Introduction
The life expectancy of Aboriginal and Torres Strait Islander (hereafter, respectfully, Indigenous) peoples is improving in Australia, resulting in growing numbers of elders (AIHW, 2015). While the total Indigenous population is projected to increase by 59% between 2011 and 2031, numbers of older Indigenous peoples (≥65 years) are projected to grow by 200% (Biddle, Reference Biddle2013). In mid-2018, it was estimated that there were already more than 123 000 Indigenous peoples aged 50 years or over (AIHW, 2018a) and recent data show that there are 120 aged care organisations across Australia that provide home care to a client base comprising at least 50% Indigenous peoples (AIHW, 2020).
Indigenous elders ‘play a vital role in sustaining strong cultural practices and traditions within their communities with important roles and responsibilities such as passing on knowledge, languages and customs, participating in decision-making ceremonies and looking after country’ (Commonwealth of Australia, 2013: 38). This is despite burdensome health and social challenges: compared with non-Indigenous Australians, older Indigenous peoples experience greater comorbidity, disability, racism, financial insecurity, homelessness and challenges to health and social services’ access (AIHW, 2019). An estimated 13 800 (14%) of older Indigenous peoples (≥50 years) in 2014–15 were part of the ‘Stolen Generations’ (AIHW, 2018b) who, as children in the 20th century, were forcibly removed from their families under successive government policies (Human Rights and Equal Opportunity Commission, 1997). Compared with Indigenous elders who were not removed, members of the Stolen Generations experience double the rates of poor health and social outcomes (AIHW, 2018b).
Clearly, Indigenous-led, culturally safe aged care services are desperately needed to meet the unique needs of older Indigenous peoples and promote and safeguard elder well-being. Aboriginal and Torres Strait Islander elders have reported feeling unwelcome in mainstream organisations where non-Indigenous people have little understanding or respect for their culture (Ranzijn et al., Reference Ranzijn2010). Experiences of unfair treatment (e.g. racist comments, being ignored or served last when accessing services) is reported by an alarming 31% of older (≥45 years) Indigenous peoples in Australia, and 15% of these report avoiding situations, such as health and government services, as a result (Temple et al., Reference Temple, Kelaher and Paradies2019). Indigenous elders in Canada similarly report racism and discrimination as barriers to service access (Schill et al., Reference Schill, Terbasket, Thurston, Kurtz, Page, McLean, Jim and Oelke2019). Of paramount importance, then, is the availability of culturally safe aged care and primary health care services delivered by trustworthy providers. International evidence including studies from the United States, Canada, Alaska, Australia and Brazil demonstrate that primary health care and aged care services promote the well-being of older First Nations’ peoples through culturally safe care, maintaining Indigenous identity and promoting independence (Davy et al., Reference Davy, Kite, Aitken, Dodd, Rigney, Hayes and Van Emden2016).
Over the last decade, the Australian aged care system has undergone extensive scrutiny and reform in response to sector-wide challenges identified in the report ‘Caring for Older Australians’ (Productivity Commission, 2011). The 2013 Living Longer Living Better reforms package provided $3.7 billion of funding (Department of Health, 2012) and an Aged Care Roadmap detailed short, medium and long term plans for a more equitable and consumer-led aged care sector (Aged Care Sector Committee, 2016). The recent Royal Commission into Aged Care Quality and Safety identified widespread neglect across the aged care system. For Indigenous peoples, it recommended: ‘integrating aged care with other services, such as primary health, mental health and disability services, including services provided by Aboriginal Community Controlled Health Organisations and other existing Aboriginal health and community organisations’ (Commonwealth of Australia, 2019: 190).
Aboriginal Community Controlled Health Organisations (ACCHOs) are ‘a primary health care service initiated and operated by the local Aboriginal community to deliver holistic, comprehensive, and culturally appropriate health care to the community which controls it, through a locally elected Board of Management’ (National Aboriginal Community Controlled Health Organisation No date). There are 143 ACCHOs across Australia, with services in all states and territories (National Aboriginal Community Controlled Health Organisation No date). All ACCHOs provide holistic primary health care services to older Indigenous peoples though few are formally funded to provide aged care services such as home care, respite care and residential aged care. In contrast, there are Aboriginal Community Controlled Organisations (ACCOs) that are not primary health care organisations but rather specialise in providing home-based and residential aged care services to Indigenous elders. These aged care ACCOs are similar to ACCHOs in that they are ‘an incorporated organisation initiated by the Aboriginal Community and governed by an Aboriginal Body elected by the Aboriginal Community’ (Nunkuwarrin Yunti of South Australia Inc., 2015).
