Mental disorders, including depression, anxiety and psychological distress, are highly prevalent, affecting approximately 450 million people of all ages worldwide(Reference Paskulin, Drehmer and Olinto1). In Iran, mental disorders have dramatically increased from 27·7 to 34·2 % between 1998 and 2007 in adults, showing the high priority of these problems to research and action(Reference Noorbala, Bagheri Yazdi and Hafezi2). In China, anxiety is also a serious social and public health problem and has become a substantial burden(Reference Prina, Ferri and Guerra3). It is well known that anxiety is recognised as a multifactorial chronic disease that may be related to hereditary, environmental and dietary factors(Reference Kang, Bae and Kim4,Reference Salehi-Abargouei, Esmaillzadeh and Azadbakht5) .
As an important aspect of lifestyle, diet has been suggested as a contributing factor to anxiety. In recent decades, numerous studies on the association between diet and psychological disorders have mostly targeted individual foods or nutrients and food groups(Reference Jacka, Overland and Stewart6–Reference Kiecolt-Glaser, Belury and Andridge8). For example, some studies have reported that dietary intakes of Fe, vitamin B6, n-3 fatty acids, folate, vitamin B12, Se and Zn are closely related to anxiety(Reference Zhang, Kleiman-Weiner and Luo9–Reference Popa and Ladea12). However, in reality, people generally consume a combination of various foods and nutrients in each meal, not individual foods and nutrients(Reference Shu, Zheng and Zhang13). Moreover, individual nutrients or foods may also have interactive or synergistic effects that make it difficult to provide a complete picture of the relationship between diet and mental health(Reference Wang, Yang and Wang14). Consequently, a dietary pattern analysis has emerged as an alternative, holistic approach to examining the associations between overall diet and anxiety, and it allows us to better capture the role of multiple dimensions of diet in cognitive health, and potentially facilitate nutritional recommendations(Reference Hu15).
To date, several epidemiological studies have reported the association of dietary patterns with the risk of anxiety(Reference Salehi-Abargouei, Esmaillzadeh and Azadbakht5,Reference Yazdi, Roohafza and Feizi16–Reference Weng, Hao and Qian22) . Most of these studies, however, have been conducted in western populations(Reference Salehi-Abargouei, Esmaillzadeh and Azadbakht5,Reference Hosseinzadeh, Vafa and Esmaillzadeh18–Reference Vaz Jdos, Kac and Emmett21) , and evidence from Asia, including the Chinese population, is extremely limited. Until recently, only one published study has examined the association between dietary patterns and anxiety in Chinese, but it was done in adolescents(Reference Weng, Hao and Qian22). Furthermore, to the best of our knowledge, no study exploring the relationship between dietary patterns and the risk of anxiety in a middle-aged Chinese population has been reported. Hence, the purpose of the current study was to clarify the association of empirically derived dietary patterns with the risk of anxiety in middle-aged adults in eastern China.
Materials and methods
Study population
This study was carried out in the city of Linyi, Shandong Province, from May 2016 to June 2017, as reported previously(Reference Wang, Yang and Wang14). Shandong province is in the east coast of China with a population of 99 million, while Linyi is a prefecture-level city of Shandong, with a population of 11 million. The study sample was randomly selected using stratified cluster sampling from three areas (Lanshan, Luozhuang and Hedong) and nine counties (Lanling, Junan, Qishui, Tancheng, Mengyin, Pingyi, Feixian, Yinan and Linshu). A total of 1457 participants aged 45–59 years were recruited when attending their annual health examination at the Medical Center for Physical Examination, Linyi People’s Hospital, where the study participants were interviewed by trained staffs using a printed questionnaire. We excluded thirty-four participants with missing or incomplete dietary information in their questionnaires, twenty participants with history of cancer, fifteen participants with CVD, eleven participants with chronic kidney disease, ten participants with a total energy intake >12 552 or <3347·2 kJ/d, and seven participants with missing information on any of the variables used in the main analysis. Finally, 1360 participants were included in our analysis.
