Optimal infant and young child feeding is an essential component in supporting the growth and development of children and is also a critical element in the global development initiative for a healthy, productive and sustainable world(1–3). A major facet of global infant and young child feeding recommendations is optimal breast-feeding, which is recognised as one of the most cost-effective interventions for reducing child mortality(Reference Victora, Bahl and Barros4). To promote optimal breast-feeding, the WHO and UNICEF jointly recommend: (i) early initiation of breast-feeding (EIBF) within one hour of birth; (ii) exclusive breast-feeding (EBF) for the first 6 months and (iii) continued breast-feeding (CBF) for 2 years and beyond(5–7). Despite these clear recommendations, in 2019, the WHO and UNICEF reported that only 43 % of children were breastfed within the first hour of birth, 41 % exclusively breastfed to 6 months and 45 % continued breast-feeding to 2 years(8).
Investment in breast-feeding is promoted as one of the greatest investments not only for the health and well-being of citizens but also for the economic development of a country(Reference Hansen9). The 2016 Lancet Breast-feeding Series indicates that increased breast-feeding could contribute USA$302 billion additional income per year, which is about 0·5 % of global gross national income(Reference Rollins, Bhandari and Hajeebhoy10). In addition, breast-feeding provides invaluable protection against childhood morbidity and mortality caused by infection, as well as probable reductions in non-communicable diseases including overweight and diabetes(Reference Victora, Bahl and Barros4). As a pragmatic action for protecting maternal and child health, breast-feeding has become a crucial element in addressing the 2030 Agenda for Sustainable Development(3). The major targets of achieving: (1) sustainable development goals; (2) zero hunger and (3) good health and well-being are to scale-up proven nutrition actions, including breast-feeding, as a means of reducing the burden of malnutrition, stunting and infectious disease among children(Reference Bhutta, Das and Rizvi11). These efforts were underscored when the UN recently revised its commitment to improve child nutrition, including a strong focus on increasing breast-feeding outcomes globally, through the United Nations Decade of Action on Nutrition(12).
Collectively, the ‘calls to action’ noted above, insight provided by the Lancet Breast-feeding Series, and movements such as The First 1000 d and Scaling Up Nutrition (SUN) have provided momentum to promote breast-feeding(3,Reference Victora, Bahl and Barros4,Reference Bhutta, Das and Rizvi11–14) . The Government of Bangladesh endorsed several initiatives to promote breast-feeding, including adopting the Baby Friendly Hospital Initiative, mother support groups and breast-feeding counselling among mothers(Reference Faruque, Ahmed and Ahmed15,16) . In Bangladesh, breast-feeding practices improved between 2000 and 2014, with the prevalence of EIBF and EBF increasing by 36 % and 13 %, respectively(17–20). Although previous studies have reported several predictors of EIBF and EBF in Bangladesh, including maternal BMI, education, location and mode of delivery(Reference Karim, Khan and Tasnim21–Reference Hossain, Islam and Kamarul24), little is known about CBF. In addition, a comprehensive trend analysis of these three breast-feeding indicators in Bangladesh is lacking. As such, the objective of this study was to investigate the trends and predictors of EIBF, EBF and CBF in Bangladesh between 2004 and 2018. This timeframe was selected to capture potential changes over both the United Nations Millennium Development Goals era (2000–2015) and the beginning of the United Nations sustainable development goals (2015–2030), in hopes of identifying future modifiable areas for action.
Methods
Our present study is based on the secondary analysis of publicly available data from five consecutive Bangladesh Demographic and Health Surveys (BDHS) of 2004, 2007, 2011, 2014 and 2017–2018. These nationally representative surveys were conducted by the National Institute of Population Research and Training in collaboration with ICF International and Mitra and Associates(17–20,25) . Data were collected from households following a two-stage stratified cluster sampling method (enumeration areas, then household samples). Detailed protocols for the sampling process, data collection procedures and questionnaires are available in the final reports of each BDHS(17–20,25) . Considering the outcome variables for our present analysis, we used completed data of 14 603 (weighted) women who were currently living with their youngest child aged 0–23 months.
Outcome measures
The outcome variables for our study were EIBF, EBF and CBF, which were defined according to WHO/UNICEF infant and young child feeding guidelines(26,27) . The method of collecting data and calculating breast-feeding indicators were same for all survey years(17–20,25) .
