Given the unprecedented global nature of the COVID-19 pandemic and its enormous costs across emotional, health-related, and economic domains, there has been considerable concern over the likely mental health sequelae of this worldwide disaster. Reference Niederkrotenthaler, Gunnell and Arensman1,Reference Ruiz and Gibson2 More specifically, a marked increase in suicidal thoughts, behavior, and deaths was anticipated. Reference Niederkrotenthaler, Gunnell and Arensman1,Reference Farooq, Tunmore, Wajid Ali and Suicide3 Indeed, many studies have shown a pandemic-related increase, both in mental health distress in general Reference Manchia, Gathier and Yapici-Eser4 and suicidal thoughts and behavior. Reference Farooq, Tunmore, Wajid Ali and Suicide3,Reference Sahoo and Patra5 However, the research has not been consistent, with some studies showing either no change relative to pre-pandemic levels Reference Isumi, Doi and Yamaoka6,Reference Pirkis, John and Shin7 or even a decrease. Reference Pirkis, John and Shin7–Reference Irigoyen-Otiñano, Porras-Segovia and Vega-Sánchez9 Three possible reasons for these discrepant findings include (1) use of inadequately sensitive markers of suicidal risk Reference Rogers, Richards and Cao10 ; (2) variation in the severity of the impact of the pandemic across individuals and countries Reference Sahoo and Patra5,Reference Isumi, Doi and Yamaoka6,Reference Orui, Saeki and Kozakai8 ; and (3) the possible time-sensitive nature of the mental health impact. Reference Sahoo and Patra5,Reference Pirkis, John and Shin7,Reference Irigoyen-Otiñano, Porras-Segovia and Vega-Sánchez9,Reference Tsai, McCleery, Wynn and Green11 Thus, to reach a fuller understanding of the impact of the global pandemic on suicide risk, it is critical to address all 3 factors.
The Suicide Crisis Syndrome (SCS)
Within the clinical setting, the most common method to assess patients’ suicide risk involves querying about suicidal ideation (SI), Reference Høyen, Solem and Cohen12,Reference Ribeiro, Franklin and Fox13 such that intervention decisions are largely dependent on the patients’ self-report of such ideation. Unfortunately, suicidal ideation has considerable disadvantages as a predictor to actual suicide risk. For one, although the history of SI remains a potent risk factor for suicidal behavior, 14 the rate of SI is perhaps 650 times higher than the rate of suicide deaths. Whereas the cross-national lifetime rate of suicidal ideation was estimated to be about 9.2% and of suicidal attempts to be 2.7%, Reference Nock, Borges and Bromet15 the 2021 rate of suicide deaths in the United States was 0.014%. 16 Thus, it is difficult to determine the level of acuity for any individual reporting SI, pointing to the need for additional risk assessment methods. Secondly, SI is transient, highly variable, and can occur only moments before the actual suicide attempted. Reference Deisenhammer, Ing and Strauss17 Thirdly, SI can only be assessed through self-report, the reliability of which is highly compromised by either underreporting (eg, due to embarrassment, fear of hospitalization, or fear of occupational repercussions) or overreporting (eg, in pursuit of secondary gain). Reference Høyen, Solem and Cohen12,Reference Berman18 Finally, SI can also have a chronic or waxing and waning course and therefore give a poor indication of imminent suicidal risk. Reference Kleiman, Turner and Fedor19
The suicide crisis syndrome (SCS), currently under consideration for inclusion in DSM-5-TR as a suicide-specific diagnosis, describes an acute, hyperaroused, cognitive-affective state, driven by a sense of entrapment. Reference Cohen, Imbastaro and Peterkin20 Importantly, while SI may accompany the SCS, it is not a criterion of the syndrome. The SCS has 2 criteria. Criterion A involves a sense of frantic hopelessness/entrapment and Criterion B has 4 components: affective disturbance, loss of cognitive control, hyperarousal, and social withdrawal. The SCS and its earlier iterations have shown construct validity via confirmatory factor analysis Reference Bloch-Elkouby, Barzilay and Gorman21 ; criterion validity with SI, suicidal attempts (SA), and suicidal thoughts and