The clinical state of high risk of psychosis defines a condition characterised by attenuated psychotic symptoms, brief limited intermittent psychotic episode, genetic vulnerability or the presence of basic symptoms. Reference Fusar-Poli, Borgwardt, Bechdolf, Addington, Riecher-Rossler and Schultze-Lutter1 As the name suggests, these diagnostic criteria were originally developed to identify people at high risk of developing a psychotic disorder over time. Under this conceptualisation the condition would allow detection and treatment of a group at very high risk of developing a severe and full disorder longitudinally. This paradigm would fit the aims of indicated prevention in this group, Reference Mrazek and Haggerty2 who have up to 30% risk of developing psychosis, mostly schizophrenia spectrum disorders, Reference Fusar-Poli, Bechdolf, Taylor, Bonoldi, Carpenter and Yung3 within the following 2 years. Accordingly, preventive treatments primarily aim at reducing the risk associated with the condition and thus preventing the outcome. Reference Stafford, Jackson, Mayo-Wilson, Morrison and Kendall4,Reference Van der Gaag, Smit, Bechdolf, French, Linszen and Yung5 The ‘high risk’ paradigm does not explicitly require functional impairments as inclusion criteria, Reference Fusar-Poli, Carpenter, Woods and McGlashan6 with the exception of the genetic risk and deterioration subgroup, which however is traditionally small. On the other hand, over the past few years a competing paradigm has emerged. The ‘attenuated psychosis’ syndrome (APS) has been published in DSM-5. 7,Reference Woods, Walsh, Saksa and McGlashan8 The APS construct specifically requires patient distress or disability, which has not explicitly been part of the high-risk concept, although distress and disability are implicit in the symptom severity ratings that are required for the research diagnosis of high risk, Reference Woods, Walsh, Saksa and McGlashan8 defined as ultra-high risk (so not basic symptoms). In this sense the APS better resembles the clinical condition of angina pectoris, which is per se associated with signs and symptoms impairing the quality of life (QoL) and level of functioning of the individual. The APS diagnosis has been relegated to the research appendix of the DSM-5 because of lack of consensus among researchers on the validity of this category as a syndrome and for the inconclusiveness of data supporting its diagnostic reliability. Reference Schultze-Lutter, Schimmelmann, Ruhrmann and Michel9
One way to partially circumvent this controversial issue is to clarify the functional status of people at high risk at the time of their presentation to prodromal services and independently from their longitudinal outcomes. In fact, according to the DSM criteria, 7 an impairment of functioning along with significant distress are basic criteria for the conceptual validity of all psychiatric disorders, Reference Blumenthal-Barby10 differentiating a physiological trait or asymptomatic risk factor from a disorder and determining the patient's need for treatment: ‘mental disorders are usually associated with significant distress in social, occupational, or other important activities’. 7 A number of studies investigating functioning or QoL in people at high risk have been published in recent years. Surprisingly, to date no quantitative synthesis has been published regarding the functioning and QoL of such people when they are seeking help from prodromal clinics. The results are particularly controversial when people at high risk are compared with patients with established psychosis. Reference Addington, Penn, Woods, Addington and Perkins11–Reference Ruhrmann, Paruch, Bechdolf, Pukrop, Wagner and Berning14
Our first aim was to investigate validity of the high-risk state by addressing consistency and magnitude of baseline functioning and QoL in high-risk individuals compared with a healthy control group and people with a frank diagnosis of psychosis. We additionally investigated the impact of baseline difference in high-risk functioning on the longitudinal development of psychotic disorders.
Method
The main research hypothesis and the study protocol were decided a priori. We used a systematic search strategy to identify relevant articles. Two investigators (A.S. and A.A.) conducted a two-step literature search. As a first step the Web of Knowledge database (Thomson Reuters) was searched, incorporating both the Web of Science and Medline. The search was extended until December 2013, including abstracts in English language only. The electronic research adopted several combinations of the following keywords: “at risk mental state”, “psychosis risk”, “prodrome”, “prodromal psychosis”, “ultra high risk”, “functioning”, “quality of life” and name of the possible assessment instruments (see online supplement DS1 for details). The second step involved the implementation of an additional electronic search based on a manual search of the reference lists of the retrieved articles. Abstracts of articles identified through these two steps were then screened for the selection criteria, and articles surviving this screening were assessed for eligibility on the basis of a full-text reading. Discrepancies were resolved through consensus with a third author (M.R.). To achieve a high standard of reporting we adopted the Meta-analysis of Observational Studies in Epidemiology (MOOSE) checklist. Reference Stroup, Berlin, Morton, Olkin, Williamson and Rennie15
Selection criteria
Inclusion criteria for the first two meta-analyses, focusing on the difference between the groups in functioning (meta-analysis 1) and QoL (meta-analysis 2), were as follows:
-
(a) original article, written in English;
-
(b) inclusion of a sample at high risk (i.e. presence of attenuated psychosis symptoms, genetic risk and deterioration, brief limited and intermittent psychotic episode, basic symptoms) according to international standard definition; Reference Fusar-Poli, Borgwardt, Bechdolf, Addington, Riecher-Rossler and Schultze-Lutter1
-
(c) inclusion of a comparison group of healthy participants or patients with psychosis;
-
(d) cross-sectional study, cohort study or descriptive study reporting sufficient meta-analytical data on functioning.