Early initiation of breast-feeding was defined as the proportion of children aged 0–23 months who were put to the breast within the first hour after birth, which was assessed from maternal recall. Mothers were asked ‘How long after birth did you first put (name of child) to the breast?’.
Exclusive breast-feeding was defined as the proportion of infants aged 0–5 months who were fed only human milk, which was captured by maternal recall of infant intakes in the 24 h preceding the survey. Per the UNICEF/WHO definition, infants were not considered exclusively breastfed if they consumed other food or drink (even plain water), but were considered EBF if oral rehydration salts, micronutrient drops or syrups or medicines were provided. Mothers were asked ‘Now I would like to ask you about liquids or foods that (name of child) had yesterday during the day or at night. I am interested in whether your child had the item I mentioned even if it was combined with other foods’ (responses were categorised as- Plain water? Juice or juice drinks? Yoghurt? Bread, rice, noodles, porridge or other foods made from grains? etc.).
Continued breast-feeding at 2 years was defined as the proportion of children aged 20–23 months who are fed breastmilk. Mothers were asked ‘Are you still breast-feeding (Name)?’.
Study variables
A two-level multilevel analysis was performed by grouping study variables into individual- and community-level variables.
Individual-level variables included child sex (male or female), birth order (1, 2, or 3+), mother’s age (15–24 years, 25–34 years or 35–49 years), mother’s education (no education, primary (5 years), secondary (10 years), or higher (≥ 11 years)), mother’s current working status (yes or no), number of antenatal care visits (no visits, 1–3 or 4+), place of delivery (home or health facility), mode of delivery (caesarean or vaginal), wealth index (poor (poorest + poorer), middle, or rich (richer + richest)), family size (≤ 4 or 5+) and sex of the head of household (male or female).
Community-level variables included place of residence (rural or urban) and geographical administrative divisions (Barisal, Chittagong, Dhaka, Khulna, Rajshahi, Rangpur, Sylhet or Mymensingh).
Data analysis
Data sets were cleaned before formal data analysis. Descriptive statistics including frequency and percent distribution and prevalence of EIBF, EBF and CBF for each data set (i.e., 2004, 2007, 2011, 2014 and 2017–2018) were computed according to DHS guidelines(Reference Croft, Marshall and Allen28). Pearson’s χ 2 test statistics were performed to assess associations between the prevalence of outcome variables (i.e. EIBF, EBF and CBF) and other study variables. The sampling weight provided by BDHS was applied in these analyses to ensure the acceptability of our results at the national level. The average annual average rate of change in the prevalence of outcome variables was calculated between two consecutive BDHS surveys and between 2004 and 2017–2018 via the equation Y t+n = Y t * (1 ± b %) n(29), where Y t = prevalence of EIBF/EBF/CBF of any given year ( t ), b = annual rate of change, n = number of years between two surveys and Y t+n = prevalence of EIBF/EBF/CBF of the ( t+n )th year. These are presented as an annual average rate of increase or annual average rate of reduction (AARR). A similar method was also used in earlier studies(Reference Hoque, Long and Niessen30,Reference Rahman, Rahman and Rahman31) .
To identify the factors associated with EIBF, EBF and CBF, we used the most recent data set (i.e. BDHS 2017–2018). Since BDHS data are hierarchical in nature (i.e. individuals (children) are nested within households, and households are nested within a higher level (clusters, termed enumeration areas in the BDHS)), the use of traditional logistic regression models could underestimate the standard errors of the effect sizes. With such data, it is assumed that children’s socio-economic characteristics are more likely to be similar within a cluster as compared with children from other clusters. This violates the assumption of standard model, independence of observation and equal variance across the clusters, which implies a need to consider cluster variability. With this, mixed effect multilevel modeling was employed to compute both fixed (both individual and community factors) and random (cluster variation) effects simultaneously. For our multilevel multivariable regression analyses, we fitted four models for each of the outcome variables (EIBF, EBF and CBF): Model I (null model) was fit without explanatory variables to assess the variance in the outcome of interest between clusters; Model II was fit for individual-level variables; Model III was fit for community-level variables and Model IV was fit for both individual- and community-level variables. The measure of community variations (random effect) was estimated as the intraclass correlation coefficient (ICC), and an ICC value of greater than zero was considered adequate to conduct multilevel modeling(Reference Park and Lake32). For measures of variations we also calculated median odds ratio and proportional change in variance(Reference Merlo33). Variables with P < 0·25 in the bivariate analysis were selected for multivariable analysis(Reference Agresti34). The effect of predictive variables (fixed effect) was measured using OR with 95 % CI. Akaike’s information criterion (AIC) was used to assess goodness of fit of each model. Multicollinearity between independent variables was checked using variance inflation factor (VIF); none of the variables showed multicollinearity problems (VIF < 10).
