Breast milk, the preferred source of nutrition for most infants( 1 – 3 ), is associated with well-documented health benefits for both mother and child. Increased breast-feeding could save the USA billions of dollars and hundreds of lives( Reference Bartick and Reinhold 4 ). In the USA, breast-feeding initiation among babies born in 2011 was 79 %( 5 ), compared with the national goal of 82 %( 6 ). Although the majority of women initiate breast-feeding, breast-feeding duration and exclusivity fall well short of national goals( 2 ). Only 49 % of recent mothers breast-fed for at least 6 months as recommended( 5 ), compared with the goal of 61 %( 6 ); and further, only 19 % of infants were breast-fed exclusively at 6 months( 5 ) compared with the goal of 26 % nationally( 6 ).
Breast-feeding decisions are influenced by various social and cognitive factors, including knowledge about the benefits of breast-feeding, attitudes regarding the time commitment and potential embarrassment, perceived social support and self-efficacy( Reference Khoury, Moazzem and Jarjoura 7 – Reference Wagner and Wagner 13 ). In many cases, infant feeding decisions are made prior to or very early in pregnancy( Reference Arora, McJunkin and Wehrer 11 , Reference Losch, Dungy and Russell 12 ). However, little is documented about the timing of feeding intentions and changes throughout pregnancy.
The purpose of the present study was to examine changes in breast-feeding-related knowledge, attitudes and self-efficacy, and prenatal breast-feeding intentions, among a low-income smoke-exposed population during the course of pregnancy, who were participants of a smoking cessation and environmental tobacco smoke avoidance intervention study. Furthermore, the study also examined how changes in knowledge, barriers and self-efficacy may influence early infant feeding behaviours among women who had not yet decided on a feeding plan early in their pregnancies.
Methods
The present study assessed ancillary data to a larger randomized controlled trial of a health education intervention to reduce environmental tobacco smoke exposure among women during and after pregnancy. Pregnant women were recruited from three prenatal clinics in Rhode Island, USA that serve mostly low-income women: St. Joseph’s Hospital, Memorial Hospital of Rhode Island (MHRI) and the Women’s Primary Care Center at Women and Infants’ Hospital (WIH). The study was approved by the institutional review boards of Brown University and each of the clinical sites listed.
To determine eligibility, staff screened prenatal patients at the time of their initial prenatal appointment. To be eligible for the study, women were required to speak English, to be at least 18 years of age, to be currently smoking, recently quit or exposed to environmental tobacco smoke, to be no further than 16 weeks’ gestation in a singleton pregnancy, and to have access to a working telephone and VCR/DVD player. After the initial screening, interviewers used computer-assisted telephone interviews at 16 weeks of pregnancy or earlier to obtain consent and conduct a baseline survey, followed by another at 32 weeks’ gestation to ascertain prenatal feeding intentions as well as knowledge, attitudes and self-efficacy related to breast-feeding. An additional telephone interview was conducted at 12 weeks’ postpartum to determine actual breast-feeding behaviours.
Among the 1314 eligible participants identified through screening, 64 % completed the baseline survey and were randomized to the parent randomized controlled trial (n 847). Of these, 246 participants were excluded from the present analysis for not completing the 32-week gestational interview and one participant was excluded for missing data on the primary outcome, prenatal feeding intentions. Of the remaining 600 women from the study, 399 were asked the knowledge and attitude questions, leaving 399 in the analytic sample.
The intervention videos being tested included smoke-related messages tailored to the needs of the participant, but presented within an overall theme of prenatal health. Both study groups received newsletters containing healthy pregnancy messages, but only the intervention group received messages regarding smoking cessation or environmental tobacco smoke avoidance. Healthy infant feeding and breast-feeding were included in the video and newsletters very minimally for both intervention groups. Infant feeding attitude, intention or behavioural variables were not different between intervention groups, so data from both groups were included in these analyses.
