Introduction
The Eustachian tube is normally a closed structure, which opens temporarily during swallowing and yawning, typically for less than one-half second.Reference Mondain, Vidal, Bouhanna and Uziel1 The Eustachian tube plays a crucial role in: equalising middle-ear pressure, middle-ear drainage, and protecting against both vocal and breathing autophony.Reference Bluestone2
Patulous Eustachian tube is an abnormal patency of the Eustachian tube that affects 0.3–6.6 percent of people.Reference DiBartolomeo and Henry3 Typically, patulous Eustachian tube presents with autophony, aural fullness, tinnitus and ear blockage.Reference Bluestone2 Although additional tests (e.g. computed tomography or tympanometry) have been used to improve the diagnosis of patulous Eustachian tube, it remains a clinical diagnosis based on mentioned symptoms and visualisation of tympanic membrane movement with respiration.Reference Luu, Remillard, Fandino, Saxby and Westerberg4
There is currently no general consensus regarding patulous Eustachian tube management. A variety of non-surgical treatments (e.g. therapy with topical nasal saline instillation or behaviour changes) have been described, with only temporary effects. Surgical procedures have generally shown variable results.Reference Luu, Remillard, Fandino, Saxby and Westerberg4
Most recently, the injection of autologous fat, cartilage or hydroxylapatite has been described for cases of Eustachian tube occlusion, with promising results.Reference Vaezeafshar, Turner, Li and Hwang5–Reference Wolraich and Zur10 This experimental procedure is relatively minimally invasive compared to other surgical methods. However, results vary among case studies and there is not always complete resolution of symptoms.Reference Vaezeafshar, Turner, Li and Hwang5, Reference Schröder, Lehmann, Sudhoff and Ebmeyer6 It is currently not possible to identify patients in whom complete resolution of symptoms will be achieved.
The variable reported success of injecting such materials could be explained by the injection of a unified substance volume in all patients, regardless of the anatomical conditions. Additionally, the patulous Eustachian tube could have been caused by pathology in a different (more lateral) part of the Eustachian tube in some patients. We present a case wherein saline was injected under local anaesthesia to determine the volume needed and to predict the success of patulous Eustachian tube augmentation with long-standing material.
Case report
A 38-year-old woman was referred to the Department of Otorhinolaryngology and Head and Neck Surgery in a tertiary referral hospital. She presented with a five-year history of vocal and breathing autophony, aural fullness, and ear blockage on the right side. Symptoms were extremely annoying for the patient and disappeared only during severe rhinosinusitis. Therefore, the patient looked forward to any nasal infection.
There was no significant weight loss, trauma or ear infection before symptoms appeared. The patient did not use hormonal contraception and had not been pregnant in the preceding 10 years. There was no tinnitus, hearing loss, pain or history of vertigo. The patient did not suffer from any other disease and had not undergone surgery.
Upon clinical examination using a microscope and high definition endoscopes (Figures 1 and 2), we observed movement of the healthy tympanic membrane with respiration and a widened nasopharyngeal orifice of the right Eustachian tube. No other pathology was found. Tympanometry showed a type A tympanogram. The audiogram showed no hearing loss. The diagnosis of patulous Eustachian tube was made.

Fig. 1. Endoscopic view of the right tympanic membrane during inhalation (a) and exhalation (b).
