1. Introduction
Non-suicidal self-injury (NSSI), defined as the deliberate destruction of bodily tissue without suicidal intent Reference Nock[1], is increasingly recognized as a significant public health concern: lifetime prevalence rates of NSSI have been estimated between 5.5% in adults to 17.2% in adolescents Reference Swannell, Martin, Page, Hasking and St John[2]. Among clinical inpatient samples, as many as 21% of adults Reference Briere and Gil[3] and 30–45% of adolescents [Reference Cloutier, Martin, Kennedy, Nixon and Muehlenkamp4, Reference Darche5] engage in NSSI, with rates of this behavior increasing over the past several decades Reference Hawton, Saunders and O’Connor[6]. Importantly, clear associations have been identified between NSSI and suicidal behavior Reference Hamza, Stewart and Willoughby[7], and in some cases NSSI is an even stronger predictor of suicide attempts than past suicidal behavior [8–Reference Wilkinson, Kelvin, Roberts, Dubicka and Goodyer10]. Thus, it is critical to understand factors that may predispose individuals to engage in NSSI in order to inform treatment and prevention efforts.
One construct that has featured prominently in prior research on NSSI is emotion regulation, broadly defined as implicit or explicit efforts to recognize, understand, and manage one’s emotions [11–Reference Thompson14]. Theoretical and empirical work has identified self-injurious behavior, including NSSI, as both a consequence of poor emotion regulation Reference Perez, Venta, Garnaat and Sharp[15] and a maladaptive strategy for regulating affect Reference Nock[1]. However, despite the size and scope of this literature, no synthesis of empirical findings currently exists. Furthermore, the construct of emotion (dys)regulation lacks conceptual clarity [Reference Aldao, Gee, De Los Reyes and Seager16, Reference Thompson14]. This is illustrated by the wide range of self-report measures used to assess emotion regulation, each capturing different aspects of this broad construct [Reference Aldao, Nolen-Hoeksema and Schweizer17, Reference Compas, Jaser, Bettis, Watson, Gruhn and Dunbar18]. As research examining NSSI begins to incorporate a growing array of novel measures and methodologies, it is necessary to synthesize prior research on the multidimensional nature of emotion regulation, as documented by self-report measures.
1.1. Overview of emotion dysregulation: models and measures
There have been many theoretical models proposed that characterize emotion regulation. Importantly, the regulation of emotions involves many neurobiological and physiological processes, such as emotion recognition, emotion reactivity, and cognitive control [19–Reference Phillips, Ladouceur and Drevets21]. For the purposes of the current review, we focus on abilities and strategies that are reflective of emotion dysregulation. Below we discuss theoretical models of emotion regulation commonly used in the literature and their associated measures.
According to the process model of emotion regulation Reference Gross[22], emotions are generated and expressed over a multi-stage process, with various regulation strategies available at each stage. This model specifies that regulation must involve awareness of one’s emotion, goals to regulate those emotions, (e.g., by increasing or decreasing their intensity), and the effective implementation of adaptive strategies to reach emotion-regulation goal Reference Gross, Sheppes and Urry[23]. Strategies are differentiated by whether they occur before (antecedent-focused) or after (response-focused) an emotional response, and may be implicit, i.e., automatic, or explicit, i.e., effortful Reference Gross[24]. In the extended process model of emotion regulation, Gross and colleagues highlight three points at which difficulties in the regulation process may occur: identification, selection of a strategy, and implementation or modification of a strategy Reference Gross[19]. As such, emotion dysregulation may be due to a failure to engage in any regulation, difficulties enacting a strategy successfully, or by using regulation strategies that are poorly matched to a situation. To date, the measurement of this construct has largely focused on self-report methods that assess strategy selection – what strategies do individuals rely on to regulate emotional responses.
Drawing on this framework, the Emotion Regulation Questionnaire (ERQ) Reference Gross and John[25] captures two specific strategies of emotion regulation: reappraisal, an antecedent-focused cognitive change strategy aimed to change the way one thinks about a situation, and expressive suppression, a response-focused strategy aimed to inhibit emotional expression, with the former generally deemed more effective than the latter Reference Gross[24]. Another frequently used measure, the Cognitive Emotion Regulation Questionnaire (CERQ) Reference Garnefski, Kraaij and Spinhoven[26] also emphasizes conscious, cognitive regulation strategies. A number of adaptive strategies are identified for managing the intake of emotional information, including cognitive strategies such as positive reappraisal and acceptance, and maladaptive strategies include rumination, self-blame, blaming others, and catastrophizing Reference Garnefski and Kraaij[27].
In contrast to the measures noted above, other models have emphasized the need for awareness or understanding of one’s emotions and modulation of emotional reactivity and intensity [Reference Gratz and Roemer11], [Reference Mennin, Holaway, Fresco, Moore and Heimberg13]]. Mapping onto the process model of emotion regulation, this framework emphasizes the identification of one’s own emotional reactions as a critical step in successful regulation, as well as the selection of appropriate strategies to regulate these responses. This broad, multidimensional conceptualization of emotion regulation resulted in the development of the Difficulties in Emotion Regulation Scale (DERS) Reference Gratz and Roemer[11]. The DERS, one of the most widely used measures of emotion regulation, draws on six theoretical facets of regulation: awareness of one’s emotions; understanding of how one is feeling (clarity); flexible modulation of emotions in order to engage in goal-directed behaviors; control over impulsive behaviors in the face of negative emotion; acceptance of emotional responses; and access to emotion regulation strategies. The absence of any of these abilities signifies emotion dysregulation Reference Gratz and Roemer[11].