This study aimed to explore the overarching principles, practices, enablers and challenges of Aboriginal community-controlled services that provide aged care tailored to the needs of older Indigenous peoples and examine the aged care planning activities and implementation actions that guided the integration of aged care service delivery within the ACCHO primary health care model.
Method
This study was undertaken by the Centre of Research Excellence in Aboriginal Chronic Disease Knowledge Translation and Exchange (CREATE), an Indigenous-led centre of research excellence housed within the Wardliparingga Aboriginal Health Equity theme at the South Australian Health and Medical Research Institute and funded by the National Health and Medical Research Council of Australia. We used Indigenous methodologies that incorporated Indigenous leadership and governance, strength-based perspectives, Indigenous research methods, the privileging of Indigenous voices and centring of Indigenous knowledges (Rigney, Reference Rigney1999; Wilson Reference Wilson2008; Smith, Reference Smith2012; Watson, Reference Watson2014). The research team was predominantly Aboriginal and was led by an Aboriginal chief investigator, and yarning approaches were used during data collection. In addition, we used the research process as an opportunity for capacity-building Aboriginal workforce. Throughout the research process, we followed nine ethical principles for Aboriginal health research as co-designed with Indigenous communities in South Australia (e.g., partnership, respect, reciprocity, ownership) (South Australian Health and Medical Research Institute, 2014).
The CREATE Leadership Group, comprising predominantly Indigenous and also non-Indigenous nominated representatives from the ACCHO sector, provided governance for the research. The Leadership Group met twice-yearly and identified aged care as 1 of 10 priority domains for Indigenous peoples. We undertook a systematic review of the international literature to elaborate practices applied by both primary health care and aged care services to support the well-being of older Indigenous peoples (Davy et al., Reference Davy, Kite, Aitken, Dodd, Rigney, Hayes and Van Emden2016). The Leadership Group then recommended that the research team explore best practice principles and practices in culturally aligned aged care provided by Aboriginal community controlled services since ACCHO service delivery models are infrequently described within academic reports and publications.
Recruitment and data collection
The CREATE Leadership Group identified two exemplar services to explore and define approaches to best practice in Aboriginal community-controlled aged care:
-
1) Case Study 1: Aboriginal Community Services, a metropolitan ACCO aged care service in South Australia with a long history providing home-based, respite and residential aged care services;
-
2) Case Study 2: Institute for Urban Indigenous Health, a metropolitan ACCHO primary health care service in Queensland that had recently integrated home-based and respite aged care within the organisation’s primary health care service delivery model.
The research team approached each organisation inviting participation in an in-depth case study. During initial engagement and organisational approval processes, a Memorandum of Understanding was developed describing mutually agreed terms and conditions for the scope of work that included site visits, interviews and yarning circles with interested staff, and the completion of a Case Study Tool to collect descriptive information about the organisation. The research team subsequently visited the services to meet with staff and invite their voluntary participation in semi-structured interviews and/or yarning circles. During Case Study 2, a member of staff accepted an invitation to fulfil the role of an Aboriginal Research Fellow. In a two-way learning approach, the Aboriginal Research Fellow received support and capacity strengthening from the research team and provided the research team with expert insights and interpretations regarding aged care practice. The Aboriginal Research Fellow undertook interviews and analysis and contributed to the interpretation and reporting of results.
Data collection for Case Study 1 was undertaken during multiple sites visits in July 2016 by three Aboriginal members of the research team. For Case Study 2, site visits and data collection occurred during May and June 2017 with interviews and yarning circles undertaken by the Aboriginal Research Fellow, an Aboriginal researcher and a non-Indigenous member of the research team. During interviews and yarning circles, participants were asked about their current role, about how aged care services came about in the organisation (i.e. why, for whom, when, and what was crucial for ensuring its development/implementation), how aged care services currently work (i.e. how it has changed over time, what currently works well and for whom, what currently does not work so well, what improvements could be made, and what is crucial for its sustainability) and what best practice does or should look like in the ACCHO sector (i.e. what is needed to consistently provide best practice service delivery, what issues should be considered in relation to the development of a best practice service delivery framework for ACCHOs). Interviews and yarning circles were digitally recorded with consent, and participants were provided with an opportunity to review transcribed text.
Analysis
A framework approach to analysis (Ritchie et al., Reference Ritchie, Lewis, Nicholls and Ormston2014) was undertaken in NVivo Pro (QSR International) using an a priori coding framework developed by the research team. Transcribed and de-identified text from interviews and yarning circles were coded according to seven broad categories within the analysis framework: the community and organisational context; aged care service planning, integration and provision; contributing factors necessary for implementation and sustainability of services; challenges associated with service provision; perceived outcomes of service provision; recommendations for maintaining and expanding services; and implications for other ACCHOs considering aged care implementation and provision. Relevant contextual information sourced from the case study sites’ websites and 2014/2015 annual reports was used in the analysis.