Meta-analysis 3 focused on the difference in functioning between high-risk participants who made (HR-T) or did not make (HR-NT) a transition to psychosis at follow-up in descriptive longitudinal studies. Inclusion criteria (a) and (b) were the same as above, with an additional criterion that the article reported baseline data on functioning together with the longitudinal transition outcome at follow-up. Exclusion criteria were common to all analyses: articles were excluded if they were abstracts, pilot data-sets or reviews, failed to report enough data for meta-analysis or had overlapping data-sets. Specifically, in case of multiple publications deriving from the same study population, we selected the article reporting the largest and most recent data-set.
Recorded variables
Data extraction and quality assessment were independently performed by two investigators (A.S. and A.A.). Inconsistency and disagreements on quality rating were double-checked and resolved with a third author (M.R.). The following variables were recorded from each article: author, year of publication, quality criterion (see below), comparison group type (healthy participants or patients with established psychosis), epidemiological data of high-risk and control samples (baseline sample sizes, mean age, proportion of females), the high-risk diagnostic instrument adopted, the instrument employed to assess functioning and the level of functioning. The last variable was the primary outcome measure for the first meta-analysis. The following data on functioning were extracted: mean value and standard deviation of the mean in both the high-risk and comparison groups, direction of the difference and level of significance of the difference. Reference Rosenthal16 We additionally extracted data on QoL as defined by the mean of different psychometric instruments and used it as secondary outcome measure. If the data were reported for subgroups we merged the values (online Table DS1). For meta-analysis 3 we extracted baseline functioning in the HR-T and HR-NT groups as the primary outcome. Demographic data, publication year and duration of follow-up (months) were extracted finally to assess their putative moderator effect.
Quality assessment
Although quality assessments can be reliably conducted in meta-analyses of experimental studies their use in observational research is controversial, with no clear consensus on rating methods or their appropriate use in the analysis. Reference Juni, Witschi, Bloch and Egger17 We adapted the Newcastle–Ottawa Scale for the evaluation of non-randomised studies (www.ohri.ca/programs/clinical_epidemiology/oxford.asp). The scale evaluates the quality of observational studies, allocating a maximum of nine stars for the highest quality. This tool has been adopted in recent meta-analyses. Reference Mertz, Kim, Johnstone, Lam, Science and Kuster18
Statistical analysis
We performed three meta-analyses using Comprehensive Meta-Analysis Software version 2. Reference Borenstein M Hedges, Higgins and Rothstein19 When the same outcome was evaluated within the same study with more than one scale we retained just one measure according to a predefined order (see Method in online supplement DS1). As a measure of effect size in meta-analyses 1 and 2 Hedges' g was adopted, i.e. the difference between the functioning (or QoL) means of the comparison and high-risk groups, divided by the standard deviation and weighted for sample size, to correct for bias from small sample sizes. In meta-analysis 3 Hedges' g was employed to test differences in functioning between the HR-T and HR-NT groups. The influence of putative continuous moderators (year of publication, demographic variables, length of follow-up) was tested using meta-regression analyses, dividing the significance level (P = 0.05, two-tailed) by number of moderators tested to adjust for multiple comparisons. The slope of meta-regression line – β coefficient: direct (+) or inverse (−) – indicates the strength of the relationship between moderator and outcome. Meta-regressions were performed when at least ten studies were available for the preselected outcome of interest. We additionally performed a supplementary analysis using the cross-sectional studies employing the Global Assessment of Functioning (GAF). Furthermore, since the most recent studies adopting the Comprehensive Assessment of At-Risk Mental States (CAARMS) for high-risk state included functioning as a diagnostic criterion, Reference Schultze-Lutter, Schimmelmann, Ruhrmann and Michel9 a subgroup analysis was performed to control for this possible confounder. Further methodological details are available in online supplement DS1.
Heterogeneity, publication bias and sensitivity
Heterogeneity among study point estimates was assessed using Q statistics, Reference Paulson and Bazemore20 with the proportion of the total variability in the effect size estimates being evaluated with the I 2 index. Reference Lipsey and Wilson21 As meta-analysis of observational studies is supposed to be characterised by significant heterogeneity, random effect models were used. In general, random effect models are more conservative than fixed effect models, and appear to better address heterogeneity between studies and study populations, allowing for greater flexibility in parsing effect size variability. Moreover, they are less influenced by extreme variations in sample size. Reference Cooper, Hedges and Valentine22 The possibility of a publication bias in our study was tested with the Duval & Tweedie trim and fill method. Reference Duval and Tweedie23 This method imputes values estimated to be missing from the analysis (e.g. for publication bias) and re-estimates the effect size. If the conclusion of the meta-analysis remains unchanged following the trim and fill adjustment the results can be considered as robust. To further assess the robustness of the results, we performed sensitivity analyses by sequentially removing each study and rerunning all three meta-analyses. We also conducted a second sensitivity analysis for meta-analysis 2 excluding studies with quality ratings in the lowest quartile, to determine whether potential methodological weaknesses influenced meta-analytic estimates.