As noted above, the constructs of emotion regulation and dysregulation are broad and multidimensional. The literature has largely examined the extent to which broad domains and/or specific strategies are adaptive or maladaptive. Thus, the current review aims to synthesize this literature by examining both overall dysregulation and deficits within specific domains of emotion regulation with regard to NSSI. As there has been no single, unitfying conceptual model for emotion (dys)regulation in the literature to date, the current meta-analysis examines subscales from each of these three measures in the analyses below.
1.2. Emotion dysregulation and NSSI
As emotion dysregulation becomes central to our understanding of psychopathology more broadly [Reference Aldao, Gee, De Los Reyes and Seager16, Reference Aldao, Nolen-Hoeksema and Schweizer17], it has achieved greater recognition as a potential risk factor for engagement in NSSI. Various models of NSSI characterize the behavior as a maladaptive response to strong negative affect, with theoretical and empirical work suggesting that NSSI may serve an affective regulation function [Reference Brown, Comtois and Linehan28–Reference Linehan31], stemming from poor emotion regulation skills (i.e., emotion dysregulation). For example, the argument that NSSI serves the function of avoidance or escape from unwanted emotional arousal is set forth in the experiential avoidance model of deliberate self-harm Reference Klonsky[30]. This need for avoidance is exacerbated by individuals’ emotion regulation skill deficits, poor distress tolerance, and difficulty modulating negative emotions when aroused. Similarly, a direct link is proposed between emotion dysregulation and dysregulated behaviors (such as NSSI) among individuals with borderline personality disorder in the emotional cascade model Reference Selby and Joiner[32]. This model suggests that rumination intensifies emotional experiences, leading individuals to engage in dysregulated behaviors as a temporary distraction from negative emotion. Most contemporary models of NSSI now recognize the potential contribution of emotion regulation deficits, as well as individual factors that may exacerbate those deficits (e.g., high levels of aversive emotions and cognitions, acute negative affective states [Reference Nock1, Reference Klonsky30].
Despite widespread recognition that emotion dysregulation may contribute risk for NSSI, no systematic review of empirical studies has been conducted. A recent meta-analysis of longitudinal risk factors for NSSI found affect dysregulation to be a significant, but weak, predictor of NSSI Reference Fox, Franklin, Ribeiro, Kleiman, Bentley and Nock[33]. In this meta-analysis, however, affect dysregulation was broadly defined to include emotional suppression, emotional reactivity, and negative affect. In addition to the need to distinguish the role of emotion regulation as separate from emotional reactivity and other aspects of affective experiences, questions remain regarding which, if any, specific dimensions of emotion dysregulation may contribute higher levels of risk. Several studies offer preliminary insights into the importance of considering discrete facets of emotion regulation in understanding risk for NSSI. For example, a recent study of psychiatrically hospitalized adolescents found higher risk for chronic suicidal behavior among those reporting non-acceptance of emotional responses and limited access to emotion regulation strategies, compared to other domains of emotion dysregulation on the DERS Reference Wolff, Davis, Liu, Cha, Cheek and Nestor[34]. A study specifically examining NSSI reached similar conclusions, with limited access to emotion regulation strategies showing unique associations with self-injurious behavior Reference Perez, Venta, Garnaat and Sharp[15]. A synthesis of the empirical literature is warranted to better characterize differential associations between these dimensions of emotion dysregulation and NSSI, as well as to examine potential moderators of these associations. Such findings have the potential to offer valuable, clinically relevant information highlighting aspects of emotion dysregulation that should be targeted in interventions.
We present a systematic meta-analysis to characterize overall associations between self-reported measures of emotion dysregulation and NSSI. In order to clarify the role of the various dimensions of emotion dysregulation, we also examined associations between NSSI and specific dimensions of emotion dysregulation. Finally, based on our comprehensive review, we discuss important gaps in the literature with the view of informing future research in this area.

Fig. 1. PRISMA flow chart of literature search.
2. Methods
2.1. Search strategy and eligibility criteria
To identify relevant studies for inclusion in this review, we conducted a systematic search of the literature in PsycINFO and Medline using the following search string: ("emotion modulation" or "affect modulation" or "affective modulation" or "emotion reactivity" or "emotional reactivity" or "affect reactivity" or "affective reactivity" or "emotion regulation" or "emotion dysregulation" or "affect regulation" or "affect dysregulation" or "affective regulation" or "affective dysregulation" or "affective functioning" or "emotional functioning" or "distress tolerance" or "affective labelling" or "affective labeling" or "affect labelling" or "affect labeling" or "emotion labelling" or "emotion labeling")1 AND (self-injur* or mutilat* or self-cut* or self-harm*). We retained only the search results from: (i) English-language publications and (ii) peer-reviewed journal publications. Using this search strategy generated 674 articles, of which 434 were unique reports. We determined eligibility by reviewing title and abstract; however, in cases where eligibility could not be determined based on title and abstract alone, we also reviewed the full text. Each search result was reviewed by two independent raters for eligibility, with discrepancies resolved by a third rater.
