Bullying victimization – abuse perpetrated by same age peers with a power differential that impedes victims from defending themselves (Olweus, Reference Olweus2013) – is associated with negative adult mental health (e.g., depression, anxiety suicidal ideation; Arseneault, Reference Arseneault2018; Moore et al., Reference Moore, Norman, Suetani, Thomas, Sly and Scott2017; Stapinski et al., Reference Stapinski, Bowes, Wolke, Pearson, Mahedy, Button and Araya2014), social and economic outcomes (Takizawa et al., Reference Takizawa, Maughan and Arseneault2014). Shields and Cicchetti (Reference Shields and Cicchetti2001) identified bullying victimization in school as being linked to earlier child maltreatment (see also Indias et al., Reference Indias, Arruabarrena and De Paúl2019; Lereya et al., Reference Lereya, Copeland, Costello and Wolke2015; Radford et al., Reference Radford, Corral, Bradley and Fisher2013). Delineating why child maltreatment is associated with bullying victimization may help identify new targets for prevention to reduce the negative sequelae of these experiences. In this regard, childhood neuro-developmental conditions (NDCs) such as attention-deficit/hyperactivity disorder (ADHD) and autism spectrum disorder (ASD) represent an important focus for study. This is because NDCs are associated with both bullying victimization and child maltreatment (Dinkler et al., Reference Dinkler, Lundström, Gajwani, Lichtenstein, Gillberg and Minnis2017; Langevin et al., Reference Langevin, Marshall, Wallace, Gagné, Kingsland and Temcheff2021; Mayes et al., Reference Mayes, Calhoun, Baweja and Mahr2015; Ouyang et al., Reference Ouyang, Fang, Mercy, Perou and Grosse2008; Rowley et al., Reference Rowley, Chandler, Baird, Simonoff, Pickles, Loucas and Charman2012; Törn et al., Reference Törn, Pettersson, Lichtenstein, Anckarsäter, Lundström, Gumpert and Halldner2015).
There are two plausible mechanisms linking NDCs to bullying victimization and maltreatment. The first sees both maltreatment and bullying victimization as two related effects of a common underlying cause – the pre-existing presence of NDCs. The second sees early maltreatment as contributing to later neurodevelopmental problems which then drive bullying victimization. In both models, child effects drive the link between NDCs and bullying victimization; the behavior of children with NDCs, marked as they are by social skills deficits and/or emotional and behavioral regulation problems, evoke a hostile reaction from peers (Fogleman et al., Reference Fogleman, Slaughter, Rosen, Leaberry and Walerius2019; Hellström, Reference Hellström2019; Jawaid et al., Reference Jawaid, Riby, Owens, White, Tarar and Schulz2012). The two models, however, differ with regard to the causal role of maltreatment in the emergence of NDCs. In the first, the sort of evocative processes linking NDCs to bullying victimization by peers also drive the experience of maltreatment: Maltreatment, although correlated is not causally related to bullying victimization. This type of NDC-evoked maltreatment is most likely to be expressed as reactive types of physical and emotional abuse by parents rather than neglect. In line with this model abuse is reported more often with children with NDCs than is neglect (see Hellström, Reference Hellström2019, for review). In the second model, maltreatment is not seen as a parental reaction evoked by pre-existing NDCs, but rather as potent influence on brain development creating risks for NDCs which later evoke bullying victimization: Maltreatment and bullying victimization are causally linked via the intervening emergence of NDCs. There are a number of lines of evidence supporting the hypothesis that maltreatment, in particular neglect, has the power to negatively impact brain development in ways that could increase the risk for NDCs. Early deprivation and neglect deprives the brain of the necessary and developmentally expected levels of stimulation required for its normal development (De Bellis, Reference De Bellis2005; McLaughlin et al., Reference McLaughlin, Sheridan and Nelson2017). Early severe neglect impacts brain function (reduced glucose metabolism) and cortical connectivity, in ways hypothesized to underlie the sequalae of neurodevelopmental and socioemotional problems following early neglect (Chugani et al., Reference Chugani, Behen, Muzik, Juhász, Nagy and Chugani2001; Eluvathingal et al., Reference Eluvathingal, Chugani, Behen, Juhász, Muzik, Maqbool, Chugani and Makki2006). Changes in prefrontal white matter structure (Hanson et al., Reference Hanson, Adluru, Chung, Alexander, Davidson and Pollak2013) and smaller superior-posterior cerebellar lobes’ volume (Bauer et al., Reference Bauer, Hanson, Pierson, Davidson and Pollak2009) mediated the neurocognitive deficits experienced following early neglect. At a neuro-cognitive level these effects are seen in impaired executive function, social cognition, working memory, and language skills – all characteristic of NDCs (McLaughlin et al., Reference McLaughlin, Sheridan, Gold, Duys, Lambert, Peverill and Pine2016; Milojevich et al., Reference Milojevich, Norwalk and Sheridan2019; Sheridan et al., Reference Sheridan, Peverill, Finn and McLaughlin2017). Such deficits in working memory and inhibition (Tibu et al., Reference Tibu, Sheridan, McLaughlin, Nelson, Fox and Zeanah2016) and reduced cortical thickness in the prefrontal cortex (McLaughlin et al., Reference McLaughlin, Sheridan and Lambert2014) were associated with severe early neglect and NDCs, particularly ADHD symptoms (Mackes et al., Reference Mackes, Golm, Sarkar, Kumsta, Rutter, Fairchild and Sonuga-Barke2020).