Results
For meta-analyses 1 and 2 electronic and manual search uncovered 1168 potential abstracts. After the first screening through abstract reading 226 full-text articles were downloaded for selection, of which 30 met the inclusion criteria as they were comparing functioning or QoL between high-risk participants and comparisons, accounting for a total of 3608 participants (meta-analysis 1: n = 3012, mean age 20.7 years, 38.8% female; meta-analysis 2: n = 945, mean age 23.7 years, 41.4% female; online Fig. DS1 (a) and (b)). There were no studies employing basic symptom criteria in the final database. For meta-analysis 3, electronic and manual search uncovered 1181 potential abstracts. After the first screening through abstract reading 244 full-text articles were downloaded for selection; of these, 10 longitudinal studies reporting baseline functioning in the transition and non-transition groups were eventually included (mean length of follow-up 28.3 months, n = 654; mean age at baseline 19.1 years, 43.5% female; online Fig. DS1 (c)). The details of the final database are reported in online Table DS2.
Functioning in high-risk individuals
Comparison with healthy control group
There was a large and significant impairment in functioning across the high-risk group compared with the healthy control group, with small 95% confidence intervals indicating the precision of the estimate (Hedges' g= −3.01, 95% CI −3.68 to −2.34, P<0.001, n = 18; Fig. 1(a)). The Duval & Tweedie trim and fill procedures found no missing study (random model applied), suggesting absence of publication bias. There was considerable heterogeneity across the included studies (Q = 497.4, I 2 = 96.6%, d.f. = 17, P<0.001) but the direction of the effect was consistent and significant for each study. No study accounted for more than 5.9% of the overall effect size. Meta-regression analysis adjusted for multiple comparison found that a proportion of females in the healthy control group was correlated with the magnitude of the effect size (β = −2.61, 95% CI −3.75 to −1.48, P<0.001, Q = 20.5, n = 15). Conversely, there was no association between level of functioning and high-risk gender, high-risk or healthy control group age or publication year. The sensitivity analysis computing after removing each study and the studies in the lower quartile of quality rating confirmed our findings with no significant change.
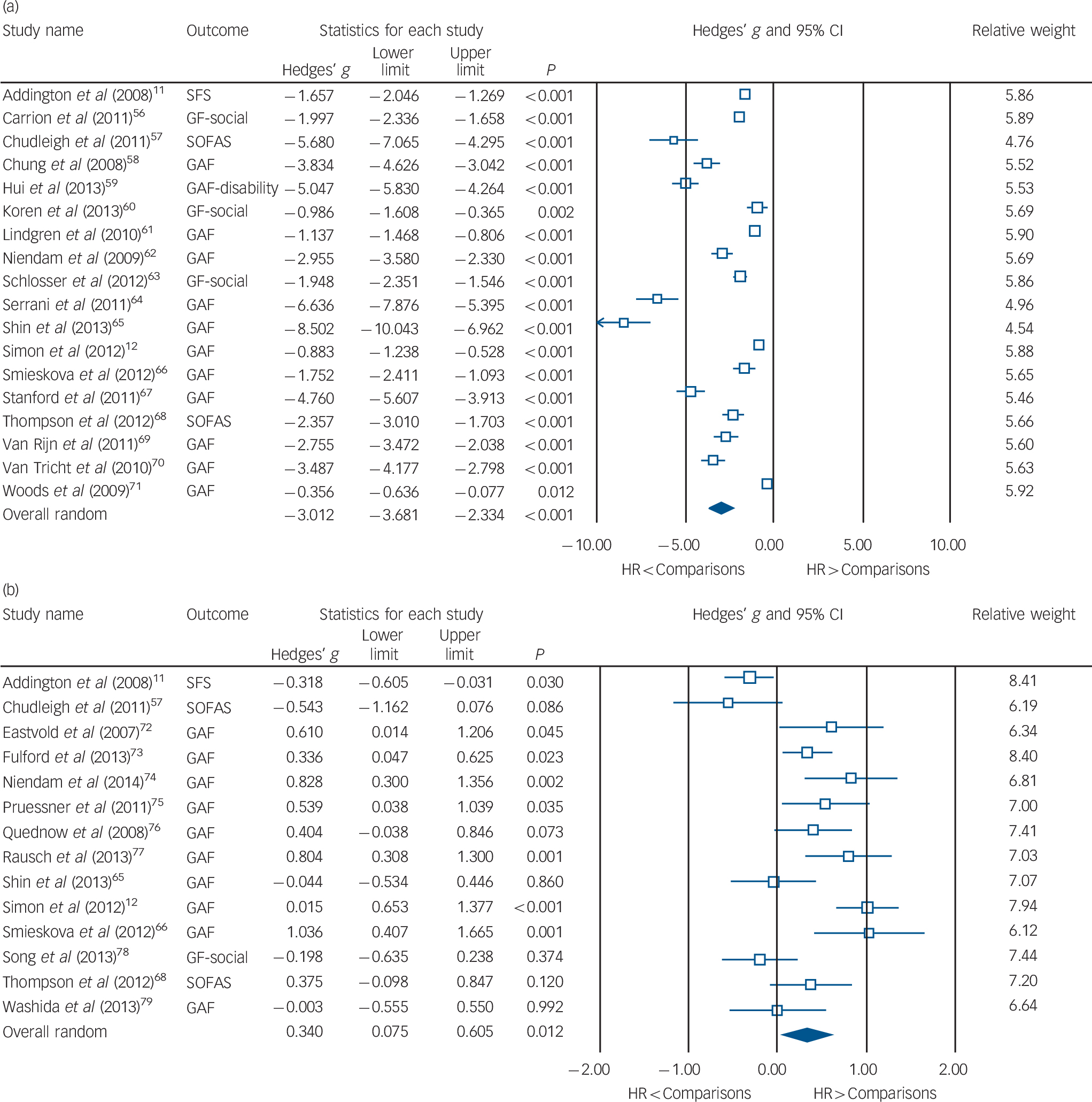
Fig. 1 Functional impairment: forest plots of meta-analysis 1. The large effect size of the subgroup analysis indicated (a) lower functioning of the high-risk group v. the healthy control group and (b) a moderate standardised difference in functioning between the high-risk group and the psychosis group.