The study inclusion criteria were: (i) any form of emotion (dys)regulation was assessed, distinct from other related constructs (therefore studies assessing related constructs, such as emotional reactivity or emotional processing were not included); (ii) consistent with the definition of NSSI, the measure of NSSI had to specify there was no suicidal intent; (iii) emotion dysregulation had to be measured as distinct from NSSI (e.g., not as a function of NSSI); and (iv) quantitative data were presented on the association between any form of emotion dysregulation and any NSSI. To provide clarity on some data, authors of studies were contacted as necessary.
We excluded 75 reports based on their titles and abstracts because they did not meet the inclusion criteria reviewed above. After this initial screen, we excluded an additional 311 articles as a result of a detailed full-text review. There were 48 publications remaining that satisfied the eligibility criteria (see Fig. 1 for PRISMA flow chart). We excluded studies after full-text review because they: (i) did not adequately measure emotion dysregulation as a distinct construct (n = 110); (ii) did not report any measures of association between emotion dysregulation and NSSI (n = 52); (iii) did not include original quantitative data (n = 50); (iv) did not separate NSSI from suicidal ideation and/or attempts (n = 45); (v) did not otherwise adequately measure NSSI as a distinct construct (n = 44); and (vi) had redundant data with included articles (n = 5); (vii) excluded for other reasons (n = 5). In cases where it could not be independently determined whether two studies contained overlapping samples, the study authors were contacted. In five cases where studies were excluded for having samples that overlapped with those in retained studies, the study that provided the larger sample was retained in every case.
Table 1 Study characteristics.
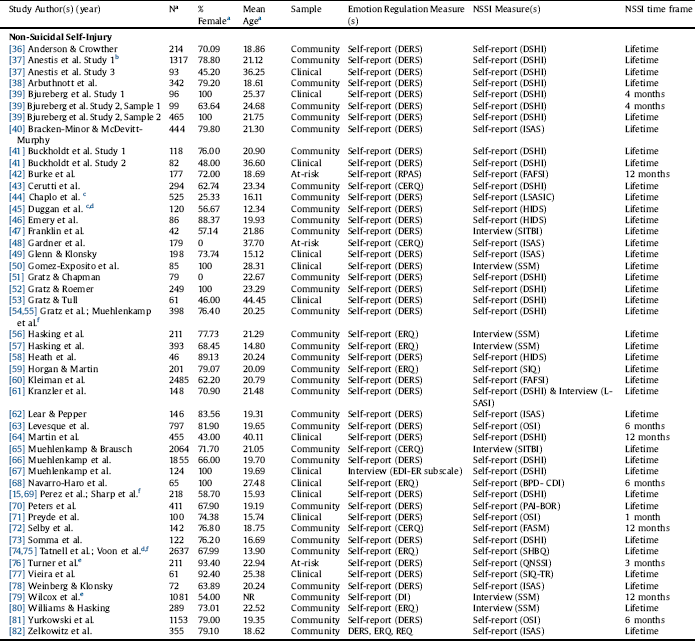
Note: BPD- (CDI) = The Borderline Personality Clinical Data Inventory, CERQ = The Cognitive Emotion Regulation Questionnaire, DERS = The Difficulties in Emotion Regulation Scale, DI = Dysregulation Inventory, DSHI = Deliberate Self-Harm Inventory; EDI-ER subscale = The Eating Disorder Inventory- Third Edition, ERQ = The Emotion Regulation Questionnaire, FAFSI = Form and Function Self-Injury Scale, FASM = Functional Assessment of Self-Mutilation; HIDS = How I deal with stress questionnaire, ISAS = Inventory of Statements About Self-Injury; L-SASI = Lifetime-Suicide Attempts Self-Injury, LSASIC = Lifetime-Suicide Attempt Self-Injury Count, NR = not reported; OSI = Ottawa Self-Injury Inventory, PAI-BOR = Personality Assessment Inventory for Borderline Personality Disorder, QNSSI = The Questionnaire for Nonsuicidal Self-Injury, REQ = RPAS = Responses to Positive Affect Scale, SHBQ = The Self-Harm Behavior Questionnaire, SIQ = Self-Injury Questionnaire, SIQ-TR = The Self-Injury Questionnaire – Treatment Related, SITBI = Self-Injurious Thoughts and Behaviors Interview; SSM = study-specific measure.
a The number, mean age, and % female of participants included in relevant analyses, rather than of the entire study sample, are presented and were incorporated in moderator analyses whenever available.
b This publication included another sample that was not eligible for the current meta-analysis.
c Separate effects were reported by sex.
d These studies employed a longitudinal design but cross-sectional analyses of emotion regulation in relation to NSSI.
e These studies employed longitudinal analyses of emotion regulation in relation to NSSI.
f In these cases, two publications drew on overlapping samples but were retained because each publication featured unique data relevant to the current meta-analysis (e.g., overall emotion dysregulation was analyzed in one and subscales in another). None of the analyses in the current review featured two studies with overlapping samples. Table 2. Meta-analytic results for the Difficulties in Emotion Regulation Scale in relation to non-suicidal self-injury.

