Introduction
Fear of death is a uniquely human experience (Becker, Reference Becker1973). It has been the subject of philosophers, writers and artists for thousands of years (Menzies, Reference Menzies, Menzies, Menzies and Iverach2018a), from the Buddhist and Stoic philosophers, to William James, who described it as ‘the worm at the core’ of human existence (James, Reference James1985/1902; p. 119). According to Becker (Reference Becker1973), awareness of our own finitude and its inevitability results in overwhelming terror. Terror management theory (TMT), an elaboration of Becker’s work, is the predominant theoretical approach to death anxiety (Menzies et al., Reference Menzies, Menzies and Iverach2015). TMT asserts that humans use the defences of cultural worldviews and self-esteem to manage this fear (Yetzer and Pyszczynski, Reference Yetzer and Pyszczynski2019). Cultural worldviews are belief systems that consist of values, moral standards and behaviours which provide a sense of meaning, structure and purpose to human existence. Adhering to a cultural worldview offers a buffer against short-term anxiety, and provides individuals with a sense of self-esteem and symbolic immortality.
Hundreds of TMT studies demonstrate that cultural worldviews and self-esteem buffer death anxiety in non-clinical populations (e.g. Greenberg et al., Reference Greenberg, Vail and Pyszczynski2014; Maxfield et al., Reference Maxfield, John and Pyszczynski2014; Yetzer and Pyszczynski, Reference Yetzer and Pyszczynski2019). Moreover, there is growing empirical evidence that fears of death may drive the maladaptive behaviour we see in clinical psychology. Preliminary evidence points to the role of death anxiety in various disorders including panic disorder, specific phobias, separation and attachment anxieties, somatic symptom disorders and depression (Iverach et al., Reference Iverach, Menzies and Menzies2014; Menzies et al., Reference Menzies, Sharpe and Dar-Nimrod2021). A recent study explored the relationships between death anxiety and psychopathology in treatment-seeking adults diagnosed with a range of mental disorders (Menzies et al., Reference Menzies, Sharpe and Dar-Nimrod2019). It found that fear of death was highly correlated with symptom severity of 12 disorders, and moreover that death anxiety strongly predicted markers of psychopathology such as number of hospitalisations, lifetime diagnoses and distress.
The strongest evidence for the role of death anxiety in psychiatric disorders can be found in obsessive compulsive disorder (OCD). Menzies et al. (Reference Menzies, Menzies and Iverach2015) observe that verbal reports and behaviours of most sufferers with OCD can be readily linked to the theme of death. Clients with the contamination subtype report fears of toxins, poisons, bodily fluids, diseases and the expectation of subsequent contamination and death (Menzies and Dar-Nimrod, Reference Menzies and Dar-Nimrod2017). Individuals who compulsively check power outlets, stoves, heaters, window and door locks reportedly do so to prevent fires, home invasions or electrocution, all of which could ultimately result in death (Menzies et al., Reference Menzies, Menzies and Iverach2015). Many people with OCD also experience magical thinking, believing that one’s thoughts could have a causal influence over reality (Menzies et al., Reference Menzies, Zuccala, Sharpe and Dar-Nimrod2021). These clients frequently report obsessions in which they are responsible for the death of a loved one.
Consistent with these verbal reports from clients, associations have been found between OCD and death anxiety among treatment-seeking, diagnosed samples. Menzies and Dar-Nimrod (Reference Menzies and Dar-Nimrod2017) found a significant positive correlation between death anxiety and OCD severity among a large sample of individuals with OCD. Furthermore, a recent study found that death anxiety was significantly associated with the severity of all six measured symptom clusters of OCD, including contamination, obsessions, checking, hoarding, indecisiveness, and ‘just right’ (e.g. needing to re-order one’s possessions until they feel ‘just right’; Menzies et al., Reference Menzies, Zuccala, Sharpe and Dar-Nimrod2020a). In addition, death anxiety has been shown to influence the pathway towards OCD, with higher death anxiety associated with a greater number of disorders experienced prior to the onset of OCD (Menzies et al., Reference Menzies, Zuccala, Sharpe and Dar-Nimrod2021).