In the current paper, we explore the plausibility of this second model by examining the longitudinal reciprocal effects of NDCs and bullying victimization in childhood and adolescence as a function of early institutional deprivation and their impact on adult mental health and functional outcomes. Early childhood parental neglect has been directly associated with both mental health difficulties and functional impairment in adulthood (Sweeting et al., Reference Sweeting, Garfin, Holman and Silver2020). This association has been further characterized by the mediating effect of bullying victimization on the association between child maltreatment (within the family) and mental health difficulties (Banny et al., Reference Banny, Cicchetti, Rogosch, Oshri and Crick2013; Lereya et al., Reference Lereya, Copeland, Costello and Wolke2015; Macalli et al., Reference Macalli, Orri, Tzourio and Côté2021; Wang, Reference Wang2020). Kim and Cicchetti (Reference Kim and Cicchetti2010) showed the effects of specific maltreatment types, including neglect, on later psychopathology through emotion dysregulation and negative peer relations. However, these pathways have not been examined as a function of neglect resulting from early institutional deprivation, particularly in conjunction with the mediating effects of NDCs. To do this, we used data from the English and Romanian Adoptees (ERA) study which has tracked the development of children who experienced up to 43 months of severe neglect in the form of global deprivation in Romanian orphanages in the 1980s, around the time of the fall of the Communist regime, before being adopted by UK families. The conditions in the institutions were characterized by high levels of psychosocial deprivation and neglect, whereby children received minimal attention and care from staff and were engaged in extremely limited social or cognitive stimulation. Crucially for the current paper, adoptees typically entered the institutions in the first few weeks of life and at the time of adoption, experienced an abrupt and precisely timed change from a time-limited period of maltreatment (in this case institutional deprivation) into a well-functioning and well-resourced family. This situation created a natural experiment whereby the effects of neglect could be studied unconfounded by the ongoing adversity and familial risk for NDCs that often complicate interpretation of studies on victimization and adversity in biological families. Furthermore, parenting in the adopted homes was universally positive with no evidence of post-adoption maltreatment (Castle et al., Reference Castle, Beckett, Rutter and Sonuga-Barke2010).
In the ERA, extended periods of severe deprivation (at least greater than 6 months duration) led to distinctive pattern of NDCs with substantially elevated levels of clinically significant ADHD, ASD and Disinhibited Social Engagement – a pattern of inappropriate over familiarity with strangers (DSE; Kennedy et al., Reference Kennedy, Kreppner, Knights, Kumsta, Maughan, Golm and Sonuga-Barke2017; Sonuga-Barke et al., Reference Sonuga-Barke, Kennedy, Kumsta, Knights, Golm, Rutter and Kreppner2017). The distinctive patterns, their size and their strong association with deprivation duration, as well as the fact that the timing of placement was largely dependent on circumstances on the ground in Romania at the time of regime change make it unlikely that these problems were caused by preinstitutional risks or adoption selection factors. This strengthens the inference that they were to a considerable degree due to exposure to neglect while in institutional care. Furthermore, although there was little evidence of general behavioral and emotional problems in childhood, a late emergence of mental health problems including depression and anxiety occurred in early adulthood (Golm et al., Reference Golm, Maughan, Barker, Hill, Kennedy, Knights and Sonuga-Barke2020; Pitula et al., Reference Pitula, Thomas, Armstrong, Essex, Crick and Gunnar2014; Sonuga-Barke et al., Reference Sonuga-Barke, Kennedy, Kumsta, Knights, Golm, Rutter and Kreppner2017). Crucially, evidence was recently reported that the pathway between early deprivation and mental health problems was mediated by early emerging NDCs (Golm et al., Reference Golm, Maughan, Barker, Hill, Kennedy, Knights and Sonuga-Barke2020). Here we build on these findings to longitudinally model the direct and indirect pathways from early deprivation to mental health in young adulthood through bullying victimization. We will explore the specific roles of the three deprivation-related NDCs identified in ERA – ADHD, ASD, and DSE.
To date no studies have assessed the reciprocal effects between deprivation-related neuro-developmental problems and bullying victimization over time or studied the specific effects of different NDCs on bullying victimization. There is exploratory data suggesting ADHD symptoms in kindergarten mediate the association between early severe neglect due to institutional care with bullying victimization in kindergarten (Pitula et al., Reference Pitula, DePasquale, Mliner and Gunnar2019). However, in that study, both ADHD symptoms and peer problems were measured at the same timepoint, limiting the ability to make inference about the causality and directionality of that association. Two other studies reported on the effect of disturbances in attachment following adoption from placement (e.g., foster care or orphanage). Specifically, DSE at age 5 predicted bullying victimization in kindergarten (DePasquale et al., Reference DePasquale, Lawler, Koss and Gunnar2020) and reactive attachment disorder symptoms at the time of adoption predicted bullying victimization at age 9–15 years (Raaska et al., Reference Raaska, Lapinleimu, Sinkkonen, Salmivalli, Matomäki, Mäkipää and Elovainio2012). Together, these studies provide evidence for potential risk pathways from early deprivation to bullying victimization through deprivation-related neuro-developmental and attachment problems.
Objectives and hypotheses
The overall objective of the study was to characterize direct and indirect pathways from early institutional deprivation to later mental health and functional outcomes as mediated by bullying victimization and NDCs in the child and adolescent years. Although we know that NDCs are important mediators from early institutional deprivation to mental health difficulties in young adulthood (Golm et al., Reference Golm, Maughan, Barker, Hill, Kennedy, Knights and Sonuga-Barke2020), our aim was to test those pathways alongside bullying victimization. In this study we integrate several developmental findings to test a comprehensive developmental cascade model following early institutional deprivation. Our specific hypothesis is that neglect within depriving institutions (i.e., outside the family) occurring in the earliest months of life before the emergence of NDCs (and therefore unlikely to be evoked by them) increases the likelihood of bullying victimization; an effect mediated by NDCs – with this pathway eventually leading to poor adult mental health. In line with our hypothesis we predict that in the current analysis there will be a significant pathway from early institutional deprivation to bullying, mediated via prior NDCs and leading to poor adult mental health. We will explore whether these effects are the same for different NDCs (e.g., autism, ADHD, and DSE) and whether they also drive functional outcomes such as unemployment and education. We further explore the possibility that bullying victimization mediates the effect of early deprivation on NDCs in childhood and adolescence, whereby bullying victimization increases the risk for NDCs, impacting later mental health and functional outcomes.