Fig. 2. Funnel plot for effect sizes in the meta-analyses. The vertical line indicates the weighted mean effect. Open circles indicate observed effects for actual studies, and closed circles indicate imputed effects for studies believed to be missing due to publication bias. The clear diamond reflects the unadjusted weighted mean effect size, whereas the black diamond reflects the weighted mean effect size after adjusting for publication bias.
2a. Overall emotion regulation and non-suicidal self-injury.
2b. Difficulties in Emotion Regulation – Lack of Emotional Awareness scale and non-suicidal self-injury.
2c. Difficulties in Emotion Regulation – Lack of Emotional Clarity scale and non-suicidal self-injury.
2d. Difficulties in Emotion Regulation – Difficulties Engaging in Goal-Directed Behavior scale and non-suicidal self-injury.
2e. Difficulties in Emotion Regulation – Impulse Control Difficulties scale and non-suicidal self-injury.
2f. Difficulties in Emotion Regulation – Non-acceptance of Emotional Responses scale and non-suicidal self-injury.
2g. Difficulties in Emotion Regulation – Limited Access to Emotion Regulation Strategies scale and non-suicidal self-injury.
2h. Emotion Regulation Questionnaire – Cognitive Reappraisal scale and non-suicidal self-injury.
2i. Emotion Regulation Questionnaire – Expressive Suppression scale and non-suicidal self-injury.
2.2. Data extraction
To identify potential moderators, we extracted data on nine study characteristics. We included four sample characteristics: (i) sample age group (i.e., youth up to age 18) versus adult (including college age samples)); (ii) mean age of sample; (iii) sample clinical status (i.e., clinical/at-risk versus community); and (iv) percentage of female participants in the study sample. Data were also extracted for five study design characteristics: (i) form(s) of emotion dysregulation assessed; (ii) method of assessing emotion dysregulation (i.e., self-report versus task)2 ; (iii) method of assessing NSSI; (iv) time-frame of NSSI assessment (12 months or fewer versus lifetime); and (v) cross-sectional versus longitudinal analysis. Extraction was conducted by one of the investigators and 20.83% of studies were checked for accuracy.
2.3. Data analysis
Based on the inclusion criteria noted above, the included studies utilized one of three emotion dysregulation measures: the DERS, ERQ, or CERQ. The DERS is a 36-item measure with 6 scales Reference Gratz and Roemer[11]: nonacceptance of emotional responses (i.e., “When I’m upset, I become angry with myself for feeling that way”), difficulty engaging in goal-directed behavior (i.e., “When I’m upset, I have difficulty getting work done”), impulse control difficulties (i.e., “I experience my emotions as overwhelming and out of control”), limited access to emotion regulation strategies (i.e., “When I’m upset, I believe there is nothing I can do to make myself feel better”), and lack of emotional clarity (i.e., “I am confused about how I feel”). The CERQ is a 36-item measure that assesses 9 scales of cognitive emotion regulation Reference Garnefski and Kraaij[27]. Of the 9 scales, only studies utilizing two of the scales, rumination/focus on thought (i.e., “I am preoccupied with what I think and feel about what I have experience”) and catastrophizing (i.e., “Thinking that what I experienced is the worst ever”), had enough studies to be included in the meta-analysis. Lastly, the ERQ is a 10-item measure assessing cognitive reappraisal (i.e., “I change the way I’m thinking about the situation”) and emotional suppression (i.e., “I control my emotions by not expressing them”) Reference Gross and John[25].
For the primary index of effect size we report the odds ratio (OR). If ORs were not reported in the original articles, we derived them from available data reported in the study (e.g., means and standard deviations, correlation) whenever it was possible to do so. We calculated all ORs such that values greater than 1.0 indicate a positive association between emotion dysregulation and NSSI. To convert data into ORs and conduct all analyses, we used Comprehensive Meta-Analysis Version 3.3.070 Reference Borenstein, Hedges, Higgins and Rothstein[35] (Biostat, 2014). We calculated the overall weighted effect size by pooling ORs across all relevant studies. For all analyses, we generated random-effects models in preference to fixed-effects models, in order to account for the high expected heterogeneity across studies resulting from differences in samples, measures, and design. We evaluated this heterogeneity across studies using the I2 statistic, which represents the percentage of the variance in an effect estimate that is a product of heterogeneity across studies rather than sampling error (i.e., chance). I2 values of around 25% indicate low heterogeneity, while I2 values of 50% indicate moderate heterogeneity. An I2 value of 75% is an indicator of substantial heterogeneity that is due to real differences in study samples and methodology, which suggests that the observed heterogeneity is over and above what would be expected with random error (Higgins, Thompson, Deeks, & Altman, 2003). When high heterogeneity is observed, random-effects models are preferred over fixed-effects models—random-effects models account for this heterogeneity by incorporating both sampling and study-level errors, with the pooled effect size representing the mean of a distribution of true effect sizes instead of a single true effect size. Conversely, fixed-effects models estimate only within-study variance because they assume that a single true effect size exists across all studies and any variance detected is due strictly to sampling error.