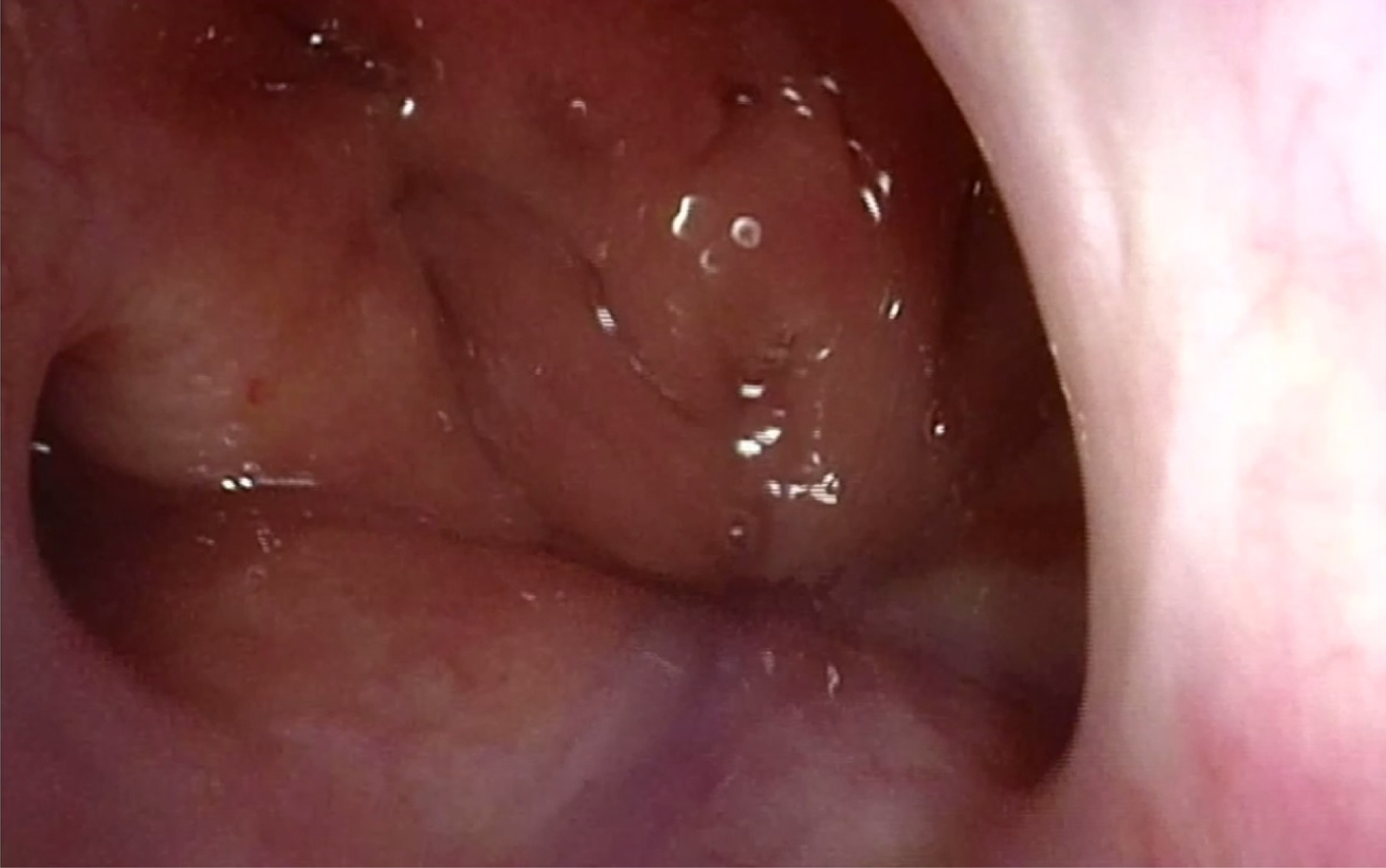
Fig. 2. Endoscopic view of the widened nasopharyngeal orifice of the right Eustachian tube.
Therapy with topical nasal saline instillation was recommended and had no effect. Therefore, augmentation of the nasopharyngeal orifice of the right Eustachian tube was indicated.
First procedure: saline
Augmentation of the right Eustachian tube was performed as a two-step procedure. Initially, the nasopharyngeal orifice of the right Eustachian tube was visualised through the right nasal cavity using a 30-degree, 4-mm nasal high definition endoscope under local nasal anaesthesia (achieved using cotton swabs with tetracaine 1 percent for 10 minutes and lidocaine 10 percent spray). Then, a 25 cm long transoral Radiesse malleable needle (model 9010M1; Merz Aesthetics, Franksville, Wisconsin, USA), with a 16-gauge malleable shaft, was inserted through the right nasal cavity. The needle was placed into the submucosal space, parallel to the lumen of the Eustachian tube, and directed towards the isthmus. Saline (0.3 + 0.3 ml) was injected into two separate locations: the anterior and posterior aspect of the nasopharyngeal orifice of the right Eustachian tube (Figure 3).