behavior (STB) Reference Bloch-Elkouby, Barzilay and Gorman21–Reference Yaseen, Hawes, Barzilay and Galynker25 ; predictive validity to near-term SI, SA, and STB Reference Bloch-Elkouby, Barzilay and Gorman21–Reference Cohen, Mokhtar and Richards23 ; and incremental predictive validity to SA after accounting for SI Reference Rogers, Vespa, Bloch-Elkouby and Galynker26 and SI plus depressive symptoms. Reference Yaseen, Hawes, Barzilay and Galynker25 Measures of the SCS have also been validated in multiple countries and in multiple languages. Reference Otte, Lutz and Streb24,Reference Høyen, Cohen and Solem27–Reference Wu, Lee and Rogers29 Furthermore, SCS symptoms were more tightly linked to stressful life events experienced during the pandemic than were SI. Reference Rogers, Richards and Cao10
Suicide Risk During the Pandemic
Unsurprisingly, a number of studies have shown an increase in suicide risk during the pandemic. Reference Farooq, Tunmore, Wajid Ali and Suicide3,Reference Pirkis, John and Shin7,Reference Orui, Saeki and Kozakai8 Likewise, in a large (N = 24 378) online, cross-sectional survey study of Chinese university students, mandatory quarantined status was positively associated with self-harm/suicidal ideation (OR = 4.98). Reference Pirkis, John and Shin7 Further, in a systematic review by Farooq et al., common contributors to suicidal ideation across international studies included loneliness, financial strain, academic stress related to quarantine, and physical and mental exhaustion, particularly in health care workers. Reference Farooq, Tunmore, Wajid Ali and Suicide3
In contrast, several other studies report different findings, such that risk appeared to either remain the same or even decline. In a study of data from 21 countries, suicide rates decreased in 12 countries or regions in the early months of the pandemic. Reference Pirkis, John and Shin7 Seven regions showed an increase, mainly small, and the remaining regions showed no change. Similarly, Orui et al. reported an increase in national suicide rates in Japan but a decrease in areas affected by the 2011 tsunami. Reference Orui, Saeki and Kozakai8 Thus, local conditions appear to impact the response to the trauma of the pandemic. Likewise, in a Spanish study of emergency room (ER) visits pre and post lockdown, there was a decrease in both the number of visits to the ER and in patients presenting with suicidal behavior in the initial 3 months of the pandemic. Reference Irigoyen-Otiñano, Porras-Segovia and Vega-Sánchez9 The authors speculated, however, that suicide risk might change over time as the pandemic persisted. Likewise, a whole population-based study from Wales showed a decrease in suicide rates during the pandemic along with an increased rate of deaths of unknown cause. However, they also showed a widening all-cause mortality gap in individuals with an index incident of self-harm compared to matched controls. Reference Lee, Han, Kim and Kwak30 This study points to the possible confound of disruptions in accurate record keeping during the pandemic as well as to the importance of assessing risk over time.
Thus, the actual impact of the pandemic on suicidal risk may vary considerably depending on temporal features, such as length of time exposed to pandemic parameters. Accordingly, research has shown differential responses to acute versus chronic stress, such that people tend to rally under acute stress but then show greater distress under chronic stress. Reference Giessing, Oudejans and Hutter31,Reference McGonagle and Kessler32 Further, as the experience of the pandemic and the associated government responses will vary across both individuals and countries, it is important to consider how the severity of pandemic parameters, such mandatory lockdowns and death and case rates, may impact suicidal risk. Finally, while studies drawn from public databases are useful for assessing epidemiological rates of death by suicide, they are limited in their ability to assess psychological states that indicate suicide risk. This is important because, unlike completed suicides, identification of pre-suicidal psychological states provides opportunity for targeted interventions.