Table 2 Meta-analytic results for the Difficulties in Emotion Regulation Scale in relation to non-suicidal self-injury.

Note: k = number of unique effects; OR = pooled odds ratio; CI = confidence interval.
Findings with high heterogeneity suggest it is necessary to conduct moderator analyses to uncover potential sources of this heterogeneity. Potential moderators were evaluated using random effects analysis. We first assessed each potential moderator separately, and calculated an estimate of the effect size at each level of the moderator. Moderators that reached the threshold of p > 0.05 are reported.
When interpreting the results of meta-analyses, a common concern is the possible influence of publication bias. That is, because studies with small effect sizes or non-significant findings are less likely to be published, their findings may be left out of meta-analyses. This can potentially lead to inflation of estimates of the overall effect size. We evaluated potential publication bias by calculating the following publication bias indices: Duval and Tweedie’s trim-and-fill analysis (Duval & Tweedie, 2000) and Egger’s regression intercept(Egger, Davey Smith, Schneider, & Minder, 1997). Duval and Tweedie’s trim-and-fill analysis generates an estimate of the number of missing studies based on asymmetry in a funnel plot of the standard error of each study in a meta-analysis (based on the study’s sample size) compared to the study’s effect size. This analysis also yields an effect size estimate and confidence interval, adjusting for these missing studies. We note that this procedure assumes effect sizes to be homogeneous; therefore, if significant heterogeneity exists, results should be interpreted with caution. Egger’s regression intercept derives potential publication bias indices by using a linear regression approach that assesses study effect sizes compared to their standard error.
3. Results
The present meta-analysis included 48 publications based on 49 unique samples3 assessing the relation between emotion dysregulation and NSSI (see Table 1). We first present results for overall emotion dysregulation and moderator analyses for overall emotion dysregulation, followed by analyses for the association between NSSI and specific dimensions of emotion dysregulation as reflected by the DERS, ERQ, and CERQ, respectively.
3.1. Overall emotion dysregulation and NSSI
A total of 41 unique effects were identified for overall emotion dysregulation in relation to NSSI, with a positive weighted effect size observed (pooled OR = 3.03 [95% CI = 2.56–3.59]). Heterogeneity was high, indicating that moderator analyses were appropriate. In terms of potential publication bias, Egger’s regression test indicated that significant publication bias was present (intercept = 1.89 [95% CI =.54–3.24], t = 2.82, p <.01). Additionally, the funnel plot of effect sizes was notably asymmetrical (see Fig. 2a). When the trim-and-fill method was used to correct parameter estimates for potential publication bias, the adjusted weighted OR was reduced to 2.40 (95% CI = 2.01–2.86) suggesting that there is a significant relation between emotion dysregulation and NSSI.
3.2. Moderator analyses
Most studies featured adult samples or a combination of adults and adolescents, with 10 studies featuring 8 purely adolescent samples. The majority of studies had samples that were predominantly female, with only 7 studies including mostly male samples. It should be noted that none of the identified studies included task data and all studies included in this review relied on self-report measures of emotion regulation. Consequently, this study design feature was not included in moderator analyses. Additionally, too few studies featured interview-based measures of NSSI or longitudinal analyses of emotion dysregulation in relation to NSSI for consideration in moderator analyses (i.e., < 3). Therefore, age, sex, sample type, and timing of NSSI were tested as moderators.
Age was not a significant moderator of the strength of the association between overall emotion dysregulation and NSSI, regardless of whether age was treated categorically with comparisons made between youth and adults (p =.09) or analyzed as a continuous variable (b =.02, p =.25). Similarly, we did not find the percentage of female participants in each study (b <.01. p =.33), or sample type (i.e., clinical/at-risk versus community; p =.16) were significant moderators. However, time frame of NSSI assessment emerged as a significant moderator (p =.04), with a larger effect size in the relation between overall emotion dysregulation and NSSI observed for lifetime NSSI (OR = 3.21 [95% CI = 2.63–3.91]) than for past-year NSSI (OR = 2.32 [95% CI = 1.84–2.92]).
We also conducted an analysis directly comparing individuals with recent NSSI (defined as engaging in this behavior in the past 12 months) with individuals with a past history of NSSI (defined as having engaged in this behavior, but not in the past 12 months), to ascertain whether recency of NSSI was associated with emotion dysregulation. Across the four studies that allowed for this analysis, a small-to-medium effect was observed, with recent NSSI associated with greater emotion dysregulation, relative to past NSSI (OR = 1.68 [95% CI = 1.03–2.73]).
3.3. DERS subscales
Specific dimensions of emotion dysregulation as reflected by the DERS subscales were also examined in relation to NSSI (see Table 2). All domains of emotion dysregulation were positively associated with NSSI, with pooled OR’s ranging from 1.53 (95% CI = 1.25–1.88) for the lack of emotional awareness subscale to 3.89 (85% CI = 2.44–6.23) for the limited access to emotion regulation strategies subscale. Regarding potential publication bias for specific DERS subscales, Egger’s regression test indicated significant publication bias in the case of the non-acceptance of emotional responses scale, the difficulties engaging in goal-directed behavior scale, and impulse control difficulties scale. Funnel plots of the effect sizes for DERS subscales (see Figs. 2b to 2 g) were fairly asymmetrical in the case of the non-acceptance of emotional responses scale and the difficulties engaging in goal-directed behavior scale, suggesting the presence of publication bias, but not in the case of the impulse control difficulties scale. Additionally, the funnel plot for the limited access to emotion regulation strategies scale appeared asymmetrical. Although the trim-and-fill method produced a reduction in estimated effect sizes, significant effects remained for all DERS subscales, with adjusted OR’s ranging from 1.56 (95% CI = 1.27–1.91) for the lack of emotional awareness scale to 2.70 (95% CI = 2.05–3.56) for the impulse control difficulties scale. These results are summarized in Table 1.
