), yet only a small proportion are admitted or suffer serious adverse events (SAE).
What did this study ask?
What proportion of EMS syncope patient transports are at low risk (i.e., absence of EMS interventions, hospitalization, and SAE)?
What did this study find?
This prospective cohort study found that 40% of syncope transports are at low risk.
Why does this study matter to clinicians?
This group of patients represents potentially avoidable transports once a clinical decision tool is developed with a substantial opportunity cost for EMS systems.
INTRODUCTION
Syncope, defined as a sudden transient loss of consciousness followed by spontaneous complete recovery, accounts for ∼1% of all North American emergency department (ED) visits.Reference Thiruganasambandamoorthy, Taljaard and Stiell1, Reference Moya, Sutton and Ammirati2 A recent Canadian study showed that 70% of syncope patients arrived by ambulance,Reference Thiruganasambandamoorthy, Hess and Turko3 but only 17% were admitted and 9.7% suffered serious adverse events (SAE) within 30 days. This discrepancy between the number transported and the proportion hospitalized or suffering an SAE suggests that many syncope patients are at low risk and may not benefit from emergency medical services (EMS) care.
In modern EMS systems, paramedics assess patients at the scene, transport them to increasingly crowded EDs, and endure offload delays until ED stretchers are available. In some jurisdictions, treat-and-release protocols for conditions like hypoglycemia and supraventricular tachycardia allow EMS providers to assess and discharge select patients without transporting them.Reference Minhas, Vogelaar and Wang4 Although the likelihood of SAE is higher in syncope, a validated decision tool, which does not yet exist, could reduce EMS transports and enable low-risk diversion to more appropriate care settings.
Our objective was to estimate the proportion of syncope patients transported to the ED by ambulance who are at low risk based on an ED diagnosis of vasovagal syncope and the absence of EMS intervention, hospitalization, and SAE at 30 days. We also sought to describe EMS interventions in this cohort.
METHODS
Setting and patients
This prospective cohort study, a substudy of the Risk-Stratification of adult ED Syncope (RiSEDS) study, was conducted at five large Canadian EDs (Ottawa Hospital Civic and General campuses – Ottawa, ON; Kingston General Hospital and Hotel Dieu – Kingston, ON; University of Alberta Hospital – Edmonton, AB) from February 2012 to February 2013.Reference Thiruganasambandamoorthy, Stiell and Sivilotti5 Patient demographics, medical history, and disposition were collected within the RiSEDS study, along with EMS-identified SAE, EMS interventions, and ED diagnosis. ED physicians screened consecutive patients presenting with syncope, pre-syncope, fainting, blackout, loss of consciousness, fall, collapse, seizure, and dizziness or light-headedness. Patients≥16 years of age who met the definition of syncope and were transported to the ED by ambulance were eligible. Previously enrolled patients and those with any of the following were excluded: pre-syncope, persistent altered mental status, alcohol or drug intoxication, witnessed seizure, or loss of consciousness following head trauma. Patients whose syncope caused a head injury were included, but those who sustained major trauma requiring hospitalization were excluded because of difficulty determining whether outcomes were due to syncope or trauma. The Hospital Research Ethics Boards approved the study without requirement for written consent.
Outcome measures
We defined “low-risk” syncope patients as those who received no EMS intervention, were discharged from the ED with a diagnosis of vasovagal syncope, and experienced no SAE within 30 days. EMS interventions were identified in EMS call reports, hospitalizations based on hospital records, and final ED diagnosis was a specific field on the RiSEDS data form. We conducted 30-day telephone follow-up to identify other healthcare visits, new diagnoses, interventions, and SAEs.
SAEs included any of the following within 30 days as per published reporting guidelines: death, dysrhythmia, myocardial infarction, serious structural heart disease, aortic dissection, pulmonary embolism, severe pulmonary hypertension, subarachnoid hemorrhage, significant hemorrhage, or procedural interventions to treat a cause of syncope.
Analysis
Means and standard deviations (SD) are reported to describe continuous variables and frequencies with proportions for dichotomous variables. Sample size was based on the larger RiSEDS study.Reference Quinn, Stiell and McDermott6
RESULTS
Figure 1 shows that ED physicians at five study sites enrolled 1,473 patients with true syncope: 990 (67.2%) were transported to the ED by ambulance, and 54 patients (5.5%) were lost to follow-up. Of these (see Figure 1/Appendix A), 505 (51%) had vasovagal syncope, and, after exclusion of 41 patients with no 30-day follow-up data, 393 (39.7%; 95%CI 36.6, 42.8) were at low-risk – potentially appropriate for alternative management based on their diagnosis and the absence of EMS intervention, hospitalization, or 30-day SAE.
