Introduction
The ‘Papillon’ technique of contact X-ray brachytherapy (CXB) uses 50-kV X-rays to deliver up to 30 Gy per fraction to treat early-stage rectal tumours. It is delivered fortnightly over three or four fractions, via a treatment rectoscope under direct vision using dedicated machines such as the Papillon 50 (Ariane, Alfreton, UK). The technique is associated with no mortality and very little morbidity, Reference Myint, Gerard and Myerson1 aside from short-term bleeding in around 26% of patients. Reference Myint2 Although the technique has been around for over 80 years, it has recently seen a resurgence in the UK as a viable treatment option. Colorectal cancers are currently the fourth most common type of cancer in England, with 27% of these being rectal cancers. 3 The number of these patients deemed suitable for CXB is increasing due to improved availability of CXB in the UK and increased early detection from screening. Reference Myint4,Reference Logan, Patnick, Nickerson, Coleman, Rutter and von Wagner5
The National Institute for Health and Care Excellence currently supports the use of this procedure only for early-stage rectal cancer for which surgery is unsuitable or has been declined 6 due to a lack of high-quality evidence regarding efficacy. Although there is currently only one-level 1b randomised controlled trial for CXB, the phase 3 OPERA trial is currently open. 7 The current gold standard for treating rectal cancer is surgery, which has considerable mortality and morbidity for elderly patients Reference Myint, Ramani, Montazeri, Perkins, Myerson and Gerard8 and results in a permanent stoma in about a third of patients. Reference Myint2 Avoidance of a permanent stoma is an important outcome measure with great impact on patient quality of life. Reference Marijnen, van de Velde and Putter9 The need for a standardised set of criteria to guide CXB referral is becoming essential, yet the dearth of published data means that centres are instead relying on clinician experience and expertise.
The aim of this audit is to assess whether the correct categories of patients were referred for CXB treatment from a major cancer centre. Results from this audit could inform and guide future referral choices. The lack of guidelines meant that published data had to be collated to provide a standard for comparison. Referral guidelines are an important aspect of evidence-based practice, and this paper aimed to highlight key referral criteria to help inform this.
Methods