With these concerns in mind, the present study investigated the relationship between severity and length of time exposed to key parameters of the COVID-19 pandemic (eg, time under lockdown, magnitude and time since peak number of cases and deaths) and SCS across 10 different countries, using an online survey study.
Specifically, we predicted that rates of SCS would be higher in countries with higher peak daily cases and deaths and in individuals who have been exposed longer to pandemic markers (eg, to national lockdowns). Of note, this study focuses only on the first wave of the pandemic, prior to the introduction of vaccines, effective treatments, and other factors that may have reduced the pandemic’s detrimental psychosocial effects.
Methods
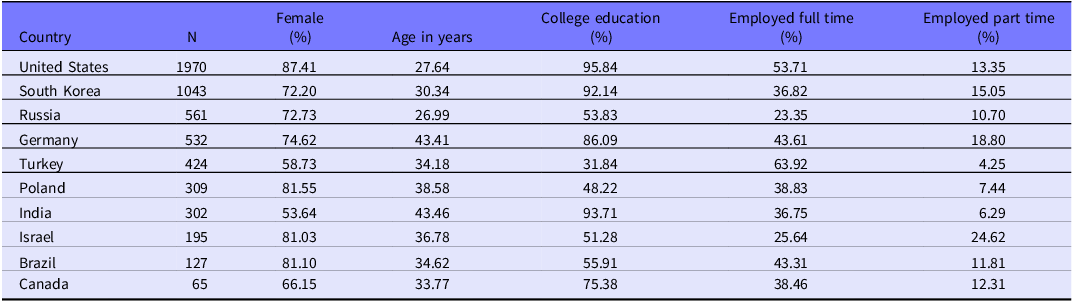
Participants were a convenience sample of 5528 adults (Mage = 30.99 years, SD = 12.44, range = 18 to 89 years) who completed an online survey assessing emotional reactions, including suicidal symptoms, during the COVID-19 pandemic. Participants were recruited from 10 countries (Brazil: n = 127; Canada: n = 65; Germany: n = 532; India: n = 302; Israel: n = 195; Poland: n = 309; Russia: n = 561; South Korea: n = 1043; Turkey: n = 424; and the United States: n = 1970). Participants were required to be 18 years or older and live in one of the collaborating countries during the COVID-19 pandemic. There were no exclusion criteria. Most participants self-identified as cisgender women, single/never married, and had completed college/university (Table 1).
Table 1. Demographic data per country
Participants were recruited via postings on social media platforms from June 2020 to January 2021. Prior to data collection, survey batteries were translated into each site’s appropriate languages, using an iterative process. Reference Sousa and Rojjanasrirat33 Each measure underwent forward and blinded backward translations by 2 bilingual translators. Consensus meetings were held to address disagreements and finalize translations.
Anonymous survey links guided participants to an online platform (Qualtrics). Turkey also utilized paper copies of self-report questions, and responses were manually added to the online platform. Upon providing electronic or written informed consent, participants answered a battery of questions. Most countries did not provide monetary compensation. The South Korean sample was offered direct payment, and participants in the United States were entered into a cash prize lottery. Every study component was approved by relevant institutional review boards or institutional ethics committees from the principal investigators’ institutions.
Measures
COVID-19 variables
The date and number of peak daily cases and peak daily deaths for each country were obtained from the World Health Organization (WHO) 34 and dates of local and national lockdowns and COVID-19 recommendations from the British Broadcasting Corporation (BBC). 35 The terms lockdowns and recommendations are defined by the BBC as follows: “Some of the more common approaches have seen governments issue recommendations on social distancing for part or all of the country, while others have acted to restrict all non-essential internal movement. The latter is often called a lockdown.” All COVID-19 information pertains to each country’s first wave as depicted graphically in the WHO charts and occurred between December 2019 and January 2021. National lockdown data were available for 4 countries (Germany, India, Poland, and Russia); national recommendation data for 7 countries (Canada, Germany, India, Poland, Russia, South Korea, and the United States); and local lockdown data for 6 countries (Brazil, Canada, Germany, India, Russia, and the United States). As local recommendation data were only available for 2 countries (Brazil and South Korea), these data were excluded from further analyses.