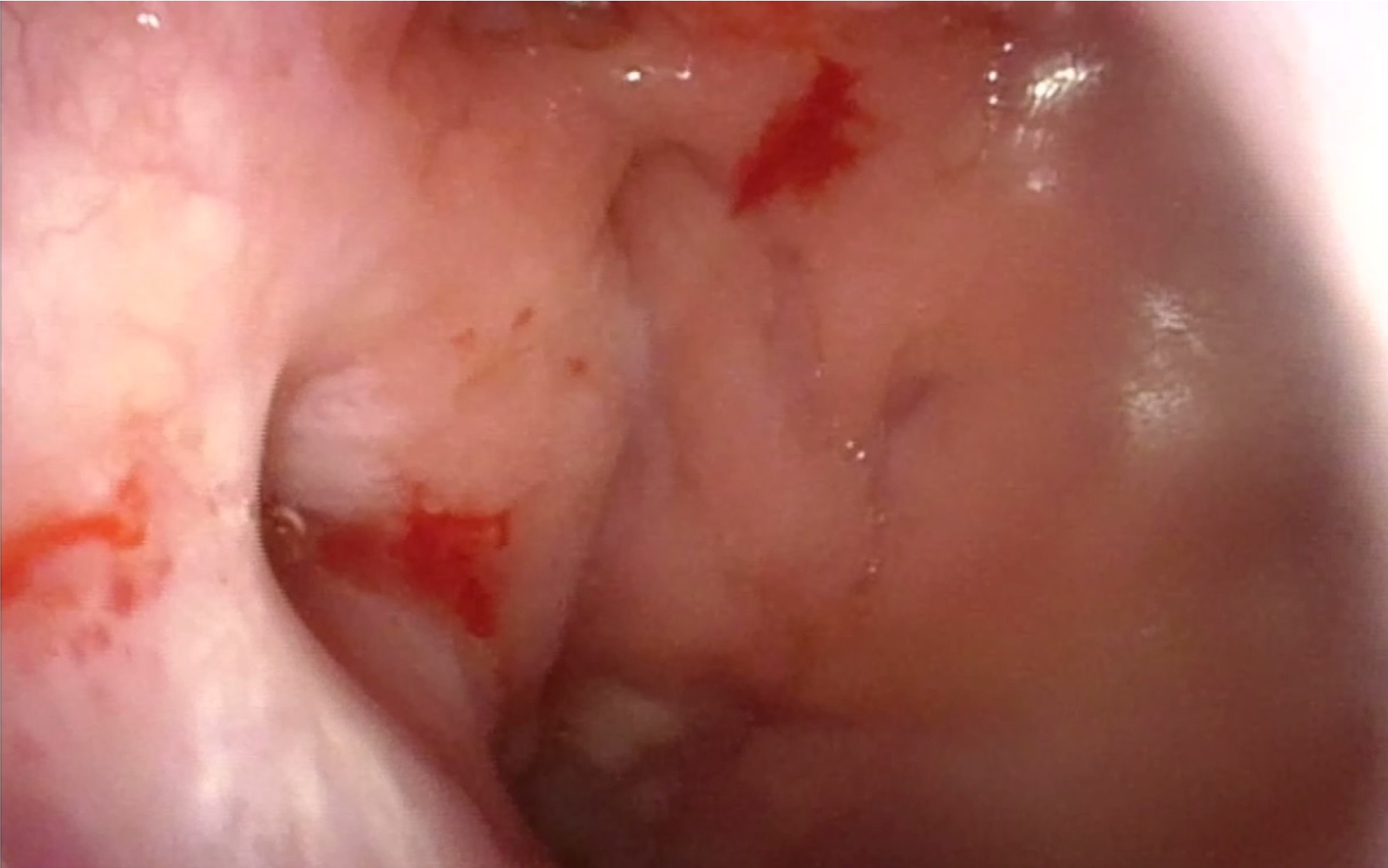
Fig. 3. Endoscopic view of the nasopharyngeal orifice of the right Eustachian tube after saline injection.
The patient achieved complete symptomatic relief and the movement of the right tympanic membrane with respiration disappeared. However, after 10 minutes, there was partial restitution of symptoms. The tympanic membrane did not move with respiration. The effect lasted until about 1 day later and then symptoms slowly started to aggravate to the pre-procedural level. The procedure was very well tolerated.