GAF, Global Assessment of Functioning; GF-social, Global Functioning – social scale; HR, high risk; SOFAS, Social and Occupational Functioning Assessment Scale; SFS, Social Functioning Scale.
Comparison with the psychosis group
People in the high-risk group were less impaired on functional status than patients with frank psychosis. The magnitude of this effect was small to moderate (Hedges' g= 0.34, 95% CI 0.07 to 0.60, P = 0.012, n = 14; Fig. 1(b)), with large confidence intervals indicating imprecision. There was no publication bias. There was significant heterogeneity across studies (Q = 63.3, I 2 = 79.5%, d.f. = 13, P<0.001). Meta-regression analyses adjusted for multiple comparisons revealed better functioning in women in both high-risk (β = −1.76, 95% CI −3.03 to −0.49, P = 0.007, Q = 7.4, n = 14) and psychosis group (β = −2.43, 95% CI −3.61 to −1.25, P<0.001, Q = 16.3, n = 14) comparisons (online Fig. DS2). Conversely, there was no association in either group with age or with publication year. These results were confirmed by sensitivity analyses. Results of the supplementary analyses investigating the mean GAF scores of the three comparison groups, and the possible effect of the high-risk diagnostic tool (i.e. CAARMS v. Structured Interview for Prodromal Symptoms, SIPS), are reported online (Figs DS3 and DS4).
Quality of life
Meta-analysis 2 showed that the high-risk group had poorer QoL than the healthy control group (Hedges' g= −1.75, 95% CI −2.83 to −0.67, P = 0.001, n = 4; Fig. 2(a)). Furthermore, we found no difference in QoL between the high-risk and psychosis groups (Hedges' g= 0.02, 95% CI −0.64 to 0.67, P = 0.958, n = 3; Fig. 2(b)). The heterogeneity in the subgroup analysis was considerable (high-risk v. healthy control group: Q = 91.8, I 2 = 96.7%, d.f. = 3, P<0.001; high-risk v. psychosis group: Q = 16.1, I 2 = 87.6%, d.f. = 2, P<0.001); however, given the small number of studies, we did not perform meta-regression analyses. The sensitivity analysis computing after removing each study confirmed our findings, with no significant change.

Fig. 2 Quality of life: forest plots of meta-analysis 2. The subgroup analysis indicated that quality of life of the high-risk group was worse than that of the healthy control group (a) but similar to that of the psychosis group (b).
HR, high risk; MANSA, Manchester Short Assessment of Quality of Life; MSQoL, Modular System for Quality of Life; QLS, Quality of Life Scale.
Functioning and psychosis transition
There was meta-analytical difference in baseline level of functioning between the HR-T and HR-NT groups (mean follow-up 28.9 months, s.d. = 16.0). The magnitude of the effect was moderate, with those in the HR-T group showing poorer baseline functioning than the HR-NT group (Hedges' g= 0.43, 95% CI 0.17 to 0.68, P = 0.001, n = 10; Fig. 3). The trim and fill procedure showed that the result was robust against publication bias. The heterogeneity between studies was moderate (Q = 20.0, I 2 = 54.9%, d.f.= 9, P= 0.018). Meta-regressions adjusted for multiple comparisons revealed a significant correlation with publication year (β = −0.10, 95% CI −0.17 to −0.03, P = 0.005, Q = 7.8, n = 10), but no association with length of follow-up (P = 0.121), gender of participants (P = 0.651) or age (P = 0.254). The sensitivity analysis computing after removing each study confirmed our findings with no significant change.