Outcome variables for the current analysis were prenatal feeding intention and actual feeding behaviours. Participants’ self-reported prenatal feeding intention was queried at both baseline (approximately 12–16 weeks’ gestation) and 32 weeks’ gestation, with response categories of ‘exclusive breast-feeding’, ‘breast-feeding and formula in combination’, ‘exclusive formula’ and ‘undecided’. Responses coded by the interviewer as ‘don’t know’ were re-coded as ‘undecided’. Given the known benefits of any breast-feeding and the small number of women planning to exclusively breast-feed, a dichotomous breast-feeding intention variable (‘exclusive breast-feeding or breast-feeding and formula-feeding’ v. ‘exclusive formula-feeding or undecided’) was also examined.
Infant feeding initiation at delivery and infant feeding at 30 d were queried at 12 weeks’ postpartum. Women were asked to describe their current feeding practices with choices of ‘breast-feeding only’, ‘breast-feeding and formula’ and ‘formula only’. Also, women were asked if they ever breast-fed; if yes, they were asked the age of the baby when he or she was first fed formula or some other food other than breast milk. Women who breast-fed for at least 1 d and initiated formula or another type of food supplementation later than 1 d were categorized as ‘initiating breast-feeding’. Women who never attempted to breast-feed or breast-fed for less than 1 d and initiated formula/other food supplementation within the first day were categorized as ‘exclusive formula-feeding’.
Feeding at 30 d was similarly determined. Women who reported exclusive breast-feeding at the time of the 12-week survey or women who initiated formula or other food when the baby was 30 d or older were both considered to be ‘exclusively breast-feeding’ at 30 d postpartum. Among women who initiated breast-feeding and breast-fed for at least 30 d, those who additionally initiated formula or other food supplementation prior to 30 d were considered to be ‘breast- and formula- (mixed) feeding’ at 30 d postpartum. Women who never breast-fed or stopped breast-feeding completely before 30 d were considered to be ‘exclusively formula-feeding’.
Measures of breast-feeding knowledge, attitudes and self-efficacy adapted from previous studies were conducted at baseline and at the 32-week survey( Reference Khoury, Moazzem and Jarjoura 7 , Reference Mitra, Khoury and Hinton 8 ). The response options (true/false) used in the original work were modified to a five-point Likert scale ranging from ‘agree a lot’ to ‘agree a little’, ‘neither agree nor disagree’, ‘disagree a little’ and ‘disagree a lot’. Responses coded by interviewers as ‘don’t know’, which likely represented legitimate ambivalence or lack of information, were recoded to the ‘neither agree nor disagree’ category.
Responses were assigned numerical values ranging from −2 to +2, where +2 represented the strongest response in the direction favouring breast-feeding support. A global index was created by averaging the responses from each of the eighteen individual items created by Mitra et al.( Reference Mitra, Khoury and Hinton 8 ) (referred to as the ‘Mitra index’ hereafter). A higher overall Mitra index score represented more favourable breast-feeding-related thoughts or attitudes. Mitra index subscales were created and labelled as the following factors: ‘knowledge’, ‘self-efficacy’, ‘embarrassment barriers’, ‘social and time barriers’ and ‘social support barriers’. Cronbach’s α was estimated for each of the overall Mitra index and subscale scores. The overall Mitra index exhibited strong internal consistency with a raw score of 0·76.
Sociodemographic characteristics were queried at the baseline gestational interview including mother’s age, race/ethnicity, educational attainment, employment status, household income, marital status, country of birth, native language and years lived in the USA. Parity was ascertained from the hospital discharge records pertaining to participants’ deliveries.
Differences in baseline sociodemographic characteristics by feeding intention were examined using χ 2 analyses for all categorical variables. ANOVA models were constructed to test for differences in mean Mitra index scores by breast-feeding intention category at baseline. Demographic variables associated with breast-feeding intention at baseline were included in the models. Significance tests were calculated for pairwise comparisons of Mitra index scores using t tests corrected for multiple comparisons using the Tukey–Kramer procedure.