Experimental research to date also demonstrates the causal role of death anxiety in OCD. Strachan and colleagues (Reference Strachan, Schimel, Arndt, Williams, Solomon, Pyszczynski and Greenberg2007) demonstrated that death reminders can exacerbate handwashing behaviours in students who report excessive hand washing. In an extension of this research, Menzies and Dar-Nimrod (Reference Menzies and Dar-Nimrod2017) compared individuals with the washing subtype of OCD, to individuals with OCD who did not have contamination concerns (i.e., non-washers). Among OCD washers, reminders of death significantly increased washing duration, and soap and paper towel usage, compared with those who had not been primed with death. No such effects were found among the non-washers. This suggests that mortality concerns may drive compulsive washing behaviour.
Thus, experimental studies have demonstrated the relevance of death anxiety (and by extension, TMT) to OCD. However, one aspect of TMT remains unexamined in OCD. Whilst TMT originally posited cultural worldview defence and self-esteem as the predominant protectors against death anxiety, some have argued that there is a third buffer – the attachment system (Maxfield et al., Reference Maxfield, John and Pyszczynski2014; Mikulincer, Reference Mikulincer2019). Cultural worldviews and a sense of self-esteem are established in childhood, and are firmly entrenched in the attachments developed with the primary caregivers. That is, children learn to adopt their parents’ values and worldviews to reduce parental disapproval (Greenberg et al., Reference Greenberg, Vail and Pyszczynski2014). By meeting accepted standards for being valuable and good, children in turn receive love and protection from their caregivers, thus providing a base for the development of self-esteem (Greenberg et al., Reference Greenberg, Vail and Pyszczynski2014). According to Yetzer and Pyszczynski (Reference Yetzer and Pyszczynski2019), the failure to develop secure attachment and self-esteem in childhood can undermine the development of the anxiety-buffering system. It is the failure of this anxiety-buffering system that is believed to result in death anxiety (Yetzer and Pyszczynski, Reference Yetzer and Pyszczynski2019). Furthermore, when self-esteem fails to develop due to childhood adversity or trauma, individuals often resort to alternative tactics to manage their anxiety, such as phobic avoidance, obsessive reassurance-seeking or self-medicating through substance use (Maxfield et al., Reference Maxfield, John and Pyszczynski2014). Not only are these individuals anxious due to an absence of secure attachments, they are more prone to adopting maladaptive coping strategies, and also unable to rely on secure relationships for emotion regulation during times of stress (Maxfield et al., Reference Maxfield, John and Pyszczynski2014).
Children who lack early positive experiences with their caregivers often develop an insecure attachment style (Mikulincer, Reference Mikulincer2019). Those who seek proximity by being overly worried or demanding are referred to as ‘anxiously attached’. They are often hypervigilant to potential threats and internal distress signals, and lack belief in their own self-efficacy, leading to the use of maladaptive proximity-seeking strategies such as exaggerated vulnerability and helplessness. Children who avoid intimacy and demonstrate extreme affect avoidance are known as ‘avoidant attached’ (Mikulincer, Reference Mikulincer2019). These individuals find emotions such as fear, guilt, anger and shame highly aversive as they may signal vulnerability, and therefore attempt to downregulate emotions and avoid affective responses to attachment figure availability. Insecurely attached individuals will adopt strategies to either ‘hyperactivate’ (anxiously attached) or ‘deactivate’ (avoidant attached) the attachment behavioural system. Whilst securely attached individuals can use their healthier self-esteem and interpersonal relationships as protection when anxieties are triggered, insecurely attached individuals resort to less adaptive coping mechanisms (Mikulincer, Reference Mikulincer2019; Yetzer and Pyszczynski, Reference Yetzer and Pyszczynski2019).