Coding was undertaken by an Aboriginal researcher, the Aboriginal Research Fellow and a non-Indigenous researcher. Three Aboriginal researchers, the Aboriginal Research Fellow and two non-Indigenous researchers contributed to the analysis of coded data. Draft case study reports were compiled by the research team, reviewed and refined by key personnel within the case study sites prior to co-development of recommendations and finalisation of the reports. Key findings from the two case studies were synthesised, presented to and discussed with the CREATE Leadership Group during three face-to-face meetings and one teleconference. The Leadership Group contributed to the contextualisation of the findings for the ACCHO sector, offered additional insights from services in jurisdictions beyond the selected case study sites and highlighted challenges impacting Indigenous older peoples and the ACCHO sector more broadly.
Results
Across the two case study sites, there were 46 members of ACCHO staff and Board of Management members who participated (Table 1). During Case Study 1, 18 members of staff participated in interviews, and during Case Study 2 there were 15 participant interviews, 3 group interviews (with two staff members in each) and one yarning circle with 7 participants. Data from Case Studies 1 and 2 was used to inform the principles, enablers, challenges and outcomes of Aboriginal community-controlled aged care, and data drawn from Case Study 2 informed the ways of working, aged care planning and implementation actions related to aged care service provision integrated within primary health care. The reported principles, enablers, challenges and perceived outcomes of Aboriginal community-controlled aged care are listed in Table 2 and described in detail below.
Table 1. Case study participants

Table 2. Summary of principles, enablers, challenges and outcomes of Aboriginal community-controlled aged care service delivery

Principles
Guiding principles of Aboriginal community-controlled aged care service delivery were identified across the two aged care case studies. The identified principles highlighted how respect for culture, cultural identity, cultural safety and community connection are paramount to promote holistic (i.e., social, emotional, cultural, physical) well-being in aged care service delivery.
Staff members spoke of the significance of being an Aboriginal organisation which meant respecting traditional Aboriginal customs, values and beliefs and supporting the Aboriginal identity of clients. This underpinned all aspects of service delivery and was closely related to other principles. Connection with elders and communities was enabled by the employment of Indigenous staff who actively built and maintained relationships with elders, their families and communities to understand the unique needs of elders and facilitate connections.
[I]t’s about them probably, knowing this is an Aboriginal organisation and Aboriginal people work here. They kind of feel connected to start with, they’re willing to have a go, to come out and have a go. [Aboriginal ACCO staff member]
Participants described providing culturally safe care to older Indigenous peoples which was guided by strong Aboriginal governance and enabled through Indigenous workforce and cultural safety training for all staff.
“Sorry, just to add to that, and I guess it is the, it’s the value of having Aboriginal workers and the value of having other Aboriginal elders - that’s a huge part of the feedback is, um, you know, it’s culturally safe and it’s, um, and I feel something familiar and, yeah, that sense of connectedness, I guess, that comes with that”. [Non-Indigenous ACCHO staff member]
A focus on holistic well-being consistent with Aboriginal understandings of health was demonstrated through programs that supported the social, emotional, cultural and physical well-being of older Indigenous clients. The services provided opportunities for aged care clients to strengthen their Indigenous identity and practice culture as well as connect with other community members during social events, cultural celebrations and trips on country.
[I]t’s about meeting other Aboriginal people that they know. It’s about being in a happy environment, it’s about sharing food, sharing stories. [Aboriginal ACCO staff member]
Participants reflected respect for self-determination when describing client-directed care approaches where older Indigenous peoples were supported to make decisions about the nature of care they receive.
Don’t make decisions for them, ask them. And I know that it’s – it’s talked about a lot, and it doesn’t happen often enough. I think that’s something people could learn from us. [non-Indigenous ACCO staff member]
In both organisations, participants spoke of consulting with older Indigenous peoples and providing tailored services to meet the unique needs of their local communities.
[A]s well as having the elders on our governing Board, our Board of management, we also have a client advisory group, that client advisory group for the Adelaide programs is made up of elders who receive our services and we meet three or four times a year just to talk about what we’re doing how well we’re doing it whether there are any things which we should be doing more of or changing and that’s direct feedback to us from some of the elders. [Aboriginal ACCO staff member]
Individuals spoke of a strong personal commitment to work and managers spoke of employing staff with a fundamental compassion for older Indigenous peoples and a willingness to go the extra mile. Some participants, and in particular non-Indigenous staff members, reflected on the importance of maintaining credibility in the eyes of clients, client’s families and the broader community.