A subgroup analysis was conducted among categories of baseline feeding intention (undecided, any breast-feeding (exclusive or mixed) and exclusive formula-feeding) to examine differences between baseline and 32-week Mitra index scores within each category of breast-feeding initiation (exclusive formula-feeding and breast-feeding). All scores and sub-scores were assessed as having a Shapiro–Wilkes test of ≥0·89, indicating that there is extremely low probability that these values are not normally distributed. Paired t tests were calculated to assess differences between baseline and 32-week overall Mitra index and subscale scores. ANOVA models were constructed for the Mitra index score and sub-scores at baseline and 32 weeks’ gestation to assess differences between feeding initiation groups with potentially confounding demographic variables (as in models of baseline values above) included in each model (n 103 for full models). Data were analysed using the statistical software package SAS version 9.4.
Results
Participants were distributed fairly evenly between the age groups of <21 years (28 %), 21–25 years (38 %) and >25 years (34 %). The majority of the sample was comprised of young adult women (66 % of women were 25 years of age or younger). Overall, 40 % of participants self-identified as non-Hispanic White, 13 % as non-Hispanic Black, 27 % as Hispanic and 19 % as ‘other’ or identified with two or more racial groups; 16 % were born outside the USA. Over a third of the sample (36 %) had not completed high school or earned a general education degree. Only 13 % of participants reported a household annual income of greater than $US 30 000; and 58 % were not employed full- or part-time. Approximately 46 % of the sampled women were not with a partner (had never been married or were currently divorced or separated); and equal proportions had previously delivered one or more live birth (Table 1).
Table 1 Sample characteristics by feeding intention at 16 weeks’ gestation or earlier among low-income smoke-exposed women (n 399) recruited from three prenatal clinics in Rhode Island, USA, February 2006–June 2009

GED, general education degree.
Individual n may not add to the total sample size due to missing values.
Baseline prenatal feeding intentions
At baseline, nearly half (44 %) of the sample reported an intention to breast-feed in some capacity with 18 % planning to breast-feed exclusively and 26 % reporting an intention to both breast-feed and formula-feed. Just under a quarter of participants planned to only feed formula, and about a third had not yet decided on a feeding plan. Feeding intention differed by age, education, racial/ethnic groups, nativity and having had a previous live birth (Table 1).
Women who planned to breast-feed were more likely to be younger, having their first child, Hispanic, be born outside the USA, be higher educated and speak Spanish based on bivariate analyses. Women who were undecided about how they would feed their baby were more likely to be younger, of more than one racial or ethnic group, be high-school educated, be born in the USA, speak English and have no previous live births.
Knowledge and attitudes about breast-feeding
The baseline Mitra index scores differed by feeding intention (Table 2). Women intending to exclusively breast-feed had higher overall Mitra index and subscale scores than women intending to exclusively formula-feed or women who were undecided about feeding plans. With the exception of knowledge sub-scores, women planning to exclusively breast-feed had similar subscale scores to women planning to breast-feed either exclusively or in combination with formula. Women who were undecided had similar knowledge sub-scores compared with women planning to combination feed, but similar embarrassment barriers sub-scores to women planning to exclusively formula-feed. Otherwise, women who were undecided had overall Mitra index, self-efficacy, time and social barriers, and social support barriers scores that were higher than those of women planning to exclusively formula-feed, but lower than those of women planning to breast-feed exclusively or combined with formula.
Table 2 Mean baseline overall Mitra index and subscale scores for prenatal knowledge, attitudes and self-efficacy related to breast-feeding by feeding intention at 16 weeks’ gestation or earlier among low-income smoke-exposed women (n 399) recruited from three prenatal clinics in Rhode Island, USA, February 2006–June 2009

Least-square means adjusted for age category, race, education, nativity, native language and previous live birth. Index scores range from −2 to +2, with greater means indicating more favourable scores. Significance of noted pairwise comparisons were corrected for multiple comparisons using Tukey–Kramer’s procedure (P<0·05).
a Significant difference between women intending to exclusively breast-feed.
b Significant difference between women intending to breast-feed and formula-feed in combination.
c Significant difference between women intending to exclusively formula-feed.
d Significant difference between women who were undecided.
