Introduction
Middle-ear surgery poses some particular challenges to the surgeon that can be aided by sympathetic anaesthesia. One must consider the type of procedure being performed to decide upon how best this is delivered. The patient's co-morbidities will be important, and in low-income settings the resources to detect and manage this will be relevant prior to deciding how to safely provide anaesthesia. Importantly, in the resource-poor setting, it is important to tailor the anaesthetic technique based on potentially limited equipment and infrastructure.
Many simple procedures can be performed under local anaesthesia (LA) with or without sedation. In the developing world setting, this may be a safe and effective way of providing anaesthesia; LA avoids the risks of general anaesthesia (GA), the requirement of equipment necessary to provide a GA safely, and even the need of an anaesthetist when a suitably trained person is not available. However, LA can be practically challenging in this environment, where communication may be limited because of a non-English speaking population. The LA technique requires co-operation and understanding by a suitable candidate. Engagement with a local staff member to help with this process proves invaluable.
Studies in high-income countries have demonstrated that most patients prefer LA, despite occasional discomfort, anxiety and claustrophobia during the procedure.Reference Yung1 Local anaesthesia may be preferable to the operating surgeon, as it allows the hearing to be tested intra-operatively, and may minimise blood loss. (Details of LA application for ear surgery are included later in this paper.) However, sudden movements and LA toxicity are poorly tolerated, and some middle-ear procedures are lengthy. Therefore, GA is still a widely used technique.
General anaesthesia
Pre-operative considerations
Pre-operative assessment is always important, but in this setting it may face certain challenges. There may be communication difficulties, a lack of medical records or a paucity of information on past medical history.
Particular consideration may be given to: paediatric patients, especially with regard to upper respiratory tract infections and the risk of airway complications (e.g. desaturation, coughing, bronchospasm); co-existing syndromes that may affect the anaesthetic or provision of a safe airway; co-morbidities, such as smoking, obesity, reflux or a difficult airway; anticoagulant medication (if safe, consider discontinuing use prior to surgery in order to prevent intra-operative bleeding); and a history of anxiety (pre-operative assessment will help assess the need for peri-operative anxiolysis).
Furthermore, controlled hypotension is important to facilitate a bloodless field. However, it may be relatively contraindicated in patients with end-organ dysfunction detected pre-operatively, such as: transient ischaemic attack, cerebrovascular disease or carotid stenosis (risk of cerebral infarction); ischaemic heart disease, angina or previous myocardial infarction (risk of cardiac ischaemia or infarction); and renal impairment or chronic kidney disease (risk of worsening renal function).
Intra-operative considerations
A safe anaesthesia technique for middle-ear surgery will: provide a bloodless surgical field with good visibility; enable avoidance of intratympanic pressure fluctuations; prevent post-operative nausea and vomiting; allow consideration of careful head positioning for optimal exposure of the surgical field; and ensure patient safety. The anaesthetic technique needs to maintain a sufficiently deep level of anaesthesia to prevent sudden patient movement, but also needs to allow for fast emergence and recovery, especially in the same-day surgery or ambulatory setting. Facial nerve monitoring is sometimes indicated in otological procedures and necessitates short-acting neuromuscular blockade agents for intubation. Special attention should be given to avoid post-extubation coughing, a Valsalva-like manoeuvre or bucking on extubation. This will prevent bleeding, early displacement of ossicular prostheses, and the risk of post-operative hearing loss, balance loss or dizziness.
Airway type
The airway has to be secured well, as access will be limited and the head may be turned frequently during the procedure.
Regarding the type of airway, a south-facing oral Ring–Adair–Elwin endotracheal tube provides a secure and definitive airway for a long procedure. Taping the tube so it is directed towards the non-operative ear facilitates optimal access for the surgeon to the operative field. The use of neuromuscular blockade to optimise intubation conditions can affect intra-operative facial nerve monitoring, and so short-acting agents may be advisable. A flexible supraglottic airway provides an excellent alternative; if used, this can be taken out in recovery to ensure a smooth emergence.
Endotracheal intubation is associated with the potential complications of sore throat, cough, dental injury, difficult emergence and the need for paralysis and intubation.
Use of the laryngeal mask airway does not require administration of neuromuscular blockade; furthermore, its use facilitates the resumption of spontaneous ventilation and is associated with a decreased likelihood of airway reflex stimulation.