Because that would be the worst thing, if I say, “I’ll get this all fixed and wave my magic wand,” and then I couldn’t do it, that client is not going to trust me any longer. They are going to think that, oh, yeah, she says she’ll do it and doesn’t. So I don’t. Unless I know damn well I can do it, I don’t ever say I can. I’ll just say, “I will try.” [non-Indigenous ACCO staff member]
Enablers
Many factors that contribute to effective Aboriginal community-controlled aged care service delivery were identified across the two case studies. Participants spoke of strong governance where the Board of the organisation provided integral connection to community, strategic planning, needs assessment and priority setting to inform the development of programs targeted to the needs of elders in the community.
[H]aving a good mix on the Board is very important, a mixture of skills and experience and knowledge, clearly our Board has a very good mix in that respect, have a very good understanding of their role and responsibility and executing their fiduciary duties et cetera. What’s also important about our Board is that they have a very good relationship with the management team and also all of our staff, they feel part of the organisation and that relationship between the management and in particular myself and the Board is – is probably one of the strongest parts of the – the organisation’s operations. [Aboriginal ACCO staff member]
Effective leadership was another identified enabler of aged care service provision across both aged care service providers.
Yeah, it’s – it’s a hard one to define, but I think that it comes from the top. So, it comes from (CEO’s) philosophy. It comes from him wanting something better for the elders. [non-Indigenous ACCO staff member]
An organisational culture centred on respect for clients’ Aboriginal identity was frequently reported as was the importance of a local, caring, qualified and culturally safe aged care workforce necessary for culturally safe aged care service provision. Effective workforce recruitment and training processes were considered important across both organisations where workforce shortages were commonplace.
“So we then partnered with a training centre. We had to, and we developed the resources so they weren’t being trained in normal aged care, they were being trained in our aged care, so it was kind of contextualised and everything else. And as a result I’m thinking maybe, I’ve seen a few, about 60 something people have been trained up, um, since and the majority of those guys are in employment now”. [Aboriginal ACCHO staff member]