All statistical tests were two-sided and considered significant at P < 0·05 level. Data were analysed by using Stata v14.2 (StataCorp.).
Ethics
Since the present study was based on secondary data analyses of data obtained from the 2004, 2007, 2011, 2014 and 2017–2018 BDHS, ethical approval was not required. The data files are publicly available at (https://www.dhsprogram.com/). Formal ethical approval for all BDHS was obtained by ICF international, and participants provided free, informed consent.
Results
Background characteristics
A total of 14 603 mother–child paired data were extracted from five consecutive, publicly available BDHS data sets collected between 2004 and 2018. Demographic and socio-economic characteristics of study population are presented in Table 1. Pooled data indicate that 49 % of children were female, 59 % were delivered at home, 59 % of mothers were aged between 15 and 24 years, 29 % of mothers completed their primary education and 24 % lived in urban areas (pooled data not shown in the table).
Table 1. Background characteristics of the children aged 0–23 months and their families surveyed for Bangladesh demographic and health surveys*
(Number and percentages)

Weighted frequencies and percentages are reported after rounding.
* Wealth index was computed by principal component analysis based on household assets and materials used to build houses, using the national wealth index quintile provided in each data set.
Trend in early initiation of breast-feeding, exclusive breast-feeding and continued breast-feeding during 2004–2018
The prevalence of EIBF, by study year, is presented in Fig. 1. The overall prevalence of EIBF increased more than twofold during this time, from 25·9 % (95 % CI 23·8, 28·1) in 2004 to 60·4 % (95 % CI 58·3, 62·6) in 2017–2018. Figure 2 illustrates that the prevalence of EBF also increased during this time, from 35·9 % (95 % CI 32·2, 39·8) in 2004 to 67·5 % (95 % CI 64·1, 70·7) in 2017–2018. As shown in Fig. 3, continued breast-feeding up to 2 years decreased from 93·9 % (95 % CI 92·1, 95·3) in 2004 to 85·4 % (95 % CI 81·8, 88·4) in 2017–2018.

