INTRODUCTION
Q fever is a zoonosis occurring worldwide caused by Coxiella burnetii, an intracellular bacterium. Although most human infections remain asymptomatic or present as a non-specific flu-like illness, severe acute Q fever presents primarily with atypical pneumonia or hepatitis. The infection poses an increased risk for pregnant women and persons with heart-valve disorders or impaired immunity, who may develop chronic disease with endocarditis as its most frequent chronic clinical manifestation. Q fever in pregnancy, whether symptomatic or asymptomatic, may result in adverse pregnancy outcomes. Cattle, sheep and particularly goats are considered the primary reservoirs from which human infection occurs, typically by inhalation of infected aerosols, and less commonly through ingestion [Reference Raoult, Marrie and Mege1–Reference Carcopino3].
For many years, Q fever in humans was very rare in The Netherlands, with around 15 reported cases per year [Reference van Gageldonk-Lafeber4], but since the end of May 2007, outbreaks have occurred in rural areas mainly in the southern part of the country, with 20–25% of the reported cases requiring hospitalization [Reference Schimmer5]. In 2007, 178 Q-fever cases were reported, most of which occurred in May and June 2007. In total, 31% (n=55) of these cases occurred in a relatively small rural area [Reference Karagiannis6]. In 2008 and 2009, large outbreaks of Q fever recurred with increasing numbers of reported cases and an expanding geographic area [Reference Schimmer5, Reference Schimmer7].
Dairy-goat farms are considered the most likely source of infection for these outbreaks, although evidence is still inconclusive [Reference Schimmer5, Reference Schimmer7, Reference Van Steenbergen8]. Q-fever abortion waves have been reported at several dairy-goat farms, starting at least 2 years before the first recognized human outbreak [Reference Schimmer5, Reference Wouda and Dercksen9]. This time lag raised the question whether unrecognized human outbreaks may have preceded May 2007, particularly since most severe cases present as pneumonia, for which laboratory tests are often not requested. In fact, the diagnoses of the May/June 2007 outbreak cases were delayed by several weeks, until pneumonia patients were retested for C. burnetii, triggered by an increase in the number of Q fever reports in humans in the region [Reference Van Steenbergen8, Reference Morroy10].
Syndromic surveillance allows monitoring of clinical syndromes such as ‘pneumonia’ or ‘lower-respiratory infection’ (LRI) independent of laboratory confirmation. It also permits detection of outbreaks of diseases for which diagnostics are either not available or not requested. In order to optimize its sensitivity for detection of local outbreaks, surveillance of syndrome spikes can be performed in space and time [Reference Lazarus11, Reference Heffernan12]. Earlier we demonstrated the value of this approach by showing that syndromic surveillance of Dutch hospitalizations can indeed detect local lower-respiratory disease outbreaks [Reference van den Wijngaard13].
In the current study, we retrospectively explored whether there is evidence for human Q-fever outbreaks in The Netherlands in 2005–2007, before the May/June 2007 outbreak. Using space–time scan statistics, we looked for local increased numbers of hospitalized patients with LRIs and other syndromes that can be associated with C. burnetii infection. Based on available epidemiological and surveillance data, and the geographical proximity of small-ruminant farms that tested positive for Q fever, we then assessed whether these local increases could have been caused by Q fever or by other infections like respiratory syncytial virus (RSV) or influenza. Finally, we evaluated whether real-time syndromic surveillance of hospitalizations could have accelerated the detection of human Q-fever outbreaks.
METHODS
Hospitalization data
For the period 1 January 2005 to 30 September 2007, hospitalization data were obtained from the Dutch National Medical Register, which has about 80% population coverage. We excluded data before 2005, as data on farms that tested positive for Q fever was not then available. The data included discharge and secondary diagnoses by date of hospitalization. We selected all hospitalization records showing diagnoses involving clinical syndromes compatible with Q fever, i.e. LRI, hepatitis, and/or endocarditis. We used a case definition for LRI, which has proved functional for detecting severe respiratory disease outbreaks in hospitalization data [Reference van den Wijngaard13]. See Appendix A (available online) for detailed hepatitis and endocarditis case definitions.