Variables used in the analyses included:
-
1. Two nationwide indicators of COVID-19 severity: peak daily cases and peak daily deaths per 100 000 people. Since all participants from the same country had the same value for each of these variables (eg, all 1970 participants from the United States have the same peak daily case and peak daily death rate), they are termed nationwide severity variables.
-
2. Five individually based time-course variables reflect the time in days from the onset of critical COVID-19 markers (peak daily cases, peak daily deaths, national lockdown, national recommendations, and local lockdowns) to survey completion for each participant. The first 2 variables reflect disease parameters and the next 3 reflect government responses to the pandemic. Though participants in the same country shared the COVID-19 marker (eg, date of national lockdown), the completion date of each participant varies. Hence, the days varied across individual participants, for example, from national lockdown to study participation. We, therefore, refer to these variables as individual time-course variables. As all participants entered the study after their country’s date of peak cases, all time-course variables had positive values.
Suicide Crisis Inventory—2 (SCI-2) Reference Bloch-Elkouby, Barzilay and Gorman21
The SCI-2 consists of 61 self-report questions that evaluate the severity of SCS symptoms grouped into 5 domains: entrapment, affective disturbances, loss of cognitive control, hyperarousal, and social withdrawal. Participants reported how intense each symptom was over the last several days on a 5-point Likert scale ranging from 0 (“Not at all”) to 4 (“Extremely”). The SCI-2 has demonstrated excellent internal consistency plus strong convergent and discriminant validity. Reference Bloch-Elkouby, Barzilay and Gorman21 Based on our original validation study with psychiatric patients, participants who scored 164 or above were considered to screen positive for SCS, and those who scored below 164 to screen negative. In this sample, 17 participants were missing SCI data.
MINI for Suicidality Disorders Studies 7.0.2 Reference Sheehan, Lecrubier and Sheehan36
The MINI is a self-report questionnaire that identifies lifetime and past month SI and behaviors with non-overlapping time periods. The reliability and validity of the MINI have been established. History of suicide attempts was assessed with a binary variable (yes/no) and recorded for both lifetime and past month.
Data Analysis
Initial analysis included inspection for normality, confirmation of the association between the SCI and MINI suicide attempt items, and assessment of intercorrelations between COVID-19 variables. In primary analyses, the 2 nationwide COVID-19 severity variables were compared across participants who were SCS positive or not, using independent sample median tests (due to non-normal sample distribution for variables before and after data transformation). The 5 individually based time course variables were also compared across SCS status, using independent t-tests. To account for possible demographic differences across countries, these last comparisons were repeated, covarying for demographic variables (sex, age, education), using logistic regression. These variables were included in multivariable analyses as they have been previously associated with suicidal and general mental health risk Reference Berkelmans, van der Mei, Bhulai and Gilissen37 and are easily comparable across countries. Sex compared self-identified female respondents to a collapsed category of non-female, including male (2358; 42.7%) plus transgender/non-binary/unsure/decline (N = 77; 1.4%) as gender diversity was not assessed consistently across countries. Education was coded as a binary variable marking the presence/absence of college education.
Due to the nature of web-based surveys, most study participation occurs within a very narrow window, at the launching of the survey, or when reminder links are posted. Because the dates of study participation within individual countries’ data sets, therefore, lacked adequate variability, a separate examination of the individually based time course variables for each country was not feasible. For example, in the US subsample (N = 1970), 63.8% of the sample participated on 3 dates just 15 days apart (October 27, 2020, October 28, 2020, and November 11, 2020), although data collection occurred over 6 months. In the pooled sample, however, the variability for the time course data was much improved, allowing for valid analyses.