Notably, securely attached adults report lower levels of death anxiety compared with insecurely attached individuals (Mikulincer and Florian, Reference Mikulincer and Florian2000). Experimental findings further elucidate this differential response to death. Two studies have shown that participants with insecure attachment styles demonstrate heightened worldview defence following reminders of death, compared with individuals with secure attachment styles (Caspi-Berkowitz, Reference Caspi-Berkowitz2003; Mikulincer and Florian, Reference Mikulincer and Florian2000). Thus, without secure attachment bonds to rely on when death is salient, these individuals attempt to enhance their impoverished self-concept via other strategies (i.e. defending their shared cultural worldviews).
Unfortunately, no study to date has explored the moderating role of attachment on the relationship between OCD and death anxiety. Although the evidence supporting the role of attachment in buffering against death anxiety appears clear, existing studies have relied on non-clinical samples. Furthermore, despite the compelling outcomes in the experimental study of death anxiety in an OCD sample (Menzies and Dar-Nimrod, Reference Menzies and Dar-Nimrod2017), this study neglected to include a measure of attachment – a known buffer against death anxiety (Mikulincer, Reference Mikulincer2019). While a later study by Menzies and colleagues (Reference Menzies, Sharpe and Dar-Nimrod2019) did administer a measure of attachment styles, the study failed to find a moderating effect of attachment on death anxiety and psychopathology. This was possibly due to the use of a one-item attachment measure by Hazan and Shaver (Reference Hazan and Shaver1987) that has been criticised for its brevity (Collins and Read, Reference Collins and Read1990). In addition, the study included a clinical sample with various diagnoses. As such, the role of attachment style in moderating the relationship between death anxiety and OCD severity remains unclear.
Given these limitations, the current study aimed to investigate the relationship between death anxiety and the possible moderating effects of attachment in a treatment-seeking sample of individuals with OCD, using a comprehensive measure of attachment style. Given previous findings it was hypothesised that: (1) there will be a significant correlation between death anxiety and OCD scale scores, and (2) attachment style will moderate the relationship between death anxiety and OCD.
Method
Participants
An a priori power analysis using G*Power was conducted based on previous effect sizes reported in the literature (e.g. Menzies and Dar-Nimrod, Reference Menzies and Dar-Nimrod2017; Menzies et al., Reference Menzies, Zuccala, Sharpe and Dar-Nimrod2020a). This revealed that a sample size of 29 participants would allow 80% power to detect a correlation of r = .5 at α = .05.
Inclusion criteria were: (1) being over 18 years old, (2) having a current diagnosis of OCD, and (3) OCD being the principle diagnosis, if additional diagnoses were present. A total of 52 clients at a private clinical psychology practice in Sydney, Australia, who presented with OCD were offered inclusion in the present study; 48 consented to participate and completed a battery of measures. The sample had a mean age of 31.2 years (SD = 11.70) and consisted of 33 women (68.8%), with 45 participants identifying as Caucasian (93.8%) and three identifying as Asian (6.3%). Participants had on average 15.95 years of education (SD = 1.87). A total of 37.5% identified as married or in a de facto relationship, 58.3% identified as single, and 4.2% were divorced. Participants did not receive any compensation for taking part.
Procedure
Data collection took place between April and August 2020, during the COVID-19 pandemic. A clinical psychologist with significant clinical and research experience administered the Anxiety and Related Disorders Interview Schedule for DSM-5 (ADIS-5L), to determine eligibility (i.e. a current principal diagnosis of OCD). All participants were then administered the battery of self-report measures. These measures were completed individually by participants at the psychology practice site, using pencil and paper.
Measures
The Anxiety and Related Disorders Interview Schedule for DSM-5: Lifetime Edition (ADIS-5L; Brown and Barlow, Reference Brown and Barlow2014)
The ADIS-5L is a structured clinical interview that assesses current and lifetime diagnoses of anxiety, mood, and obsessive-compulsive and related disorders according to DSM-5 criteria. In the current study, it was also used to assess markers of psychopathology (e.g. severity of diagnosis, overall distress). Good to excellent inter-rater reliability and agreement has been determined for previous versions of the ADIS (Brown et al., Reference Brown, Di Nardo, Lehman and Campbell2001).