This study required a two-phase approach commencing with a preliminary literature review gathering published data in lieu of national guidelines. The second phase comprised an audit of referral patterns and outcomes against the published data.
Phase one: literature review
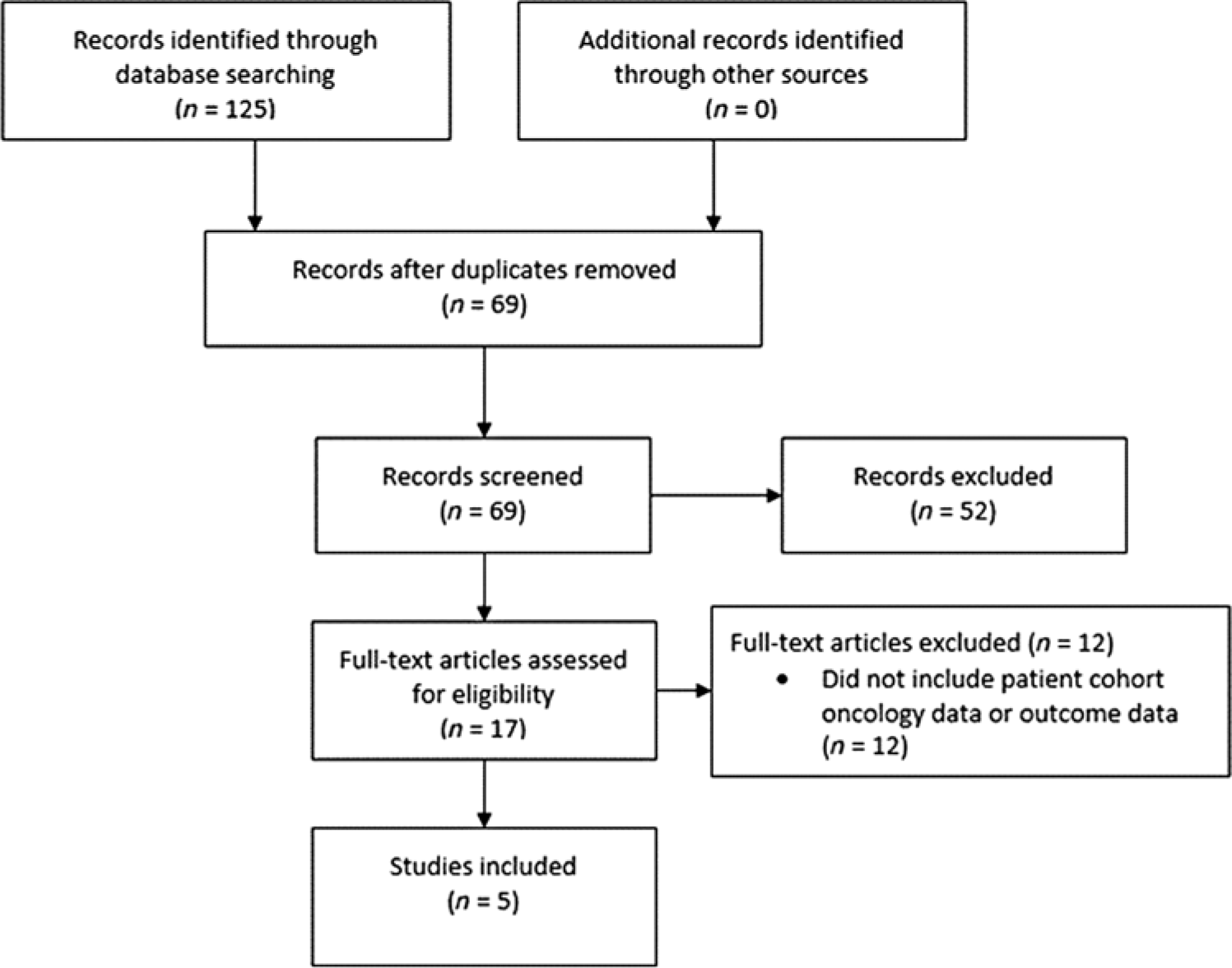
A search utilising variations and combinations of the keywords ‘Papillon therapy’ and ‘Rectal cancer’ was performed throughout the Medline, Scopus and Web of Science databases using the inclusion and exclusion criteria summarised in Table 1. Screening and quality assessment were performed as per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Reference Liberati, Altman and Tetzlaff10 guidelines and summarised in Figure 1. The remaining papers were considered the most relevant and highest quality evidence available to be included in the review. These were then analysed to extract patient and tumour characteristics data and outcome data for the cohort treated in each study. Outcome data comprised median follow-up, initial complete clinical response (cCR) rate, local recurrence (LR) rate after cCR (including after salvage surgery), local control (LC) after cCR, rate of distant metastases and overall survival (OS).

Figure 1. PRISMA flow diagram.
Table 1. Literature review inclusion and exclusion criteria

Phase two: audit
The patient cohort comprised patients referred and treated with CXB between 2013 and 2019. Extracted data included TNM staging, tumour location and differentiation, patient age and performance status (PS). Dates and results of the most recent radiological assessment were also included, along with cause of death (where appropriate) and any additional treatment received if local or distant progression was developed. Rationale for patient referral was extracted to identify those who were not suitable for surgery or wanted to avoid a stoma. All referred patients received CXB treatment at another regional centre, and the treatment was delivered according to departmental protocol. This consisted of 30 Gy of 50-kV X-rays delivered at each visit, using a Papillon 50 machine, as an outpatient every 2 weeks, with most patients receiving a total of 90 Gy delivered in three fractions over 4 weeks. Reference Myint, Smith and Gollins11 All patients were also prescribed either short-course radiotherapy of 25 Gy in 5 fractions over 5 days or long-course radiotherapy of 45 Gy in 25 fractions over 35 days, with or without concurrent chemotherapy. Palliative patients were excluded from the cohort to ensure accurate comparison with the published data. The project was approved by the Clinical Governance Committee as a retrospective audit with no requirement for ethical clearance.