Prospective randomised studies by Webster et al.,Reference Webster, Morley-Forster, Janzen, Watson, Dain and Taves2 and Atef and Fawaz,Reference Atef and Fawaz3 showed that use of a laryngeal mask airway in endoscopic ENT surgery was associated with: better cardiovascular stability during airway management on induction and emergence; superior maintenance of a stable plane of anaesthesia and controlled hypotension; an improved surgical field; smooth emergence from anaesthesia; and faster awakening time.
Large retrospective studies by Ayala et al.Reference Ayala, Sanderson, Marks, Hoffer and Balough4 and Taheri et al.Reference Taheri, Hajimohamadi, Soltanghoraee and Moin5 on laryngeal mask airway use in otological surgery corroborate these findings, indicating improved intra-operative haemodynamic stability, reduced anaesthetic drug use, shortened operative time and decreased incidence of adverse respiratory events. Disadvantages include the risks of malposition and extubation during head movement or mastoid dressing application at the end of the procedure.Reference Mandel6
Positioning
The patient is placed supine on the operating table. A reverse Trendelenburg position will improve venous drainage from the head and cause some hypotension. The patient's head is turned to the contralateral side, and precautions are taken to minimise venous congestion and obstruction. It is important to ascertain the range of head movement pre-operatively, and to account for any cervical spine abnormalities.
An arm board can be used on the non-operative side, but will need to be removed on the operative side, with the arm tucked into the patient's side to allow access to the surgical field.
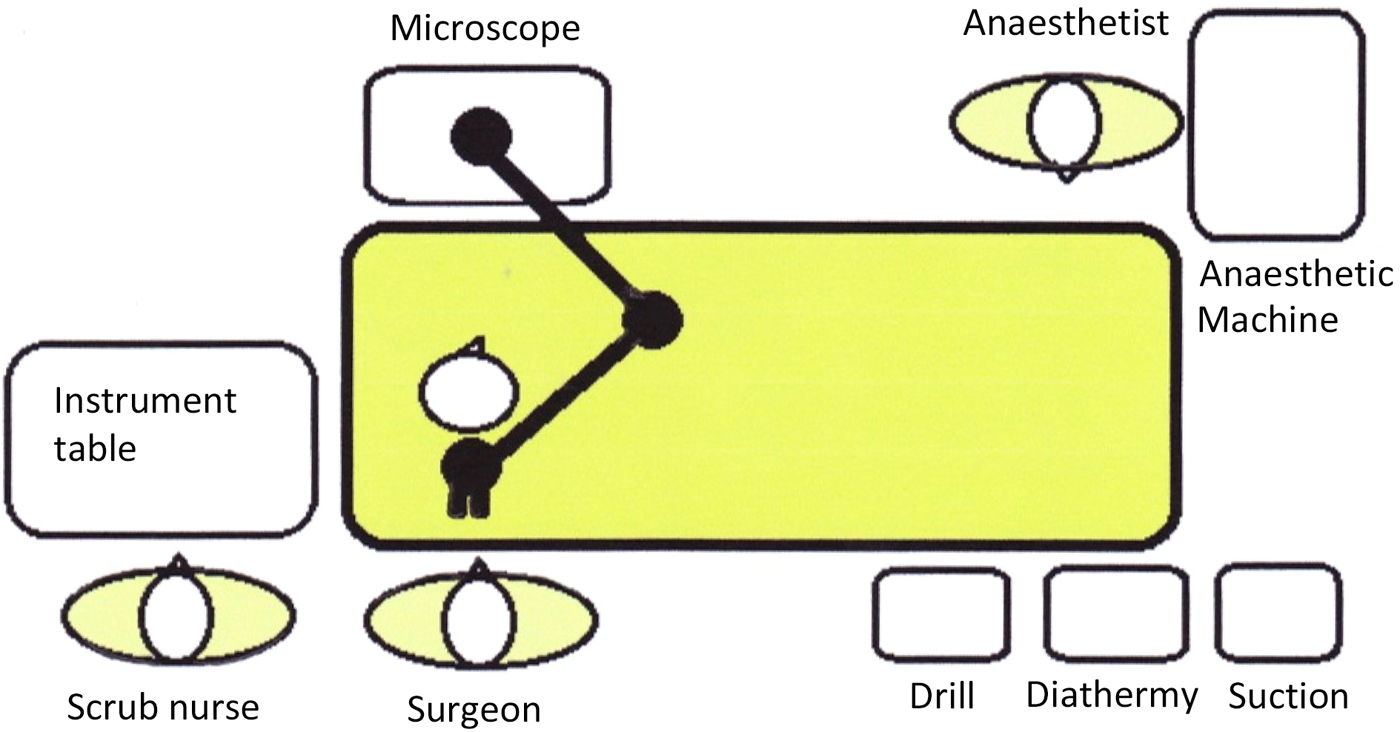
The ability to move the patient, rolling them away or towards the surgeon and altering the degree of ‘head-up’ position, are all important, as they aid the surgeon's view of the operative field. This is an additional consideration when securing the airway, and raises the importance of clear communication between the surgeon and anaesthetist. Often two straps are required to secure the patient to the operating table, in order to increase safety when rolling the bed from side to side. The positioning of equipment in the operating theatre needs to be considered; it should be sympathetic to the fact that the surgeon is operating near the airway, and the associated equipment (e.g. microscope) needs to be safely positioned (Figure 1).