The Multidimensional Fear of Death Scale (MFODS; Hoelter, Reference Hoelter1979)
The MFODS is a 42-item self-report measure with good psychometric properties (Walkey, Reference Walkey1982). It has shown strong construct, discriminant and convergent validity (McClatchey and King, Reference McClatchey and King2015) and excellent internal consistency (Menzies et al., Reference Menzies, Sharpe and Dar-Nimrod2019). There are eight subscales, with higher scores representing less death anxiety. An overall score can be generated by adding all the subscale scores together. Internal consistency in the present sample was excellent (α = .95).
The Vancouver Obsessive Compulsive Inventory (VOCI; Thordarson et al., Reference Thordarson, Radomsky, Rachman, Shafran, Sawchuk and Hakstian2004)
The VOCI is 55-item self-report measure with six subscales. Studies have shown that it has good psychometric properties (Thordarson et al., Reference Thordarson, Radomsky, Rachman, Shafran, Sawchuk and Hakstian2004). Previous studies have utilised the total VOCI score as an indication of overall OCD severity (e.g. Menzies and Dar-Nimrod, Reference Menzies and Dar-Nimrod2017; Menzies et al., Reference Menzies, Sharpe and Dar-Nimrod2019). A higher score on this measure indicates more severe OCD symptoms. The internal consistency of the overall scale in the current study was excellent (α = .95), further supporting the use of the total score as a reliable measure of OCD severity.
The Big Five Aspects Scale (BFAS; DeYoung et al., Reference DeYoung, Quilty and Peterson2007)
The BFAS was utilised to control for neuroticism being a potential confounding factor. Only the 20-item neuroticism subscale of the BFAS was employed. The BFAS has good psychometric properties (DeYoung et al., Reference DeYoung, Quilty and Peterson2007), and strong criterion validity (DeYoung et al., Reference DeYoung, Weisberg, Quilty and Peterson2013). The internal consistency in the present sample was excellent (α = .95).
Experiences in Close Relationships-Revised (ECR-R; Fraley et al., Reference Fraley, Waller and Brennan2000)
The ECR-R is a 36-item self-report measure with good psychometric properties (Sibley et al., Reference Sibley, Fischer and Liu2005), construct validity (Fairchild and Finney, Reference Fairchild and Finney2006) and good internal consistency (Goodall et al., Reference Goodall, Trejnowska and Darling2012). The ECR-R instructs participants to rate how they generally feel in emotionally intimate relationships, and is therefore not impacted by the respondent’s current relationship status. Eighteen items measure anxious attachment and 18 items measure avoidant attachment, with higher scores on each subscale indicating greater levels of attachment difficulties, and lower scores indicating greater attachment security. In the present sample, the internal consistency for the anxious subscale was excellent (α = .90), and for the avoidant subscale was acceptable (α = .79).
Results
The characteristics of the present sample are reported in Table 1. MFODS scores for the sample were significantly lower than general population norms (e.g. mean = 150.20; Sharma et al., Reference Sharma, Monsen and Gary1997), indicating higher death anxiety in the sample compared with normative community data. A total of 66.7% of the sample had an additional diagnosis to OCD, the most common of which were generalised anxiety disorder (31.3%) and persistent depressive disorder (18.8%). To examine the distribution of OCD subtypes in the current sample, Z-scores were created for the six VOCI subscales. Next, we identified which subtype each participant had the highest Z-score on, consistent with the method used by Menzies et al. (Reference Menzies, Zuccala, Sharpe and Dar-Nimrod2020a). This resulted in 27.1% of the sample scoring highest on the ‘contamination’ subscale, 20.8% scoring highest on ‘indecisiveness’, 18.8% on ‘obsessions’, 14.6% on ‘hoarding’, 10.4% on ‘checking’, and 8.3% on ‘just right’.