3.4. ERQ subscales
Seven studies were available for the ERQ subscales in relation to NSSI. Cognitive reappraisal difficulties (pooled OR = 1.53 [95% CI = 1.29–1.83]) and expressive suppression (pooled OR = 1.55 [95% CI = 1.21–1.99]) were both positively associated with NSSI. There was no evidence of publication bias based on Egger’s regression test for either ERQ subscale (for cognitive reappraisal difficulties, intercept = 2.44 [95% CI = -.71 – 5.59], t = 1.99, p =.10; for expressive suppression, intercept = -.54 [95% CI = -6.72 – 5.64, t =.22, p =.83). Asymmetry was present in the funnel plot for cognitive reappraisal difficulties but not for expressive suppression (Figs. 2h and 2i). Similarly, the effect size was reduced but remained significant for cognitive reappraisal difficulties (adjusted OR = 1.40 [95% CI = 1.17–1.67]) but remained unchanged for expressive suppression.
3.5. CERQ subscales
A sufficient number of unique effects to calculate pooled effect sizes was available only for the subscales of the CERQ corresponding to the tendency to ruminate and to catastrophize as forms of emotion dysregulation (ks = 3). Small-to-medium pooled effects were observed in both cases (ORCERQ Rumination = 1.83 [95% CI = 1.30–2.58], p =.001; ORCERQ Catastrophize = 1.79 [95% CI = 1.34–2.40], p <.001).
4. Discussion
Although emotion dysregulation is often cited as a primary reason that individuals engage in NSSI, previous reviews have not synthesized this literature. The current meta-analytic review aimed to characterize overall associations between emotion dysregulation and NSSI, and to examine patterns of association between NSSI and specific dimensions of emotion dysregulation. A total of 48 studies were identified, demonstrating the substantial attention devoted to this topic over the past several years. Consistent with prevailing theories of NSSI, results demonstrated a significant association between these constructs in the predicted direction, such that greater emotion dysregulation was associated with a greater likelihood to engage in NSSI. The overall pooled odds ratio was 2.40, a medium effect size, with the strength of associations varying according to the dimension of emotion dysregulation analyzed. Results of the current meta-analysis have critical implications for the treatment and prevention of NSSI in both adolescents and adults.
Findings revealed a robust association between NSSI and emotion dysregulation across numerous samples, with no differences emerging based on sample age, sex, or sample type (i.e., clinical versus community). In prior meta-analyses of both coping and emotion regulation, age has been an inconsistent moderator of effects [Reference Aldao, Nolen-Hoeksema and Schweizer17, Reference Compas, Jaser, Bettis, Watson, Gruhn and Dunbar18], and in a recent meta-analysis examining associations among emotion regulation and anxiety and depressive symptoms, age was not a moderator of any effects Reference Schäfer, Naumann, Holmes, Tuschen-Caffier and Samson[83]. This may be due in part to problems in measurement approaches that do not account for developmental differences and evaluation of emotion (dys)regulation across various ages Reference Compas, Jaser, Bettis, Watson, Gruhn and Dunbar[18]. Further, a small number of studies in the current meta-analysis reported effects for adolescents (as opposed to adults or combined), which may have limited our power to detect a significant moderating effect of age. Of all moderators assessed, only time frame of NSSI assessment emerged as significant, with a larger effect size observed for lifetime NSSI than for past-year NSSI. This finding may not be surprising given that measures of lifetime NSSI encompass a larger time frame, but is reflective of important measurement differences across studies of NSSI that may significantly impact results.
Across measures, some dimensions of emotion dysregulation were more strongly related to NSSI than others. The DERS subscale of limited access to emotion regulation strategies showed the greatest association with NSSI, with an effect size in the medium-to-large range. This finding is consistent with other studies that suggest the availability of multiple regulation strategies is a particularly important facet to consider in the assessment and treatment of NSSI and related symptoms [Reference Perez, Venta, Garnaat and Sharp15, Reference Wolff, Davis, Liu, Cha, Cheek and Nestor34]. Cognitive aspects of emotion dysregulation (i.e., poor reappraisal, catastrophizing, rumination, and suppression) showed weaker associations with NSSI, with odds ratios in the small-to-medium range. Such findings suggest that treatment efforts may benefit from a focus on helping patients to learn and access specific emotion regulation strategies considered more adaptive, such as reappraisal, distraction, or mindfulness, in preventing NSSI. However, it should be noted that considerably more studies included the measurement of emotion dyregulation using the DERS compared to the CERQ (which includes rumination and catastrophizing), pointing to the need for further research to examine these strategies in greater depth.