Assessment of dietary intake
Dietary assessment was performed by a trained dietician through a semi-quantitative FFQ that was designed and validated for the middle-aged Chinese population(Reference Wang, Yang and Wang14). For each food item in this FFQ, the participants were asked to recall their average frequency of consumption in the last year and the estimated portion size using local weight units (1 Liang = 50 g) or natural units (cups). To capture the frequency of food consumption, nine response options were provided, including never or occasionally, 1–3 times/month, 1–2 times/week, 3–4 times/week, 5–6 times/week, 1 time/d, 2 times/d and 3 times/d. Consequently, the selected frequency category for each food item was converted to an average daily intake and used in our analysis.
Assessment of anthropometric measurements
Height and weight were measured in light clothes and without shoes to the nearest 0·1 cm and 0·1 kg, respectively. BMI (kg/m2) was computed as weight in kilograms divided by height in metres-squared. Waist circumference (WC, cm) was measured at the umbilical region with an inelastic measuring tape at the end of normal expiration to the nearest 0·1 cm(Reference Ito, Kawakami and Tanisawa23). All measurements were conducted by the trained staffs using standardised procedures.
Assessment of blood pressure
A well-trained nurse measured the blood pressure using a standard mercury sphygmomanometer with the participant in sitting position after at least 5 min of rest. Then, the mean value of three measurements was used in the analysis.
Assessment of other variables
Information about education level (primary school or below, middle and high school, junior college or above), marital status (single and married) and smoking status (never smoker, former smoker and current smoker) was collected using a self-administered questionnaire. Physical activity was self-reported based on hours/week spent in different occupational, household, transportation and leisure time activities. Detailed information on physical activity is described elsewhere(Reference Wang, Yang and Wang14). Total energy intake was estimated through the semi-quantitative FFQ, expressed in kilojoules per day (kJ/d).
Definition of terms
A simplified Chinese version of the Generalised Anxiety Disorder Scale (GAD-7) was used to screen for anxiety symptoms. GAD-7 has been found to be a reliable and valid measurement of anxiety severity(Reference Herr, Williams and Benjamin24). Participants with scores 5–9 and ≥10 were considered to have mild and moderate to severe anxiety symptoms, respectively. Hypertension was defined as systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mmHg, or having received antihypertensive therapy(Reference Zhang, Zhang and Shi25). Obesity was defined by BMI ≥28 kg/m2(Reference Shu, Zheng and Zhang13).
Statistical analyses
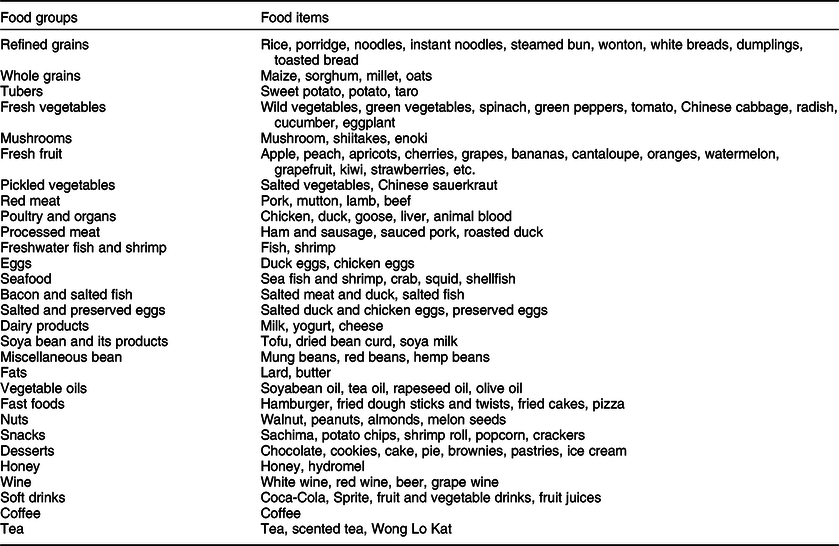
Details of dietary pattern scores derived by the factor analysis are described elsewhere(Reference Wang, Yang and Wang14). The eighty-five food items in this FFQ were aggregated into twenty-nine predefined food groups based on the similarity of type of food and nutrient composition (Table 1). The Kaiser–Meyer–Olkin (KMO) measure of sampling adequacy and the Bartlett’s test of sphericity were used to evaluate the adequacy of correlation matrices with the data. A factor analysis (principal components) was used to derive the major dietary patterns based on the frequency of consumption of twenty-nine predefined food groups in our analysis. The factors were rotated by orthogonal transformation (varimax rotation) to achieve a simpler structure with greater interpretability. The number of retained patterns was determined according to eigenvalue >1·5, scree plot and the interpretability of factors(Reference Wang, Yang and Wang14). Labelling of dietary patterns was based on the interpretation of foods with high factor loadings for each dietary pattern(Reference Newby and Tucker26). Finally, only food groups with an absolute factor loading ≥0·3 were considered to be important contributors to this pattern and included in the present study.