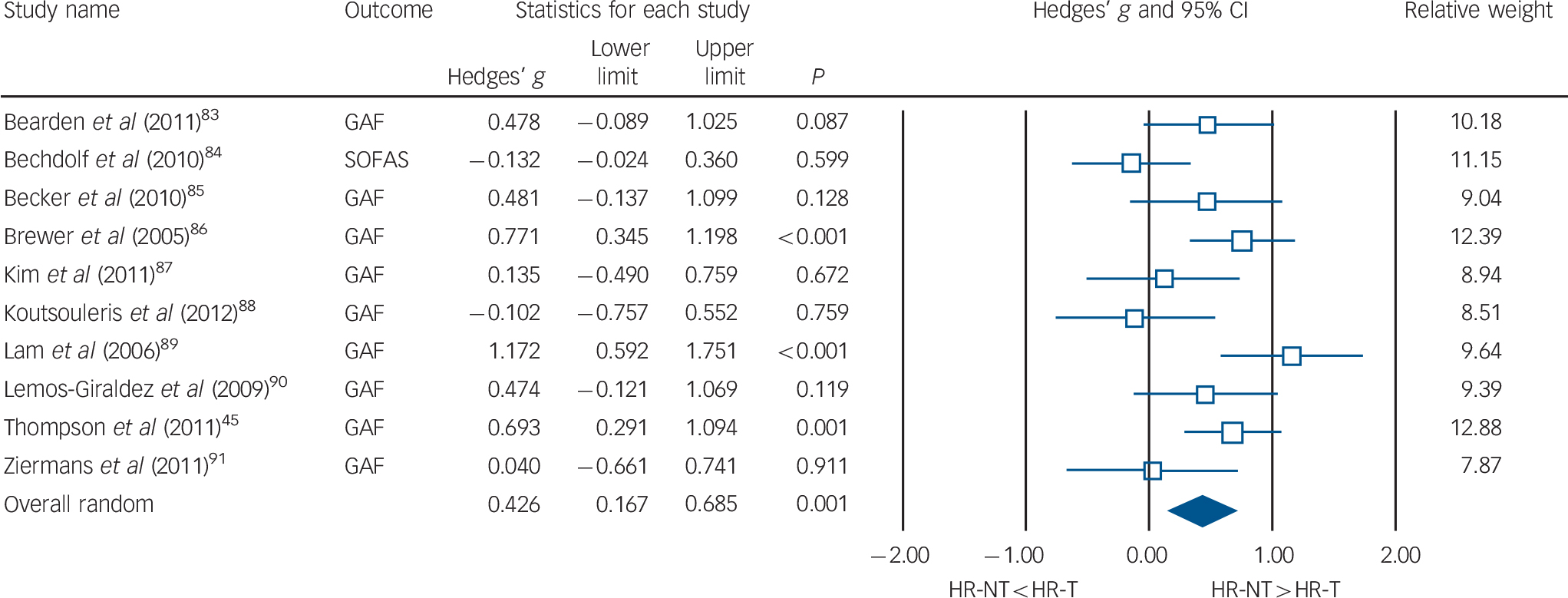
Fig. 3 Baseline functional impairment and transition to psychosis: forest plot of meta-analysis 3. Participants at high risk who developed psychosis during the follow-up period had poorer baseline functioning than participants who did not.
GAF, Global Assessment of Functioning; HR-NT, high risk, no transition to psychosis; HR-T, high risk, transition to psychosis; SOFAS, Social and Occupational Functioning Assessment Scale.
Discussion
People at high risk of psychosis (defined on the basis of ultra-high risk criteria) had a statistically significant impairment in global functioning that was very large compared with a healthy control group, but only small to moderate when compared with patients with psychosis. Within the high-risk group, lower baseline level of global functioning predicted the later onset of psychosis. Impairments of QoL in the high-risk group were similar to those observed in the psychosis group. The results were robust and not affected by publication bias.
The results of our meta-analysis are important for research and clinicians working in the field of psychosis prevention because there is no consensus with respect to the functional status of people at high risk of psychosis. For example, some authors argue that such people are not at all dysfunctional, as their signs and symptoms represent ‘normal developmental processes’ or expressions of psychosis vulnerability that are common in the general population. Reference Castle24 These authors also suggested that help-seeking is only a behaviour not suggestive of functional impairments and questioned whether these individuals actually need treatment, Reference Castle24 concluding that ‘it is not appropriate to treat high-risk people before the psychosis onset’. Reference Castle25 To our knowledge this is the first ever meta-analysis clearly addressing these speculations and investigating the functional status of high-risk participants compared with healthy control and psychosis groups.
Functional impairment
We clearly found that functioning of people at high risk was strongly impaired compared with the healthy control group but only modestly impaired compared with people with psychosis. These impairments may have been present for a long period prior to referral to high-risk services. Reference Fusar-Poli, Meneghelli, Valmaggia, Allen, Galvan and McGuire26 Our supplementary analysis focusing only on studies employing the GAF indicated a mean score of about 79 for the healthy control group, 50 for the high-risk group and 45 for the psychosis group. This pattern suggests that the functional level in people at high risk is closer to that observed in people with psychosis as opposed to that observed in healthy individuals. This pattern is further supported by the meta-analysis of the QoL, which found no significant difference between the high-risk and psychosis groups and again a significant reduction in QoL compared with the healthy control group. It is relevant that functional impairment as well as QoL reported for the high-risk group was observed at the initial assessment in early detection centres before any focused intervention was initiated. Impairments in functioning and QoL are therefore a key feature of the high-risk state, at least as defined with the ultra-high risk criteria (we found no basic symptom studies eligible for the current meta-analysis). Since QoL in the high-risk group was similar to that observed in patients with psychosis, it is possible to argue that severe functional impairment may lead to self-stigmatising by high-risk patients independently of any diagnostic label. Reference Ruhrmann, Klosterkotter, Bodatsch, Nikolaides, Julkowski and Hilboll27 To better understand the magnitude of the functional impairment of the high-risk state, it can be qualitatively compared with that of other psychiatric disorders (Fig. 4).