Method
Participants
Data were taken from the ERA study and included 165 Romanian (between 1 and 43 months in institutions; 91 females) and 52 UK adoptees (adopted before the age of 6 months with no deprivation history; 18 females) and their adoptive families who entered the study in the mid-1990s (for more details see Sonuga-Barke et al., Reference Sonuga-Barke, Kennedy, Kumsta, Knights, Golm, Rutter and Kreppner2017).
Procedure and measures
Assessments were carried out at ages 6, 11, and 15 years and in young adulthood (22–25 years). The procedure is described in detail in previous work utilizing these data (see Sonuga-Barke et al., Reference Sonuga-Barke, Kennedy, Kumsta, Knights, Golm, Rutter and Kreppner2017). Primary assessments took place in the individuals’ homes. Some questionnaire measures at the young adult follow-up were completed online or returned by post. For practical and scientific reasons, different assessment instruments, including interviews and standardized questionnaires, were used at different ages. Parent reports are available at all age assessments. Variables used in this study included ASD symptoms, ADHD symptoms, DSE symptoms and bullying victimization at ages 6 through 15 years and internalizing problems, and employment and education outcomes at young adulthood. Parent reports were used for all variables at ages 6 and 11 and ASD symptoms, ADHD symptoms, and DSE symptoms, and internalizing symptoms at age 15. Self-ratings were used to assess bullying victimization at age 15, and internalizing problems and functional outcomes in young adulthood.
Childhood and adolescence
Institutional deprivation
As in previous analyses (Sonuga-Barke et al., Reference Sonuga-Barke, Kennedy, Kumsta, Knights, Golm, Rutter and Kreppner2017), we divided the Romanian adoptees into two groups to capture the distinctive effects of deprivation duration in the ERA - those who spent more than 6 months in institutions (high deprivation group, n = 98 at entry) and those who spent less (n = 67 at entry). This threshold represents the point at which there is a step-change in adverse cognitive, functional and mental health outcomes. Those Romanian adoptees who experienced less than 6 month deprivation were largely unaffected by their experience with outcomes in the normal range and no different from the non-deprived controls while those over 6 months showed significant and substantial impairment across a broad range of outcomes including clinically significant symptoms of ADHD, ASD, and DSE (Golm et al., Reference Golm, Maughan, Barker, Hill, Kennedy, Knights and Sonuga-Barke2020; Kennedy et al., Reference Kennedy, Kreppner, Knights, Kumsta, Maughan, Golm and Sonuga-Barke2017; Sonuga-Barke et al., Reference Sonuga-Barke, Schlotz and Kreppner2010, Reference Sonuga-Barke, Kennedy, Kumsta, Knights, Golm, Rutter and Kreppner2017). However, the rates of impairment within this group did not increase further with additional months in the institution after this point. Therefore, we retained this threshold in the current paper. As in previous analyses, we then combined the <6 months group with the UK adoptees, with which they did not differ in terms of outcomes, to create a large or low deprivation group (n = 119 at entry).
Bullying victimization
We assessed bullying victimization using parents’ responses to two interview questions at age 6 (teased by other children, picked on or bullied) and one interview question at age 11 (ever been bullied). At age 15, bullying was assessed using self-report on 3 items from the Impact of Life Events Questionnaire (people telling nasty stories about you, being physically bullied by other young people, being teased in a nasty way by other young people; Crane et al., Reference Crane, Heron, Gunnell, Lewis, Evans and Williams2016). To account for discrepancies in assessment format across time points, we coded answers as either any report of bullying = 1 or no indication of bullying = 0.
Disinhibited social engagement
DSE symptoms were measured based on researcher ratings of parents’ responses to age-appropriate variations of three interview questions at age 6, 11, and 15 (α = .59, .70, .86, respectively). The questions were in relation to interactions with strangers, tapping the constructs of being “too friendly”, showing “inappropriate intrusiveness”, and being “unaware of social boundaries” (Sonuga-Barke et al., Reference Sonuga-Barke, Kennedy, Kumsta, Knights, Golm, Rutter and Kreppner2017). A rating of “definite evidence of disinhibition” (rating of 2 on a 0–2 scale) represented a positive endorsement.
Autism symptoms
Parent ratings on a 15-item version of the Social Communication Questionnaire (Rutter et al., Reference Rutter, Bailey and Lord2003; Sonuga-Barke et al., Reference Sonuga-Barke, Kennedy, Kumsta, Knights, Golm, Rutter and Kreppner2017), adapted to be appropriate across the ages included here, were used at age 6, 11, and 15 as an index of autism symptoms (α = .70, .76, .82, respectively). Five items were sampled from each scale – social reciprocal interaction, communication, and repetitive and stereotyped behaviors (see Sonuga-Barke et al., Reference Sonuga-Barke, Kennedy, Kumsta, Knights, Golm, Rutter and Kreppner2017 for the item selection rationale). Items were rated as absent (0) or present (1).
ADHD symptoms
Symptoms of inattention and overactivity were based on the sum of parent endorsement of three items: restless, squirmy, and inattention (range of 0–3). Items were taken from the Revised Rutter scale (Elander & Rutter, Reference Elander and Rutter1996) at ages 6 and 11 and the Strengths and Difficulties Questionnaire (Goodman, Reference Goodman1997) at age 15 (α = .68, .73, .75, respectively). A rating of two (certainly applies) on a 0–2 rating scale represented a positive endorsement.
Internalizing symptoms
Emotional symptoms assessed at age 15 (but not 6 and 11) were based on a sum of parent endorsement of three items from the Strength and Difficulties Questionnaire (SDQ; Goodman, Reference Goodman1997): worries, sadness and anxiety (α = .60).
Young adulthood
Internalizing symptoms
The anxiety and depression scales of the Connors Comprehensive Behavior Rating Scale (Conners, Reference Conners2008) were used with young adults. Ratings of 2 and above (on a 0–3 scale) were taken to reflect symptom endorsement for anxiety and depression. The anxiety scale had eight items and the depression scale had nine items (α = .87 and .81, respectively). A composite internalizing symptoms z-score was calculated based on the sum of the depression and anxiety z-scores.