Change in prenatal feeding intentions
Most women were consistent from early in pregnancy (~16 weeks) to late pregnancy (32 weeks) in their intended feeding method (Fig. 1). Of those planning early in pregnancy to exclusively breast-feed, 58·9 % were still planning to exclusively breast-feed later in pregnancy, but 31·5 % were then planning to breast-feed in combination with feeding formula. Of those planning initially to feed in combination, 74·0 % were still planning to feed in combination later in pregnancy, while 12·5 % were then planning to exclusively breast-feed. Women planning to exclusively formula-feed early in pregnancy were very likely (70·2 %) to still plan to exclusively formula-feed at 32 weeks’ gestation, although 11·7 % had decided to feed formula in combination with breast-feeding and 17·0 % were newly undecided. The highest proportion (40·6 %) of women who were undecided about their plan early in pregnancy was still undecided at 32 weeks’ gestation. Almost one-third of those undecided were newly planning to both breast-feed and feed formula, compared with 16·4 % who had decided to exclusively formula-feed and 12·5 % who decided to exclusively breast-feed.
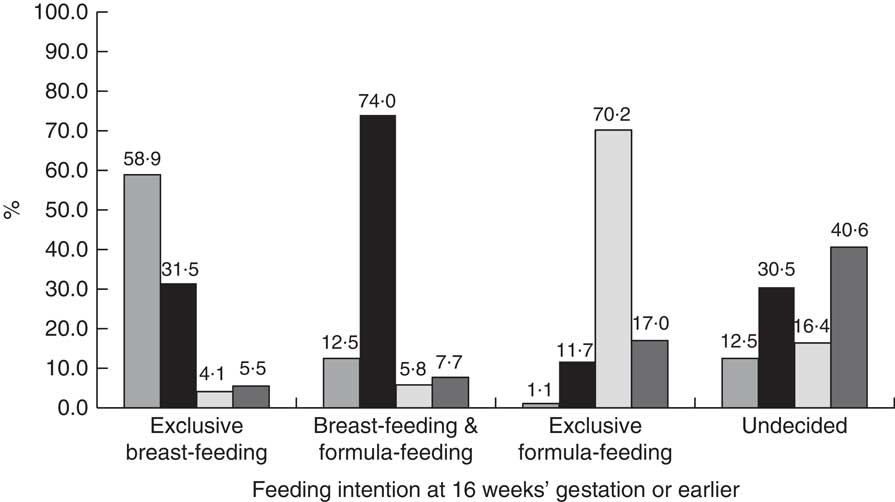
Fig. 1 Feeding intentions at 32 weeks’ gestation (![]() , exclusive breast-feeding;
, exclusive breast-feeding; ![]() , breast-feeding and formula-feeding;
, breast-feeding and formula-feeding; ![]() , exclusive formula-feeding;
, exclusive formula-feeding; ![]() , undecided) by intentions reported at 16 weeks’ gestation or earlier among low-income smoke-exposed women (n 399) recruited from three prenatal clinics in Rhode Island, USA, February 2006–June 2009
, undecided) by intentions reported at 16 weeks’ gestation or earlier among low-income smoke-exposed women (n 399) recruited from three prenatal clinics in Rhode Island, USA, February 2006–June 2009
Postpartum infant feeding behaviours
Breast-feeding initiation was observed by feeding intentions reported at baseline (Fig. 2). Of women planning at baseline to exclusively breast-feed, 91·0 % initiated breast-feeding, compared with 80·9 % of women planning at baseline to combination feed. Of women who planned at baseline to exclusively formula-feed, 18·1 % initiated at least some breast-feeding. Additionally, 57·0 % of those who were initially undecided initiated breast-feeding.