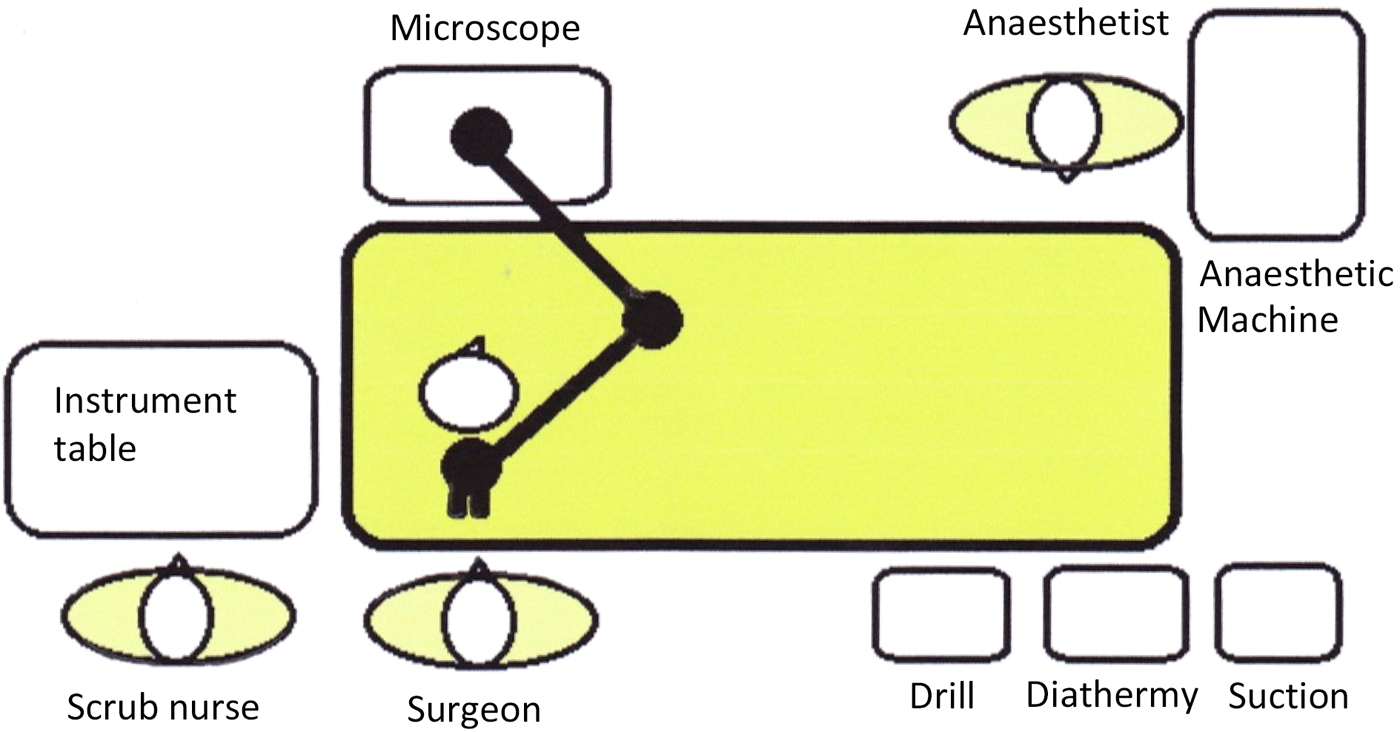
Fig. 1. Example of operating theatre layout for middle-ear surgery.