Participants spoke of effective communication and clear referral pathways across the primary health care and aged care teams as positively contributing to service provision. Effective organisational structures and operating systems were a necessary enabler of aged service delivery, with effective financial management systems enabling the management of multiple income streams across aged care and primary health care services. Engaging with community through continuous quality improvement processes ensured that services were safe and tailored to the needs of older Indigenous clients. Finally, relationships with external organisations ensured that through effective advocacy, the holistic needs of older clients could be met, and workforce training needs could also be met through external providers where necessary.
Ways of working: aged care integrated within the ACCHO
Participants described how integration of aged care within the ACCHO enabled older Indigenous clients to access both holistic primary health and aged care services through a continuous and coordinated care model. Care coordination was provided through the work of both the Primary Health Clinic and Aged Care Teams and managed through informal ‘yarns’ (an informal style of conversation) and formal multidisciplinary case conferences attended by the elder as well as key personnel such as Aged Care Workers, General Practitioners, Aboriginal Health Practitioners and Allied Health personnel.
The ACCHO established referral pathways to their Aged Care Team that included self-referral, and referral from both the health clinic and community teams (e.g. the Social and Emotional Wellbeing Team). A practical model of the organisation’s aged care referral pathway is depicted in Figure 1.
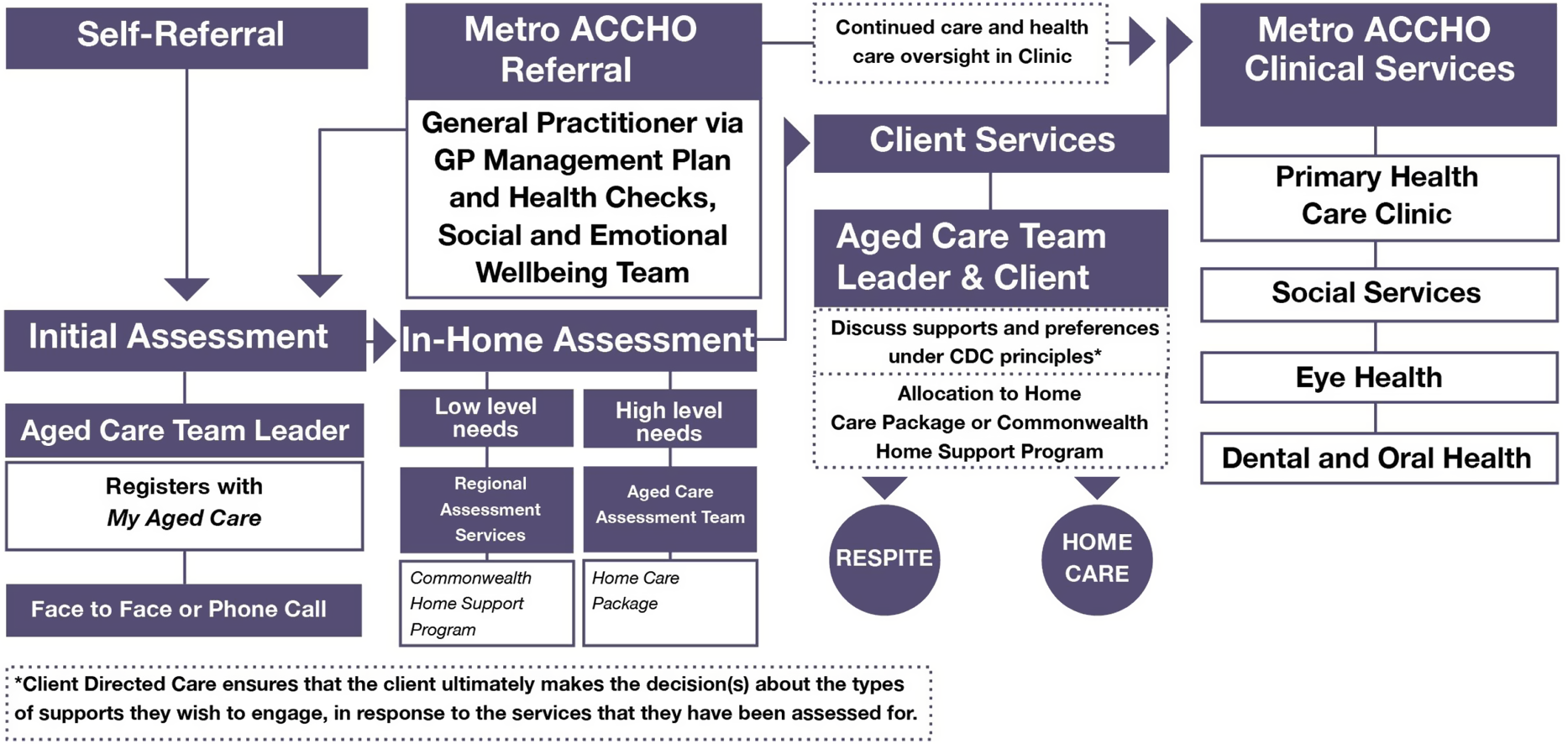
Figure 1. Referral pathways for aged care clients within the ACCHO
The Aged Care Team spoke of supporting clients to navigate the aged care system and to get the most out of the funding available to them. This included registering for aged care services, accessing in-home assessments and yarning with clients to create an Aged Care Plan based on their needs and preferences. This could include home care services (such as personal care, clinical care, domestic assistance, home maintenance), respite care, social support and advocacy. A Community Visitor Scheme was also in place to connect with Indigenous older peoples living in both mainstream residential facilities and at home.
Aged care planning
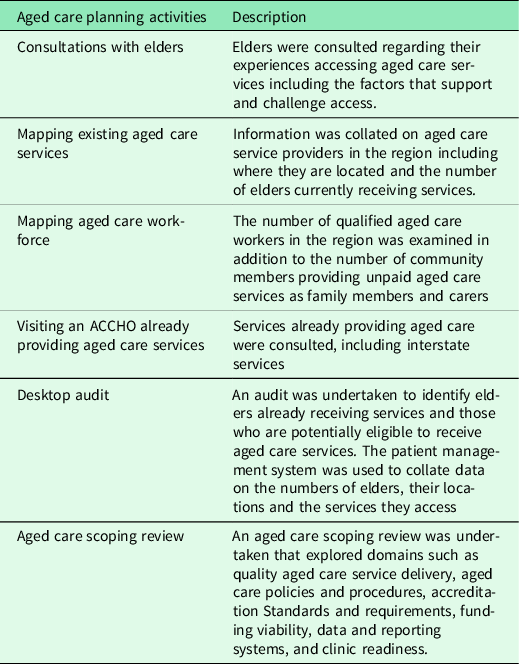
ACCHO staff members provided several examples of planning activities they had undertaken to determine the readiness of the organisation to integrate aged care with primary health care services. These included activities to identify community need, determine aged care service gaps, identify the current and potential aged care workforce and understand how other ACCHOs provided aged care. Various audits and internal scoping exercises were undertaken to determine the readiness of the organisation and financial viability of taking on aged care. A summary of the aged care planning activities undertaken by the ACCHO is provided in Table 3.