Table 1. Summary of participant characteristics (n = 48)
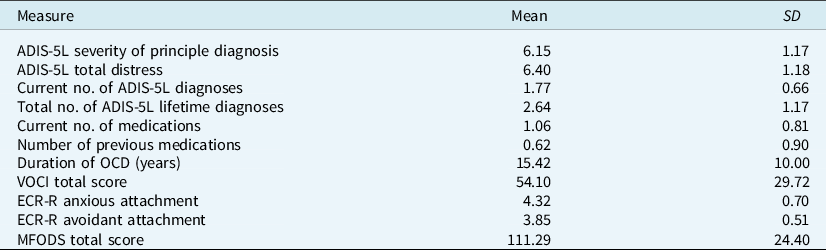
ADIS-5L, Anxiety and Related Disorders Interview Schedule for DSM-5 – Lifetime Version; VOCI, Vancouver Obsessional Compulsive Inventory; ECR-R, Experience in Close Relationships-Revised; MFODS, Multidimensional Fear of Death Scale, on which higher scores indicate less death anxiety, and lower scores indicate higher death anxiety.
To explore the first hypothesis, correlations were examined between death anxiety scores and OCD severity. This revealed a significant and sizeable correlation between total MFODS and total VOCI score (r = –.72), suggesting that higher levels of death anxiety were associated with significantly higher OCD severity. Consistent with previous studies (e.g. Menzies et al., Reference Menzies, Sharpe and Dar-Nimrod2019), additional analyses investigated whether these results could be confounded by a third variable, neuroticism. For this purpose, a hierarchical regression was conducted, with BFAS scores entered in the first step, and both BFAS and MFODS scores entered in the second step. Regression analyses indicated that MFODS scores significantly predicted total VOCI scores, above and beyond the effects of neuroticism: β = –.556, t 45 = –5.26, p<.0001, ΔR 2 = .240.
The results of the ECR-R for this sample indicated significantly higher attachment insecurity (see Table 1), with scores more than one standard deviation above non-clinical community norms for attachment anxiety and avoidance (e.g. means of 3.17 and 2.78, respectively; Fairchild and Finney, Reference Fairchild and Finney2006). However, neither anxious nor avoidant attachment style significantly predicted OCD severity ratings: β = .090, t 45 = .599, p = .552, and β = –.047, t 45 = –.312, p = .756, respectively. Stepwise hierarchical regression analysis was conducted to explore the potential moderating role of attachment in the relationship between OCD severity and death anxiety. MFODS, and ECR anxious and avoidant attachment scores were entered in the first step of the regression analysis. In order to avoid potentially high multicollinearity, variables were mean centred, and two interaction terms between MFODS and ECR anxious and avoidant attachment scores were created. In the second step, neither ERC anxious attachment, β = –.062, t 45 = –.553, p = .583, nor ECR avoidant attachment, β = .076, t 45 = .702, p = .487, significantly moderated the relationship between MFODS and VOCI scores, ΔR 2 = .007.
Given the strong associations that have previously been found between death anxiety and markers of psychopathology, secondary analysis was undertaken to further explore these relationships in the current sample (Table 2). Significant correlations were found between all markers of psychopathology assessed using the ADIS-5L and MFODS scores (all p-values<.002).
Table 2. Summary of Pearson correlations between total MFODS score and psychopathology markers using the ADIS-5L (n = 48)
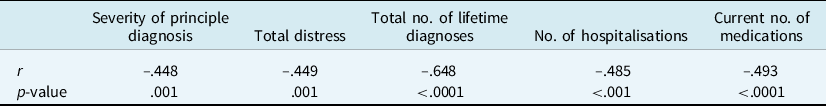
ADIS-5L, Anxiety and Related Disorders Interview Schedule for DSM-5 – Lifetime Version; MFODS, Multidimensional
Fear of Death Scale, in which higher scores indicate less death anxiety, and lower scores indicate higher death anxiety.