Our findings complement those of a previous meta-analysis examining risk factors for NSSI Reference Fox, Franklin, Ribeiro, Kleiman, Bentley and Nock[33]. Although we did not examine specific diagnoses in this review, findings are consistent with prior analyses of the link between emotion regulation strategies and psychopathology, including depression, anxiety, eating disorders, and substance use Reference Aldao, Nolen-Hoeksema and Schweizer[17], as well as broader internalizing and externalizing problems Reference Compas, Jaser, Bettis, Watson, Gruhn and Dunbar[18]. Compared to Fox and colleagues Reference Fox, Franklin, Ribeiro, Kleiman, Bentley and Nock[33], our findings suggest a stronger association between emotion dysregulation and NSSI, which may reflect our inclusion of both cross-sectional and longitudinal studies, and/or our narrower definition of emotion dysregulation. In particular, the current meta-analysis excludes measures of emotional reactivity. Prior work suggests that emotion dysregulation may uniquely predict NSSI over and above emotional reactivity, while the reverse may not be true Reference Zelkowitz, Cole, Han and Tomarken[82]. This suggests that emotion dysregulation may serve as a unique correlate of NSSI, as well as a particularly fruitful treatment target. In addition, given the complexity of the construct of emotion dysregulation and guided by the extended process model, research that examines each component of the emotion regulation process, from identification to implementation, is needed. While the current review demonstrates overall associations between NSSI and emotion dysregulation, further research is needed to better understand how and at what point the emotion regulation process contributes to greater likelihood of engaging in self-harm.
Meta-analyses by Aldao et al. and Compas et al. reveal significant associations between emotion (dys)regulation and psychopathology [Reference Aldao, Nolen-Hoeksema and Schweizer17, Reference Compas, Jaser, Bettis, Watson, Gruhn and Dunbar18]. These meta-analyses find significant associations between psychopathology and cognitive reappraisal and secondary control coping (which includes cognitive reappraisal). Our findings expand on these meta-analyses, suggesting a small association between cognitive reappraisal and NSSI. However, it is interesting to note that although the current results reveal a medium-to-large effect size for the association between non-acceptance of emotional responses and NSSI, Aldao and colleagues found no association between non-acceptance and psychopathology. As they pointed out, these two strategies (reappraisal and acceptance of emotional response) are often important components of treatments that address emotion dysregulation, such as cognitive behavioral therapy and dialectical behavior therapy. This suggests that facilitating acceptance of emotional responses may be an advantageous treatment target that is specific to decreasing NSSI behavior. It is possible that our finding of a stronger relation between non-acceptance and NSSI differs from Aldao et al. because NSSI is a transdiagnostic behavior and is not specific to one diagnostic category Reference Aldao, Nolen-Hoeksema and Schweizer[17]. NSSI may be a coping behavior (serving to distract or avoid) that results from non-acceptance of emotional responses [Reference García-Nieto, Carballo, de Neira Hernando, de León-Martinez and Baca-García84, Reference Lloyd-Richardson, Perrine, Dierker and Kelley85]; however, more research is needed to further clarify these discrepant findings.
Our results demonstrate evidence of links between well-characterized emotion regulation strategies that protect against and increase risk for psychopathology, and NSSI. Although NSSI represents a transdiagnostic type of psychopathology manifested in behavior, it shares features of other types of psychopathology, and may benefit from similar interventions. At the same time, NSSI may pose unique challenges, in that the function of this behavior may actually be to regulate emotion. This requires successful treatments to not only facilitate the use of adaptive emotion regulation strategies, but also to provide alternate behaviors in which to engage under circumstances of heightened emotion or reactivity. Aldao et al. (2010) suggest that the strategies of rumination, avoidance, and suppression are risk factors for psychopathology, whereas reappraisal, problem-solving, and acceptance may serve as protective factors Reference Aldao, Nolen-Hoeksema and Schweizer[17]. Our results similarly show that NSSI is positively associated with rumination and suppression (risk factors), as well as with reappraisal difficulties and non-acceptance (inverted protective factors). Avoidance and problem-solving were not included as subscales in the current meta-analysis. However, it is possible that the strategy we found with the strongest association to NSSI—lack of access to emotion regulation strategies--may represent one facet of a broader problem-solving construct. That is, part of problem-solving is generating possible solutions and without the ability to identify other emotion regulation strategies, an individual may rely on NSSI to cope with stressors or intense emotions. Indeed, prior work highlights that NSSI may serve as both a response to negative affect and a strategy for regulating it Reference Klonsky[30].
It should also be noted that while the current meta-analysis helps to advance our understanding of the relationship between emotion dysregulation and NSSI, the reasons for this association remain unknown. Some theories have posited that NSSI serves as a means of regulating emotions by avoiding or distracting from emotional experiences [29,32]. Others have suggested that because of the high degree of overlap between physical and emotional pain, the physical pain relief associated with NSSI leads to emotional pain relief Reference Franklin, Puzia, Lee, Lee, Hanna and Spring[47]. Our findings, however, reflect associations between overall (i.e., trait-level) emotion dysregulation and NSSI, and cannot disentangle state-specific experiences of dysregulation that may prompt episodes of NSSI. These potential mechanisms of affect regulation in individuals engaging in NSSI, and the specific time frames in which they occur, are important to identify as they may provide future targets for treatment interventions. Understanding these mechanisms is an important step toward developing more effective treatments for NSSI.