Hypotension
The middle-ear space is small, with an estimated volume of 2 cm3 (greater when considering the variable mastoid space as well). The field of view, obtained via either an operating microscope or rigid endoscope, is always a challenge, as procedures are performed down the limited space of the ear canal and via the mastoid. As such, even a very small quantity of active bleeding can severely hamper the surgeon's ability to safely operate in this region. Great care must be taken to prevent inadvertent damage to the delicate hearing structures, balance system and facial nerve. A clear view is of paramount importance. Reducing the bleeding is the primary goal of the bloodless-field anaesthesia used.
In order to achieve a bloodless field for middle-ear surgery, various anaesthetic techniques may be utilised.Reference Liang and Irwin7 Adopting controlled hypotension is important, as are strategies to reduce head and neck venous pressure.
The technique requires careful consideration. Often patients are young and otherwise healthy, but they may present with hypertension and obesity, which increase their risk of cardiovascular disease. The goal should be to maintain blood pressure within 20–30 per cent of pre-operative values. A discussion with the rest of the team about the risks and benefits of controlled hypotension should take place.
Physical and pharmacological techniques are employed to create a bloodless field. The physical methods include: a 15–20 degree head-up tilt, avoiding venous obstruction, normocapnia and controlled hypotension (systolic blood pressure = 80–90 mmHg, mean arterial pressure = 50–65 mmHg). The pharmacological methods include: inhalational anaesthesia (sevoflurane, isoflurane), vasodilators (nitroglycerine, sodium nitroprusside), beta-adrenergic agonists (esmolol, labetalol), alpha-2 agonists (clonidine), opioids (remifentanil) and magnesium sulphate.
Surgical site infiltration with local lidocaine (2 per cent) and adrenaline (1:80 000 or 100 000), carried out by the surgeon, reduces skin bleeding on incision. Topical adrenaline (1:1000) may also be applied on cottonoids, by the surgeon, to reduce bleeding from microscopic surfaces throughout the procedure.
Anaesthetic agents
The use of nitrous oxide is avoided as it increases the pressure within the middle ear, and may contribute to post-operative nausea and vomiting. Nitrous oxide diffuses into air-filled cavities (middle ear), causing an increase of middle-ear pressure. Rapid absorption of nitrous oxide at the end of anaesthesia can also cause profound negative pressure, resulting in hearing loss, graft disruption, nausea, vomiting and tympanic membrane rupture. Despite this, some surgeons may ask for nitrous oxide in an attempt to reverse pre-existing tympanic membrane retractions, as its ability to increase middle-ear pressure is sometimes a beneficial property.
The surgeon may employ facial nerve monitoring, if the required equipment is available. In such circumstances, the neuromuscular blockade needs to be short-acting so it wears off by the time that facial monitoring is required. Discussion of the World Health Organization checklist will allow all of those involved to know what is being used.
Regarding the depth of anaesthesia, an immobile patient is required, particularly during stimulating parts of a procedure and where the surgical moves are especially delicate (e.g. ossiculoplasty or working next to a dehiscent facial nerve).
Usual practice involves a combination of an opioid-based anaesthetic and low-dose inhalational agent, or total intravenous anaesthesia with propofol and remifentanil. The advantages of total intravenous anaesthesia include: a bloodless field whilst maintaining haemodynamic stability, smooth emergence, a reduction in post-operative nausea and vomiting, less airway reactivity, and excellent depth of anaesthesia when a propofol and remifentanil combination is used. In addition, there is a significant cost reduction compared with the use of inhalational agents.
When comparing commonly used agents, isoflurane lowers blood pressure via a vasodilating effect whilst preserving cerebral autoregulation, but at higher concentrations it causes an increase in intracranial pressure due to increased cerebral blood flow and impairment of cerebral autoregulation.
Sevoflurane causes hypotension by direct vasodilatation, without modifying cochlear blood flow.Reference Liang and Irwin7 Furthermore, it has a low blood gas solubility and low airway irritability, making it a good induction agent in paediatric patients. Its use, however, has been associated with a higher incidence of post-operative behavioural changes and emergence agitation.
All inhalational agents in high concentrations can interfere with the measurement of evoked potentials used for facial nerve monitoring.
Further reductions in blood pressure during surgery can be achieved using drugs such as vasodilators (nitroprusside, nicardipine and nitroglycerine), alpha-2A adrenergic agonists (clonidine and dexmedetomidine), beta-adrenergic antagonists (propranolol and esmolol), or alpha- and beta-adrenergic antagonists (labetalol). The use of magnesium as a loading dose and subsequent infusion has been shown to improve post-operative analgesia and reduce shivering when compared to remifentanil. However, in the groups studied, neuromuscular blockade was reversed with atropine and neostigmine at the start of surgery, which is unnecessary when a remifentanil infusion is used.