Discussion
Consistent with the first hypothesis, sizeable positive correlations were found between OCD scores and death anxiety. Furthermore, these effects were not explained by neuroticism. That is, in support of previous findings (Menzies and Dar-Nimrod, Reference Menzies and Dar-Nimrod2017; Menzies et al., Reference Menzies, Sharpe and Dar-Nimrod2019), after controlling for neuroticism, death anxiety continued to significantly predict OCD severity scores. This finding provides additional support for the assertion that death anxiety may play a crucial role in clinical disorders such as OCD (Iverach et al., Reference Iverach, Menzies and Menzies2014; Menzies and Dar-Nimrod, Reference Menzies and Dar-Nimrod2017; Menzies et al., Reference Menzies, Sharpe and Dar-Nimrod2019; Menzies et al., Reference Menzies, Zuccala, Sharpe and Dar-Nimrod2020a). Secondary analysis was conducted to explore whether death anxiety was related to a range of psychopathological markers. In support of research by Menzies and Dar-Nimrod (Reference Menzies and Dar-Nimrod2017), moderate to large correlations were found between fear of death and total distress scores, number of lifetime diagnoses, number of medications and hospitalisations. Thus, these findings are in line with the argument that fear of death is a transdiagnostic construct (Iverach et al., Reference Iverach, Menzies and Menzies2014).
Contrary to the second hypothesis, attachment style did not moderate the relationship between OCD and death anxiety. Although this finding was somewhat unexpected given prior findings that suggest attachment style buffer against fear of death (Maxfield et al., Reference Maxfield, John and Pyszczynski2014; Mikulincer, Reference Mikulincer2019; Yetzer and Pyszczynski, Reference Yetzer and Pyszczynski2019), it is consistent with the one study which has explored these relationships in clinical populations (Menzies et al., Reference Menzies, Sharpe and Dar-Nimrod2019). The failure to detect a buffering effect of secure attachment against death anxiety may simply support the original supposition of TMT. That is, that psychological disorders arise when defence of cultural worldview, self-esteem boosting activities and secure attachments fail to sufficiently protect the individual against existential threat (Iverach et al., Reference Iverach, Menzies and Menzies2014). Despite extensive research demonstrating that attachment style buffers against fear of death even when the first two defences fail, these studies have been conducted in general community samples rather than clinical populations (Yetzer and Pyszczynski, Reference Yetzer and Pyszczynski2019). It is therefore possible that secure attachments may be sufficient to protect psychologically robust individuals against existential terror, but are insufficient in the presence of clinical levels of distress.
The failure to find a buffering effect may also be due to the severe levels of death anxiety found in this clinical population, above and beyond the high levels of overall distress. It is possible that the normally attenuating effects of secure attachment were an inadequate protective mechanism in the face of heightened death anxiety. Death anxiety in the current sample was significantly higher than community norms (Sharma et al., Reference Sharma, Monsen and Gary1997). Moreover, compared with non-clinical populations (e.g. Fairchild and Finney, Reference Fairchild and Finney2006), patients in the present study reported higher rates of both anxious and avoidant attachment patterns. As such, it is possible that the usually effective protection of a secure attachment is rendered inadequate in individuals with a mental illness who lack secure attachments and report heightened death anxiety.
Another possibility that has yet to be explored in the literature is the notion that even secure attachments could be cause for concern in individuals with a mental illness, particularly OCD. Many verbal reports from OCD patients suggest that magical thinking and engagement in compulsive rituals are attempts to ward off the potential death of a loved one (Menzies et al., Reference Menzies, Menzies and Iverach2015; Menzies et al., Reference Menzies, Zuccala, Sharpe and Dar-Nimrod2020a). Rather than providing an expected sense of comfort and safety, secure attachments may represent yet another worry for individuals with OCD. Put simply, the more invested in an attachment the individual is, the more they stand to lose in the event of that person’s death. Qualitative reports from clients with OCD seem to support this idea. In a collection of interviews with clients about death anxiety, one individual stated that he believed his psychological distress was about ‘mortality. It’s somehow linked to my mother’s loss. Somehow it’s all about loss’ (Menzies and Menzies, (Reference Menzies and Menzies2019; p. 128). Similarly, another patient with OCD recalled the death of a family member when he was 10 years old, which left him crying in the bathroom: ‘I don’t remember why. I think it was just because … the idea of losing someone … I guess it’s the idea of anyone can lose someone’ (Menzies and Menzies, 2019; p. 163). It is possible that the measures used in the study failed to sufficiently capture the concept of ‘loss of secure attachments’ and its potential impact on levels of death anxiety. These qualitative data are further bolstered by the empirical finding that the fear of the death of others is positively correlated with various symptom domains of OCD, including compulsive checking, harm obsessions, indecisiveness and ‘just right’ experiences (Menzies et al., Reference Menzies, Zuccala, Sharpe and Dar-Nimrod2020a). In fact, fears of loved ones’ deaths demonstrated a greater association with overall OCD severity than fears of one’s own death, further highlighting the additional worries that close relationships may bring to individuals with OCD.