Fig. 1. Trends in early initiation of breast-feeding, within one hour of birth, in Bangladesh, 2004–2018 (error bars indicate 95 % CI).
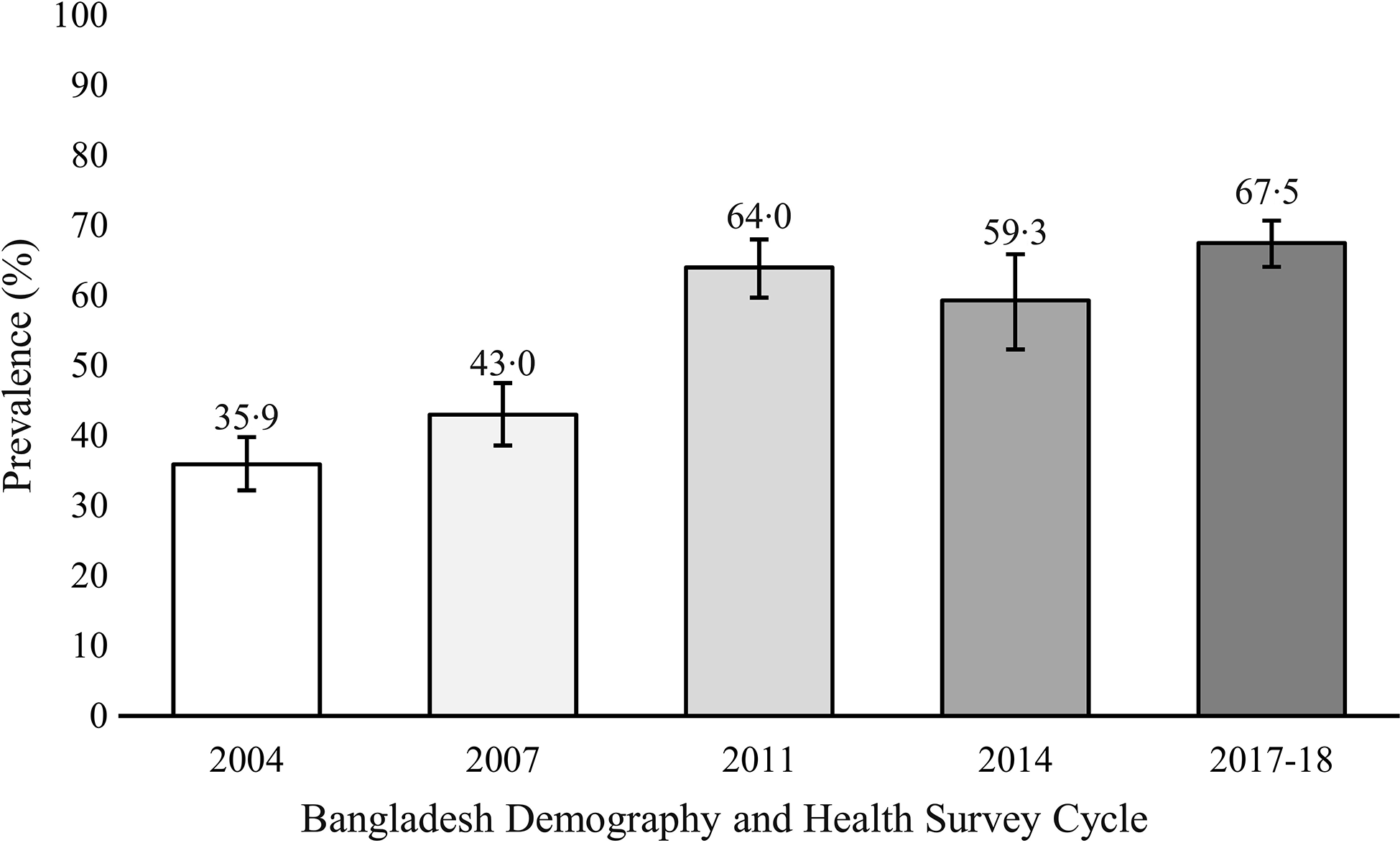
Fig. 2. Trends in exclusive breast-feeding to 6 months in Bangladesh, 2004–2018 (error bars indicate 95 % CI).

Fig. 3. Trends in continued breast-feeding to 2 years in Bangladesh, 2004–2018 (error bars indicate 95 % CI).
Table 2 shows average annual rate of change in breast-feeding indicators during 2004 to 2017–2018. EIBF and EBF showed an increasing trend; however, CBF showed a negative trend. Annual average rate of increase was highest for EIBF and EBF during 2004 to 2007 and 2007 to 2011, respectively. During our study period, an average annual rate of CBF decreased by 0·67 % (AARR = −0·67). Year wise prevalence of EIBF, EBF and CBF by individual- and community-level factors are presented in Supplemental Tables 1, 2, and 3, respectively.
Table 2. Average annual rate of change in the breast-feeding practices in Bangladesh 2004–2017/18

Positive values indicate an average annual rate of increase (AARI), while negative value indicates an average annual rate of reduction (AARR).
Predictors of early initiation of breast-feeding
As shown in Table 3, the null model (Model I) reveals that clustering exists in determining EIBF status. ICC value of null model indicates that 9 % of the variance in EIBF is a result of cluster variability. The final model (Model IV) showed the effect of community heterogeneity, suggesting that if a mother–child pair moved to a community with a higher probability of EIBF, the median increase in the odds of having EIBF would be 1·55-fold (median odds ratio = 1·55). Additionally, 36 % of the variance is the odds of EIBF across communities was explained by both individual- and community-level factors, as indicated by the proportional change in variance.