Table 1 Food grouping used in the dietary pattern analysis
All statistical analyses were conducted with the IBM Statistical Package SPSS, version 23.0 (SPSS Inc). First, data were tested for normality using histograms, and logarithmic transformation was applied whenever appropriate. Data were expressed as mean (sd) for continuous variables, and sum (percentages) for categorical variables. We used the χ 2 test to assess the differences in categorical variables, and one-way ANOVA was used to examine significant differences in continuous variables across quartile categories of dietary pattern scores. Besides, we applied multivariate logistic regression to evaluate the association between dietary patterns and the risk of anxiety, adjusting for potential confounders. Model 1 was adjusted for age (years). Model 2 was adjusted for age (years), gender (male/female), marital status, education level (primary school or below, middle and high school, junior college or above), smoking status (never, former and current), chronic diseases (obesity, hypertension and diabetes), physical activity level (MET-h/week), economic income, use of antidepressant drugs and total energy intake (kJ/d). Model 3 was further adjusted for BMI. All tests were two-sided, and P-values <0·05 were considered significant.
Results
The characteristics of participants with and without anxiety are shown in Table 2. Of the 1360 participants, the overall prevalence of anxiety was 5·4 % (males 1·6 %; females 3·8 %). There were significant differences between participants with and without anxiety by age, gender, education and prevalence of diabetes and hypertension (P < 0·05).
Table 2 Characteristics according to participants with and without anxiety*
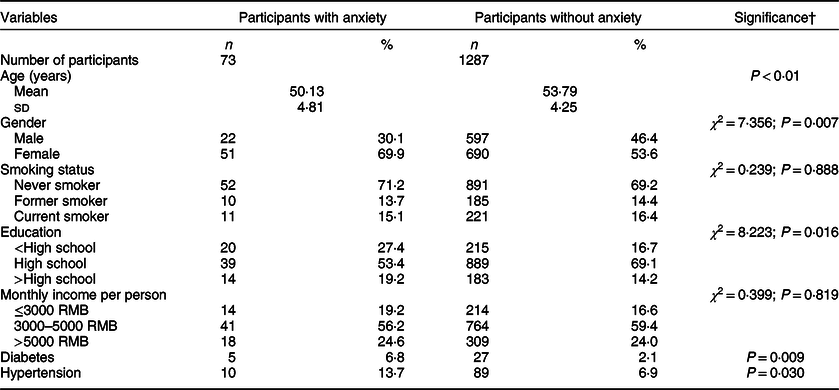
RMB, Ren min bi.
* Categorical variables are presented as sum and percentages, and continuous variables are presented as mean and sd.
† P-values for continuous variables (ANOVA) and for categorical variables (χ 2 test).