Table 3. Aged care planning activities undertaken by the ACCHO
Implementation actions
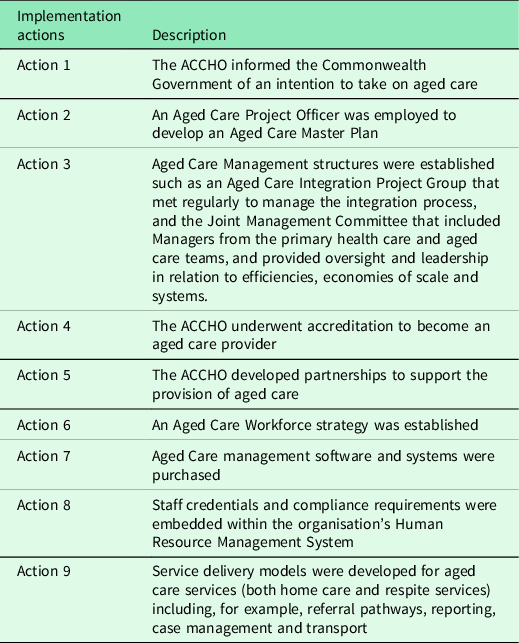
The integration of aged care with the ACCHO’s primary health care model was seen to be enabled by the recruitment of key personnel with experience and knowledge of the aged care system (including terminology, software and systems, funding and output measurement) who guided the aged care planning and integration processes including development of an Aged Care Master Plan. The analysis identified nine implementation actions, not necessarily sequential, that supported the integration of aged care services within the ACCHO, as detailed in Table 4.
Table 4. Implementation actions for the integration of aged care within the ACCHO
Challenges
To reduce barriers to access for older Indigenous clients, both case study sites strived to provide aged care services at no out of pocket cost, and as a result funding challenges were frequently reported by participants. During the process of integrating aged care services, the ACCHO went into financial deficit. The ACCHO also met with a great deal of complexity in coordinating multiple sources of funding (both primary health care and aged care funding streams) and in providing a range of unfunded services such as advocacy and support.
Participants from both organisations reported workforce shortages, particularly a shortage of Indigenous staff. A lack of existing workforce led the ACCHO to invest strongly in growing their own qualified culturally safe aged care workforce through partnering with training organisations and developing resources.
I believe there’s – there’s lots of opportunity for us to continue to grow, and, that growth is really dependant and reliant on us growing our staff, our staffing numbers, so having the right people with the right skills available at the right time is particularly important for us as we move forward and continue to grow. [Aboriginal ACCO staff member]
The challenge of change management processes was discussed in relation to integrating aged care within the ACCHO’s primary health care service delivery model (e.g. communicating with staff, establishing referral pathways). Related to this was the burden placed on ACCHO staff to rapidly develop their knowledge of the aged care system (e.g., processes, funding, terminology, applications and accreditation requirements) and to develop effective financial management systems to manage the increased complexity.
The government’s aged care reforms were also described as a challenge, as was a reported lack of coordination between government departments.
“There seems to be a real lack of integration between government bodies, so Department of Health for instance allocates a package but it’s paid through the Department of Human Services, um, so if their data programs aren’t you know, connecting, then that can create issues at a service level, so for instance, um, just in the last month for some reason, no one can quite tell me why, a client was only paid part of her subsidy.” [non-Indigenous ACCHO staff member]
ACCHO workforce also described that the eligibility requirements of the aged care system were challenging for elders, and particularly for those with non-Indigenous spouses whose aged care eligibility criteria were different. They referred to challenges elders face in navigating the online portal for aged care access, and the considerable time they invest in supporting elders to navigate the system. Finally, they spoke of needing to support clients to interpret and respond in a timely way to unclear correspondence from social services and government departments.
Perceived outcomes
Participants felt that ACCOs have inherent benefits, including that their connection to elders and community means they can better tailor services to client needs and promote Aboriginal identity and cultural connections.
“[H]e just lit up as soon as he saw a Nunga come in and we started talking about people that he knew, he was originally over from (regional town), all this sort of stuff and he knew all the (Aboriginal kinship group) mob from (name of place) so he really lit up”. [non-Indigenous ACCO staff member]
Participants reported that they were able to increase the number of elders receiving aged care which enabled the service to reduce the pressures and responsibilities on family carers. They also reported that providing better support for elders’ social, emotional and cultural well-being led to improvements in physical health outcomes. In particular, they reported that they were able to increase access to affordable, culturally safe and quality aged care.
“By using the integrated model of care, um, and by establishing the way that we have around putting the – the older – the elder, at the centre of all of their care, not just aged care, we’ve been able to do it cost free, so there’s no - no need for co-contribution for our elders, so that we’ve broken down whatever barriers we can, to access the services, you know.” [Aboriginal ACCHO staff member]
Participants provided examples of how the integrated care model and close connections with elders ensured the changing needs of older clients were identified and safeguarded in an ongoing way, through additional supports and services.