Table 3. Factors associated with early initiation of breast-feeding in Bangladesh, BDHS 2017–2018
(Odd ratio and 95 % confidence intervals)

Ref., reference category; se, standard error; ICC, intraclass correlation; PCV, proportional change in variance; MOR, median odd ratio; AIC, Akaike’s information criterion. Early initiation of breast-feeding was defined as the proportion of children aged 0–23 months who were put to the breast within the first hour after birth.
* P < 0·05, *** P < 0·001.
† Model I (Null model) was fitted without determinant variables.
‡ Model II is adjusted for individual-level variables only.
§ Model III is adjusted for community-level variables only.
‖ Model IV is the final model adjusted for both individual- and community-level variables.
The mode of delivery and geographic region (division) were significant predictors of EIBF. Infants born via Caesarean section were 66 % less likely to EIBF (OR = 0·34, 95 % CI 0·27, 0·42). Infants from Chittagong division were 29 % less likely to EIBF compared with Barisal division (OR = 0·71, 95 % CI 0·51, 0·98).
Predictors of exclusive breast-feeding
The predictors of EBF are presented in Table 4. The null model (Model I) indicates the existence of significant clustering (ICC = 14·54 %) which justifies multilevel analyses. The final model (Model IV) revealed that if a mother–child pair moved to a community with a higher probability of EBF, the median increase in the odds of having EBF would be 1·66-fold (median odds ratio = 1·66). Additionally, nearly half of the variance in the odds of EIBF across communities was explained by both individual- and community-level factors ( proportional change in variance = 48·21 %).
Table 4. Factors associated with exclusive breast-feeding in Bangladesh, BDHS 2017–2018
(Odd ratio and 95 % confidence intervals)

Ref., reference category; se, standard error; ICC, intraclass correlation; PCV, proportional change in variance; MOR, median odd ratio; AIC, Akaike’s information criterion. Exclusive breast-feeding was defined as the proportion of infants aged 0–5 months who were fed only human milk, excluding other food or drink (even plain water), but allowing for consumption of oral rehydration salts (ORS), micronutrient drops or syrups or medicines.
* P < 0·05, ** P < 0·01.
† Model I (Null model) was fitted without determinant variables.
‡ Model II is adjusted for individual-level variables only.
§ Model III is adjusted for community-level variables only.
‖ Model IV is the final model adjusted for both individual- and community-level variables.
Maternal working status was predictive of EBF, with mothers who were currently working being 32 % less likely to exclusively breastfeed their baby (OR = 0·68, 95 % CI 0·48, 0·95). Mothers who delivered at health facility and belong to larger household had a 1·81- and 1·70-times higher odds of exclusively breast-feeding, respectively. Geographic region (division) was also predictive of EBF.
Predictors of continued breast-feeding
In Table 5, the null model indicates the appropriate use of multilevel analysis (ICC = 26·47 %), suggesting that variation in CBF status may be attributed by cluster variation. The median odds ratio of 1·36 of the final model (Model IV) revealed the effect of community heterogenicity; however, the variance was not significant.
Table 5. Factors associated with continued breast-feeding in Bangladesh, BDHS 2017–2018
(Odd ratio and 95 % confidence intervals)

Ref, reference category; se, standard error; ICC, intraclass correlation; PCV, proportional change in variance; MOR, median odd ratio; AIC, Akaike’s information criterion. Continued breast-feeding to 2 years was defined as the proportion of children aged 20–23 months who were fed breastmilk. Continued breast-feeding to 2 years was defined as the proportion of children aged 20–23 months who were fed breastmilk.
† Model I (Null model) was fitted without determinant variables.
‡ Model II is adjusted for individual-level variables only.
§ Model III is adjusted for community-level variables only.
‖ Model IV is the final model adjusted for both individual- and community-level variables.
** P < 0·01.
*** P < 0·001.
Urban v. rural residence was the only significant predictor of CBF in our analysis. Children residing in rural Bangladesh had 2·39-fold higher odds (95 % CI 1·32, 4·31) of continued breast-feeding to 2 years compared with their urban counterparts.
Discussion
This study investigated the trends and predictors of EIBF, EBF and CBF in Bangladesh by analyzing five consecutive, publicly available, nationally representative BDHS data sets from 2004 through 2017–2018. We presented the results in individual (child, maternal and household) and community-level factors as a means of identifying potential modifiable factors to improve EIBF, EBF and CBF in Bangladesh.