Functional outcome
Two domains were used to calculate a composite score of functional outcome based on interviews completed primarily with young adults: low education achievement and unemployment. There were data available from 158 young adults. We supplemented these with six parent reports when self-report was unavailable for a total of 164 responses. Out of the 164, there were two participants with missing data on one of the two functional outcome questions; therefore we had a total of 162 responses for the combined functional outcome score. Higher scores represent poor functional outcome, whereby 0 = no impairment, 1 = either low education or unemployment, 2 = low education and unemployment. A person was considered unemployed if they were not in work, education or training. A person was considered to have low educational achievement if they had not studied further than secondary education (i.e., GCSE’s).
Statistical analysis
We calculated descriptive statistics for all the variables used in this study and examined differences across deprivation groups. Depending on the variable type, we used chi square tests of independence (with Yates correction) for the bully victimization rates, the Wilcoxon Rank-Sum Test (Mann-Whitney U Test) for DSE and ADHD symptoms, and functional outcome, and Welch’s t-test for ASD and internalizing symptoms. We also estimated bivariate correlations among these variables.
Before testing the path analysis model, we examined differences between males and females on all the main outcomes and assessed the association between emotional symptoms in adolescence with internalizing symptoms in young adulthood to determine whether to control for these variables in the model. We then tested the path analysis model to assess sequencing of NDCs and bullying victimization across childhood and adolescence as a function of deprivation and their impact on internalizing symptoms and functional outcomes in young adulthood. Direct paths from deprivation groups to all variables at ages 6 through young adulthood were estimated. Cross-lagged effects were also estimated between bullying victimization and NDCs to determine the temporal associations among those domains. In addition, contemporaneous associations among all variables and cross-lagged associations among NDCs were controlled for in the model. We also ran sensitivity analysis to check whether the combination of the <6 months group with the UK adoptees to create a low deprivation group impacted the results. The results from the path analysis model estimated using the Romanian sample only (n = 165) are included in Figure 1 in the supplementary file.
The path analysis model was estimated using R software with the lavaan package (version 0.6–7; Rosseel, Reference Rosseel2012). Due to the binary and ordinal nature of some variables, weighted least square estimation was used with robust standard errors and fit statistics. Pairwise approach was used when missing data were present, whereby all available data points from a particular participant were used when estimating the correlation matrix for the path analysis. Model fit was evaluated using the SRMR, the RMSEA, the CFI, and the TLI.
Results
Descriptive statistics, group differences, and correlations
Although sex differences have been previously reported with regards to some of the domains measured in this study, there were no significant differences between males and females on any outcomes (i.e., SCQ, ADHD, DSE, internalizing symptoms, and functional outcome score) in our sample, therefore sex was not included as a covariate in subsequent analysis. Internalizing symptoms at age 15 as reported by parents were not significantly correlated with self-reported internalizing problems in young adulthood, and thus not considered in further analyses.
The rate of bullying victimization across childhood and adolescence by deprivation group is shown in Figure 1. Based on chi-square tests of independence, the high deprivation group had higher rates of bullying victimization at age 6 (χ2(1) = 3.90, p = .048) and 15 (χ2 (1) = 7.63, p = .006) than the low deprivation group. There was no statistically significant difference between groups in rates of bullying victimization at age 11, χ2 (1) = 3.31, p = .069. Significant differences between groups existed for all other variables (Table 1). The high deprivation group had more DSE, ASD, and ADHD symptoms at ages 6, 11, and 15, and higher internalizing and poorer functional outcomes in young adulthood compared to the low deprivation group (all ps < .05). DSE, ASD, and ADHD symptoms were all significantly and positively correlated at ages 6, 11, and 15. Internalizing problems were significantly positively correlated with DSE symptoms at ages 6 and 11, ASD symptoms at age 11, ADHD symptoms at ages 6, 11, and 15, and bullying victimization at age 15. Poor functional outcomes at young adulthood were significantly positively associated with DSE, ASD, and ADHD symptoms at ages 6, 11, and 15, and bullying victimization at age 15 (see Table 2).
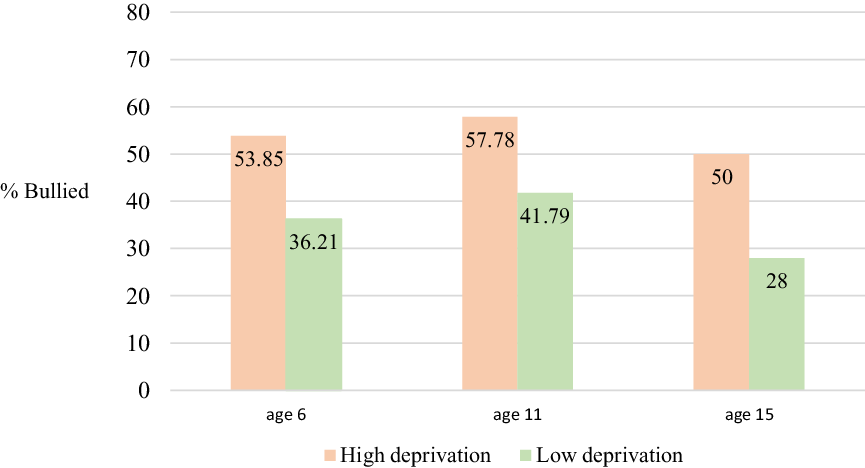
Figure 1. Rate of bullying victimization across age by deprivation group. Note. High deprivation group = Romanian adoptees who spent more than 6 months in institutions and low deprivation group = Romanian adoptees who spent less than 6 months in institutions and UK adoptees. The sample size for the high deprivation and low deprivation groups at each age was as follows: age 6: 52 and 116; age 11: 90 and 67; age 15: 70 and 100, respectively.