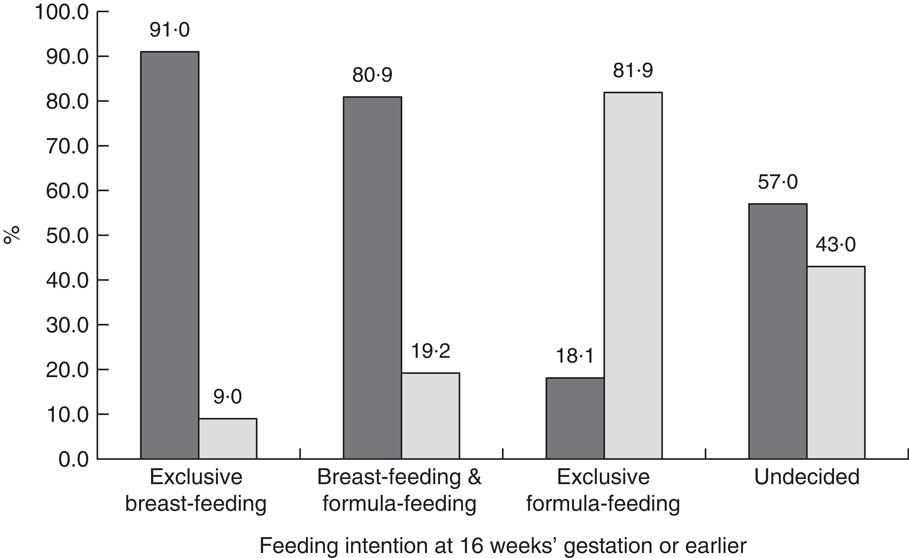
Fig. 2 Infant feeding at delivery (![]() , any breast-feeding;
, any breast-feeding; ![]() , exclusive formula-feeding) by intentions reported at 16 weeks’ gestation or earlier among low-income smoke-exposed women (n 399) recruited from three prenatal clinics in Rhode Island, USA, February 2006–June 2009
, exclusive formula-feeding) by intentions reported at 16 weeks’ gestation or earlier among low-income smoke-exposed women (n 399) recruited from three prenatal clinics in Rhode Island, USA, February 2006–June 2009
By 30 d postpartum, feeding patterns showed that early many women completed their initial infant feeding plan, although supplementation occurred across all feeding intention groups (Fig. 3). Over 75 % of women planning to exclusively breast-feed were still breast-feeding at 30 d postpartum, with 47·6 % still exclusively breast-feeding. Just over 65 % of women planning to combination feed were still breast-feeding at 30 d postpartum, with 29·9 % exclusively breast-feeding. Over 12 % of women planning to exclusively formula-feed were breast-feeding at 30 d postpartum, most of whom (9·7 %) were also feeding formula. Also, less than half (38·5 %) of women who were undecided about their feeding method were breast-feeding in some capacity at 30 d after delivery. Of those initially undecided, 16·4 % were exclusively breast-feeding and 22·1 % were feeding both breast milk and formula, with an additional 61·5 % exclusively formula-feeding.

Fig. 3 Infant feeding at 30 d (![]() , exclusive breast-feeding;
, exclusive breast-feeding; ![]() , breast-feeding and formula-feeding;
, breast-feeding and formula-feeding; ![]() , exclusive formula-feeding) by intentions reported at 16 weeks’ gestation or earlier among low-income smoke-exposed women (n 399) recruited from three prenatal clinics in Rhode Island, USA, February 2006–June 2009
, exclusive formula-feeding) by intentions reported at 16 weeks’ gestation or earlier among low-income smoke-exposed women (n 399) recruited from three prenatal clinics in Rhode Island, USA, February 2006–June 2009
Knowledge, attitude and self-efficacy changes were assessed from baseline to 32 weeks for all categories of feeding intention at baseline, by the actual initial feeding method reported (Table 3). Women who were undecided about feeding plans early in pregnancy, but initiated breast-feeding, significantly increased their overall Mitra index score from 0·60 to 0·85 (P<0·0001), whereas women who initiated exclusive formula-feeding had no change in the overall Mitra index score. At 32 weeks, women who initiated exclusive breast-feeding reported higher overall Mitra index score than women who initiated exclusive formula-feeding (P=0·0022).
Table 3 Adjusted mean overall Mitra index and subscale scores at 16 weeks’ gestation or earlier (baseline) and 32 weeks’ gestation by feeding initiation among women who were undecided about feeding plans, planned any breast-feeding or planned to feed formula exclusively; low-income smoke-exposed women (n 399) recruited from three prenatal clinics in Rhode Island, USA, February 2006–June 2009

Group differences are least-square means adjusted for age category, race, education, nativity, native language and previous live birth. Index scores range from −2 to +2 with greater means indicating more favourable scores.
*P<0·05 indicates differences between feeding initiation groups.