There have been several calls to action to increase breast-feeding rates globally. For instance, UNICEF stated that breast-feeding could play a key role in achieving many of the SDG focused not only on hunger and health but also those goals to address poverty, economic growth, inequalities, education and sustainability(3). Beyond meeting these global goals, breast-feeding has the potential to address child mortality: as part of the 2016 Lancet Breast-feeding Series, an estimated 823 000 under five deaths could be averted annually by near-universal scaling up of breast-feeding(Reference Victora, Bahl and Barros4). We found that Bangladesh has made remarkable progress in increasing the rates of early initiation (25·9 % to 60·4 %) and exclusive (35·9 % to 67·5 %) breast-feeding between 2004 and 2018. According to the most recent data (i.e. BDHS 2017–2018), the prevalence of EIBF and EBF of 60·4 % and 67·5 % in Bangladesh was higher than neighbouring India (2015–2016 DHS: EIBF – 42 % and EBF – 55 %)(35) and Nepal (2016 DHS: EIBF – 55 % and EBF – 65 %)(36). CBF rates were already impressive during the period between 2004 and 2018, but did experience a slight decrease (93·9 % to 85·4 %). Prevalence of CBF is high in the South Asia region: 85 %, 90 % and 74 % in Bangladesh (2017–2018), Nepal (2016) and India (2015–2016), respectively(25,35,36) . Although not the focus of this analysis, improvements in these key breast-feeding indicators can likely be linked to recent efforts to scale-up interventions like breast-feeding counselling, mass media campaigns and other education programmes throughout South Asia(Reference Benedict, Craig and Torlesse37).
Several modifiable demographic factors were significant predictors of the breast-feeding indicators of interest in the 2017–2018 data set. The greatest increase in EIBF was seen between the period of 2004 and 2007, with an increase of 19 %, with only modest gains in the subsequent years assessed. Mode of delivery is an acknowledged predictor for EIBF; a systematic review and meta-analysis reported that the rates of EIBF were 43 % lower after the Caesarean delivery as compared with vaginal delivery(Reference Prior, Santhakumaran and Gale38). Failure to initiate breast-feeding within the recommended hour after birth has been attributed to time required for recovery from anaesthesia and other surgical procedures(Reference Duodu, Duah and Dzomeku39). Caesarean delivery could be a key factor halting the breast-feeding initiation in Bangladesh, as we found that Caseation section delivery reduced the likelihood by of EIBF by 66 % as compared with the vaginal delivery. The 2014 BDHS reported that 24·3 % of infants were born via Caesarean delivery(20), with another report suggesting an alarming number of unnecessary Caesarean deliveries, which increased by 51 % between 2016 and 2018(40). Non-medically indicated Caesarean delivery should be avoided both to support breast-feeding initiation, but also safeguard both mother and infant health. However, promotion of early skin-to-skin contact (Kangaroo care), both among vaginal and Cesarean section deliveries, could increase EIBF(Reference Singh, Khan and Carvajal–Aguirre41). Similar to other research(Reference Prior, Santhakumaran and Gale38), Caesarean delivery was not a significant predictor of EBF in Bangladesh.
It is important to note that socio-economic characteristics changed over the 14-year period (2004–2018) of this study. For instance, the prevalence of maternal employment increased by ∼20 percentage points between 2004 and 2018, which could have affected breast-feeding practices among working mothers. We found that, overall, working mothers were 32 % less likely to EBF (0·68 (95 % CI 0·48, 0·95)). Our findings are consistent with a study in Ghana that identified two key factors for exclusive breast-feeding – breast-feeding knowledge and maternal workplace factors such as office hours, company policy on maternal leave, unfavourable institutional policies and work-life balance(Reference Abekah-Nkrumah, Antwi and Nkrumah42). A qualitative study in urban Bangladesh reported that increased workload, lack of day-care facilities within workplaces and a lack of caregivers at home were all major barriers to breast-feeding exclusivity among working mothers(Reference Hasan, Smith and Selim43). Similar barriers have also been identified in China, where mothers who experienced either inadequate employment benefits, longer commute times to work, unfavourable workplace environments and increased labour intensity work would reduce the breast-feeding frequency or cease breast-feeding altogether(Reference Chen, Xin and Gaoshan44). This inverse relationship between maternal employment status and breast-feeding is a global phenomenon(Reference Çiftçi and Arikan45), so efforts towards workplace lactation support programmes are warranted. These programmes not only improve breast-feeding outcomes but also lower absenteeism and increase job satisfaction(Reference Wyatt46). In the present study, mothers who delivered in a healthcare facility were 1·81 times more likely to EBF compared with the home delivery. Delivery at a healthcare facility is a well-established predictor of EBF, as trained healthcare professionals can provide education and support to mothers to assist with establishing breast-feeding soon after birth(Reference Alebel, Tesma and Temesgen47). Furthermore, we found that larger family size (5+ members) predicted a 1·7 times higher odds for EBF, which is consistent with previous research(Reference Manyeh, Amu and Akpakli48).