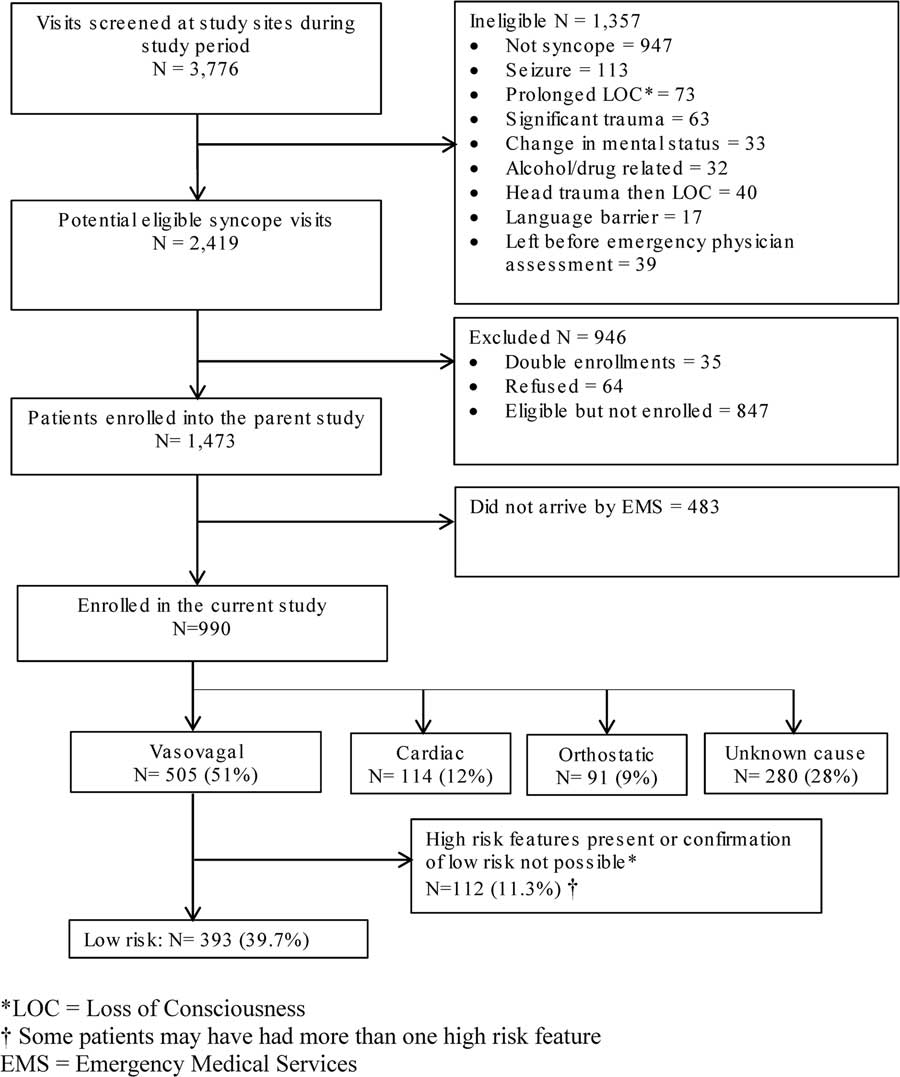
Figure 1 Selection of patients for the study.
Table 1 shows that mean age was 58.9 years (SD, 23.1) and 543 patients (54.9%) were female. The most common ED diagnosis was vasovagal syncope (51.0%) and 166 patients (16.8%) were hospitalized during the index visit. Paramedics provided one or more interventions for 121 patients (12.2%). One underwent transcutaneous pacing, and 38 received cardiac medications, including acetylsalicylic acid (ASA) or aspirin (n=20), nitroglycerine (n=13), atropine (n=4), and metoprolol (n=1). Sixty-two received symptom-relief medications, including dimenhydrinate (n=41), morphine (n=9), metoclopramide (n=4), ondansetron (n=3), fentanyl (n=3), ketorolac (n=1), and diphenhydramine (n=1). Seventeen received glucose for suspected hypoglycemia, and 1 received midazolam for a suspected seizure (although physicians subsequently confirmed that all suffered true syncope). Thirty underwent spinal or extremity immobilization for injuries.
Table 1 Patient characteristics (N=990)
Table 2 shows that 137 (14.6%; 95%CI 12.4, 16.9) patients suffered an SAE within 30 days. Of these, 32 (3.4%) were detected by EMS, 58 (6.2%) during ED evaluation, and 47 (5.0%) within 30 days of ED disposition. SAEs included 9 (0.9%) deaths, 63 (6.7%) dysrhythmias, 32 (2.9%) other cardiac outcomes, and 35 (3.5%) non-cardiac events.