Results
Development of criteria
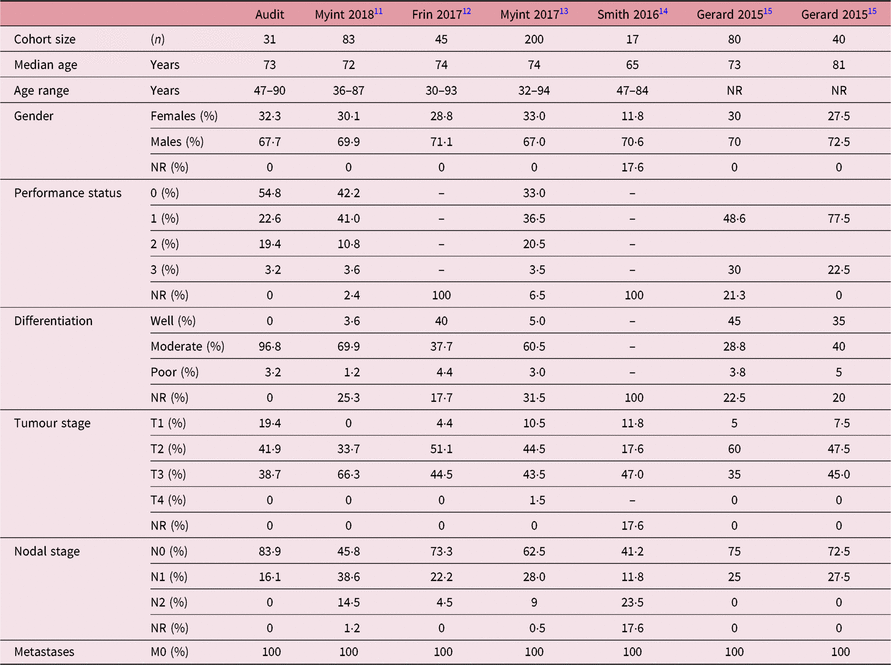
Referral and outcome data were gathered from five papers relating to six cohorts as summarised in Tables 2 and 3. All five of the included papers agreed that to be eligible for Papillon treatment, the patient must have a visible tumour or post-excision scar as a target at which to direct the CXB boost. Reference Myint, Smith and Gollins11,Reference Frin, Evesque and Gal12 Tumours from stage Tis-T4 were all treated across the five studies, with the main limitation mentioned being the size of the tumours, as bulkier tumours are difficult to treat due to a limitation arising from the maximum physical size of the treatment applicator. Reference Myint, Smith and Gollins13 Three of the five papers agreed that the maximum tumour size treatable with CXB was 3 cm, Reference Myint, Smith and Gollins11,Reference Myint, Smith and Gollins13,Reference Gerard, Frin and Doyen15 whereas two treated larger tumours, one treating up to 4 cm Reference Frin, Evesque and Gal12 and the other did not specify a maximum size, but explained tumours over 3 cm were treated using overlapping fields. All papers agreed that patients with tumours larger than their maximum size treated by CXB could have external beam radiotherapy tumour debulking prior to CXB dose boost. All studies included patients with and without nodal involvement at the time of diagnosis (N0–N2). The maximum distance from the anal verge of the tumour treated by CXB was either ≤10 cm Reference Frin, Evesque and Gal12,Reference Gerard, Frin and Doyen15 or ≤12 cm. Reference Myint, Smith and Gollins11,Reference Myint, Smith and Gollins13,Reference Smith, Al-Amin, Wright, Berry, Nicoll and Myint14
Table 2. Comparison of referral data

Abbreviation: NR, not reported or unknown.
Table 3. Comparison of outcome data

Abbreviations: FU, Follow-up; NR, not reported or unknown; cCR, Initial complete clinical response; LR, Local recurrence after cCR (including after salvage); LC, Local control; Mets, Presence of distant metastases; OS, Overall survival.
Where the information was given (n = 4), all papers treated well to poorly differentiated tumours, with the majority of tumours well or moderately differentiated. Reference Myint, Smith and Gollins11–Reference Myint, Smith and Gollins13,Reference Gerard, Frin and Doyen15 Similarly, the same papers included PS of patients (n = 3) and treated patients of any PS (PS0-3). No patients with metastatic disease were included in any of the studies, though three of the papers did state that patients with M1 disease and other patients who could not be treated with curative intent were treated palliatively using CXB. Reference Myint, Smith and Gollins11,Reference Myint, Smith and Gollins13,Reference Gerard, Frin and Doyen15 The median age of patients across the studies was comparable with a wide age range of 30–94 across all studies.