With regard to CBF to 2 years, we found that rural residents had a 2·39 times higher likelihood of continued breast-feeding than urban residents. Although previous studies have explained such differences by higher maternal employment in the cities and more widespread availability and financial access to human milk substitutes in urban centres(Reference Kavle, LaCroix and Dau49,Reference Thu, Eriksson and Khanh50) , maternal employment was not a significant predictor in our models. Of note, only modest changes in CBF were found across the survey period (<1 %, see Table 2).
The trends for a number of socio-economic characteristics factors changed over the 14 years encompassing these five national data sets; however, these changes did not always impact breast-feeding outcomes as anticipated. For example, maternal education is a well-established predictor of breast-feeding(Reference Neves, Barros and Gatica-Domínguez51). In this analysis, the proportion of women with no education decreased from 33 % to 6 % between the 2004 and 2017–2018 surveys; however, maternal education was not a significant predictor of any of the breast-feeding outcomes. Similarly, although the prevalence of the number of antenatal care visits increased over time, we could hypothesise that interaction with healthcare providers could improve breast-feeding outcomes. However, we did not find the number of Antenatal Care (ANC) visits is a significant breast-feeding predictor. These null results underscore the importance of country-specific analyses to understand the drivers of breast-feeding in specific contexts. Future research should explore why such predictors in other settings do not translate to this Bangladeshi context.
A major strength of this study is the analysis of five consecutive, nationally representative data sets over 14 years. This allowed us to track the progress and identify factors that influence EIBF, EBF and CBF, as well as to identify the gaps for future consideration. Another strength is the consistent data collection methods and terminology/definitions of EIBF, EBF and CBF used in all our analysed data sets. This study has a number of limitations. A major limitation of this study is the data; with consecutive, cross-sectional data collection, no causal relationships can be established, and it is possible that reverse temporal relationships or bidirectional relations could emerge. We thus advise caution in interpretation. Our analyses are also subject to residual confounding bias because these publicly available, secondary data from five consecutive demographic and health surveys may not have collected all potential factors that could have influenced breast-feeding practices in Bangladesh. Another challenge of the study was to generate generalised results (pooled analysis) from five cumulative time points (2004–2017/20) as socio-economic characteristics have changed considerably over this 14-year period. We therefore used the latest 2017–2018 data set to establish association across variables.
Conclusion
Rates of EIBF and EBF have been increasing since 2004, and Bangladesh has already achieved the World Health Assembly Resolution 65·6 to increase the rate of EBF to 50 % by the year 2025(52). While CBF rates have decreased slightly since 2004, 85 % of Bangladeshi children still meet the WHO recommendation of continued breast-feeding to 2 years. The major significant predictors of optimal breast-feeding outcomes include vaginal delivery, mother not working, delivery at healthcare facility, larger family size and rural residency. There is also indication of geographic differences across Bangladesh, which warrants further investigation.
Acknowledgements
The authors wish to acknowledge the authority of the National Institute of Population Research and Training (NIPORT), Bangladesh, for providing access to the data sets used in this study.
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
M. S. A. and F. M. Y. formulated the research question and designed the study; M. S. A. analysed the data; M. S. A., F. M. Y. and K. C. W. interpreted the findings and wrote the article. All authors read and approved the final manuscript.
There are no conflicts of interest.
Supplementary material
For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S0007114521004761