Table 2 Serious adverse events (SAE) occurring within 30 days

* Five total during ED evaluation (two sepsis, one acute renal failure, one ectopic pregnancy, one pleural effusion), six total after ED disposition (one aseptic meningitis, one cerebrovascular accident, one partial small bowel obstruction, one appendicitis, one bilateral subdural hematoma, one sternal osteomyelitis).
† One death attributed to myocardial infarction, one to atrial fibrillation, and seven to unknown causes.
DISCUSSION
Limitations
Patients were recruited from large urban EDs and their affiliated EMS systems, and our findings may not generalize to other practice settings. Emergency physicians did not complete study forms for 847 eligible syncope patients; however, these were of similar age and gender to those enrolled, suggesting selection bias is unlikely. Fifty-three patients were lost to follow-up, but they were younger (mean age, 43.6), more often vasovagal (77.4%), and none were hospitalized during their index visit, making them a lower-risk group. Study diagnoses were based on discharge diagnoses documented by ED physicians, and it is unclear whether an EMS provider could achieve similar diagnostic differentiation based on limited information available at the scene.
Although we identified a large opportunity cost for EMS systems, with 40% of syncope transports being potentially avoidable, we did not conduct a formal economic evaluation. Future studies should conduct cost-benefit analyses and examine the potential impact of a clinical decision tool, particularly on offload delays.
CONCLUSION
We found that 40% of syncope patients transported to the ED by ambulance are at low risk, representing a substantial target for avoidable EMS transports and an opportunity for resource conservation. These patients had vasovagal syncope, did not require EMS intervention or hospitalization, and did not experience an SAE within 30 days. Our findings, consistent with other studies,Reference Thiruganasambandamoorthy, Hess and Turko3, Reference Quinn, Stiell and McDermott6–Reference Birnbaum, Esses and Bijur9 suggest the need for a decision tool to identify low-risk patients unlikely to benefit from EMS transport who are candidates for diversion to alternative care settings or rapid offload to low-acuity ED care locations. Such a tool could reduce EMS workload and cost, mitigate offload delays, and improve the utilization of an increasingly precious resource – the monitored ED stretcher.
The Ontario government recently proposed legislation to expand paramedic scope of practice, allowing non-ED options such as primary or community-based care.Reference Hoskins10 Our findings suggest that syncope represents an important candidate condition for an EMS treat-and-release or treat-and-refer protocols; however, these must be accurate and sensitive enough to identify a small number of patients who might experience short-term serious outcomes. Such pathways might involve urgent follow-up by a family physician or rapid access clinic, and presupposes accessibility of such care. However, additional work is needed to determine whether a decision rule is feasible and can be reliably incorporated into EMS practice.
Acknowledgements
We gratefully acknowledge all of the emergency physicians at The Ottawa Hospital – Civic and the General campuses, Kingston Health Sciences Centre, and University of Alberta Hospital who recruited the patients and the emergency medicine residents who helped in this process. We also gratefully acknowledge the emergency medical services providers and organizations (Regional Paramedic Program for Eastern Ontario, Emergency and Transportation Services – County of Frontenac, and Emergency Medical Services – Alberta Health Services) for providing the Ambulance Call Reports. We also thank the following members of our research team: Ottawa site – Pam Ladouceur, RN; Sarah Gaudet, RN; Karen Pratt, RN; Dr. Aparna Vaidyanathan, MBBS; Soo-Min Kim, BScH; My-Linh Tran; Sheryl Domingo; and Angela Marcantonio; Kingston site – Jane Reid, RN; Vi Ho, MD; Laura Goodfellow, R; and Vlad Latiu, MD; and Edmonton site – Justin Lowes, BSc; Danielle DeVuyst, RN; Pamela Pang, RN; and Natalie Runham, RN.
Funding: This study was supported by Physicians’ Services Incorporated Foundation, Canadian Institutes of Health Research and Ontario Innovation Fund for Academic Health Sciences Centres of Ontario through The Ottawa Hospital Academic Medical Organization (TOHAMO). Dr. Rowe is supported by Canadian Institutes of Health Research (CIHR) as a Tier I Canada Research Chair in Evidence-based Emergency Medicine through the Government of Canada (Ottawa, ON), and Dr. Thiruganasambandamoorthy is supported by the Jump Start Resuscitation Scholarship and currently holds the National New Investigator Salary Award through the Heart and Stroke Foundation of Canada.
Competing interests: None declared.
SUPPLEMENTARY MATERIALS
To view supplementary material for this article, please visit https://doi.org/10.1017/cem.2018.464