We analysed 108 338 hospitalizations for LRI after excluding 5% of 114 245 records because of patients readmitted within six consecutive weeks; 3826 hospitalizations for hepatitis after excluding 29% of 5382 records because of readmissions from 1999 to 2007 (to avoid chronic cases first hospitalized before 2005); and 2130 hospitalizations for endocarditis after excluding 18% of 2612 records because of readmissions from 1999 to 2007 (to avoid chronic cases first hospitalized before 2005). Data were aggregated by week of hospitalization, postal code, and patients' age group (0–4, 5–19, 20–49, 50–64, ⩾65 years). Of these, we regarded the 20–49 and 50–64 years age groups to be at higher risk for Q fever, since most reported cases were adults, with the median age ~50 years [5, 7]. Since higher levels of spatial resolution can result in more sensitive detection of outbreaks [Reference Olson, Grannis and Mandl14, Reference Higgs15], we used 4-digit postal codes designating 4023 areas in a 16·3 million population. This provided the highest level of spatial resolution available within national privacy regulations.
Infectious disease surveillance data
To assess alternative causes (other than Q fever) for detected local clusters of syndromic hospital cases, we explored mandatory reports of psittacosis, Legionnaires' disease, hepatitis A, B and C, and Q fever, although prior to 2007 Q-fever cases may have remained undetected or misdiagnosed. The counts of reports were aggregated by week of disease onset and 4-digit postal codes. We used regional data on influenza-like illness (ILI) to assess whether a rise in local LRI cases could be due to influenza. These data are collected weekly by a sentinel network of general practitioners, the Continuous Morbidity Registration (CMR) centres, which provide 1% population coverage, representative by age, gender, geographic distribution and population density [Reference Donker16]. ILI is defined as an acute beginning of a respiratory infection with fever (rectal temperature ⩾38°C), and with at least one of the following symptoms present: cough, coryza, sore throat, frontal headache, retrosternal pain, myalgia. Due to the limited number of sentinel practices, these weekly data were aggregated into four major regions instead of 4-digit postal codes, as for the hospitalization data.
Data on positive goat and sheep farms
To identify possible point sources of C. burnetii, we used Q-fever-related abortion waves on dairy-goat and dairy-sheep farms as reported to the Dutch Animal Health Service. For each farm that tested positive for C. burnetii between 2005 and 2008, we recorded its 4-digit postal code and the date of its first submission of placental tissue.
Diagnostic tests for Q fever as a cause of abortion waves in animals were first available in 2004. In 2005 the first positive results were obtained from two dairy-goat farms, in 2006 from six dairy-goat farms and one dairy-sheep farm, in 2007 from seven dairy-goat farms, and in 2008 from eight dairy-goat farms and one dairy-sheep farm. Until 12 June 2008, reporting of abortion waves and subsequent laboratory testing of placental tissue were voluntary in The Netherlands; thus previous Q-fever abortion waves cannot be excluded in areas making no reports. For one farm, placental tissue from 2001 was retrospectively tested and found positive for C. burnetii.
We regarded these farms as possible point sources of C. burnetii during the entire study period, as some were known to have had abortion problems in the year before and/or after they first submitted placental tissue. Moreover, infected animals can become long-term shedders, and C. burnetii is very persistent in the environment [Reference Rousset17].
Scan statistics for space–time clusters
In order to detect a possible increase in Q-fever-related regional cases in the hospitalization data, we used a space–time permutation scan statistic that compared observed and expected numbers of cases in flexible circular areas over flexible time periods [Reference Kulldorff18]. SaTScan software and SAS (version 9.1, SAS Institute Inc., USA) were used to run the scan-statistic [Reference Kulldorff19, Reference Abrams and Kleinman20].
For each week in the analysis period, we ran the scan statistic on data from the preceding year, thus simulating prospective (real-time) surveillance. This generated weekly space–time signals. To indicate the significance of detected space–time signals, we used recurrence intervals, which indicate how often a signal of the observed significance would be observed by chance under the hypothesis of no outbreak [Reference Kleinman, Lazarus and Platt21]. That is, if the recurrence interval of a signal is say 1 year, one signal of the observed significance is expected in 1 year. If the recurrence interval of a signal was ⩾1 year, it was viewed as a significant signal. Besides that, we also used a threshold of recurrence intervals ⩾5 years to indicate highly significant signals. We defined a cluster as a group of successive overlapping space–time signals, since overlap suggests the same cause; we defined a cluster signal as an individual space–time signal within a cluster. Unlike an earlier study [Reference van den Wijngaard13], in the present study we also assessed whether the same cause for successive overlapping cluster signals seemed unlikely due to shifts in space or time windows or shifts in predominant age groups or discharge diagnoses. We used previously validated parameter settings for the scan statistic, with minimal constraints on the maximum space and/or time windows, to avoid incorrect assumptions about time, geographical location, or size of possible Q-fever outbreaks [Reference van den Wijngaard13].