Results
Descriptive Analyses
In the total sample, 584 respondents (10.6%) scored at or above the cut-off of 164 on the SCI-2. Incidence ranged from 3.6% (Israel) to 15.2% (Poland). See Table 2.
Table 2. Time course variables a and SCS rates per country
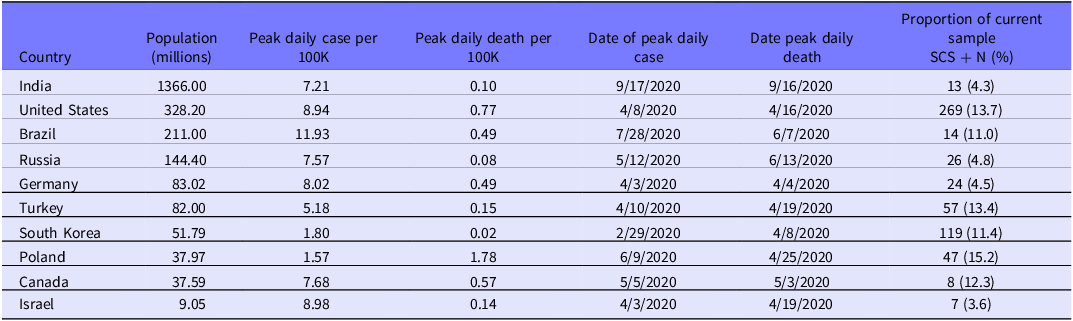
a COVID-19 data adapted from the WHO34; SCS, suicide crisis syndrome.
Case and death rates
The dates of the first case reported were relatively similar across countries, with the earliest reported on January 19, 2020 (United States), and the latest on March 4, 2020 (Poland). In the first wave of the pandemic, however, the dates of peak daily cases varied across countries, with the earliest date recorded on February 29, 2020 (South Korea), and the latest on September 17, 2020 (India). Dates of peak daily deaths also varied across countries, the earliest on April 4, 2020 (Germany), and the latest on September 16, 2020 (India). The mean peak daily case per 100 000 people across countries was 6.89, with a range of 1.57 (Poland) to 11.93 (Brazil). The mean peak daily death per 100 000 people was 0.46 with a range of 0.02 in South Korea to 1.78 in Poland. See Table 2.
Time frame of lockdowns and recommendations
National lockdowns commenced in a short time frame. Germany had the earliest date of national lockdown on March 23, 2020, and Russia had the latest on March 28, 2020. The onset of localized lockdowns also occurred in a very short time frame: March 11, 2020, for Russia and March 25, 2020, for Canada. The dates of national recommendations ranged from February 23, 2020 (South Korea), to March 19, 2020 (India). See Table 3.
Preliminary Analyses
Normality of distribution
Neither of the 2 nationwide COVID-19 variables fit a normal distribution by Kolmogorov–Smirnov tests and data transformation did not improve normality. Given the restricted range of the nationwide severity variables, that is, only 10 values, 1 for each country, it was necessary to use non-parametric tests with these data. For the 5-time course values, Kolmogorov–Smirnov tests showed acceptable levels of skewness (−0.282 to −0.519) and kurtosis (−0.700 to 0.018), and a visual examination of the plots for these variables indicated normality. Hence, we elected to use parametric tests for these variables.
Criterion validity of the SCS in relation to suicide risk
To confirm the construct validity for the SCI-2 as a marker of suicide risk in this sample, we assessed the relationship between total SCI-2 score and history of suicide attempts. Participants who endorsed both lifetime (N = 570) and past month (N = 48) suicide attempts had higher SCI-2 scores than those who did not, with large effect sizes (Mann–Whitney U test = 834330.5, standardized test statistic = −15.96, P < 0.001 for lifetime; Mann–Whitney U test = 212348.5, standardized test statistic = 7.4, P < 0.001 for past month). Thus, these data support the construct validity of the SCS as a marker of suicide risk.