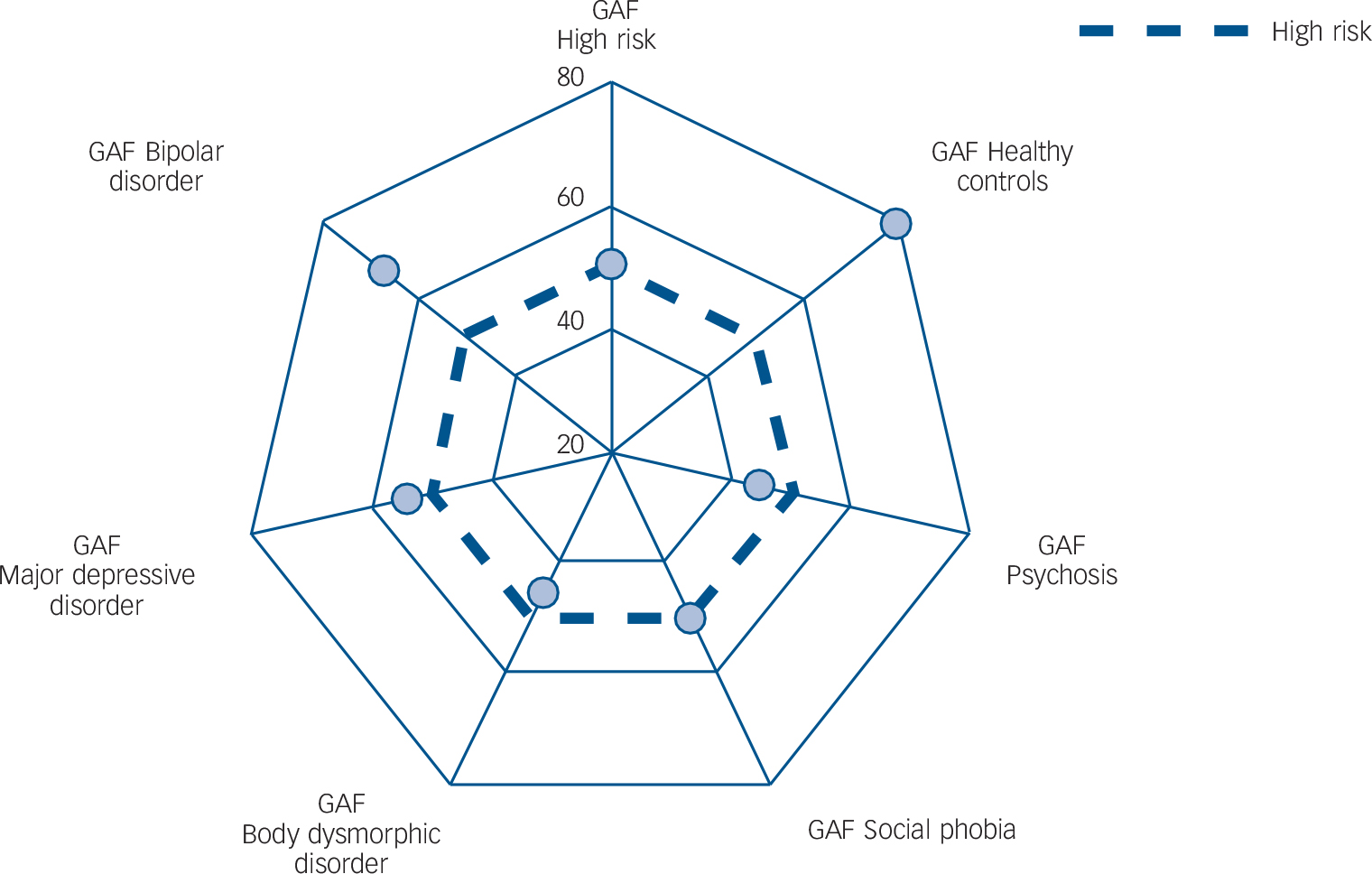
Fig. 4 Qualitative comparison of Global Assessment of Functioning (GAF) scores in different psychiatric conditions.
The plot displays the result of our supplementary meta-analysis of GAF point estimates for the high-risk group (defined with ultra-high risk criteria), the healthy control group and the psychosis group, which has been qualitatively compared with GAF estimates in bipolar disorder (taken from Hajek et al), major depressive disorder (from Schaub et al), body dysmorphic disorder (from Phillips et al) and social phobia (from Kelly et al). Reference Hajek, Slaney, Garnham, Ruzickova, Passmore and Alda52–Reference Kelly, Dalrymple, Zimmerman and Phillips55 The dashed line represents the high-risk group mean GAF score, to facilitate visual comparison.
Although such a comparison should be interpreted cautiously as it is not based on original data, on a qualitative basis the graph indicates that the point estimate of the global functioning in the high-risk group is lower than those observed in bipolar disorder, and similar to that of major depressive disorders and social phobia. This is the first meta-analytical evidence that high-risk individuals are ‘probably at risk but certainly ill’, as previously advocated. Reference Ruhrmann, Schultze-Lutter and Klosterkotter28 The findings of large functional impairments in the high-risk group clearly contradict the speculative assumption that they represent normal developmental phenotypes and are not in need of care. Conversely, in synopsis of the results of the meta-analyses and the qualitative placement of the observed GAF scores shown in Fig. 4, it seems strongly justifiable to conclude that the functional state observed in those meeting high-risk criteria calls not only for prevention of a future transition to psychosis, but also for treatment of the current mental state and problems.