“…transport officers, they’re really good at communicating back to the team where, say, there are changes they can sense if there are difficulties in getting a person in the car and all of those sorts of things that come up”. [Aboriginal ACCHO staff member]
ACCHO workforce reported that the integrated model enabled elders to access their local ACCHO for both aged care and holistic primary health care reducing the complexities associated with navigating multiple services. Integration of services also enabled optimal discharge planning following hospitalisations and efficient referrals between the clinic and aged care teams. Integration of services also created economies of scale that supported unfunded activities such as transport services for elders. Finally, the service invested in workforce strategies which lead to increased numbers of local qualified culturally safe aged care workers.
“So really an important thing too about the social determinants stuff, you look at somewhere like (Place Name) where employment, unemployment rates are high, and particularly for our people, the vast majority of guys that come through the training were long-term unemployed”. [Aboriginal ACCHO staff member]
Discussion
The ACCHO sector has been supporting older Indigenous peoples with holistic primary health care over many decades following the establishment of the first Aboriginal community-controlled service in 1971 (Khoury, Reference Khoury2015). Culture is at the centre of all ACCHO primary health care service delivery (Harfield et al., Reference Harfield, Davy, McArthur, Munn, Brown and Brown2018) with culturally respectful care attributed to employment of Aboriginal staff, welcoming spaces, the integration of cultural protocols, a social view of health and strategies to promote access (Freeman et al., Reference Freeman, Edwards, Baum, Lawless, Jolley, Javanparast and Francis2014). This cultural safety is valued by Indigenous clients who also value the accessibility, holistic and diverse nature of ACCHO services (Gomersall et al., Reference Gomersall, Gibson, Dwyer, O’Donnell, Stephenson, Carter, Canuto, Munn, Aromataris and Brown2017). The added benefit that ACCHOs bring as an aged care provider, as demonstrated through the case studies reported here, is their ability to promote elder well-being and protect elder safety through intimate knowledge of and connections to family and community. The integrated primary health and aged care model also promotes access by reducing the complexities elders face in navigating multiple services and systems. It is well recognized that the social determinants of health play a key role in shaping the life expectancy gap for Indigenous peoples (Commonwealth of Australia, 2013; AIHW, 2016). ACCHOs lead the way in providing holistic services to tackle social factors (Khoury, Reference Khoury2015), and those supported to provide aged care services will be in a strong position to manage the comorbidities and social complexities that many older Indigenous peoples’ face.
This study demonstrates that ACCHOs are ideally positioned to provide aged care services since they provide culturally safe client-centred care, promote the cultural identity and connectedness of older Aboriginal peoples, support self-determined decision-making and enable elders to remain independent for as long as they can. This is consistent with a review of international evidence that identified culturally safe care, maintaining Indigenous identity and promoting independence were key domains related to well-being for older Indigenous peoples (Davy et al., Reference Davy, Kite, Aitken, Dodd, Rigney, Hayes and Van Emden2016). A range of perceived benefits of Aboriginal community-controlled aged care were reported by participants in this study including increased access to affordable, culturally safe and quality aged care that strengthened cultural identity and connections and led to improvements in health outcomes. This provides evidence to support the recommendation of the Royal Commission into Aged Care Quality and Safety (Commonwealth of Australia, 2019: 190) that aged care for Indigenous older peoples should be integrated with ACCHO and ACCO services. Our findings suggest that this would increase access to aged care services for Indigenous elders and promote and support elders to navigate multiple health, social and aged care services. In order for the Aboriginal community-controlled sector to be successful, however, the challenges identified within this study related to the aged care system and to the process of integrating aged care must be considered. Concurrent investment must also be provided to strengthen the Indigenous aged care workforce and tackle workforce shortages.
The findings elaborated here highlight the strengths and successes of metropolitan Aboriginal community-controlled aged care models, much needed given that a majority (81.4%) of Indigenous peoples live in urban and regional areas (ABS, 2018). This adds to the existing evidence base on well-being and quality of life in older Aboriginal peoples (Radford et al., Reference Radford, Mack, Robertson, Draper, Chalkley, Daylight, Cumming, Bennett, Jackson Pulver and Broe2014; Davy et al., Reference Davy, Kite, Aitken, Dodd, Rigney, Hayes and Van Emden2016; Smith et al., Reference Smith and Gilchrist2017; Davy et al., Reference Davy, Braunack-Mayer, Brown, Harfield, Lynch and Kite2018; Smith et al.., Reference Smith, Gilchrist, Taylor, Clinch, Logiudice, Edgill, Ratcliffe, Flicker, Douglas, Bradley and Bessarab2021) and remote aged care service delivery for Aboriginal peoples (Smith et al., Reference Smith, Grundy and Nelson2010; LoGiudice et al., Reference LoGiudice, Smith, Lindeman, Carroll, Atkinson, Schaper, Lautenschlager, Murphy and Flicker2012; Bell et al., Reference Bell, Lindeman and Reid2015). The elucidated aged care planning processes and implementation actions can inform an expansion of Aboriginal community-controlled aged care services to meet the growing numbers of older Indigenous peoples. Importantly, the findings elaborated here are likely to be of relevance to primary health care providers, academics and policy makers in Canada, the US and New Zealand in developing models of service delivery to better support their respective First Nations, Native American and Maori elders.