Table 1. Pairwise comparisons across deprivation groups
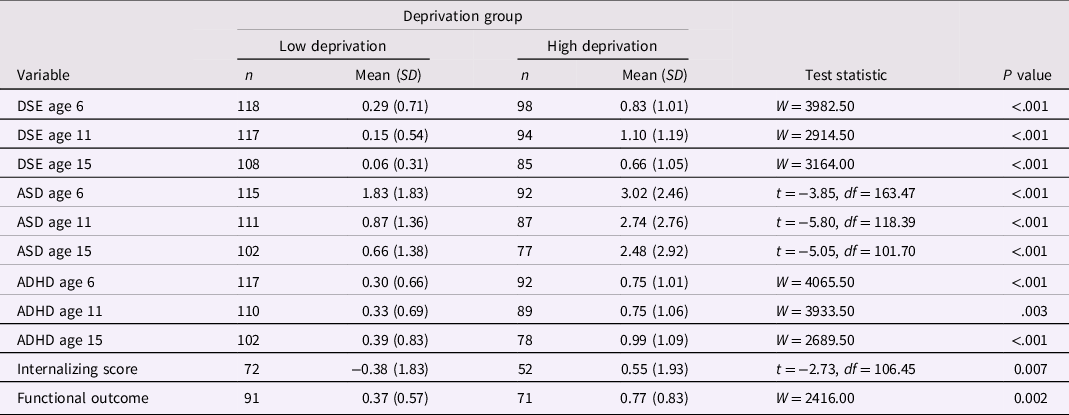
DSE Disinhibited social engagement symptoms; ASD autism spectrum disorder symptoms (social communications questionnaire); ADHD symptoms.
Table 2. Correlations among variables

Note. Spearman correlation and pearson correlation were used with ordinal and continuous variables, respectively. DSE Disinhibited social engagement symptoms; ASD autism spectrum disorder symptoms (social communications questionnaire); ADHD symptoms.
*Significant at p < .05.
Path analysis model results
The path analysis model had a good fit to the data (CFI = 1.00, TLI = 0.99, RMSEA = 0.02, SRMR = 0.09). Figure 2 shows the significant paths in the path analysis model (see supplementary material for all paths, significant and nonsignificant). Deprivation significantly predicted all three NDCs and bullying victimization at age 6 and ASD and DSE symptoms at age 11. Deprivation did not have significant unique effects on any age 15 or young adult variables. Nonetheless, all indirect pathways tested from deprivation to variables at age 11 through age 6 variables were significant, as shown in Table 3. Deprivation also had a significant indirect pathway through ASD symptoms at age 11 to ASD symptoms at age 15, but not to bullying victimization at age 15.
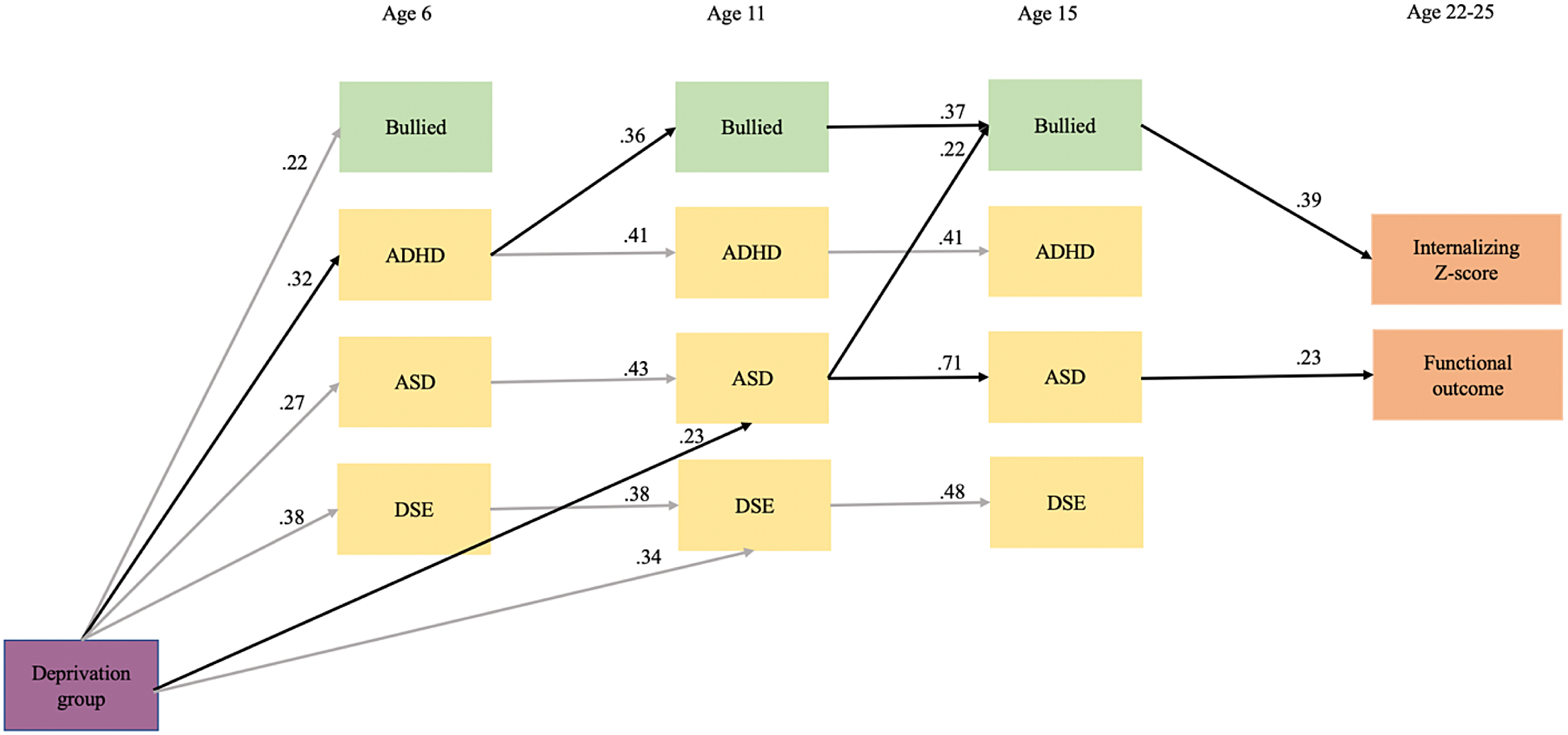
Figure 2. Path analysis model. Note. Only significant paths are shown in the model. Contemporaneous associations, cross-lagged associations among NDCs, and the association between the endogenous variables are not included in the visual to reduce clutter. Black paths highlight the significant pathways from deprivation to mental health and functional outcomes in young adulthood through NDCs and bullying victimization in childhood and adolescence (see Table 3 for further detail). DSE Disinhibited social engagement symptoms; ASD autism spectrum disorder symptoms (social communications questionnaire); ADHD symptoms.