Intercorrelations between COVID-19 variables
As expected, all COVID-19 individual time course variables were highly intercorrelated (r = 0.346–0.999). Nationwide severity variables were also highly intercorrelated (rho = 0.645–0.950), and 14 out of 20 correlations between nationwide severity and individually based time course variables were significant at rho > 0.20. Hence, we elected to analyze all COVID-19 variables separately to avoid potential collinearity. Additionally, due to the recency of the COVID-19 pandemic and the preliminary nature of our understanding of its psychosocial impact, it is useful to examine each factor individually.
Primary Analyses
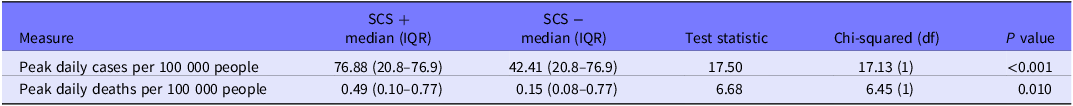
Bivariate analyses
As shown in Table 4, SCS status was significantly related to peak daily cases and peak daily deaths per 100 000 people in independent sample median tests. In other words, people who scored above the cut-off for the SCS lived in countries with a higher peak of daily cases and daily deaths during the first wave of the pandemic than those who scored below the SCS cut-off.
Table 4. Relationship of SCS status to peak daily cases and peak daily deaths: Independent samples median test
The relationships between SCS status and individual time course variables were analyzed using independent sample t-tests (Table 5). Significant differences were found for each comparison. In other words, more time had passed since the dates of (national) peak daily cases and deaths as well as the onset of national recommendations and national and local lockdowns for people who scored above the cut-off for the SCS than for those who scored below (1 to 2 weeks on average).
Table 5. Relationship of SCS status to individual time course variables: Independent sample t-tests

P < 0.002 for all tests.
a N = 5511 for 10 countries.
b N = 4765 for 8 countries.
c N = 1687 for 7 countries.
d N = 3540 for 5 countries.
Multivariable analyses
To account for potential demographic differences across countries, 5 multivariable regressions were performed, regressing SCS status on days since peak daily cases, daily deaths, national recommendations, and national and local lockdowns, with the demographic variables of age, female gender, and college education included as covariates. In 4 analyses, the COVID-19 time course variables remained significant contributors to SCS status (AOR: 1.002–1.010). In all analyses, younger age and female gender also increased the likelihood of exceeding the SCS cut-off. Lack of college education was a significant predictor of SCS only in the model with days since national lockdown (Table 6).
Table 6. Multivariate logistic regressions: Individual time course and demographic variables

Discussion
The purpose of the present study was to gain a deeper understanding of how COVID-19 has impacted individuals’ suicide risk, specifically by evaluating the relationship between rates of SCS and both the severity of and length of exposure to pandemic-related stressors. These included both the epidemiological impact of the disease itself as well as government policies reacting to the pandemic.
Importantly, results indicated that the severity of COVID-19 parameters and length of time that individuals are exposed to them were associated with higher rates of SCS. Specifically, individuals classified as having the SCS, as demonstrated by a cut-off score of 164 or higher on the SCI-2, were more likely to live in countries with proportionately higher peak daily cases and deaths during the first wave of the pandemic. Additionally, a longer duration between the onset of pandemic parameters and survey completion was associated with a higher incidence of SCS. These findings remained significant for all time course variables, except for days since national recommendations, when controlling for age, female gender, and college education status.
Although the adjusted odds ratios for the time course variables may seem small, it is important to note that they pertain to daily rates. The adjusted odds ratio for days since national lockdown, for example, showed that survey participants would be approximately 30% more likely to screen positive for SCS with an additional month (eg, from 13.7% to 17.8% in the United States). The adjusted odds ratios for days since peak death and days since local lockdowns demonstrate that survey respondents are approximately 9% more likely to be flagged for SCS within a month. These results underscore how much of a public health concern COVID-19 and associated parameters present to individuals’ suicide risk around the world.