Both the KMO index (0·633) and Bartlett’s test (P < 0·001) showed that the correlation among the variables was sufficiently strong for a factor analysis(Reference Zhang, Zhang and Shi25). Four dietary patterns in this population have been identified previously(Reference Wang, Yang and Wang14). The traditional Chinese dietary pattern is characterised by a high consumption of whole grains, fresh vegetables, mushrooms, pickled vegetables, fresh fruits, poultry and organs, freshwater fish and shrimp, egg, soya bean and its products, vegetable oil and tea. The western dietary pattern is characterised by a high consumption of red meat, processed meat, freshwater fish and shrimp, seafood, dairy products, fats, fast foods, nuts, snacks, desserts, soft drinks and coffee. The grains–vegetables dietary pattern is characterised by a high consumption of whole grains, tuber, fresh vegetables, fresh fruit, miscellaneous bean and honey. The high-salt dietary pattern is characterised by a high consumption of refined grains, mushrooms, pickled vegetables, processed meat, bacon and salted fish, salted and preserved eggs, miscellaneous bean and wine. Overall, these factors explained 36·9 % of the whole variance. The factor loading matrices of the four dietary patterns are shown in Table 3.
Table 3 Factor loading matrices for the four dietary patterns*
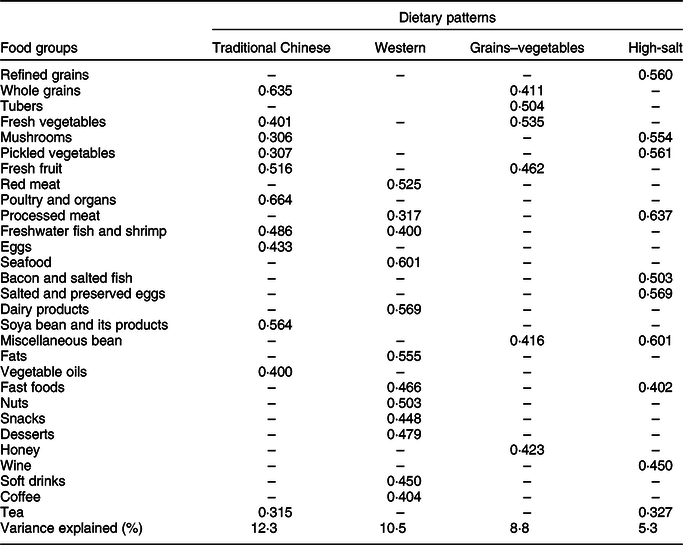
* Absolute values <0·3 were excluded for simplicity.
The characteristics of study participants by quartile (Q) categories of the major dietary pattern score in Linyi are shown in Table 4. Compared with the participants in the lowest quartile, those in the highest quartile of the traditional Chinese dietary pattern were more likely to be older, female, non-smokers with a higher income and education level and had lower WC, total energy intake and physical activity level. Besides, the participants in the top quartile of the western dietary pattern were more likely to be younger, male with higher income, had higher BMI, WC, total energy intake and income, and had lower physical activity level. Similarly, in comparison to the participants from the lowest quartile of the grains–vegetables dietary pattern, those in the highest quartile were more likely to be older, female, never-smoker with higher income and had lower BMI, WC, total energy intake, prevalence of diabetes and hypertension and physical activity level. In contrast, the participants in the highest quartile of the high-salt pattern were more likely to be male and had higher WC and lower education level and income than those in the lowest quartile.
