To the Editor—Sinks in healthcare facilities are a potential reservoir for dissemination of multidrug-resistant gram-negative bacilli and Candida spp.Reference Kizny Gordon, Mathers and Cheong 1 , Reference Jencson, Cadnum, Piedrahita and Donskey 2 Unfortunately, sink drainage systems provide a favorable environment for pathogen colonization and biofilm formation, but they are not amenable to cleaning and disinfection.Reference Livingston, Cadnum, Gestrich, Jencson and Donskey 3 Pouring disinfectants into sink drains has been reported to be beneficial, but reductions in sink colonization have often been limited or transient.Reference Parkes and Hota 4 We hypothesized that disinfectants poured into drains might have limited efficacy in part because they flow rapidly down the drain, providing inadequate contact time and poor penetration into many of the areas harboring microorganisms. Thus, we conducted a pilot study to test the hypothesis that approaches that allow instillation of disinfectant throughout the proximal drainage system for a prolonged period would improve the efficacy of liquid disinfectants.
In initial experiments, we installed a stop valve immediately distal to the P trap in a research laboratory sink known to be colonized with Pseudomonas aeruginosa. Closure of the valve resulted in stoppage of flow; opening the valve allowed liquids to flow normally. We tested the impact of 3 interventions: (1) pouring 500 mL of 5% acetic acid down the drain over 1 minute; (2) pouring 500 mL of a 1 to 10 dilution of household bleach down the drain over 1 minute; and (3) pouring 500 mL of a 1 to 10 dilution of household bleach down the drain over 1 minute with the stop valve closed allowing complete filling of the drainage system from the valve to just above the strainer for 1 hour followed by opening of the valve and flushing with water for 30 seconds. To assess the impact of the interventions, quantitative cultures for gram-negative bacilli were collected from the proximal sink drain to depth of 2.5 cm below the strainer before treatment and intermittently for 15 days post treatment. The experiment was repeated twice for each intervention.
A second set of experiments was conducted in 4 patient rooms with sink colonization by gram-negative bacilli. Among the 4 sinks, 2 were treated by pouring 500 mL of disinfectant down the drain and the other 2 were treated by instillation of the disinfectant for 1 hour. The experimental methods were as described previously with the following exceptions: (1) the valve was placed proximal to the P trap approximately 15 cm below the strainer; (2) the disinfectant used was a commercial improved hydrogen peroxide product; and (3) the sinks were operated by patients and staff as needed. The experiment was repeated twice; sinks treated with one method during the first run were treated with the opposite method during the second run. For both sets of experiments, an ordinary least-squares regression model was used to compare treatment groups.
As shown in Fig. 1(A), pouring bleach or acetic acid into the laboratory sink resulted in only transient suppression of proximal drain colonization, whereas instillation of bleach for 1 hour resulted in suppression at this site for several days (P <.001). The organisms recovered throughout the experiment were identified as P. aeruginosa.
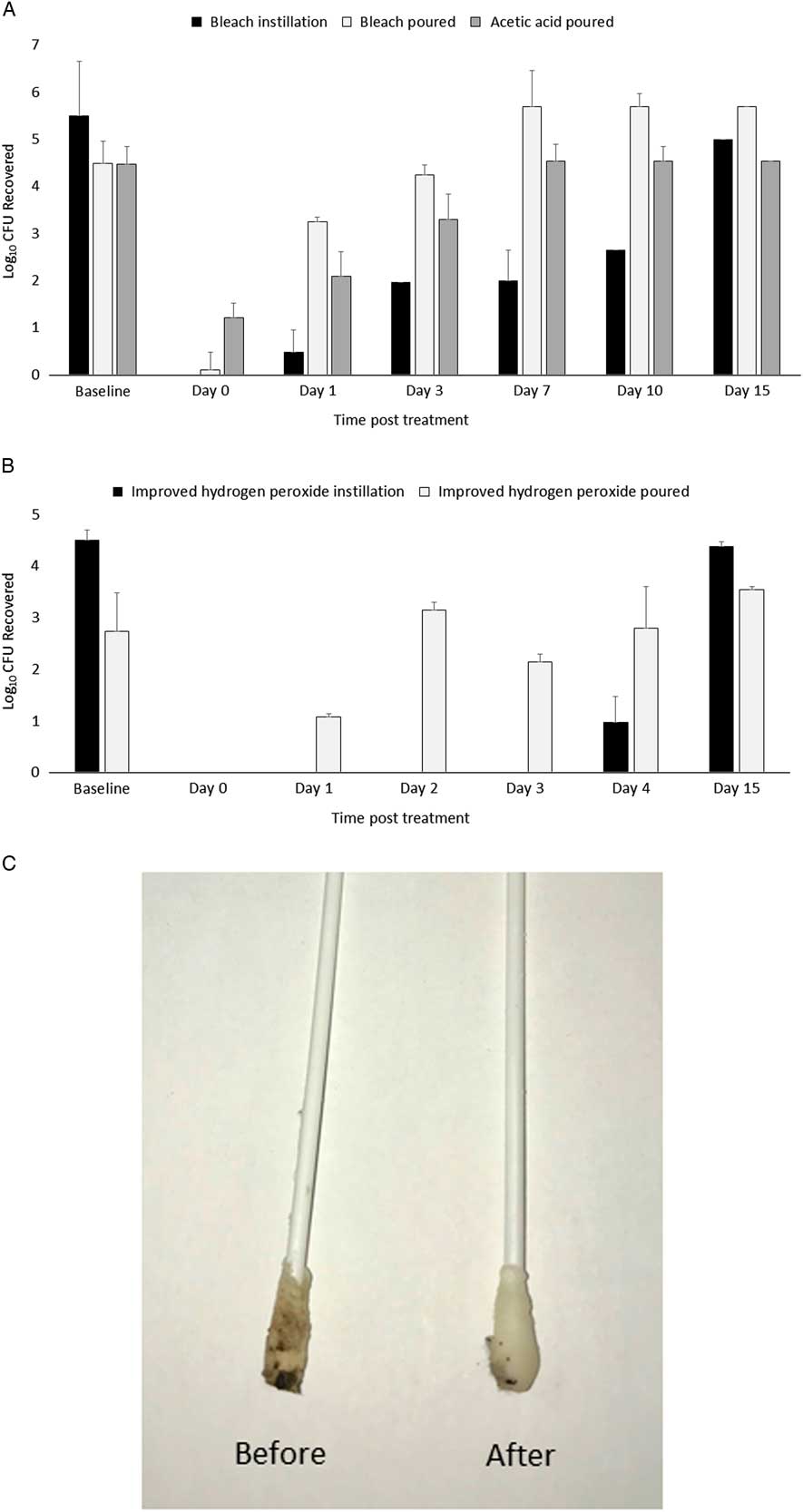