Anti-emetic drugs are routinely administered because of the often anticipated emetogenicity of this type of surgery.
A combination of ondansetron (5HT3 antagonist) and dexamethasone is superior to either drug alone.Reference Liang and Irwin7
Equipment
Delivering a GA in a low-income country may involve the use of old and unfamiliar equipment, so it is vital the anaesthetist has time to familiarise themselves with what is available.
A ready supply of ‘piped’ oxygen may not be installed and oxygen concentrators may be required.
Anaesthetic machines have been developed for use in this type of setting, with simplicity and safety being key aspects of their development.8 For example, the Glostavent® Anaesthesia Machine is designed to deliver safe inhalational anaesthesia in any environment, with or without electricity or compressed gases. Its mechanical ventilator makes it suitable for use as an anaesthetic machine for spontaneous breathing or ventilated patients, or as a ventilator in a recovery room or for longer-term ventilation in an intensive care unit.
Standard monitoring of blood oxygen saturation and carbon dioxide is required, as is an electrocardiogram. Arterial cannulation allows for invasive blood pressure measurement and can be particularly helpful when controlled hypotension is used, but may not be available in all settings.
Middle-ear surgery is variable in duration and can span several hours. The patient's temperature is maintained during surgery using active warming measures, such as forced warm air blowers. It has been demonstrated that even small amounts of hypothermia (less than 1 °C) can increase bleeding from operative sites.
Middle-ear surgery that is prolonged in duration, together with the hypotensive anaesthesia, can make the patient prone to pressure sores. These should be protected against with the use of careful patient positioning and padding under pressure points.
Emergence
Emergence needs to be smooth, to avoid increased venous pressure. When bandages are applied at the end of the procedure, the surgeon needs to take care to limit movement of the endotracheal tube and ensure its stability. This helps to prevent coughing and bucking on the airway, which may result in surgical bleeding. Similarly, post-operative nausea and vomiting need to be controlled, to prevent graft or prosthetic disruption or movement.
Post-operative considerations
Preventing nausea and vomiting with adequate hydration, and minimising opioids using multimodal analgesia is important. The patient is placed in the supine but slightly head-up position. Thus, when awake they may be able to observe their surroundings without the need to lift their head and body up, as that may worsen dizziness, nausea and vomiting.
Communication in recovery may be challenging, as the patient may be hard of hearing as a result of pre-existing pathology and/or mastoid bandages covering the ears.
Local anaesthesia
Dosing
An ‘x’ per cent solution contains 10‘x’ mg/ml. Therefore, 2 per cent lidocaine contains 20 mg/ml. A ‘1’ in ‘y’,000 solution contains + 1 mg in ‘y’ ml. Therefore, 1 in 80 000 adrenaline contains 1 mg in 80 ml. A 2–3 mg/kg dose of lidocaine is increased to 7 mg/kg when combined with adrenaline. A 2 mg/kg dose of bupivacaine (Marcaine™) is increased to 3 mg/kg when combined with adrenaline.
Practical application in ear surgery
Proper haemostasis is essential to optimise performance in otological surgery.
For both conscious sedation and GA, it is recommended that the anaesthetic technique includes LA around the auditory canal, conducted in a four-quadrant fashion, at the bony-cartilaginous junction, with lidocaine 2 per cent with adrenaline 1:100 000, or an equivalent. The post-auricular skin and region of the tragus are also injected if a post-auricular incision or tragal graft is required for the procedure (Figure 2).

Fig. 2. Infiltration of local anaesthetic at the bony-cartilaginous junction of the external ear canal (arrows).
Injecting an LA with adrenaline prior to scrubbing provides time for the vasoconstrictive properties to work. Xylocaine or bupivacaine will assist in reducing the anaesthetic load required throughout the case.
To further assist with haemostasis, the external auditory canal can then be gently packed with neurosurgical patties soaked in adrenaline (1:1000 or 1:10 000).
It is imperative to inject slowly under microscopic or endoscopic guidance with a 25 or 27 gauge needle, to minimise trauma, and to avoid haematomas or small blebs of the LA from collecting under the ear canal skin. Injection should continue until the entirety of the ear canal skin blanches.
As with all local injections, aspiration should be performed prior to injection to avoid intravascular complications and LA toxicity.