All papers included patients with inoperable tumours, those opted against surgery due to the associated morbidity and possible mortality and those who refused a stoma. Although not all studies included how many operable patients were treated with CXB, four out of the five papers indicated that the majority of patients treated were operable, with CXB treatment chosen to increase the chance of organ preservation and stoma avoidance. Reference Frin, Evesque and Gal12–Reference Gerard, Frin and Doyen15
The limited number of papers reflects the fact that Papillon technique is not regarded as a standard of care for rectal cancer, with only four centres in the UK currently offering CXB. Reference Rao, Stewart and Martin16 All the papers suffered from the same limitation of being retrospective studies which may have some degree of selection bias. Despite these shortcomings, all papers met the inclusion criteria and, due to the lack of any large multi-centre randomised trial, represent the highest quality of relevant evidence available at this time. From these results, a list of criteria for radical intent CXB treatment was derived for the audit as shown in Table 4.
Table 4. Criteria for radical intent CXB treatment

Audit results: patient characteristics
Over the audit period, 45 patients were referred for CXB treatment; of these, 5 were excluded as they were still undergoing Papillon treatment, and 9 were excluded as they were being treated with palliative intent. A study size of 31 patients may be considered a relatively small cohort, but 2 of the comparator cohorts had similar numbers (n = 40, n = 45) and 1 had fewer (n = 17). Patient demographics can be seen in Table 2; the median age of patients referred was 73, which was within a year of the median age of 4 of the 6 cohorts. Of the other two cohorts, one had a higher median age and one was lower. The gender ratio was similar across all studies, with male being the majority in all of them. PS was not included in all published data, although most patients were PS 0–1, which matched with the audit cohort. One of the criteria for referral identified above was that the patient was unsuitable for surgery or had refused surgery to avoid a stoma. Only two of the studies included the proportion of patients who were considered operable, so these data were not included in Table 2. The audit cohort identified 42% of patients as unfit for surgery, compared to 57% described as either inoperable or high risk in one study Reference Frin, Evesque and Gal12 and 27% described as inoperable in another. Reference Gerard, Frin and Doyen15
Audit results: tumour characteristics
Differentiation of tumour data was available in five of the six cohorts. However, in all five of these, a significant proportion was not known (17·7–31·5%). The majority of the audited cohort presented with moderately differentiated tumours (96·8%), which was higher than all the comparators; but, in all cohorts, well to moderate differentiation was the majority. The audit cohort had pre-treatment tumour stages between T1 and T3, while most of the tumours in all cohorts were stage T2 or T3. Nodal status was predominantly N0 in all studies with the audited cohort reporting 83·9% N0 nodal stage. No patients with metastatic disease were included in any of the cohorts.
Audit results: outcome data
Median follow-up of all seven cohorts ranged from 20 to 64 months with the audit cohort towards the shorter end at 22 months. Initial cCR, LR, sustained LC, metastatic spread and OS rates were compared. An ‘initial cCR’ was defined as following CXB but before any necessary salvage surgery. The rate of initial cCR for the audit cohort was high at 93·6%; this was similar to three of the six comparator groups. The LR rate after cCR included recurrence in all patients considered to have achieved a cCR following CXB and any necessary salvage surgery. A total of 20·7% of the audit cohort experienced LR for which no further treatment was possible; this was comparable to the reported rates which ranged from 11 to 27%. Sustained LC in the audit cohort was achieved for 25 of the 31 (80·6%) patients referred for CXB which is similar to 2 of these comparator cohorts with the other 3 cohorts reporting both higher and lower rates (60–95%). The rate of distant metastases was relatively low within the reported data, ranging from 8·5 to 20·5%, while the audit cohort rate was 13·8%. Finally, it was encouraging to see the audit cohort reporting the highest rate of OS at 83·9%, with one study reporting a similar rate of 82% Reference Smith, Al-Amin, Wright, Berry, Nicoll and Myint14 and the others ranging from 60 to 73%. Figure 2 shows the Kaplan–Meier plot for this within the studied cohort.

Figure 2. Kaplan-Meier plot of overall survival.