The strengths of the ACCHO sector have been recognized in the recent National Agreement on Closing the Gap which was signed by all Australian governments and a collective of ACCOs – the Coalition of Peaks (Australian Government, 2020). The Agreement provides a blueprint for closing the gap on Indigenous disadvantage in Australia. ‘Building the Community-Controlled Sector’ is the second of four priority reforms, with co-signatories stating under Item 43 that:
‘the Parties acknowledge that Aboriginal and Torres Strait Islander community-controlled services are better for Aboriginal and Torres Strait Islander peoples, achieve better results, employ more Aboriginal and Torres Strait Islander peoples and are often preferred over mainstream services’. ( Australian Government, 2020 , 8).
If the first target of the National Agreement – to ‘Close the Gap in life expectancy within a generation, by 2031’ (Australian Government, 2020: 17) – is to be realized, the integration of aged care service provision within ACCHO primary health care services must be adequately resourced and supported by aged care workforce strategies, capacity building initiatives and governance and operational support. The access challenges experienced by older Indigenous peoples (Australian Association of Gerontology, 2018) must also be addressed, and identified actions for service providers considered (Department of Health, 2019).
This study applied case study methodology to understand the principles and practices of Aboriginal community-controlled aged care service provision. As such, the findings provide best practice exemplars but may not represent the experiences of all services across the Aboriginal community-controlled sector. The findings may be useful for ACCHOs considering integrating aged care. Points of difference will depend on the ACCHOs size, context, workforce capacity and the needs of the elders they serve. The case studies were undertaken with metropolitan-based services, and there are likely to be unique challenges facing ACCHOs in regional and remote settings in relation to taking on aged care service provision and building a culturally safe aged care workforce. Future research could explore the aged care service requirements of Aboriginal and Torres Strait Islander communities in different settings (i.e., urban, regional, remote). A comparison of aged care service delivery characteristics and outcomes across Aboriginal community-controlled services compared with those of mainstream (i.e., government-run or privately owned) aged care services could also be explored in future studies.
Conclusion
Culturally responsive and accessible aged care services must be developed to meet the unique and often complex needs of a growing number of Indigenous elders. The Aboriginal community-controlled sector is ideally positioned to provide tailored aged care and to promote connection between Indigenous elders and health and social services. Where stand-alone Aboriginal community-controlled aged care services are not available, the ACCHO sector must be adequately resourced and supported to integrate aged care and primary health care service delivery models. Concurrent investment in strategies to strengthen the Indigenous aged care workforce is necessary to promote culturally safe aged care and effective advocacy for Indigenous elders.
Acknowledgements
The authors would like to thank and acknowledge the CREATE Leadership Group who identified case study sites, guided the research team and provided ongoing contributions to the refinement and interpretation of findings. The authors would like to thank and acknowledge staff members within the case study sites who participated in the research, Ben Thomson who supported the refinement of the case study report for Case Study 2, and Karen Glover who undertook interviews for Case Study 1.
Financial support
This study was funded by the National Health and Medical Research Institute of Australia (NHMRC #1 061 242). AB is supported by a Senior Research Fellowship (NHMRC #1 137 563).
Conflicts of interest
None declared.
Ethical standards
The authors assert that all research procedures complied with ethical standards of the National Health and Medical Research Council of Australia as outlined in ‘Ethical conduct in research with Aboriginal and Torres Strait Islander Peoples and communities: Guidelines for researchers and stakeholders 2018’ and with the Helsinki Declaration of 1975, as revised in 2008.
This study received ethical approval from the Aboriginal Health Research Ethics Committee (04-16-651), South Australia; The University of Adelaide Human Research Ethics Committee (H-2015-221), South Australia; St Vincent Hospital Melbourne (HREC-A 110/16), Victoria; Aboriginal Health & Medical Research Council Ethics Committee of New South Wales (1123/15), New South Wales; Central Australian Human Research Ethics Committee (HREC-15-352), Northern Territory; Menzies School of Health Research Human Research Ethics Committee (HREC 2015-2481), Northern Territory; Western Australian Aboriginal Human Research Ethics Committee (680), Western Australia.