Our findings are important for multiple reasons. They uphold results from existing literature noting the pandemic itself as being associated with negative implications on people’s mental health. 38,Reference Haider, Tiwana and Tahir39 Additionally, they demonstrate that measures and policies created in response to the disease also have mental health ramifications, especially in relation to suicide risk. Although it was difficult to anticipate the exact consequences when first implementing these parameters in the context of COVID-19, our results are not entirely surprising given existing research examining the relationship between previous epidemics and mental health. For example, Esterwood and Saeed Reference Esterwood and Saeed40 reported that during and after the SARS CoV-1, Middle Eastern respiratory syndrome (MERS), and Ebola epidemics, individuals experienced heightened anxiety and depressive symptoms. Overall, the present study reiterates the pressing need to consider people’s mental health while simultaneously preventing the spread of diseases.
These findings add to the extant literature in that they address how variation in the severity of exposure to pandemic-related stressors across individuals and countries can impact suicide risk. Likewise, these results may shed light on previous findings of a decrease in suicide deaths Reference Pirkis, John and Shin7,Reference Orui, Saeki and Kozakai8 or suicide-related emergency room visits Reference Irigoyen-Otiñano, Porras-Segovia and Vega-Sánchez9 in the early stage of the pandemic. Our findings point to an effect of time, such that chronicity of exposure to pandemic stressors appears to increase the severity of SCS symptoms. Consistent with prior research into the differential effects of chronic versus acute stress, Reference Giessing, Oudejans and Hutter31,Reference McGonagle and Kessler32 an initial decrease in suicide rates may have reflected a rallying response to the acute stress of the pandemic, potentially followed by increased psychological morbidity as acute stressors become chronic ones.
The present study also adds to existing literature by providing perspectives from 10 countries across 4 continents. Due to the nature of the data collection process, however, there was a small range of survey completion dates within each country. Thus, we are limited in our ability to separate the time-related effects from country-related effects. Nonetheless, the consistency of our findings across the large, international sample aligns with previous research that highlights cross-cultural effects of COVID-19 on mental health. Reference Ding, Yang and Chin41,Reference Gloster, Lamnisos and Lubenko42 Our results are also consistent with SCS research specifically, such that SCS occurs cross-nationally Reference Rogers, McMullen and Liang43 and is associated with personal stressors incurred during the first year of the pandemic. Reference Rogers, Richards and Cao10,Reference Rogers, Cao and Richards44 Finally, our results held up after controlling for sex, age, and college education, factors that varied widely across countries in our sample. In sum, our findings show that at both the country and individual levels of analysis, the severity of exposure to pandemic parameters is associated with increased suicidal risk.
Although the study did not provide head-to-head comparisons of effect sizes, the results suggest preliminary evidence that the time since national lockdowns had a particularly strong association with the SCS. Time from the onset of national lockdowns and dates of peak daily deaths to survey completion had the strongest effect sizes in bivariate analyses (Cohen’s d = 0.381 and 0.224). In multivariate analyses, the adjusted odds ratio for days since national lockdown had almost non-overlapping confidence intervals with other time course variables. Previous research corroborates the impacts of pandemic severity and lockdowns, such that COVID-19 severity was associated with heightened rates of anxiety and depression, Reference Le and Nguyen45 and lockdowns were associated with increased feelings of loneliness and distress. Reference Panchal, Salazar de Pablo and Franco46 Times of peak deaths and maximum lockdowns were also associated with greater periods of mental health problems. Reference Scarpetta, Columbo and Hewitt47 Overall, mandating lockdowns in response to high death rates should be done with caution, and there should be corresponding mitigation attempts to support people’s mental health. Reference Scarpetta, Columbo and Hewitt47
Finally, this study contributes additional evidence of the construct validity, cross-cultural relevance, and clinical utility of the SCS as a clinically relevant construct, showing its sensitivity to a wide range of global stressors. Furthermore, the SCI-2 easily translated into different languages and was applicable in 10 different countries on 4 different continents. Although we have previously demonstrated a strong relationship between the SCS and subjectively reported stressful life events, Reference Rogers, Richards and Cao10 to our knowledge, this is the first paper that shows a relationship between the SCS and objectively measured stressful life events.