Comorbidity
It may be argued that functional impairment in those at high risk of psychosis is secondary to comorbid disorders diagnosed in this group. There is evidence that affective comorbidities are highly prevalent in these individuals, Reference Salokangas, Ruhrmann, von Reventlow, Heinimaa, Svirskis and From29 affecting psychopathology, neurobiology and baseline functioning. Reference Fusar-Poli, Nelson, Valmaggia, Yung and McGuire30,Reference Modinos, Allen, Frascarelli, Tognin, Valmaggia and Xenaki31 However, in an earlier meta-analysis we found comorbid affective disorders to be present in less than half of the high-risk group (comorbid depressive disorder 41%, anxiety disorder 15%). Reference Fusar-Poli, Nelson, Valmaggia, Yung and McGuire30 Consequently, the functional and QoL impairment observed in the high-risk group could not entirely be secondary to the presence of affective comorbidities. The European Prediction of Psychosis (EPOS) study estimated the impact of both high-risk and depressive psychopathology on baseline GAF scores, using the Beck Depression Inventory and the SIPS as independent variables; step-wise linear regression retained SIPS-positive and SIPS-negative scores only, explaining 14.9% of variance and thus indicating that GAF scores were predominantly determined by deterioration of role functioning. Reference Ruhrmann, Schultze-Lutter, Salokangas, Heinimaa, Linszen and Dingemans32 On the other hand, even if comorbid symptoms fulfilling the thresholds for certain DSM or ICD disorders had an impact on the GAF ratings, these scores could be interpreted as a true expression of the high-risk state: such comorbid symptoms could well be considered as part of the high-risk state, in line with retrospective findings indicating that prevalence of depressive mood at the time of psychosis onset is 83%, Reference Hafner, Maurer, Trendler, an der Heiden, Schmidt and Konnecke33 and with phenomenological evidence of affective dysregulation at the core of psychosis liability. Reference Mishara and Fusar-Poli34 Affective symptoms may thus be part of the high-risk state and might be expression of an early, mild stage of the same neurobiological process that causes psychosis. Reference Hafner, Maurer, Trendler, an der Heiden, Schmidt and Konnecke33
Specificity and sensitivity
We also supported the notion that functional impairment may help in enriching the risk (specificity) of high-risk samples. Reference Fusar-Poli and Van Os35 In fact, as compared with ultra-high-risk individuals, Reference Kempton, Bonoldi, Valmaggia, McGuire and Fusar-Poli36 short-term transition risk in individuals with psychotic-like symptoms but good functioning is extremely low (about 1.2% within 2 years). Reference Kaymaz, Drukker, Lieb, Wittchen, Werbeloff and Weiser37 However, it is possible that rigorous functioning criteria might enrich the high-risk sample but at the cost of sensitivity. Another study investigating the prevalence of high-risk symptoms in a community sample aged 11–13 years found the proportion of participants meeting CAARMS high-risk criteria declined from 7.7% to 0.9% when a 30% decrease of functioning was considered a criterion. Reference Kelleher, Murtagh, Molloy, Roddy, Clarke and Harley38 Thus, at least at the population level, adding this functioning criterion may lead to an immense loss of sensitivity. A corresponding finding was reported from the Personal Assessment and Crisis Evaluation (PACE) 400 study. Reference Nelson, Yuen, Wood, Lin, Spiliotacopoulos and Bruxner39 It has still to be elucidated in longitudinal follow-up studies whether there is a criterion leading to a better balance of sensitivity and specificity; however, risk stratification might overcome this problem. Reference Ruhrmann, Schultze-Lutter, Salokangas, Heinimaa, Linszen and Dingemans32 Furthermore, even without transition to psychosis, functional decline may constitute an outcome of the high-risk state with a comparable clinical significance. Thus, besides a loss of sensitivity, defining impaired functioning as an obligatory entry criterion for high-risk status may result in missing the main goal of prevention, i.e. lowering the huge personal and socioeconomic burden of the disease related to impaired functioning. Reference Gustavsson, Svensson, Jacobi, Allgulander, Alonso and Beghi40 Future studies may therefore have to find a balance between sufficient risk enrichment in terms of transition to psychosis and sufficient sensitivity in terms of functional outcome.