Among the initially undecided group, no differences in any of the baseline subscale scores were found between women who breast-fed and those who did not. Knowledge changed only among women who initiated breast-feeding (0·71 to 1·03, P=0·0009), while no change in knowledge was observed for women who later formula-fed exclusively. Similarly, self-efficacy for breast-feeding increased significantly among women who later breast-fed (0·93 to 1·14, P=0·0520). At 32 weeks, no differences were found between feeding initiation groups in knowledge sub-scores, although self-efficacy was significantly higher among women who breast-fed compared with exclusive formula feeders (P=0·0020).
Embarrassment barriers sub-scores were similar at 32 weeks for both feeding groups, and did not change significantly for either group. Time and social barriers sub-scores increased from baseline to 32 weeks for women who breast-fed (0·93 to 1·22, P=0·0018), but did not change for those who exclusively formula-fed. Social support barriers sub-scores increased from baseline to 32 weeks among women who initiated any breast-feeding (0·84 to 1·10, P=0·0351). At 32 weeks, exclusive formula feeders had lower time and social barriers (0·86 v. 0·86, P=0·0018) and social support barriers sub-scores than women who breast-fed (0·74 v. 1·10, P=0·0351).
Among those who intended to breast-feed, no differences in baseline Mitra scores or sub-scores were found between those who initiated breast-feeding and those who did not. At 32 weeks’ gestation, women who would initiate breast-feeding scored higher on the overall Mitra index compared with those who would later feed formula (1·16 v. 0·85, P<0·05) as well as higher on the knowledge (1·23 v. 0·88, P<0·05), self-efficacy (1·43 v. 1·06, P<0·05) and social support barriers (1·35 v. 0·97, P<0·05) subscales. Among women who intended to feed formula, no differences in Mitra index scores were found between those who initiated breast-feeding compared with those who initiated exclusive formula-feeding.
Changes in Mitra index scores were found for women who intended at baseline to breast-feed and initiated breast-feeding. The overall Mitra index score increased from 1·06 to 1·16 (P=0·0057). Average embarrassment barriers sub-score increased for this group (0·28 v. 0·53, P=0·0040) and the increase in knowledge sub-score also approached statistical significance (1·11 v. 1·23, P=0·0667). No changes were found for those who intended to breast-feed but initiated exclusive formula-feeding.
Among women who intended to feed formula, those who initiated breast-feeding averaged an increase in overall Mitra index score from 0·06 to 0·51 (P=0·0370), whereas those who initiated exclusive formula-feeding increased from 0·08 to 0·23 (P=0·0005). Both groups also increased mean knowledge sub-scores, with those who initiated breast-feeding increasing from 0·33 to 0·82 (P=0·0093) and those who initiated exclusive formula-feeding from 0·13 to 0·42 (P=0·0300).
Women who intended to formula-feed and initiated formula-feeding increased in embarrassment (−0·40 to −0·15, P=0·0256) and time and social barriers sub-scores (0·38 to 0·66, P=0·0188). Women who intended to formula-feed but initiated breast-feeding increased in social support barriers sub-score (0·05 to 0·70, P=0·0272).
Discussion
The present data demonstrate that infant feeding decisions for many women evolve throughout pregnancy, although a large proportion of women are able to state their intention early and most followed through on that intention. However, almost a third (32 %) of women in this sample were still undecided at 16 weeks of pregnancy and 20 % at 32 weeks. In fact, 41 % of those undecided at baseline were still undecided at 32 weeks. Additionally, breast-feeding was initiated by 57 % of those who were at baseline undecided along with 18 % of those intending to formula-feed (Fig. 2). Exclusive and mixed breast-feeding was continued at 30 d among 3 and 10 %, respectively, of those who were intending to exclusively formula-feed as well as among 16 and 22 %, respectively, of those who were undecided. Although others have asserted that most feeding decisions are made before pregnancy( Reference Losch, Dungy and Russell 12 ) or early in pregnancy( Reference Arora, McJunkin and Wehrer 11 ), the current study identifies that a small proportion, but important group of women, decide how they will feed their infant during pregnancy, some very soon before delivery. Additionally, we document the plasticity of breast-feeding plans during pregnancy among those with seemingly firm plans. These findings highlight opportunities for breast-feeding education, support and motivation of low-income women throughout pregnancy.