Table 3. Indirect effects tested in the path analysis model
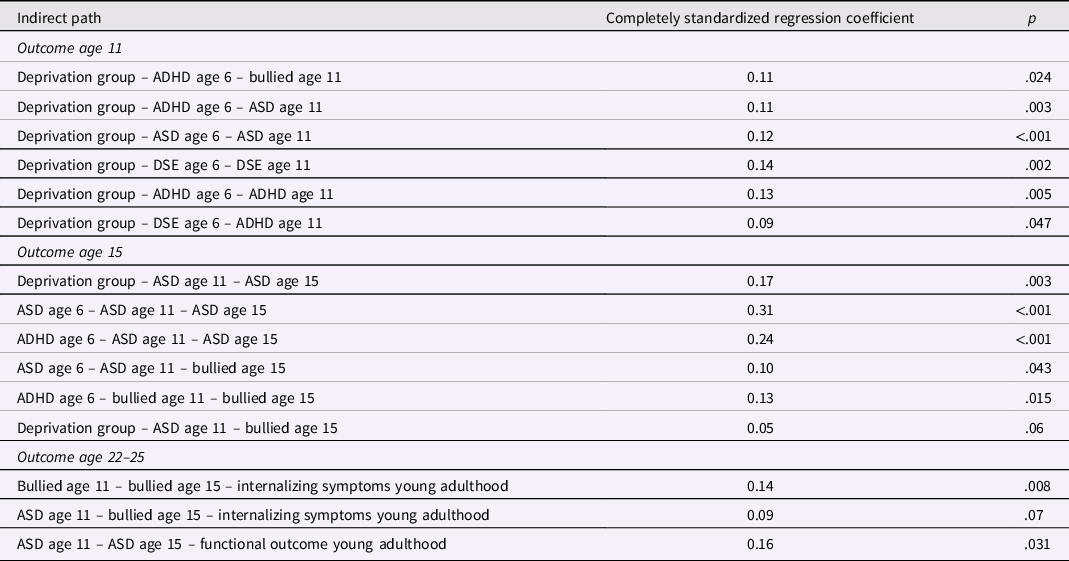
Note. DSE Disinhibited social engagement symptoms; ASD autism spectrum disorder symptoms (social communications questionnaire); ADHD symptoms.
There was strong continuity for NDPs across ages 6 through 15, whereas bullying victimization showed significant stability between age 11 and 15 years only. ADHD at age 6 predicted bullying victimization at age 11, whereas ASD at age 11 predicted bullying victimization at age 15. Further, there were significant indirect pathways from ASD and ADHD symptoms at age 6 to bullying victimization at age 15 through ASD symptoms and bullying victimization at age 11, respectively. In addition, bullying victimization at age 15 was significantly associated with internalizing problems in young adulthood and offered an indirect pathway from bullying victimization but not ASD symptoms at age 11. Finally, ASD symptoms at age 15 were directly associated with functional problems in young adulthood and offered an indirect pathway from ASD symptoms at age 11. Results remained similar when controlling for the effect of age 6 IQ on young adult outcomes, albeit model fit worsened (see Table 2 in the supplementary material).
Discussion
In this study, we provide compelling evidence that severe and extended deprivation very early in life occurring in institutions (i.e., outside of families) is associated with significantly elevated rates of bullying victimization during childhood and adolescence which in turn impacts negatively on mental health in adult life. Furthermore, we supported our hypothesis that this pathway between early institutional deprivation and bullying-related poor mental health was mediated by the emergence and persistence of NDCs. In doing this we highlight the power of neglect-type maltreatment and not just abuse to create risks for bullying victimization. At the same time we illustrate the possibility that the association between maltreatment and bullying victimization observed in the context of NDCs can represent more than just a shared effect evoked by the behaviors of people with NDCs. Crucially in this regard the overwhelming majority of ERA adoptive families provided high quality care with no evidence of maltreatment recorded (Castle et al., Reference Castle, Beckett, Rutter and Sonuga-Barke2010) and although it is possible that adoptees experienced some abuse in the institutions, alongside their deprivation, this was certainly not the pre-dominant form of maltreatment nor is it likely that it was evoked by NDCs – given the age at which the individuals entered and left the institutions.
There were a number of findings of particular note. First, all the evidence suggests that the direction of effects is from NDCs to bullying victimization – with no cross lagged effects in the opposite direction. This pattern is consistent with the notion that the behaviors and/or symptoms of individuals with NDCs evoke negative responses from peers, a finding supported by previous research on the peer relationships of people with ADHD and autism and the determinants of bullying more generally (see Hellström, Reference Hellström2019; Jawaid et al., Reference Jawaid, Riby, Owens, White, Tarar and Schulz2012; Mayes et al., Reference Mayes, Calhoun, Baweja and Mahr2015). This is the first study to provide strong longitudinal evidence for the pathway from ADHD and ASD symptoms to bullying victimization while also controlling for earlier victimization and other NDCs. Second, ADHD and autism played separate and distinctive roles in mediating the deprivation – bullying – mental health pathway. The prospective link between bullying victimization and ADHD symptoms was established earlier in development (between age 6 and 11) than that seen for autism and bullying victimization (between age 11 and 15). This may reflect developmental differences in the manifestation and impact of these two forms of deprivation specific NDCs and how they impact on peer relationships, with ADHD behaviors and related impairments being more apparent and disruptive to social relations in the early school years than autism. On the other hand, autism-related difficulties may become more impairing socially in adolescence when particular friendships are developed and relationships become more exclusive. For instance, children with ASD may be placed in special education classes or be heavily involved in support services at younger ages, before being introduced to regular or mainstream classrooms later in the school years where they could be more exposed and vulnerable to bullying by peers. There is evidence to show that the receipt of some important special education services declines across the school years for children with ASD (Wei et al., Reference Wei, Wagner, Christiano, Shattuck and Yu2014). Further, based on clinical guidelines and national data from the US, children with ADHD are more likely to be prescribed and take medication in middle childhood and adolescence (AAP, 2011; Danielson et al., Reference Danielson, Bitsko, Ghandour, Holbrook, Kogan and Blumberg2018), which could potentially attenuate the possibility that those symptoms will evoke bullying victimization by peers.