Table 4 Characteristics of study participants in Linyi by quartile (Q) categories of major dietary pattern scores*
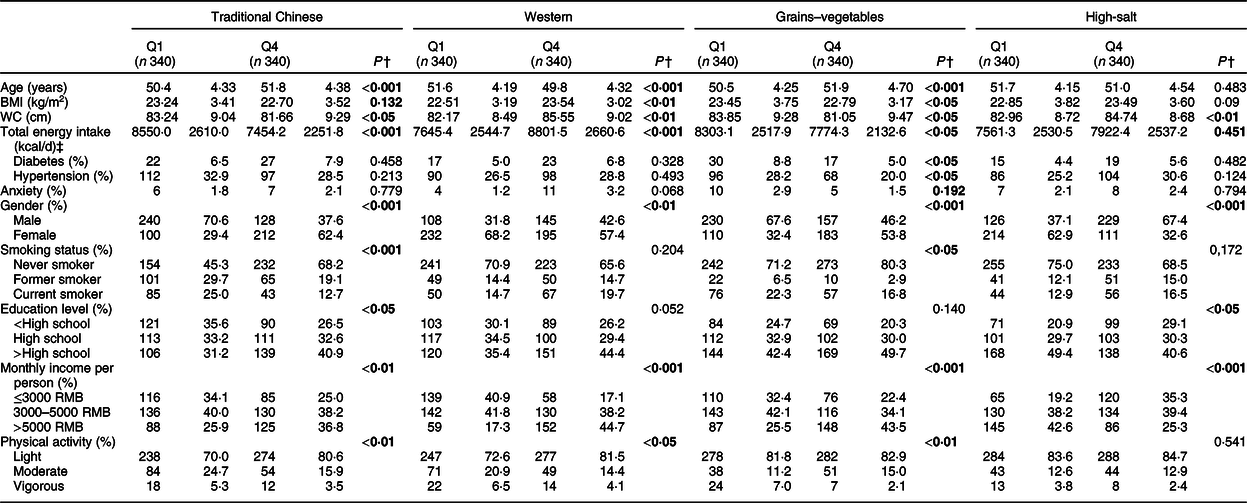
RMB, Ren min bi; WC, waist circumference.
Bold values indicate that the differences are statistically significant.
* Categorical variables are presented as sum and percentages, and continuous variables as mean and sd.
† P-values for continuous variables (ANOVA) and for categorical variables (χ 2 test). P < 0·05 is considered statistically significant.
‡ To convert kcal to kJ, multiply it by 4·184.
Multivariable-adjusted OR (95 % CI) for anxiety across quartile (Q) categories of dietary pattern scores are shown in Table 5. After adjusting for potential confounders, participants in the highest quartile of the western dietary pattern had greater odds for anxiety (OR 1·35, 95 % CI 1·000, 3·086, P < 0·05) compared with those in the lowest quartile. Besides, compared with the lowest quartile of the grains–vegetables pattern, the highest quartile had lower odds for anxiety (OR 0·78, 95 % CI 0·574, 1·000, P < 0·05). These associations remained significant even after adjusting for potential confounders. However, the traditional Chinese and high-salt dietary patterns showed no significant associations with the risk of anxiety (P > 0·05).
Table 5 Multivariable-adjusted OR (95 % CI) for anxiety across quartile (Q) categories of dietary pattern scores*
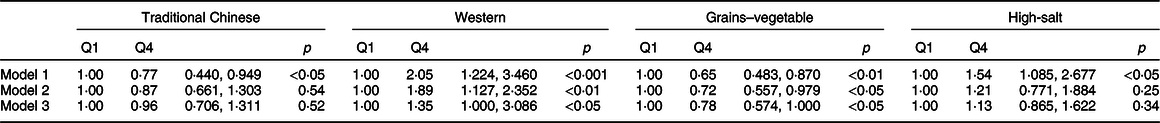
Q1, the lowest quartile of dietary patterns (reference); Q4, the highest quartile of dietary patterns.
* Model 1 adjusted for age; model 2 further adjusted for age, gender, marital status, education level, smoking status, chronic diseases (including obesity, hypertension and diabetes), physical activity, income, use of antidepressant drugs and total energy intake; model 3 additionally adjusted for BMI.
Discussion
In the current study, four dietary patterns were identified: traditional Chinese, western, grains–vegetables and high-salt diets. The main findings of our study are that the western pattern is associated with an increased risk, whereas the grains–vegetable pattern is associated with a reduced risk of anxiety. Limited epidemiological studies have examined the associations between dietary patterns and anxiety in China. To the best of our knowledge, this is the first study describing the relationship between major dietary patterns and the risk of anxiety in middle-aged adults in eastern China.