Limitations and Future Directions
This study has numerous strengths, such as a large sample comprising participants from around the world; however, there were also limitations. A convenience sample was used with all self-report measures. These features can hinder the generalizability of findings and allow for the possibility of self-selection bias. Specifically, our sample was biased toward educated, young, and female participants as well as those motivated to partake in a survey about mental health and suicidal ideation during COVID-19. Future research should try to reach more representative samples across countries.
Additionally, there may be differences that were not accounted for between countries, and, as previously mentioned, there was limited variability in terms of survey completion dates, thereby interfering with the ability to conduct country-level analyses. Nonetheless, multivariate analyses controlling for relevant demographic differences corroborated the findings from bivariate analyses. Future research could assess a broader range of variables that may differ across countries. Further, the cut-off score of 164 on the SCI-2 for probable SCS has not been validated on a non-patient population. Lastly, graphical representations were used from WHO charts to obtain information regarding the time course of the first COVID-19 wave. Specific numbers and dates were linked to points along a graph within interactive graphics. Though the visual representations allow for easy identification of the first wave time frame, it is difficult to know conclusively the exact start dates within each country. Future research with alternative, non-graphical sources of temporal information would be useful.
Despite these limitations, this study provides insight into the relationship between COVID-19 severity and time course parameters and their impacts on mental health, specifically with respect to SCS and suicide risk in a large, international sample. This deeper understanding is helpful in guiding ongoing suicide rate reduction efforts in response to COVID-19 and other future large-scale catastrophes.
Our findings bring light to several compelling avenues of research worth exploring. One area of interest involves longitudinal responses to the COVID-19 pandemic and other global or wide-ranging disasters. Although, at this point, the pandemic is officially over, COVID-19 persists within the population. Investigation of how people’s psychological reactions have changed over time and the extent to which emotional distress persists after the acute danger subsides remain relevant. Additionally, it is critical to examine the efficacy of different mental health mitigation efforts, particularly in the context of lockdowns. While COVID-19 no longer threatens global catastrophe, there are likely to be future pandemics for which we will need to prepare.
Further, this study also provided evidence of the sensitivity of the SCS to a global disaster. Future research could examine the incidence and severity of the SCS in other disasters, including both natural and man-made disasters, such as war, with a long-term goal of developing low cost and easily administered intervention techniques to alleviate both acute emotional distress and suicide risk.
Conclusion
In conclusion, the present study documented the association between the incidence of individuals who screen positive for SCS, an acute, negative affect state robustly associated with suicidal risk, and the length of time and severity of exposure to both disease characteristics and resulting government responses, particularly national lockdowns. These findings underscore the mental health risks of global pandemics, emphasize the importance of temporal context, and highlight the need for coordinated mental health outreach and policy in such circumstances.
Acknowledgments
We acknowledge the American Foundation for Suicide Prevention (AFSP) for their ongoing support of this research, grant TBT-1-136-22.
Author contribution
Lisa Cohen and Yinan Liang are co-first authors.
Lisa Cohen: Study conception and design, data analysis, manuscript preparation; Yinan Liang: Study conception and design, literature review, data collection and analysis, manuscript review and editing; Devon Peterkin: Literature review, manuscript preparation and editing; Kamryn McGibbon: Literature review, manuscript preparation and revision; Frank Rappa: Literature review, manuscript preparation and revision; Megan Rogers: Data management/cleaning, manuscript review and editing; Igor Galynker: Study design and oversight, manuscript review, editing, design and implementation of the ISPARC program. Other authors were international collaborators responsible for instrument translation and study implementation in their respective countries.
Competing interests
No authors have any competing interests to report.