Second procedure: calcium hydroxylapatite
Augmentation with calcium hydroxylapatite, using Radiesse Voice injectable implant (Merz Pharmaceuticals, Frankfurt am Main, Germany), was performed 14 days later using the same technique. Because there was almost immediate partial restitution of symptoms, this time 0.4 + 0.4 ml of calcium hydroxylapatite was injected into the two locations (Figure 4).
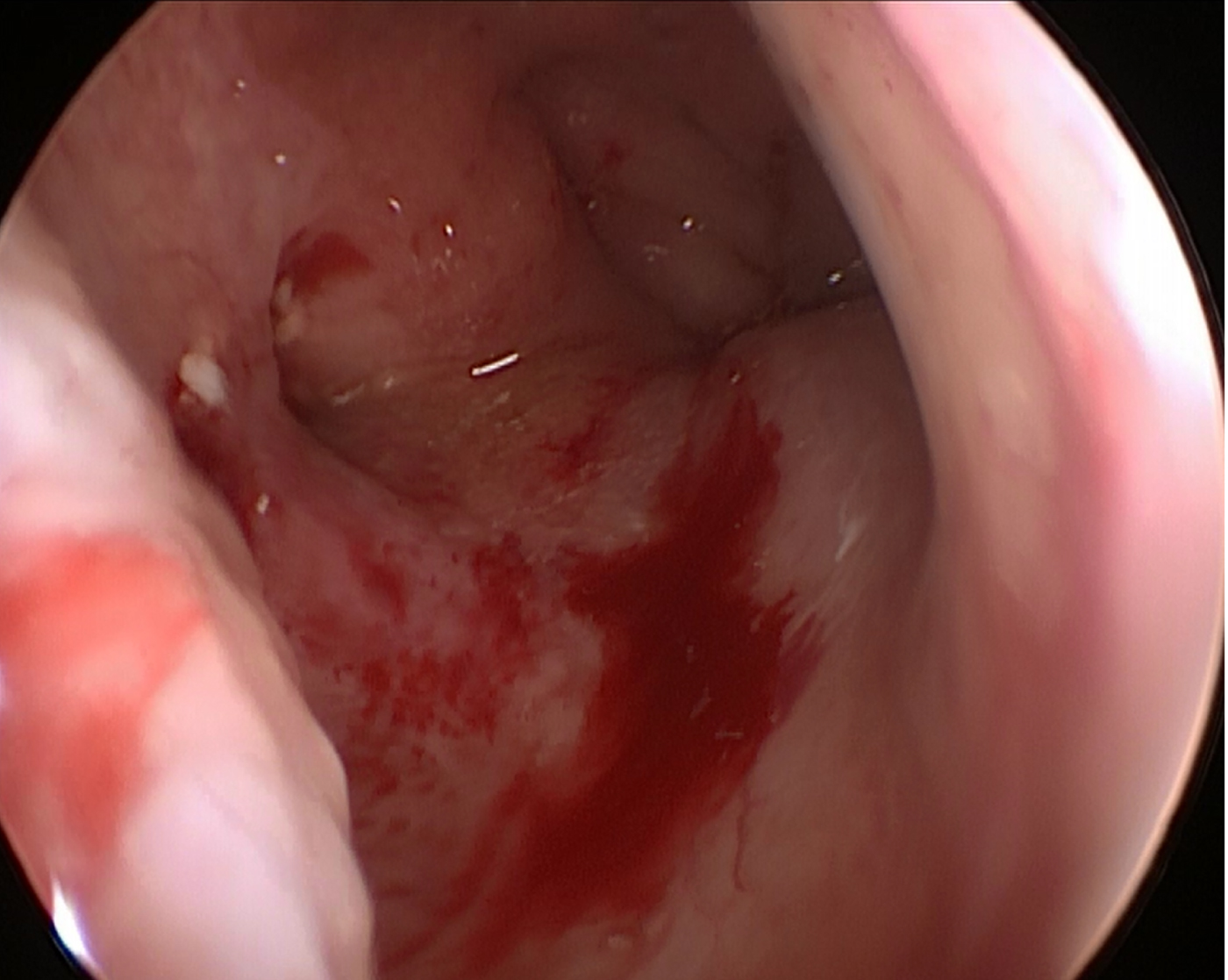
Fig. 4. Endoscopic view of the nasopharyngeal orifice of the right Eustachian tube after augmentation with calcium hydroxylapatite.