Third, while there were strong continuities in bullying from early adolescence onwards – consistent with prior research (Sourander et al., Reference Sourander, Helstelä, Helenius and Piha2000), bullying in adolescence was not related to bullying in childhood, suggesting two separate developmentally distinct bullying processes one in childhood and the other in adolescence. Interestingly, deprivation increased the risks of this early exposure to bullying by age of 6, although it remains unclear why this was the case. NDCs were not measured prior to this age in the full ERA sample, but it is possible that the patterns of deprivation-related impairment experienced by the ERA adoptees were already having an impact on social relations even in this very early period of development. This hypothesis is consistent with other finding that that ADHD symptoms mediated the effect of early institutional neglect on bullying victimization in kindergarten (Pitula et al., Reference Pitula, DePasquale, Mliner and Gunnar2019). Further, in the ERA sample, pretend and social role play at age 4 were observed less frequently in the Romanian adoptees as compared to the UK adoptees (Kreppner et al., Reference Kreppner, O'Connor, Dunn and Andersen-Wood1999), which in combination with possible language difficulties at that age may create increased social vulnerability and peer difficulties. Fourth, DSE, although strongly driven by prior deprivation, was unrelated to either bullying or poor outcomes in adulthood. This is consistent with prior studies that suggest that DSE although extremely distinctive of the ERA adoptees was a rather benign feature of the syndrome of behaviors associated with deprivation (Kennedy et al., Reference Kennedy, Kreppner, Knights, Kumsta, Maughan, Golm and Sonuga-Barke2017). In some ways this is surprising given that inappropriate social approach, a lack of understanding of social boundaries and excessive self disclosure are core features of DSE, which have been previously implicated with social vulnerability and bullying victimization in kindergarten in post-institutionalized adoptees (DePasquale et al., Reference DePasquale, Lawler, Koss and Gunnar2020). It is possible that attachment-related difficulties are important early markers for vulnerability to bullying victimization due to their association with other NDCs such as ADHD and ASD. Further, socially inappropriate behaviors characteristic of DSE are typically those reflected in children’s relationships with adults and may not necessarily be as apparent to peers as ADHD and ASD symptoms, particularly during the school years.
Fifth, although there was a significant bivariate correlation between bullying victimization at age 15 and young adult functional outcomes, the unique effect of bullying victimization, while controlling for NDCs at age 15 and deprivation status, was limited to mental health outcomes. This finding is consistent with a study showing that when entered alongside other child maltreatment experiences, bullying does not have a significant direct effect on functional impairment in adulthood (Sweeting et al., Reference Sweeting, Garfin, Holman and Silver2020). Still, prior research suggests a broader pattern of bullying-related impacts in adult life (see Arseneault, Reference Arseneault2018). One possible explanation is that in previous study samples the bullying exposures were confounded by low SES strengthening the link with these outcomes. The adoptive families in the ERA sample were by and large well educated and financially stable, which may have mitigated some of the negative impact on functioning outcomes. Despite the long-term persistence of difficulties in a substantial proportion of the Romanian adoptees exposed to extended deprivation – it seems highly likely that adoption in well resourced, committed and caring families (Castle et al., Reference Castle, Beckett, Rutter and Sonuga-Barke2010), did in fact change the course of lives of their adoptive children in compared to their peers who remained in the institutions. The most obvious evidence for this relates to rapid catch-up seen during the year or two following adoption seen for nearly all children. However, ERA did not allow a direct comparison of the development of adopted and non-adopted orphans and so definitive evidence for this is lacking. Another possibility is that due to the nature of our high risk sample, bullying victimization does not contribute to functional outcomes over and above the high NDCs in this sample. In our model, ASD symptoms in adolescence significantly predicted poor functional outcomes in young adulthood, consistent with previous literature (see Holwerda et al., Reference Holwerda, Van Der Klink, Groothoff and Brouwer2012). As expected, the group of adoptees with high institutional deprivation presented with significantly higher internalizing symptoms and poor functional outcomes in young adulthood. Bullying victimization was a key mediator of the pathway to mental health difficulties. Although NDCs were identified previously as mediators from early institutional deprivation to mental health difficulties in young adulthood (Golm et al., Reference Golm, Maughan, Barker, Hill, Kennedy, Knights and Sonuga-Barke2020), it appears that this developmental cascade is further characterized by the mediating role of bullying victimization. Specifically, children with deprivation-related NDCs were at increased risk for bullying victimization, which in turn predicted internalizing symptoms in young adulthood. These results are consistent with findings reported with other groups of children vulnerable to neurodevelopmental problems such as preterm children, whereby a study found that bullying victimization mediated the association between elevated neurodevelopmental problems and psychotic experiences in adulthood (Liu et al., Reference Liu, Mendonça, Johnson, O’Reilly, Bartmann, Marlow and Wolke2021). In our model, deprivation status and NDCs at age 15 did not have a unique impact on internalizing symptoms in young adulthood while controlling for bullying victimization at age 15. These results support the conclusion that bullying victimization can be a consequence of child maltreatment and an independent risk factor for later mental health difficulties (e.g., Lereya et al., Reference Lereya, Copeland, Costello and Wolke2015; Macalli et al., Reference Macalli, Orri, Tzourio and Côté2021) and extend these effects to developmental cascade models of early institutional neglect. Considering the sample characteristics and the study design, these effects are unconfounded by familial risk for NDCs and internalizing problems commonly found in biological families or intergenerational transmission of violence, considering that bullying victimization happens outside of the family context. Taken together, the findings are consistent with McCrory and colleague’s theory of latent vulnerability – neurocognitive effects of early maltreatment increase one’s vulnerability to mental health problems following stressors later in life (Reference McCrory, Gerin and Viding2017). We showed how deep-seated neuro-developmental impacts of institutional neglect increase not only the risk of bullying victimization but also vulnerability to the mental health impact of this victimization.
