A 61-year-old male was referred for assessment of bilateral optic disk edema, which was noticed 3 months ago when he complained of slow progressively worsening vision in both eyes. At that time, visual acuity was recorded as 20/25 on the right and 20/30 on the left. Around the same time, the patient was diagnosed with stage IV poorly differentiated gastric adenocarcinoma. Enlarged perigastric lymph nodes and diffuse bony metastasis were present at the time of diagnosis. After bilateral optic nerve head edema was confirmed, a contrast-enhanced magnetic resonance imaging (MRI) of the brain was performed and interpreted as normal. MRI of the spine demonstrated diffuse osseous metastases. High-volume lumbar puncture (LP) demonstrated mildly elevated leukocyte count and protein levels but no evidence of malignant cells on cytological analysis. Systemic chemotherapy was commenced. Visual acuity continued to deteriorate and the patient was referred to our service 3 months later. Visual acuity was 20/50 in each eye, there was no relative afferent pupillary defect, and formal visual fields demonstrated marked generalized depression in both eyes. There was bilateral severe optic nerve head swelling (Figure 1). Neurologic exam demonstrated a wide-based gait and slightly decreased strength in the left leg.
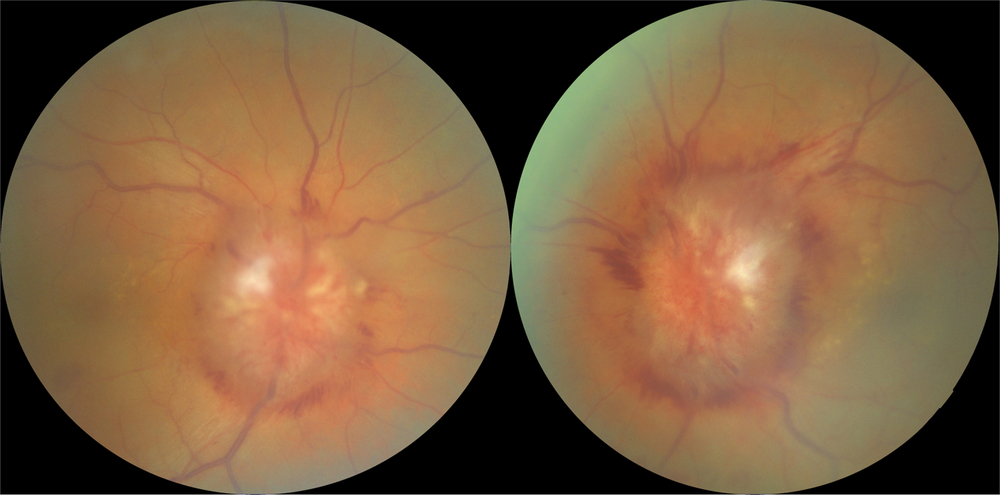
Figure 1: Fundus photographs demonstrating severe bilateral optic nerve head swelling.
Repeat MRI of the brain demonstrated dilated optic nerve sheaths bilaterally consistent with papilledema but was otherwise unremarkable. Magnetic resonance venography to rule out dural sinus thrombosis due to underlying hypercoagulable state and CT scan of the chest and a Doppler ultrasound of the neck veins to rule out superior vena cava obstruction as a cause of papilledema were performed and were both unremarkable. An LP was repeated demonstrating an elevated opening pressure of 28 cm of water with white cell count of 41, protein of 14,000 mg/L (normal up to 600 mg/L) and again negative cytological analysis for malignant cells. Because of the dramatically elevated cerebrospinal fluid (CSF) protein level, the suspicion for leptomeningeal carcinomatosis (LC) was high. MRI of the spine was performed and demonstrated leptomeningeal metastasis to the surface of the spinal cord and roots of the cauda equina (Figure 2A). Third brain MRI demonstrated diffuse enhancement of leptomeninges surrounding both optic nerves suggestive of metastatic deposits (Figure 2B,C). This leptomeningeal enhancement was not appreciated on both previous MRIs which were done in two separate institutions and interpreted by two different neuroradiologists. Palliative radiotherapy to the spine and orbits commenced and chemotherapy was resumed. Despite treatment, the patient died 3 months after LC was diagnosed; autopsy was declined by the family thus pathological confirmation of the leptomeningeal metastasis was not possible.
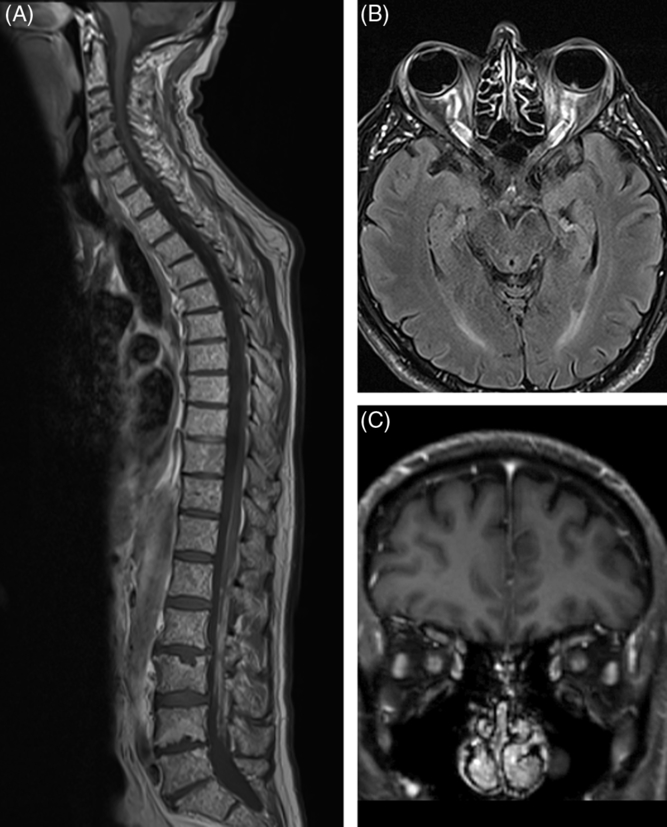
Figure 2: (A) Sagittal T1-weighted post-contrast MRI of the spine demonstrating diffuse small metastases throughout the vertebral bodies and linear enhancement along the surface of the spinal cord and roots of the cauda equina. (B, C) Axial and coronal post-contrast T1-weighted views demonstrating enhancement of both optic nerves.