Positioning the patient with the head slightly elevated helps to reduce venous bleeding. Topical adrenaline is also of benefit if the surgeon encounters bleeding throughout the case. Irrigation with normal saline and clearing the field of blood before applying topical adrenaline is helpful to maximise benefit. Patience is required to allow time for the adrenaline to work before removing it from the surgical field.
Specific anatomical considerations
When injecting an LA in the setting of a tympanic membrane perforation, care should be taken to prevent xylocaine from entering the middle-ear space. Diffusion through the round window can result in severe vertigo. Diffusion over a dehiscent facial nerve in the middle-ear space can cause temporary facial paralysis.
Avoid injecting near the mastoid tip, as the facial nerve is superficial in this region and can be inadvertently anaesthetised, resulting in a transient facial paralysis.
Local anaesthesia with sedation
Anaesthesia can also be safely provided with sedation and LA.Reference Eddusriya, Goonasekera, Rajapakse, Rajapakse and Jayasooriya9 This requires good pre-operative selection and explanation to patients. Sedative agents such as midazolam (0.05–0.1 mg/kg) and ketamine (0.5–1 mg/kg) are administered intravenously prior to the infiltration of LA.
A survey conducted by Yung on patients undergoing middle-ear operations found that the most common discomforts were: noise during the operation (26.9 per cent of patients), anxiety (24 per cent), dizziness (14.8 per cent), backache (13.9 per cent), claustrophobia (9.3 per cent) and earache (1.9 per cent).Reference Yung1 Despite these discomforts, 89 per cent of patients preferred LA to GA for a similar procedure. Therefore, this technique can be used as an alternative where suitable.
Case study
This case study reflects anaesthesia practice at the Britain Nepal Otology Service (‘BRINOS’) ear camp in Nepal.
The delivery of anaesthetic services for major middle-ear surgery (e.g. modified radical mastoidectomy) in remote and unfamiliar surroundings poses a multitude of challenges. However, the delivery of safe, efficient (large numbers) and high-quality service (or as high-quality as can be delivered given the constraints) is an exemplar of teamwork of the highest order. It involves every member of the team (both trained and untrained, clinical and non-clinical). Everybody helps each other.
As a sole anaesthetist without the usual trained anaesthetic support team in attendance, the challenge begins with the set-up of the anaesthetic delivery system, and the laying out and stocking of anaesthetic equipment and drugs. This gives a unique insight as to what is essential to the delivery of safe anaesthesia. The avoidance of waste is essential given the constraints on stocks.
It is important to plan ahead. As such, good communication between all team members is essential.
The need to take into account environmental factors is something not familiar to most of us working in the UK. A reliable power supply is usually taken for granted; this may well not be the case, and the presence of capacitors to provide an uninterrupted power supply is essential for continued operating.
At the Britain Nepal Otology Service ear camp there were two LA tables (for myringoplasties, stapedectomies etc.) in the same operating theatre area as the GA table. One needs to be aware of what is going on in order to provide support, and assist in cases where intravenous drug administration is required or a GA conversion is needed for completion of the procedure. There is also a lack of resuscitation equipment (e.g. no defibrillator).
With most of our patients being young, fit and stoical, physiological and pathological derangements were rare. Supraglottic airway devices (laryngeal masks and i-gel®) were almost exclusively used.
The anaesthetic technique was based on a GA using intravenous induction with maintenance using a total intravenous technique, with or without muscle relaxation. This provided stable conditions, with the ability to manipulate blood pressure in order to provide a satisfactory operating field.
During the last camp, the use of a modified superficial cervical plexus block was introduced successfully with a resultant reduction in opioid use (again because of limited supply). This allowed a rapid recovery with little hangover (essential as there is no recovery staff, monitoring or oxygen).
The first case of the camp is always a challenge, but once under way, things tend to settle down and one usually regains a sense of calm. Reflection is important. Reviewing anaesthetic technique must be tempered with pragmatism: what is tried and tested and works is best continued. One also learns much about oneself, one's colleagues, and the importance of teamwork and camaraderie. The latter two factors provide much satisfaction, and make the hard work worthwhile and fun.
Conclusion
Anaesthesia for middle-ear surgery requires careful consideration of patient, anaesthetic, environment and surgical factors for a suitable, safe anaesthetic. In the low-resource setting, there are often additional challenges of language and environment; communication and planning are essential for a safe procedure.
Acknowledgement
Dr Kumar Panikkar, consultant in anaesthesia and intensive care (Stoke Mandeville and Wycombe General Hospitals), and volunteer for the Britain Nepal Otology Service (‘BRINOS’).
Competing interests
None declared