We also performed space–time scans on specific infectious disease data (mandatory reports and ILI sentinel data), to assess whether these might explain the space–time clusters of hospitalizations that we detected. For the mandatory reports, the same parameter settings were used as for the hospitalizations. For the ILI data, the space–time scans were performed using both case data and population-at-risk data [Reference Kulldorff22], as previously described [Reference van den Wijngaard13].
LRI clusters
To determine the LRI clusters for which Q fever was an unlikely, possible or plausible cause, we used two-step criteria (Fig. 1). In step 1, the upper box shows the criteria for LRI clusters unlikely to be caused by Q fever, based on indications for other causative pathogens and epidemiological characteristics (e.g. patients' age) that differed from the confirmed Q-fever cases. The lower box shows the criteria for LRI clusters possibly caused by Q fever, based on epidemiological data [Reference Schimmer5, Reference Schimmer7, Reference Gilsdorf23] as well as overlap with clusters of human Q-fever reports. In step 2, we assessed whether clusters identified as possibly caused by Q fever (in step 1) showed geographical overlap with farms that tested positive in 2005–2008. If so, we considered Q fever a plausible cause for these clusters.
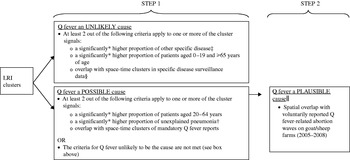
Fig. 1. Two-step criteria to explore the plausibility that Q fever caused the lower-respiratory infection (LRI) hospitalization clusters detected in 2005–2007. * Right-sided Fisher's exact test for 2×2 tables (α⩽0·05 and/or <0·01) of hospitalizations inside vs. outside of the cluster signal. The proportion of hospitalizations with a specific disease characteristic (e.g. Legionnaires' disease as discharge diagnoses, or patients aged 20–64 years) can be significantly higher in hospitalizations within the cluster signal than the proportion outside the cluster signal. † ICD-9 codes 485/486/481/4829. ‡ We considered high proportions of bronchitis/bronchiolitis (ICD-9 codes 4801/4660/4661/490) as a likely indication for RSV activity. § Mandatory reports and influenza-like illness sentinel data. || Only assessed if the cluster meets the criteria for Q fever to be a possible cause.
Hepatitis and endocarditis clusters
To assess whether detected hepatitis and/or endocarditis clusters might have been caused by Q fever, we again used two-step criteria, similar as for the LRI clusters. In step 1, we now evaluated whether hepatitis clusters overlapped with clusters of hepatitis A, B, or C reports and assessed whether hepatitis and/or endocarditis clusters had any characteristics (age distribution, specific diagnoses) suggesting causes other than Q fever. In step 2, clusters for which no alternative causes were found, were assessed for overlap with reported Q-fever abortion waves at farms in 2005–2008. If they overlapped, we considered Q fever a plausible cause for these human disease clusters.
The patients of all clusters for which we considered Q fever a plausible cause were then line-listed and inspected for data anomalies that might have caused a cluster signal. Finally, we evaluated to what extent actual prospective syndromic surveillance could have accelerated the detection of human Q-fever outbreaks.
RESULTS
LRI clusters
We detected 20 LRI clusters in hospitalization data between 2005 and 2007 [for details see Appendix B, Table B1 (available online)]. Applying the criteria in Figure 1, for seven of these LRI clusters, Q fever was considered a plausible cause; for three clusters a possible cause, and for ten clusters an unlikely cause. Figure 2 shows all LRI clusters and signals on a timescale, and Figure 3 a shows the locations of the LRI clusters for which we considered Q fever a plausible cause.

Fig. 2. All lower-respiratory infection (LRI) signals and clusters on a timescale. The legend indicates which clusters have Q fever as a plausible, possible, or unlikely cause (see criteria in Fig. 1). * For each cluster, horizontal dotted lines indicate the total cluster episode, and triangles indicate weekly generated cluster signals. As some clusters overlapped in time, consecutive clusters are presented at different heights at the y-axis. The significance level of cluster signals, as measured by the recurrence interval (see Methods section), is indicated by the colour value of the triangles. For those with uncoloured backgrounds, the recurrence interval of the signal is ⩾1 year; with coloured backgrounds, the recurrence interval is ⩾5 years). † At the end of May 2007 the first uncommon pneumonia patients were reported in the area of the initial 2007 outbreak, and on 11 July C. burnetii was confirmed to be the causative pathogen. This initial 2007 outbreak was reflected by cluster 16.

Fig. 3. (a) Lower-respiratory infection (LRI) clusters for which Q fever seemed a plausible cause, presented on the 4-digit postal code map of The Netherlands. See criteria for Q fever as a plausible cause in Figure 1. If LRI cluster areas overlapped, the smaller cluster area was drawn on top of the larger area. (b) The hepatitis cluster for which Q fever seemed a plausible cause, presented on the 4-digit postal code map of The Netherlands.