LC is an uncommon complication of advanced metastatic malignancies that is increasing in prevalence due to increased survival of cancer patients. It complicates 3–8% cases of solid malignancies, the most common sites of origin being breast, lung, and melanoma (5–25%). The incidence of LC in gastric adenocarcinoma is only 0.06% Reference Bulut, Erden, Karaca and Göker1 – Reference Kim2 . Neurological involvement at various levels of the central nervous system is common but headache remains the predominant complaint. Ocular manifestations may include vision loss usually from direct infiltration or compression of the optic nerves by cancer cells, papilledema typically caused by increase in CSF viscosity and thus decrease in its outflow, ocular motility deficits due to direct infiltration of oculomotor nerves, and pupillary abnormalities Reference Lisenko, Kumar, Yao, Ajani and Ho3 – Reference Sabater, Sadaba and de Nova5 .
Our patient was found to have bilateral optic nerve head swelling which was initially presumed to be caused by papilledema due to increase in CSF viscosity. However, severely constricted visual fields and the presence of diffuse leptomeningeal thickening and enhancement surrounding intraorbiral optic nerves on imaging suggested bilateral optic neuropathy due to compression of the optic nerves by metastatic deposits as an additional mechanism of optic nerve swelling. The presence of papilledema was supported by relative preservation of central visual acuity despite long-standing disk edema as well as an elevated opening pressure on LP. There are several proposed mechanisms for increased intracranial pressure in patients with LC: it may be secondary to high levels of CSF protein due to leptomeningeal seeding by cancer cells which increases CSF viscosity and leads to its decreased outflow. Another possibility is cerebral edema secondary to increased cerebral vascular endothelial permeability due to aberrant stimulation of the meninges by tumor cells causing release of various chemical mediators Reference Nayar, Ejikeme and Chongsathidkiet6 . Lastly, tumor cells may directly block arachnoid granulations, the presumed main site of CSF absorption.
Second mechanism for marked bilateral disk edema in our patient was most likely a superimposed bilateral optic neuropathy as demonstrated by constricted visual fields and slowly deteriorating central visual acuities. This was most likely secondary to infiltration of subarachnoid space around the optic nerves by malignant cells causing compression of the optic nerves. This process is more plausible as opposed to direct infiltration of the optic nerve by cancer cells, which typically produces very quickly deteriorating vision resulting in catastrophic visual loss.
Standard investigations for LC involve MRI with gadolinium enhancement for evaluation of focal or diffuse tumor nodules in leptomeninges. Contrast enhanced MRIs may demonstrate enhancing lesions in 70–80% of cases Reference Corbin and Nagpal7 . Diagnostic confirmation necessitates the detection of malignant cells on cytology in the CSF. However, only 54% of patients with LC will have malignant cells detected on the first LP and second LP increases sensitivity to 80% with subsequent collections increasing yield by only 2–5% per collection Reference Glantz, Cole and Glantz8 . Factors contributing to false-negative results include small CSF volume, delayed processing time, site of CSF sampling, and sampling fewer than two samples Reference Nayar, Ejikeme and Chongsathidkiet6 . The exact reason for negative CSF cytology in patients with LC remains unclear but presumably the malignant cells adhere to the leptomeninges rather than being freely suspended in the CSF Reference Wasserstrom, Glass and Posner9 . The yield of CSF cytology in evaluation of patients with suspected LC is much higher in hematological malignancies, whereas in solid malignancies MRI of the brain and spine with contrast is more likely to yield positive findings Reference Nayar, Ejikeme and Chongsathidkiet6 .
Our case illustrates the importance of considering patient’s broader clinical context while being cautious of false-negative diagnostic results. Despite a high volume of disease load in the spinal cord, CSF from both high-volume LPs were negative for malignant cells reminding us that in cases of suspected LC, contrast-enhanced MRI as well as cytological analysis of CSF may be normal. However, any abnormalities of CSF composition, specifically increased protein level and/or increased CSF cellularity should prompt further high-volume CSF collections and reimaging of the entire neuro-axis including the spine, looking for presence of malignant deposits on the spinal cord and around the optic nerves. This case also underscores the importance of prompt and thorough evaluation of patients with malignancies who present with decreased vision as it can be the first presenting symptom of metastatic disease.
Disclosures
The authors declare that they have no conflicts of interest.
Statement of Authorship
Both authors contributed to the writing and reviewing of the manuscript as well as procuring the figures. Corresponding author conceived the idea of the manuscript.