In the current study, we found no association between the traditional Chinese pattern and the risk of anxiety. Our findings contrast a previous study that showed that the health-conscious pattern is significantly associated with a lower risk of anxiety(Reference Vaz Jdos, Kac and Emmett21). The complex nature of this pattern may explain the inconsistent findings to some extent. On the one hand, the consumption of vegetables and fruits rich in folate and antioxidants has been associated with reduced inflammation and oxidative stress(Reference Murakami and Sasaki27). Recent studies have demonstrated that elevated inflammation plays an important role in psychological disorders(Reference Eswarappa, Neylan and Whooley28). Moreover, a higher consumption of fish rich in long-chain n-3 PUFA could contribute to brain functioning and serotonin neurotransmission(Reference Kiecolt-Glaser29). Furthermore, a previous study has also reported that tea consumption significantly reduced depressive and anxiety symptoms among community-living elderly(Reference Chan, Yong and Sun30). On the other hand, pickled vegetables contain large amounts of salt, which could increase the risk of hypertension, a risk factor for mental disorders(Reference Liang, Shan and Ding31). In addition, prior observational research has also shown that saturated fats abundantly found in animal organs are positively associated with diabetes, atherosclerosis and CVD(Reference Jacka, Pasco and Williams7). Hasan et al. have reported that diabetes is associated with a 2·6 times increased likelihood of having a current anxiety disorder in Australian women(Reference Hasan, Clavarino and Dingle32). Furthermore, the null association could be caused by the differences in cooking methods. In the Chinese diet, vegetables are generally eaten cooked. In a word, the above possibilities could not be excluded in this study.
The western dietary pattern, consisting of red meat, processed meat, freshwater fish and shrimp, seafood, dairy products, fats, fast foods, nuts, snacks, desserts, soft drinks and coffee, was positively associated with the risk of anxiety in our analysis. Consistent with our results, a western dietary pattern in Norwegian adults has been associated with an increased odds for anxiety(Reference Jacka, Mykletun and Berk33). The deleterious effect of the western dietary pattern on anxiety could be explained by its unhealthy components such as red meat, processed meat, seafood, fast foods, nuts, snacks, desserts, wine, soft drinks and coffee. First, red meat, processed meat, fats and fast foods containing high amounts of saturated fats and cholesterol have been shown to be associated with an increased risk of CVD and inflammation. As previously reported(Reference Eswarappa, Neylan and Whooley28), CVD and elevated inflammation might play a key role in psychological disorders. Second, a previous study has indicated that the western dietary pattern is significantly associated with an increased risk of diabetes(Reference Shu, Shen and Li34), an important risk factor for anxiety(Reference Hasan, Clavarino and Dingle32). Third, high intakes of desserts and fast foods were positively associated with the markers of systemic inflammation(Reference Lopez-Garcia, Schulze and Fung35).
In our analysis, we observed a protective effect of the grains–vegetables dietary pattern on anxiety. These findings are in line with previous reports documenting an inverse association between the health-conscious dietary pattern (high consumption of fruit and vegetables, fish and whole-grain products) and anxiety(Reference Vaz Jdos, Kac and Emmett21). There are several possible explanations for the inverse association. First, the apparent protective effect of this pattern on anxiety might be related to their high concentrations of antioxidant substances such as vitamin C, vitamin E and other carotenoid compounds. Earlier studies have shown that antioxidant compounds such as vitamins C and E abundantly found in fruits and vegetables might give protection against neurodegeneration by scavenging free radicals(Reference Mangialasche, Solomon and Kåreholt36). Second, a higher consumption of whole grains and vegetables could increase the amount of dietary fibre, which is inversely correlated with depression symptoms(Reference Miki, Eguchi and Kurotani37). Third, fresh fruits and vegetables with anti-inflammatory properties have been shown to influence the concentrations of monoamines, which are thought to play an important role in the regulation of emotions and cognition(Reference Kiecolt-Glaser29). Finally, fruits, vegetables and whole grains are an important source of B vitamins and rich in folate, which have favourable psychological effects through reducing the level of serum homocysteine and through the synthesis of monoamines, including dopamine and serotonin, in the brain(Reference Kamphuis, Geerlings and Grobbee38).
