A 39-year-old woman with biopsy-confirmed Ehlers–Danlos type IV syndrome presented to the emergency room with left-sided neck pain and headache. She also reported pulsatile tinnitus in her left ear. Physical examination demonstrated left eye injection and revealed the presence of a left carotid bruit. CT C–/C+ and CT angiography showed dysplastic vascular changes, including vascular tortuosities and unruptured aneurysms, but was otherwise interpreted as normal (Figure 1). Cerebral MR angiography did not show any arterial dissection, and lumbar puncture results were within normal limits. The patient was discharged after a short period of observation.
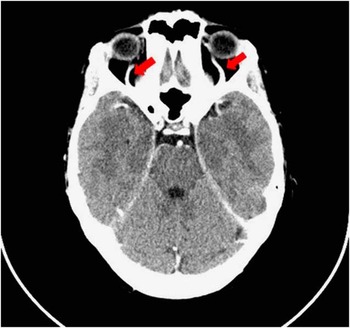
Figure 1 Contrast enhanced CT scan obtained at patient’s first visit. In retrospect, the exam showed bilateral (left more than right) enlargement of superior ophthalmic veins. Note that the unruptured aneurysms are not visualized on this image.
The patient presented again two weeks later with progressive left-sided headache, bilateral eye redness and left eye pain, ptosis and swelling. She complained of blurred vision and diplopia. In addition to conjunctival injection, examination demonstrated exophtalmos, ptosis and palpebral oedema predominantly affecting her left eye (Figure 2). A vascular murmur was heard on auscultation over the left temple. CT angiography demonstrated early opacification of both cavernous sinuses and increased size of both superior ophthalmic veins (Figure 3). Conventional angiography confirmed the presence of a fistula, originating from the cavernous segment of the left internal carotid artery (ICA) and terminating in the left cavernous sinus (Figure 4). The vascular flow from the left ICA was diverted into the cavernous sinus, and its expected vascular territory was supplied by the anterior communicating artery and vertebrobasilar system. Endovascular occlusion of the cavernous segment of the left ICA and of the fistula was performed. The day following the procedure, there was a considerable improvement in all of the patient’s ocular symptoms. Three months later, she only complained of headaches and mild diplopia on left gaze.

Figure 2 Physical examination at second visit revealed left predominant conjonctival injection, exophtalmos, and palpebral oedema. These findings, together with the presence of a bruit, are suggestive a left carotid cavernous fistula.

Figure 3 CT angiography at second visit revealed increased size of both superior ophthalmic veins and cavernous sinuses.
Direct fistulas represent an aberrant connection between the internal carotid artery and cavernous sinus, which allows for direct shunting of arterial blood into the venous system.Reference Ellis, Goldstein, Connolly and Meyers 1 These fistulas are most commonly caused by head trauma, but they may occur spontaneously in patients with collagen tissue disorders associated with increased vascular wall fragility, as is the case in type IV Ehlers–Danlos syndrome .Reference Chuman, Trobe and Petty 2
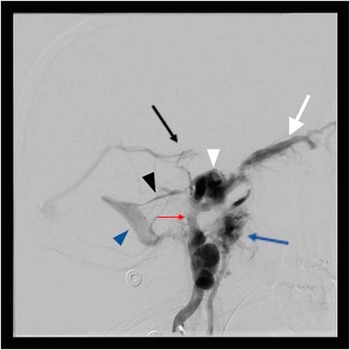
Figure 4 Conventional angiography confirmed the presence of a carotid cavernous fistula originating from the cavernous segment of the left ICA (red arrow) and terminating in the left cavernous sinus (white arrowhead). This image also shows opacification of superior ophthalmic veins (white arrow), pterygoid plexus (blue arrow), basal vein of Rosenthal (black arrow) and of the sigmoid sinus (blue arrowhead) through the superior petrosal sinus (black arrowhead).
Ocular manifestations of chemosis, conjunctival injection, proptosis and eyelid swelling occur when blood flow is redirected anteriorly from the congested cavernous sinus through the orbital veins, leading to vascular stasis, engorgement and increased venous pressure.Reference Miller 3 Headache is present in 25–84% of patients at presentation and orbital bruit in 71–80%.Reference Ellis, Goldstein, Connolly and Meyers 1 Diplopia is also a common symptom, reported in 60 to 70% of patients.Reference Miller 3 If left untreated, direct fistulas may lead to progressive vision loss and cause intracranial haemorrhages.Reference Biousse, Mendicino, Simon and Newman 4
A diagnosis of direct carotid cavernous fistula should therefore be suspected in patients presenting with conjunctival injection, headache, proptosis and ophthalmoparesis, and complaining of a bruit.Reference Feiner, Bennett and Volpe 5 Diagnosis may first be supported by noninvasive cerebral imaging. On head CT and MRI C–/C+, close attention should be given not only to the cavernous sinus, but also to the orbital veins and muscles, which can show early enlargement in the presence of a direct carotid cavernous fistula.Reference Biousse, Mendicino, Simon and Newman 4 However, cerebral angiogram remains the gold standard for the visualization of direct carotid cavernous fistulas and should be performed when there is sufficient clinical suspicion, even if noninvasive tests are inconclusive.Reference Subramanian and Williams 6
Disclosures
Josée Masson-Roy does not have anything to disclose.
Martin Savard has the following disclosures. Serono: speaker, honoraria; UCB: speaker, honoraria; ESAI: advisory board, honoraria.
Ariane Mackey has the following disclosures. Bayer: advisory board honoraria and research support.