One final consideration to note is that attachment insecurity in the current sample was higher than community norms (Fairchild and Finney, Reference Fairchild and Finney2006). Research exploring the relationship between OCD and attachment is limited. However, some evidence does suggest that patients with OCD report higher fearful attachment than non-clinical populations, with authors hypothesising that early experiences in families with high expressed emotion and hostility result in poor emotion regulation and self-concept, and an inability to rely on internal representations of secure attachment relationships (Doron et al., Reference Doron, Moulding, Nedeljkovic, Kyrios, Mikulincer and Sar-El2012; Tibi et al., Reference Tibi, van Oppen, van Balkom, Eikelenboom, Emmelkamp and Anholt2019). Future studies would consequently benefit from obtaining more relevant and detailed information about patients’ attachment histories and familial relationships in order to better understand this potentially moderating factor.
It is important to consider the limitations of the current study. First, the correlational nature of the current study limits the ability to draw causal inferences. For example, it is possible that more severe OCD leads to heightened fears of death, rather than the reverse causal direction. However, these results (e.g. significant correlations between OCD severity and death anxiety) are at least consistent with experimental findings demonstrating the causal role of death anxiety in at least one subtype of OCD (Menzies and Dar-Nimrod, Reference Menzies and Dar-Nimrod2017). Furthermore, the finding that the relationship remained significant after controlling for a likely potential confound (i.e. neuroticism) goes some way in ensuring that an additional variable is not explaining these relationships.
Second, data for this study were collected during the global COVID-19 pandemic. Hence participants were potentially primed with death reminders on a daily basis. Numerous mortality salience studies have shown that even brief death primes drive individuals to engage in behaviours that increase a sense of cultural belonging, boost self-esteem and seek proximity to a loved one (Florian et al., Reference Florian, Mikulincer and Hirschberger2002; Mikulincer, Reference Mikulincer2019). In one of the few studies to examine long-term exposure to mortality cues, Fernandez et al. (Reference Fernandez, Castano and Singh2010) found that people who work nearby the crematory grounds at Varanasi, India (i.e. individuals with daily death exposure) demonstrated chronically high levels of cultural worldview defence, compared with individuals who work away from the crematory grounds. They concluded that people who are confronted with regular exposure to death experience chronically activated defence mechanisms. It is therefore possible that the current pandemic has led to surges in attempts to activate the buffers proposed by TMT (see further, Menzies and Menzies, Reference Menzies and Menzies2020), which include attachment security. Notably, whilst the pandemic has increased the salience of mortality, it has also been argued to simultaneously disrupt usual defences such as seeking attachments, due to the necessity of lockdowns and social distancing (Menzies et al., Reference Menzies, Neimeyer and Menzies2020b). Furthermore, the fact that the contamination subtype was the most common OCD presentation in the current study also raises questions surrounding the impact of COVID on the present findings, given the obvious relevance of the virus to this particular subtype. Therefore, the pandemic may have had untold effects on participants’ anxiety levels, and on the effective use of anxiety-buffering strategies in the current study.