The need for care
Besides these speculations, our meta-analysis provides conclusive and consistent evidence that people at high risk are truly in need of care. Our analysis found no evidence of publication bias, and all the sensitivity analyses performed confirmed our findings. We investigated factors modulating functional level in high-risk participants. A small proportion of the observed heterogeneity was explained by gender, suggesting better functional level in women with psychosis. Such a result is in line with available studies in the psychosis spectrum disorders reporting higher functional levels in women than in men. Reference Grossman, Harrow, Rosen and Faull41
Our longitudinal meta-analysis revealed that high-risk individuals who later developed psychosis had poorer functioning at baseline. This finding is not new, Reference Velthorst, Nelson, Wiltink, de Haan, Wood and Lin42 and is in line with the significant predictive value of high-risk functional impairment towards transition that has been reported in large independent samples. Reference Ruhrmann, Schultze-Lutter, Salokangas, Heinimaa, Linszen and Dingemans32,Reference Cannon, Cadenhead, Cornblatt, Woods, Addington and Walker43–Reference Thompson, Nelson and Yung45 Some authors support the idea of high risk as a continuum towards psychosis, marked by a change in functioning and course of thinking. Reference Cannon, Cadenhead, Cornblatt, Woods, Addington and Walker43 These results may have both clinical and research implications. High-risk samples could be stratified at baseline on the basis of their functional level and focused interventions or experimental trials could be individualised accordingly. Additionally, since most high-risk participants received at least in part some active treatment, our longitudinal results are in line with reports of low efficacy of preventive interventions on social functioning in these people. Reference Van der Gaag, Smit, Bechdolf, French, Linszen and Yung5 In this analysis we found a significant modulating effect for year of publication, suggesting that in the most recent studies the difference in functioning between the two transition groups decreased. This can be interpreted as the consequence of changes in recruitment strategies of prodromal clinics, with inclusion of less functionally impaired patients in the most recent years. Reference Fusar-Poli, Borgwardt, Bechdolf, Addington, Riecher-Rossler and Schultze-Lutter1 Overall, when interpreting the impact of baseline functioning on transition outcomes, it is important to note that psychosis is just one possible outcome of the high-risk state; remission, transition to a non-psychotic disorder and persistence of the high-risk state account for the majority of outcomes at follow-up. Reference Fusar-Poli, Borgwardt, Bechdolf, Addington, Riecher-Rossler and Schultze-Lutter1 Our analysis was unable to test the impact of baseline level of functioning on these outcomes. Functional status, on the other hand, could be considered as a good indicator of broader clinical outcome also in patients who will subsequently develop psychosis. Reference Fusar-Poli, Borgwardt, Bechdolf, Addington, Riecher-Rossler and Schultze-Lutter1,Reference Fusar-Poli and Van Os35
Study limitations
Some limitations need to be acknowledged. First, the concept of functional impairment had some intrinsic conceptual caveats. Most of the scales adopted, especially the GAF, do not provide a clear distinction between functioning and symptoms. Reference Ustun and Kennedy46 However, the vast majority of studies of the high-risk state published to date have used the GAF as a standard measure of functioning. The Social and Occupational Functioning Assessment Scale (SOFAS) has been developed to overcome this issue. Unlike the GAF, which includes not only social and occupational performance but also symptoms as a dimension of functioning, the SOFAS aims to assess functioning without the influence of the patient's symptoms. Reference Samara, Engel, Millier, Kandenwein, Toumi and Leucht47 However, both scales have strong negative correlations with the Clinical Global Impression and the Positive and Negative Syndrome Scale. Reference Samara, Engel, Millier, Kandenwein, Toumi and Leucht47 Further development in the field may imply the use of psychometric instruments powered to disentangle these two overlapping domains. Another limitation is that we did not attempt to acquire unpublished data. Yet another is that in both subgroup analyses a large part of the heterogeneity remained unexplained. Differences in sampling procedures and assessment measures could be some of the putative moderators that further studies need to take into account to increase the generalisability of findings. Also, the quality of the studies included may have affected interpretation of the results: only half of the studies used a matched (i.e. at least by age) comparison group (see online Table DS3). Another potential limitation is that the researchers assessing functioning and QoL were masked to case–comparison allocation in only a minority of studies. However, our sensitivity analysis showed no effect of quality of studies on the meta-analytical estimates. Furthermore, given conceptual and pragmatic differences between the high-risk and DSM-5 paradigms, Reference Fusar-Poli, Carpenter, Woods and McGlashan6 and given the lack of generalisability of high-risk research to the general population, Reference Schultze-Lutter, Michel, Ruhrmann and Schimmelmann48 our findings cannot be directly used to support the validity of the APS diagnosis. Our results support conceptual validity of the high-risk state, i.e. correctly distinguishing between disorder and normality, Reference Wakefield49 rather than its construct validity. Conversely, DSM-5 criteria for a mental disorder focus on construct validity, requiring that the disorder in question is distinct from other disorders, has familial aggregation, presence in diverse populations and environmental risk factors, has concurrent validators such as cognitive and temperament correlates, biological markers and a certain comorbidity profile, and has predictive validity with respect to diagnostic stability, predictability of the course of illness, and response to treatment. Reference Epperson, Steiner, Hartlage, Eriksson, Schmidt and Jones50 Conceptual and construct validity are independent. Reference Wakefield49 Although the high-risk state may encompass different comorbid disorders, Reference Fusar-Poli, Nelson, Valmaggia, Yung and McGuire30,Reference Modinos, Allen, Frascarelli, Tognin, Valmaggia and Xenaki31 and thus lack full construct validity, it can be conceptually valid since it encompasses only disorders. However, the same arguments can be used to question construct validity of affective disorders, given their high co-occurrence during first episodes of psychosis. Reference Hafner, Maurer, Trendler, an der Heiden, Schmidt and Konnecke33 Indeed, satisfying construct validity has as yet not been achieved even for many other hitherto encoded mental disorders. A full discussion of these issues is beyond the scope of the current investigations and has been critically presented in other recent papers. Reference Fusar-Poli, Carpenter, Woods and McGlashan6,Reference Wakefield51
Clinical implications
The high-risk state (defined with ultra-high risk criteria) is characterised by consistent and serious impairments of functioning and reduction of QoL that seem to be similar to those in other coded psychiatric disorders. These impairments call not only for prevention of a future transition to psychosis and functional deterioration, but also for treatment of the current disorder.
Funding
This work was supported by the Department of Psychosis Studies, King's College London, Institute of Psychiatry, Psychology and Neuroscience. M.R., E.C. and P.P. were also supported by the University of Pavia; M.B. was also supported by the Sapienza University of Rome.







eLetters
No eLetters have been published for this article.