Discussion
Referral criteria
The different distribution of tumour (T) stage across the published evidence can partly be attributed to selectivity of studies with papers only reporting a specific cohort. However, and importantly for the validity of the outcome data, two papers found that stage of tumour was not a prognostic factor for achieving a cCR or for survival. Reference Myint, Smith and Gollins11,Reference Myint, Smith and Gollins13 Similarly, though nodal stage of patients was distributed differently in the audit cohort, with more N0 than other studies, this was also found to not be related to chance of achieving a cCR or local regrowth rates. Reference Myint, Smith and Gollins11,Reference Myint, Smith and Gollins13
While PS and age in the audit cohort were similar to the other studies, it did include more PS 0 patients than any of the other studies. Although PS and age were not found to be indications for cCR rate, Reference Myint, Smith and Gollins11 one paper did report them as factors for disease-free survival (both p ≤ 0·001). Reference Myint, Smith and Gollins13 This possibly reflected the median age and thus the likelihood of patient comorbidities as well as patient tolerance to external beam radiotherapy. Reference Myint17 It is likely, therefore, this higher proportion of PS 0 patients might have contributed to the higher OS reported in the audit cohort.
The underlying rationale for referral proved challenging to audit for several reasons. Firstly, not all of the studies included these data, despite all of them indicating that one of the main reasons for a CXB boos was to improve the rate of organ preservation and reduce permanent stoma risk. Reference Myint, Smith and Gollins11–Reference Gerard, Frin and Doyen15 Secondly, the criteria for patients either being unfit for surgery or inoperable were unclear and may have been reported differently for each study. This is a limitation for the study as having a higher proportion of operable patients who can undergo possible salvage surgery may improve overall LC rates for that cohort.
Overall, the patient and tumour characteristics of the audit cohort were similar in many ways to those of the cohorts reported in the published data. This suggested that, based on these criteria, referrals within the audit aligned well with current best evidence. This also indicated that comparison of outcome data would be valid.
Patient outcomes
Although cCR was used for comparing outcomes, the exact method and criteria used for assessing this were not explained well in all the papers and may have even changed with time or investigator expertise. This issue was acknowledged and within another recent paper which described how to accurately assess response to CXB. Reference Dunstan, Rockall, Potter and Stewart18 This possible limitation may explain the difference in initial cCR rates reported across the studies.
LR rate was similar across all seven cohorts, which is significant because this was found to be independent of PS, age, tumour stage, nodal stage, distance from anal verge, tumour size or treatment method. Reference Myint, Smith and Gollins13 The rate of distant metastases was higher in all of the studies with longer follow-up lengths, which may indicate time could be a factor for this outcome; however, one study with a longer follow-up time had a lower rate of distant metastases than the audit cohort.
Although it was difficult to make an accurate comparison of outcome data for all the reasons explored above, many of the outcomes of the audit cohort were comparable to published studies, especially LR after cCR, which reaffirms referral criteria. It is recommended that the audit be repeated after a longer follow-up period to ensure the outcome comparisons remain valid. Further work will also include stoma-free survival and bowel function data for all patients treated with CXB as this is highlighted in the literature as an important outcome and one of the main reasons that CXB is used over non-conservative surgical treatment. Like other recent studies have noted, evidence suggests that CXB treatment is indicated as a good, potentially organ preserving alternative to surgery for older, co-morbid patients who are inoperable or high surgical risk, as well as younger, stoma-averse patients, and has good cCR and LR rates. Reference Myint, Smith and Gollins11–Reference Myint, Smith and Gollins13 It is recommended that the national guidelines be updated to reflect this growing body evidence.
Limitations
As well as the limitations described above, this study has several other constraints. Firstly, as this study was a retrospective audit, the only data available at the time of review could be used. These data may include an unknown number of referred patients who were deemed unsuitable and rejected by the treating department. Criteria development was based on the strongest available current evidence, but all studies used had their own acknowledged limitations. In general, these were selective, retrospective, monocentric reviews over time periods where treatment techniques, assessment methods and equipment may have changed.
Conclusion
The results of this audit demonstrated that the demographic and pathological profile of the referred patients matched those reported in the literature. The similarity of the cohorts enabled comparison of outcome data which confirmed the validity of referral and treatment protocols. Although the limited evidence base and retrospective nature of the audit limit the strength of the findings, this work should guide future referrals until evidence from ongoing studies becomes available and can also be used to inform future audits undertaken in this area. It is also anticipated that the reviewed evidence presented here will contribute to the development of robust national guidelines.
Acknowledgements
None.