Q fever: a plausible cause
Of the seven clusters for which Q fever was considered a plausible cause, one reflected the known May/June 2007 outbreak, as it strongly overlapped in space and time with that outbreak. If monitored in real time, this cluster would have given the first signal at the end of May 2007, i.e. in the same week that suspicious pneumonia patients were first reported, and 6 weeks before the first positive laboratory results for C. burnetii were obtained [Reference Van Steenbergen8, Reference Morroy10].
Of the other six clusters, three would have given the first signal 1–2 years earlier than the known outbreak in 2007 (two in 2005 and one in 2006), one cluster 3 months earlier, one at the same time, and one cluster 4 months afterwards [Fig. 2 and Appendix B, Table B1 (online)]. All but one of these clusters occurred in the southeast or the middle of the country (Fig. 3 a) but in a more widespread area than the May/June 2007 outbreak. The two 2005 clusters and two clusters in 2007 were highly significant with recurrence intervals ⩾5 years.
Q fever: a possible cause
For only three clusters was Q fever a possible cause, i.e. not plausible because they lacked geographical proximity to Q-fever abortion waves on farms. All three clusters occurred in 2007 [see Fig. 2 and Appendix B (online)].
Q fever: an unlikely cause
The ten clusters for which Q fever was considered an unlikely cause were not assessed for geographical overlap with infected farms, because other pathogens (e.g. influenza and RSV) seemed probable. As previously described, one cluster was clearly due to Legionella, as it comprised many cases of Legionnaires' disease and overlapped in space and time with a known Legionella outbreak [Reference van den Wijngaard13, Reference Van den Hoek, IJzerman and Coutinho24].
Hepatitis and endocarditis clusters
Two hepatitis clusters (two signals) were detected in 2005–2007. The first was possibly due to hepatitis C [Appendix B, Table B2 (online)]. The other overlapped with reported abortion waves on goat farms, making Q fever its plausible cause. The cluster occurred more to the southeast (Fig. 3b) than the May/June 2007 outbreak. It would have given the first signal 2 weeks before the first reports of suspicious pneumonia patients in 2007. The cluster does not exceed the threshold level for highly significant clusters (i.e. recurrence interval ⩾5 years).
For endocarditis, we revealed probable duplicates in all three detected clusters based on line-listing the age, postal code, and diagnoses of cluster patients. Although duplicates had been excluded from the analyses by using anonymous patient identifiers, some patients appeared to have obtained two or more anonymous identifiers through transfers between hospitals. We therefore excluded the endocarditis clusters from further analysis.
DISCUSSION
Using space–time syndromic surveillance methods, we found substantial support for the occurrence of human Q-fever outbreaks in The Netherlands preceding the 2007 outbreak and covering a wider area. In proximity to infected small-ruminant farms, local clusters of human LRI and hepatitis were detected in hospitalization data for 2005–2007. Although the retrospective nature of this study precluded laboratory confirmation, available epidemiological and surveillance data suggested Q fever as the cause for several syndrome clusters that mostly occurred in the southeast and middle of the country.
Prospective syndromic surveillance on hospitalizations, as simulated in this study, would have signalled some of these clusters long before detection of the May/June 2007 outbreak. The space–time signals of LRI or hepatitis could then have prompted further evaluation and/or laboratory tests, possibly confirming C. burnetii to be the causative pathogen. Although such efforts might not have prevented the large-scale outbreaks in the following years, it possibly would have lead to the detection and the appropriate treatment of Q-fever patients in a more timely manner. Apart from that, earlier detection of human Q-fever outbreaks might have facilitated research into transmission routes between specific farms and humans. For the Dutch human Q-fever outbreaks after 2007, this research has been complicated by dissemination of disease in the dairy-goat population, leading to widespread environmental contamination. These factors complicate the identification of specific farms as the source of human infections.
Of the LRI clusters detected in this study, one reflected the already known 2007 outbreak, confirming that syndromic surveillance can indeed detect Q-fever clusters, consistent with our findings on syndromic detection of respiratory outbreaks [Reference van den Wijngaard13]. For six other LRI clusters and one hepatitis cluster as well, Q fever seemed a plausible cause. So far, hepatitis due to Q fever has been reported sporadically in The Netherlands: 33 hepatitis cases out of 1000 reported Q-fever cases in 2008 [Reference Schimmer5] and 5/178 in 2007. Hepatitis due to Q fever might be more likely from infection by ingestion rather than inhalation [Reference La Scola, Lepidi and Raoult25, Reference Marrie26] and may thus follow distribution channels of contaminated unpasteurized products like raw cheese. If such contaminated products were to cause infections nationwide (without regional clustering), this would not be detected by our space–time analysis.