Fig. 1 Efficacy of pouring versus instilling 500 mL of disinfectants on recovery of gram-negative bacilli from proximal sink drains in a research laboratory sink (A) and in sinks in rooms of hospitalized patients (N = 4) (B). For instillation, a stop valve was used to allow complete filling of the drainage system from the valve to just above the strainer for 1 hour. Quantitative cultures for gram-negative bacilli were collected from the proximal sink drain to depth of 2.5 cm below the strainer before treatment and intermittently for 15 days post treatment. For the laboratory sink, the stop valve was just distal to the P trap, whereas for the patient room sinks it was just proximal to the P trap. Swabs collected before versus after instillation of disinfectant for 1 hour are shown in panel (C).
As shown in Fig. 1(B), pouring the improved hydrogen peroxide disinfectant into the patient room sinks resulted in only transient suppression of proximal drain colonization, whereas instillation proximal to the P trap for 1 hour reduced gram-negative bacilli concentrations in the section below the strainer for several days (P <.001). After 1 hour of disinfectant instillation, numerous visible pieces of organic and inorganic material were released from the sides of the drain pipes, and swabs used to sample the sink drain were visibly cleaner than baseline swabs (Fig. 1(C)).
Our results demonstrate that pouring disinfectants down drains has only a transient impact on the microbial load just below the strainer. In contrast, use of a valve to allow instillation of disinfectant throughout the proximal drainage system with a 1-hour dwell time resulted in reduced proximal sink drain colonization for several days. This effect was probably observed due to increased disinfectant contact time and enhanced penetration into some of the areas harboring microorganisms. These findings are clinically relevant because the proximal sink drain is the primary site of dispersal from colonized sinks.Reference Kotay, Chai, Guilford, Barry and Mathers 5 Moreover, the fact that colonization of the drain was reduced for several days suggests that intermittent rather than daily application of the disinfection process might be effective in reducing the risk for dispersal.
Our study has some limitations. The study was a small proof-of-concept study that will require validation in larger studies. However, some previous studies have suggested that similar approaches can be effective in reducing sink contamination.Reference Klick, du Moulin, Hedley-Whyte, Teres, Bushnell and Feingold 6 , Reference Gbaguidi-Haore, Varin, Cholley, Thouverez, Hocquet and Bertrand 7 For example, Klick et alReference Klick, du Moulin, Hedley-Whyte, Teres, Bushnell and Feingold 6 reported that daily filling of sinks fitted with drain cutoff valves with 5% phenol solution in conjunction with heating was effective in reducing colonization with Pseudomonas spp. We did not demonstrate that the reduction in proximal sink drain colonization resulted in reduced dispersal of organisms during operation of the sinks. Finally, installing valves in sink drainage systems may not be feasible for some sink designs and could be costly and labor intensive. Thus, we are currently investigating several simpler approaches to achieve the same effect.
Acknowledgments
We would like to thank the staff of the Cleveland VA Medical Center’s Engineering Service for assistance in designing and installing sink valves.
Financial support
This work was supported by the Department of Veterans Affairs.
Conflicts of interest
C.J.D. has received research funding from Clorox, GOJO, Pfizer, Avery Dennison, PDI, and Boehringer Laboratories. All other authors report no potential conflicts.