Limitations
Despite the important contributions of this study, there are several limitations to consider. Our measure of bullying victimization only captured the presence or absence of bullying and did not assess the severity or type of bullying victimization. Previous research has supported a dose-response-relationship between victimization and internalizing symptoms (Zwierzynska et al., Reference Zwierzynska, Wolke and Lereya2013), which should be considered in future work. We also did not measure child maltreatment or other forms of victimization in adolescence, which could have also had an independent effect on internalizing symptoms in adulthood (see Schaefer et al., Reference Schaefer, Moffitt, Arseneault, Danese, Fisher, Houts and Caspi2018). Our model included NDCs mediated pathways between early neglect and bullying victimization; future work can further explicate this developmental cascade by including processes that mediate the association between bullying victimization in adolescence and mental health difficulties in adulthood (e.g., self-efficacy; Singh & Bussey, Reference Singh and Bussey2011). Further, it is worth noting the possibility that common method variance contributed to the association between self-reported bullying victimization at age 15 and young adult internalizing problems. Nonetheless, a considerable period of time had elapsed between those two timepoints, which would have mitigated this effect. In addition, the different association observed with functional outcomes in young adulthood provide further evidence to the uniqueness of bullying victimization in impacting mental health outcomes. Further, as mentioned in previous work using the ERA sample, there was notable attrition between adolescence and young adulthood, although it was found to be at random (i.e., nonselective; Sonuga-Barke et al., Reference Sonuga-Barke, Kennedy, Kumsta, Knights, Golm, Rutter and Kreppner2017). Finally, although our sample presented with various levels of early deprivation, the nature of this high risk sample may limit the generalizability of our findings to other samples of children with less severe early maltreatment.
Clinical implications
The findings underscore how persistent neuro-developmental impacts of institutional neglect can cascade across development and increase the risk toward bullying victimization in childhood and adolescence and in turn to mental health problems in young adulthood. Notably, even when it is known that maltreatment at home is not evoked by these NDCs, bullying victimization can be an outcome for children who have experienced early severe neglect, with implications for later mental health. Therefore, early prevention focused on supporting children with NDCs is important to mitigate their vulnerability towards victimization. These programs can focus on social skills, impulse control, and emotion regulation to support children in managing their symptoms and mitigate their vulnerability towards further victimization. In addition, inclusive school programs focused on developing children’s tolerance to neurodevelopmental difficulties and neurodiversity can be vital in any prevention effort (e.g., Cook et al., Reference Cook, Ogden and Winstone2020). Further, mediated pathways through bullying victimization had a key role in the emergence of mental health difficulties in young adulthood following early deprivation. These findings underscore the importance of continued school and policy efforts in tackling the widespread problem of bullying victimization, especially for children who are vulnerable or at increased risk to being bullied.
Conclusion
In summary, we extend the literatures on (a) the links between early child maltreatment, bullying victimization and mental health and (b) the impact of bullying in people with neuro-developmental problems by showing that for young people exposed to severe and extended institutional deprivation these association are mediated via specific pathways from ADHD and autism with earlier effects in the former than the latter. Further, bullying victimization had a unique effect on adult mental health but not on adult functional outcomes, which was significantly predicted by autism symptoms in adolescence. Taken together, these findings highlight the need for further research with high-risk samples to explore the effects of negative and positive life events during childhood and adolescence on adult mental health and functional outcomes to elucidate the interplay between individually- and environmentally-mediated vulnerability and protective factors over time.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S095457942200089X
Acknowledgements
We would also like to express our sincere gratitude to all the families and young people who have participated in this study over the many years it has been running. Without them this work would not be possible. We are also grateful for the comments of Dr Graeme Fairchild during initial planning meetings. Thanks go to all the previous researchers on the project especially Dr Celia Beckett, Jenny Castle, Dr Suzanne Stevens, Dr Emma Colvert, Christine Groothues and Amanda Hawkins who were involved in the collection of data during the mid-adolescent phase of the project. We thank our advisory board for all their useful suggestions especially Professor Megan Gunnar, Professor Trevor Robbins and Dr John Simmonds.
Funding statement
The Economic and Social Research Council funded the young adult follow-up of the English and Romanian Adoptees (ERA) study (RES-062-23-3300). The ERA received funding from the Department of Health [age 4-, 6-, 11 and 15-year assessments; reference number 3700295; January 1, 1993, to December 31, 1997; age 15 years follow-up; 3700295; September 1, 2003, to March 31, 2009 (National Institute for Health Research Central Commissioning Facility)], the Medical Research Council, Jacobs Foundation (October 1, 2003, to September 30, 2009), and the Nuffield Foundation (OPD/00248/G; October 1, 2003, to September 30, 2007).
Conflicts of interest
E.S.B. received speaker fees, research funding, and conference support from, and has served as consultant to, Shire Pharma, and received speaker fees from Janssen-Cilag. E.S.B. served as consultant to Neurotech Solutions, Aarhus University, Copenhagen University, and Berhanderling, Skolerne, Copenhagen and KU Leuven. E.S.B. has received royalties from Oxford University Press and Jessica Kingsley. The remaining authors have declared that they have no competing or potential conflicts of interest.