These opportunities for enhancing breast-feeding support are further underscored by changes in the knowledge, attitudes and self-efficacy Mitra index sub-scores documented among these groups. Women who are undecided early in pregnancy are still likely to be undecided late in pregnancy or plan to combine feeding breast milk and formula. Increases in knowledge, self-efficacy, social support barriers, and time and social barriers subscale scores were all independently associated with eventual decisions to breast-feed among those who were undecided at baseline. Increases in embarrassment barriers sub-scores among women intending to breast-feed, and in social support barriers sub-scores among women planning not to breast-feed, were associated with breast-feeding initiation. Scores for every factor among the undecided group were higher for women who breast-fed, compared with values for women who exclusively formula-fed, and knowledge, self-efficacy and social support sub-scores were higher at 32 weeks among those who intended to breast-feed for those who breast-fed compared with the small group that did not initiate breast-feeding. Scores were lower among the group intending to formula-feed compared with other women, and not different between groups based on feeding initiation.
Education and motivation may also be key factors in exclusive breast-feeding. Exclusive breast-feeding is recommended as exclusivity provides added health protections over breast milk mixed with formula( 1 ). Exclusivity is recommended until at least 4 months of age by the WHO( 3 ) and the US Breastfeeding Committee( Reference Labbok and Taylor 14 ), but the USA (41 % at 3 months and 19 % at 6 months) falls far short of the national exclusivity goals of 46 % at 3 months and 26 % at 6 months. The present study identifies knowledge as the biggest factor separating women who planned early to breast-feed exclusively from women planning to supplement with formula; however, in addition to knowledge, other subscales, such as self-efficacy, social support barriers, and time and social barriers, increased among women who were initially undecided, but who initiated breast-feeding.
While the present study did not examine the independent sociodemographic factors associated with breast-feeding exclusivity, other researchers have identified age( Reference Jones, Kogan and Singh 15 – Reference Phillips, Brett and Mendola 17 ); race, ethnicity or place of birth( Reference Newton, Chaudhuri and Grossman 16 – Reference Sussner, Lindsay and Peterson 19 ); marital status or family structure( Reference Jones, Kogan and Singh 15 , Reference Phillips, Brett and Mendola 17 ); smoking status( Reference Jones, Kogan and Singh 15 ); mental and emotional health( Reference Jones, Kogan and Singh 15 ); and support from a partner( Reference Hinic 20 , Reference Rempel, Rempel and Moore 21 ) or parent( Reference Kitano, Nomura and Kido 22 , Reference Fleurant, Schoeny and Hoban 23 ) as predictors of exclusivity. Additionally, identified psychosocial predictors of exclusivity duration include attitude( Reference Bai, Middlestadt and Peng 24 – Reference de Jager, Skouteris and Broadbent 26 ), social support( Reference de Jager, Skouteris and Broadbent 26 ), and birthing situation and attendants( Reference Newton, Chaudhuri and Grossman 16 , Reference McDonald, Pullenayegum and Chapman 27 , Reference Semenic, Loiselle and Gottlieb 28 ). While emphasis is appropriately placed in health messaging motivating women to breast-feed, room should be made to emphasize in clinical discussion or public health messaging a plan to breast-feed exclusively, addressing barriers and decreases in motivation that might lead to supplementation. Stuebe and Bonuck identified prenatal knowledge and comfort with breast-feeding in a social setting to be associated with intention to breast-feed exclusively( Reference Stuebe and Bonuck 29 ). However, emphasis on these constructs beyond recent calls to action( 2 ) may improve the focus on exclusivity in clinical and public health messaging.
Further underscoring the need for emphasis on exclusivity, our research found strong initiation; but feeding patterns at 30 d demonstrated fairly common early formula supplementation, even among women intending to exclusively breast-feed. Prenatal emphasis on exclusivity planning while intentions are still being formed or confirmed may be useful. However, exclusive breast-feeding was reported by some women planning to combination feed, and even by some planning to exclusively formula-feed. This signifies that although decisions may seem to be firm, opportunities to help women choose to exclusively breast-feed still exist even for women who seem to be past that choice.