The patient again achieved complete symptomatic relief, which this time lasted. Movement of the right tympanic membrane with respiration disappeared as well. The procedure was well tolerated, but not as well as with saline. The patient remained free of symptoms six months post-operatively.
Discussion
Several issues have to be overcome before patulous Eustachian tube augmentation can be successfully utilised in routine clinical practice. Presently, it remains an experimental method. The biggest issue is the varying success of treatment among patients. This could be connected to the amount of material injected into the Eustachian tube surroundings, as this is the biggest difference among existing studies.
• Augmentation of patulous Eustachian tube for its occlusion has promising results
• Identifying the appropriate volume of injected material can be challenging
• Anatomical conditions vary among patients and there is a risk of developing chronic obstruction
• Saline injection under local anaesthesia for determining the volume of long-standing material could allow more personalised treatment
• Furthermore, it could help identify patients likely to benefit from the procedure
In the case series of Schröder et al., 1 ml of Vox® soft-tissue bulking agent was applied in the torus tubarius of 20 patients under general anaesthesia.Reference Schröder, Lehmann, Sudhoff and Ebmeyer6 Only 35 percent of patients reported significant improvement, and the intervention had to be repeated up to three times with 1 ml, until at least 50 percent of patients were satisfied. In the case series of Vaezeafshar et al., hydroxyapatite was injected at three separate locations around the torus tubarius in 14 patients under general anaesthesia, and no additional material could be placed without reflux of the injected material.Reference Vaezeafshar, Turner, Li and Hwang5 The rates of complete or significant symptom improvement ranged from 50 percent to 63 percent, with satisfaction rates of 36–50 percent. Oh et al. reported on 0.5 + 0.5 ml autologous cartilage augmentation in 25 patients under local anaesthesia, with 70 percent of patients experiencing complete relief or significant improvement and satisfaction regarding autophony.Reference Oh, Lee, Goh and Kong8
Identifying the appropriate volume of injected material could be challenging because anatomical conditions vary among patients. Rationally, the more material injected, the higher the chance of a better outcome. However, there is always the risk of developing chronic Eustachian tube obstruction and its related complications if too much permanent material is injected.
We hypothesise that the required volume of injected permanent material could be better determined by saline injection, as demonstrated in our case report. This is safe and very easy to perform. It is also very well tolerated under local anaesthesia. Therefore, the procedure could be repeated until the right volume is established.
Saline is usually absorbed within a few hours; thus, there is no risk of developing chronic Eustachian tube obstruction. Signs of Eustachian tube obstruction following saline injection can indicate that the intended volume is too high. In our case, the originally intended volume of 0.6 ml would not have been sufficient to reach complete relief if long-standing material was directly applied. However, if a rigid unified scheme had been used, a higher volume would have unnecessarily been applied. Although 0.8 ml is among the lowest of the volumes reported in existing studies,Reference Vaezeafshar, Turner, Li and Hwang5–Reference Wolraich and Zur10 it was sufficient in our patient.
Thus, with saline injection and a two-step procedure, complete relief was achieved, with a lower risk of developing complications. The technique allowed us to offer more personalised treatment with less material injected, reducing the unpleasantness for the patient. Saline injection is well tolerated and there is more chance of being able to perform it under local anaesthesia. It could therefore prevent repeated general anaesthesia procedures from being performed to determine the ideal augmented volume for significant or complete improvement, as in the studies of Schröder et al.Reference Schröder, Lehmann, Sudhoff and Ebmeyer6 and Vaezeafshar et al.Reference Vaezeafshar, Turner, Li and Hwang5
Saline injection is also potentially a useful diagnostic office procedure for patients in whom only some symptoms suggestive of patulous Eustachian tube are present (with no tympanic membrane movement on respiration), where there is no alternative diagnosis.
Our observation has to be confirmed in a larger cohort before it can be routinely applied.
Conclusion
Saline injection prior to patulous Eustachian tube augmentation with long-standing material could help determine the injection volume of permanent material, thereby increasing the success of augmentation. It could also lead to more personalised treatment and help identify patients likely to benefit from the procedure.
Acknowledgement
Supported by the Ministry of Health, Czech Republic, with a conceptual development of research organisation grant (number: FNOs/2016).
Competing interests
None declared