4.1. Limitations and future directions
The current meta-analysis reveals a number of limitations with the current literature and highlights important future directions. First, the included studies relied exclusively on self-report measures of emotion dysregulation and NSSI, which is inherently limited in its ability to provide objective and corroborated data Reference Folkman and Moskowitz[86]. Although the current study initially aimed to include psychophysiological studies, there was an insufficient number identified in the current review of the literature that met our inclusion criteria for conducting a meta-analysis. Researchers have begun to rely on objective, psychophysiological measures believed to index emotion regulatory capacity—such as respiratory sinus arrhythmia [87,88] and cardiac vagal tone measured through heart rate variability Reference Laborde, Mosley and Thayer[89]. The reliance on self-report of emotion dysregulation limits findings, especially because experimental and psychophysiological studies have often failed to show the same results as self-report studies [90–Reference Kaess, Hille, Parzer, Maser-Gluth, Resch and Brunner92]. While incorporating constructs related to emotion dysregulation (e.g., reactivity) was outside the scope of the current meta-analytic review, exploring the role of emotional reactivity and regulatory capacity, as measured by psychophysiological measures, is an important continued area of future research in understanding mechanisms involved in NSSI behaviors. To date, studies have demonstrated associations between parasympathetic responses, including RSA, as a proxy for emotion regulation and psychopathology, including NSSI [93–Reference Yaroslavsky, Rottenberg, Bylsma, Jennings, George and Baji95]. In addition, the regulation of emotion relies on a broad range of neurobiological mechanisms that assist in the identification of emotion, selection and implementation of emotion regulation strategies, which have been studied widely in adolescents and adults [20,96,97]. The integration of self-report, neurobiological, and psychophysiological measurement in understanding regulatory processes and their association with NSSI across development is a critical area of future research.
Furthermore, many studies failed to assess the intention of self-harm and were therefore excluded from analyses due to their inability to discern if these were suicidal or non-suicidal acts. Imprecision of measurement and/or language may yield inconsistent results and produce conflictual conclusions in the literature, motivating our decision to exclude many studies at the risk of omitting potentially meaningful data. Although various questionnaires were used to assess NSSI and continuous data was used whenever possible, nearly half of the studies reviewed relied on binary coding (e.g., yes/no NSSI) and did not account for factors such as frequency and severity of NSSI. The use of more nuanced measures of NSSI may yield more detailed information about this construct and its relationship to emotion dysregulation. In addition, it is possible that distinct subdomains of NSSI show differential associations with emotion dysregulation. Future research should empirically examine the strength of associations between subdomains of both NSSI and emotion dysregulation.
Most of the included studies relied on cross-sectional assessment of variables. While these data offer an interesting “snap shot” of emotion dysregulation and NSSI, longitudinal studies of these phenomena will offer insight into the persistence, and co-evolution of these processes overtime. Furthermore, longitudinal methodology is necessary to determine true risk factors for NSSI and elucidate the causal relationship between variables of interest Reference Kraemer, Kazdin, Offord, Kessler, Jensen and Kupfer[98]. Additionally, prospective studies, especially those including ecological momentary assessment methodology, could offer more accurate periodic or “real-time” reports of behavior, rather than relying on retrospective reports of emotionally laden experiences which may be influenced by recall biases [99,100]. Finally, future studies should aim to include a diverse range of subjects across demographic factors such as race/ethnicity, sex and gender, age, and psychiatric diagnoses. Although the current findings revealed no difference in associations between emotion dysregulation and NSSI based on age or sex, the majority of samples were primarily or exclusively female, limiting any definitive conclusions. In addition, sample type (clinical versus community) did not affect associations between emotion dysregulation and NSSI; however, specific diagnostic features (i.e., symptoms, diagnoses) should be considered in future work.
5. Conclusion
The current meta-analysis synthesizes over a decade of empirical research examining associations between emotion dysregulation and NSSI. Findings provide support for the notion that greater emotion dysregulation is associated with higher likelihood of engagement in NSSI among individuals across settings, regardless of age or sex. Furthermore, findings reveal facets of emotion dysregulation, such as limited access to emotion regulation strategies, may have unique implications for NSSI risk. NSSI is highly prevalent within clinical samples and represents a critical risk factor for suicide attempts. This meta-analysis highlights the importance of better understanding emotion dysregulation as a treatment target for preventing NSSI.
Contributors
All authors made substantial contributions to this work. All authors participated in the conception and refinement of the manuscript objectives, literature review, and manuscript writing and editing. Dr. Liu conducted the systematic literature search and all statistical analyses.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest statement
The authors have no real or potential conflicts of interest to declare.
Acknowledgements
The authors would like to thank all individuals who replied to inquires regarding previously published findings. The authors are grateful for support from the National Institute of Mental Health (T32MH019927; T32MH078788) and American Foundation for Suicide Prevention (PDF-010517). The content is solely the responsibility of the authors and does not necessarily reflect the official views of the National Institutes of Health or AFSP.







Comments
No Comments have been published for this article.