Among the undecided group, the changes in the Mitra index sub-scores observed between intention and initiation show that increasing knowledge, self-efficacy and both social support and time and social barriers were associated with breast-feeding. More than half of the initially undecided participants and almost one in five planning to formula-feed initiated breast-feeding. However, 15 % of those planning to initiate breast-feeding did not follow through, reporting exclusively feeding formula. These constructs of knowledge, self-efficacy, and attending to social support and time and social barriers, should be combined in health education during pregnancy, and a plan for exclusivity addressing possible future barriers or concerns may prove to be the most successful.
The current study’s findings are limited by the study design. The population was smoke-exposed and recruited from clinics serving low-income women in the north-eastern USA, so these data may not be representative of all pregnant women in the USA. As a secondary analysis of a larger randomized controlled study, the intervention was not designed to and did not target breast-feeding as an outcome. The sample size for some variables, including breast-feeding at 30 d postpartum, was limited. Also, the time points for interviews and measures were not chosen to optimally address breast-feeding study objectives, and required recall of specific feeding and supplementation behaviours sometimes weeks or months after the occurrence. Furthermore, all explanatory variables may not have been measured. For instance, previous research has found a relationship of initiation of breast-feeding with previous breast-feeding experience, parity( Reference Holbrook, White and Heyman 30 ) and participation in the Special Supplemental Nutrition Program for Women, Infants, and Children( Reference Ziol-Guest and Hernandez 31 ), none of which were addressed in the current analysis. Lastly, the type of analysis conducted was not able to be adjusted for multiple comparisons, but the number of analyses may lead to the conclusion that some significant results were due to chance alone.
While acknowledging these limitations, the present prospective study recorded breast-feeding intentions in real time at baseline and late in pregnancy. Breast-feeding behaviours at delivery and 30 d postpartum were collected at 12 weeks’ postpartum, which introduced some potential for recall bias, but this was reduced compared with studies asking in even later questionnaires. However, these results provide an important insight into women most at risk for not breast-feeding, including low-income women( Reference Haslam, Lawrence and Haefeli 32 – Reference Simard, O’Brien and Beaudoin 34 ) and women who are smoke-exposed( Reference Jones, Kogan and Singh 15 , Reference Donath and Amir 35 – Reference Weiser, Lin and Garikapaty 38 ), so the study makes a potentially important contribution to the breast-feeding and health education literature. Further research should identify when feeding intentions become finalized (i.e. later time points). Also, prenatal planning factors associated with meeting the recommendations for 6 months of exclusive breast-feeding should be identified and tested.
Based on clear evidence that, for many, infant feeding decisions are not firm even late into pregnancy, efforts to encourage women to breast-feed exclusively should be maintained throughout pregnancy with special emphasis on education about the attributes of breast-feeding as well as the benefits of exclusivity for at least 4 months.
Acknowledgements
Acknowledgements: The authors are grateful to the mothers who volunteered to participate in this study, as well as for the partnerships with Drs Maureen Phipps and Donna Parker, which made recruitment possible. They would also like to thank the Baby’s Breath study team members: Leslie Strolla, Norma Hardy, Catherine McMahon, Hilda Castillo, Yasmil Montes, Lauren Hubbard, Lizette Muriel, Dierdre Murphy and Kristen Delayo. Special thanks are owed to Thomas Lasater, PhD (deceased), the originator of the study. Financial support: This research was supported by the National Heart, Lung, and Blood Institute (NHLBI; grant number R01 HL070947-O1A). The NHLBI had no role in the design, analysis or writing of this article. Conflict of interest: None. Authorship: P.M.R. formulated the research questions, designed the study, and oversaw all conduct of the study and analysis. K.M. conducted analyses and contributed to interpretation and manuscript preparation. Ethics of human subject participation: The study was approved by the institutional review boards of Brown University, St. Joseph’s Hospital, the Memorial Hospital of Rhode Island (MHRI) and the Women’s Primary Care Center at Women and Infants’ Hospital (WIH).