Lastly, the small sample size is a limitation of the current study. It is possible that the failure to find support for the second hypothesis is due to the study being underpowered to detect a small moderation effect. The sample size also precluded any analyses regarding specific OCD subtypes. For example, it is possible that attachment styles may moderate the relationship between death anxiety and OCD severity among subtypes which specifically involve worries about the death of others (e.g. compulsive checking). Future research may benefit from exploring this relationship within individual subtypes of OCD.
Having acknowledged the limitations of the present study, the strengths should also be noted. The current study is the first to examine whether attachment style moderates the relationship between death anxiety and disorder severity in OCD. Furthermore, it has improved on previous studies (e.g. Menzies et al., Reference Menzies, Sharpe and Dar-Nimrod2019) which relied on a single item measure to explore the moderating role of attachment in psychopathology. The use of a thorough and robust measure of attachment styles has enabled a more confident conclusion that attachment is an insufficient buffer among treatment-seeking individuals diagnosed with OCD. Similarly, it has replicated previous findings regarding the relationship between fears of death and psychopathology, using a different measure of death anxiety than that used in a previous study of OCD (Menzies and Dar-Nimrod, Reference Menzies and Dar-Nimrod2017). Lastly, the present study utilised a clinical sample of treatment-seeking, diagnosed individuals. This is particularly noteworthy given previous criticisms of the death anxiety literature for its over-reliance in convenience samples, limiting the generalisability of findings (Zuccala et al., Reference Zuccala, Menzies, Hunt and Abbott2019).
Conclusion
The present findings, whilst correlational, are consistent with experimental findings that suggest the central role of death anxiety in OCD. Based on this mounting evidence, the current clinical recommendations include directly targeting death anxiety using evidence-based approaches, such as exposure therapy (Menzies et al., Reference Menzies, Zuccala, Sharpe and Dar-Nimrod2018; Menzies, Reference Menzies, Menzies, Menzies and Iverach2018b). Current treatment approaches for OCD typically focus on disproving the client’s estimates of threat (e.g. the probability of contracting an illness), rather than directly targeting the underlying cause (i.e. the fear of death; Menzies et al., Reference Menzies, Menzies and Iverach2015). However, by failing to target death anxiety, such treatments may contribute to the ‘revolving door’ of mental health (Iverach et al., Reference Iverach, Menzies and Menzies2014; p. 590), in which an individual may receive effective treatment for one condition, only to later return to treatment later in life with a different disorder, given that the underlying cause has not been resolved. Further research is needed to examine the proposal that specifically addressing death anxiety using CBT may alleviate OCD symptoms, and reduce the likelihood of future disorders (Iverach et al., Reference Iverach, Menzies and Menzies2014).
The current evidence suggests that attachment, while serving as an effective buffer against death anxiety in non-clinical samples, may be insufficient for individuals with OCD. Only one other study has explored the moderating effect of attachment between death anxiety and mental health concerns, and it used a brief and overly simplistic measure of attachment (Menzies et al., Reference Menzies, Sharpe and Dar-Nimrod2019). As such, there is scope for future studies to further investigate the moderating effect of attachment in a range of mental health disorders. For example, it is possible that attachment effectively protects the individual from death anxiety in conditions which selectively focus on one’s own death (e.g. worries about heart attacks in panic disorder) and involve fewer worries about loved one’s deaths. Future research should seek to clarify whether attachment can successfully buffer against death anxiety in mental health conditions outside of OCD.
Data availability
Data are available on request due to privacy/ethical restrictions.
Acknowledgements
None.
Author contributions
Rachel E. Verin: Conceptualization (equal), Formal analysis (equal), Methodology (equal), Writing-original draft (lead), Writing-review & editing (equal); Rachel E. Menzies: Conceptualization (supporting), Formal analysis (equal), Methodology (equal), Supervision (supporting), Writing-review & editing (equal); Ross G. Menzies: Conceptualization (equal), Formal analysis (equal), Methodology (equal), Project administration (equal), Supervision (lead), Writing-review & editing (equal).
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
The authors declare none.
Ethics statement
This study was approved by the University of Technology Sydney Human Research Ethics Committee.





Comments
No Comments have been published for this article.