The high-salt pattern is characterised by a high consumption of refined grains, mushrooms, pickled vegetables, processed meat, bacon and salted fish, salted and preserved eggs, miscellaneous bean, fast food, wine and tea. We could not find a significant association of this pattern with anxiety in the present study. There are several possible explanations for this null association. On the one hand, previous studies have reported that refined grains are associated with elevated C-reactive protein, an important risk factor for anxiety(Reference Hosseinzadeh, Vafa and Esmaillzadeh18). In addition, a high consumption of processed meat has also been associated with decreased levels of brain-derived neurotrophic factor(Reference Molteni, Barnard and Ying39). This factor has been shown to protect the neurons from oxidative stress and induces neurogenesis in the short term(Reference Shirayama, Chen and Nakagawa40). Meanwhile, pickled vegetables, processed meat and bacon and salted fish have a high salt concentration that could increase the risk of hypertension, a risk factor for mental disorders(Reference Liang, Shan and Ding31). On the other hand, as mentioned above, antioxidant compounds, for example, vitamins C and E abundantly found in mushroom and vegetables, could protect against neurodegeneration by scavenging free radicals(Reference Mangialasche, Solomon and Kåreholt36). Likewise, fish contains a large amount of long-chain n-3 PUFA, which could affect mood by altering the brain serotonergic function and its immune-neuroendocrine effects(Reference Kiecolt-Glaser29). Evidence suggests that the addition of n-3 fatty acids to antidepressants might improve mood in major depression(Reference Gertsik, Poland and Bresee41). Furthermore, the null result could also be due to reverse causality. Participants with anxiety may be advised to change their dietary behaviour and food choices. Taken together, this possibility could not be excluded in this study.
Strengths and limitations
This study has several strengths and limitations. First, to the best of our knowledge, this is the first study reporting the associations between major dietary patterns and the risk of anxiety in middle-aged adults in China. Second, dietary data of all participants were collected by trained dieticians using a semi-quantitative FFQ. The validity and reliability of this FFQ is described elsewhere(Reference Wang, Yang and Wang14). Third, we controlled for some confounders that might affect psychological conditions in our analysis. However, several limitations should also be taken into consideration when interpreting the results. First, due to the cross-sectional design of this study, causality cannot be inferred, and further prospective studies are needed to confirm our findings. Second, subjective or arbitrary decisions, for example, the number of factors extracted, methods of rotation and labelling of included factors in the factor analysis, should be taken into account(Reference Hu15). Third, although we tried to control for several confounding variables in our analysis, residual confounding from unknown or unmeasured factors was inevitable. Finally, the study participants were specifically restricted to middle-aged adults in Linyi city, Shandong Province, which might limit the generalisability of our findings.
Conclusions
We found that the western pattern is associated with an increased risk of anxiety, while the grains–vegetables pattern is associated with a reduced risk of anxiety. Our findings support the dietary recommendation promoting a high consumption of vegetables, fruits and grains and a low consumption of red meat and fast foods to prevent anxiety among the middle-aged Chinese population. Further prospective studies are required to confirm these findings.
Acknowledgements
Acknowledgements: We thank all the participants from the Department of Psychology, Linyi People’s Hospital and the Department of Psychiatry and Psychology, Xingtai People’s Hospital for their assistance and support. We also acknowledge the Medical Center for Physical Examination and Scientific Research Office, Linyi People’s Hospital for their important contributions to data collection in this study. Financial support: None. Conflicts of interest: The authors declare that there is no conflict of interests. Authorship: F.X. and J.L. conceived and designed the experiments. B.-Q.C., F.X. and J.L. conducted research. J.-L.Z. and T.C. analysed data, and J.L. wrote the paper. All authors read and approved the final manuscript. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving study participants were approved by the Institutional Review and Ethics Committee of Linyi People’s Hospital. Signed informed consent was obtained from all participants.