Our results suggest that the rise in reported Q-fever cases in 2008 and 2009 may partially reflect increased awareness among clinicians following the first recognized outbreak in 2007. This would be consistent with the fact that in 2008 and 2009, Q-fever reports originated from a wider area that overlaps with the area of most hospitalization clusters of 2005–2007 for which Q fever seemed a plausible cause. Moreover, the proportion of hospitalizations in confirmed Q-fever cases was smaller in 2008 and 2009 than in 2007, possibly indicating that increased awareness among clinicians led to diagnosis of earlier and milder Q-fever infections [Reference Schimmer5]. However, in 2007 we observed four clusters for which Q fever seemed a plausible cause vs. a total of three clusters in 2005 and 2006 combined, which suggests an actual rise in Q-fever infections in 2007.
Our finding that syndromic hospital data can reveal disease clusters possibly caused by Q fever, supports the value of prospective syndromic surveillance for detection of otherwise hidden outbreaks. We showed previously that syndromic surveillance for LRI would detect a modest number of clusters in time to investigate: on average five clusters per year at the lowest threshold level (recurrence intervals ⩾1 year), and three clusters at the highest (recurrence intervals ⩾5 years) [Reference van den Wijngaard13]. If such prospective surveillance were to focus on detection of Q-fever outbreaks, inclusion of data on infected small-ruminant farms, as in the current study, would further decrease the number of clusters to investigate. Nevertheless, even then such surveillance also requires sufficient complementary epidemiological and microbiological data to guide further investigation of detected clusters. For example, LRI clusters are best interpreted in relation to local influenza or RSV surveillance data. A prerequisite for prospective syndrome surveillance is the real-time availability of hospitalization data, including clinical diagnoses and symptoms by date of hospitalization. Although at present not available in The Netherlands, such real-time syndromic data collection might become feasible due to the nationwide implementation of electronic healthcare-information exchange. Finally, proper data collection and analysis will be more challenging in a prospective setting, for example due to data quality problems such as reporting delays.
This study has some further limitations. Due to its retrospective setting, C. burnetii infection could not be laboratory-confirmed for detected cluster patients. Therefore, we could only indicate whether Q fever seemed a plausible cause by excluding clusters with other apparent causes and assessing the presence of C. burnetii in cluster areas, as measured by overlap with infected farms. Another limitation lies in our use of voluntary reports from farmers to indicate possible C. burnetii point sources. Cluster areas not overlapping with reportedly infected farms may still have been contaminated by farms not tested or, possibly, by the spreading of manure from non-local contaminated farms. If so, this may explain those clusters that seemed possibly due to Q fever but did not overlap with reported Q fever on farms.
Serological testing of preserved human samples might confirm the occurrence of Q-fever clusters before 2007. However, to our knowledge no historical samples from specific LRI patients within the cluster areas are available. Other studies have found that substantial proportions of a human population can be exposed to Q fever without symptomatic infections [Reference Marrie and Pollak27, Reference McCaughey28]. Therefore, a solution might be to use historical samples from blood donors, if sufficient samples from the cluster areas are still available.
This study shows substantial support for the occurrence of human Q-fever outbreaks in The Netherlands before detection of the May/June 2007 outbreak and covering a wider area. Retrospectively, suspicious LRI and hepatitis hospitalization clusters from 2005 to 2007 were detected and found to overlap with small-ruminant farms reporting Q-fever abortion waves. Further research on historical serological samples from the detected cluster areas, if available, should be performed to confirm occurrence of human Q-fever outbreaks before the May/June 2007 outbreak. In a real-time setting, detection of these clusters should have prompted further investigation and additional laboratory tests, which might have resulted in detection of human Q-fever outbreaks up to 2 years earlier. In this light, it seems worthwhile to make syndromic hospitalization data available real-time for prospective outbreak detection. Finally, our study also illustrates the added value of integrated human and animal surveillance for improved detection of zoonotic disease outbreaks.
NOTE
Supplementary material accompanies this paper on the Journal's website (http://journals.cambridge.org/hyg).
ACKNOWLEDGEMENTS
We thank Dutch Hospital Data for providing data from the Dutch National Medical Register (LMR); Daan Notermans and Marianne van der Sande for reviewing and commenting on the manuscript; and Lucy Phillips for editorial review.
DECLARATION OF INTEREST
None.





