Introduction
Evidence suggests that conduct problems (i.e., violations of age-appropriate societal norms including fighting and threatening behaviors (Girard et al., Reference Girard, Tremblay, Nagin and Côté2019)) are partially predicted by previous head injuries (a bang on the head with or without a loss of consciousness (Davis & Ings, Reference Davis and Ings2015; Yates et al., Reference Yates, Williams, Harris, Round and Jenkins2006)) and vice versa (Brandt et al., Reference Brandt, Hall, Eisenbarth and Hall2022; Carr et al., Reference Carr, Hall, Eisenbarth and Brandt2023). However, despite the high prevalence of childhood head injuries (33%–55% of the 1.4 million head injury admissions in the UK (National Clinical Guideline Centre, 2014)), the link between conduct problems and head injuries over time and the risks associated with their co-occurrence are vastly under researched (McKee & Daneshvar, Reference McKee and Daneshvar2015) compared to the association between traumatic brain injuries (TBI) and conduct problems (Bellesi et al., Reference Bellesi, Barker, Brown and Valmaggia2019).
Research indicates that there are distinct developmental pathways to conduct problems (Gutman et al., Reference Gutman, Joshi and Schoon2019) and head injuries (Keenan et al., Reference Keenan, Clark, Holubkov, Cox, Patel, Moore and Ewing-Cobbs2020). The DSM-5 describes two conduct disorder pathways: childhood-onset (presentation before age 10) and adolescent-onset (presentation after age 10 (Diagnostic and statistical manual of mental disorders, 2013)). While further research suggests an additional childhood-limited high conduct problems pathway (Gutman et al., Reference Gutman, Joshi and Schoon2019). Similarly, head injuries have developmental pathways based on their initial severity and impact on infant cognition (Keenan et al., Reference Keenan, Clark, Holubkov, Cox, Patel, Moore and Ewing-Cobbs2020).
The consequences of both conduct problems and head injuries are well known and include increased likelihood of delinquency and criminal behavior (Kennedy et al., Reference Kennedy, Heron and Munafò2017; Mongilio, Reference Mongilio2022). A better understanding of how their pathways link during development is therefore important for intervention and prevention practices aimed at jointly reducing both. To create effective intervention and prevention practices we need to not only understand how conduct problems and head injuries link but also the risk factors for these links (e.g., childhood maltreatment may increase the risk for developmentally stable high risk of both head injuries and conduct problems).
The bidirectional association between childhood head injuries and conduct problems has been previously linked to cumulative risk at the child, mother, and household levels, such as alcohol consumption during pregnancy, mother psychological distress, and a low income household (Carr et al., Reference Carr, Hall, Eisenbarth and Brandt2023). In turn, cumulative risk indices (CRIs) are commonly used to inform interventions and prevention policies (Hogye et al., Reference Hogye, Lucassen, Jansen, Schuurmans and Keizer2022). Negative parenting styles (i.e., harsh, avoidant, and abusive parenting) have been associated with increased conduct problems (Hukkelberg & Ogden, Reference Hukkelberg and Ogden2021; Speyer et al., Reference Speyer, Hang, Hall and Murray2022) and could create increased opportunities to sustain a head injury (Schnitzer et al., Reference Schnitzer, Dowd, Kruse and Morrongiello2015). These associations, however, are yet to be investigated in a model of both head injuries and conduct problems.
The current study thus investigates distinct development pathways linking conduct problem symptoms and head injuries between early childhood and adolescence. By drawing on secondary data from a longitudinal cohort study, it provides an in-depth perspective on the patterns of linked head injury and conduct problems symptoms across development that is not possible from a cross-sectional design. We utilized latent class modeling on this longitudinal dataset to reveal the different pathways linking head injury and conduct problem symptoms from ages 3 to 17 years. It further elaborates to identify if distinct developmental pathways are associated with accumulated risks at the child, mother, and household levels, such as alcohol consumption during pregnancy, mother psychological distress, and a low-income household, as well as negative parenting styles.
Methods
Participants
The Millennium Cohort Study (MCS; https://www.cls.ioe.ac.uk/mcs) is an ongoing longitudinal UK birth cohort of 18,786 individuals born in the UK, aged 9 months at the first measurement timepoint (T1) between 2000 and 2002 (Fitzsimons et al., Reference Fitzsimons, Haselden, Smith, Gilbert, Calderwood, Agalioti-Sgompou, Veeravalli, Silverwood and Ploubidis2020). Participants were studied at six further timepoints at the ages of 3 (T2), 5 (T3), 7 (T4), 11 (T5), 14 (T6), and 17 years (T7). For this study, we included participants who completed the last wave at age 17, who were first-born children, whose main respondent in the study was their biological mother, and who had complete CRI data (N = 8,600; 4,320 female [50.2%]; 7,136 [83%] ‘White British’). For more information and justifications for these exclusions and for the participant flow chart see supplementary materials, Appendix A and Figure S1 respectively.
Written informed consent was provided to the MCS by the parent of each child. Ethical approval for this analysis was given by the University of Southampton Ethics Committee (ID = 62100). This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for cohort studies.
Measures
Conduct problem symptoms
Conduct problem symptoms were parent-reported at T2 (age 3) to T7 (age 17), using the five items from the Strength and Difficulties Questionnaire (SDQ) Conduct Problem Subscale (Goodman, Reference Goodman2001). This subscale is widely used as a reliable and valid measure of conduct problems and externalizing behavior (Patalay & Hardman, Reference Patalay and Hardman2019; Zendarski et al., Reference Zendarski, Mensah, Hiscock and Sciberras2021). The items were coded from 0 (not true) to 2 (certainly true) and were summed to create a total score at each timepoint (possible range: 0 – 10). Based on the newer 4-band categorization, scores reflect the following levels of conduct problems: 0–2 = “close to average,” 3 = “slightly raised,” 4–5 = “high” (clinically relevant), and 6–10 = “very high” (clinically relevant; see www.sdqinfo.org).
Head injuries
Head injuries were parent-reported from T2 (age 3) to T6 (age 14). Parents reported their child sustaining a “bang to the head” or “loss of consciousness after bang to the head.” Uniting both responses regarding head injury was a replication of the head injury variables created in previous published MCS analyses (Brandt et al., Reference Brandt, Hall, Eisenbarth and Hall2022; Carr et al., Reference Carr, Hall, Eisenbarth and Brandt2023; Mongilio, Reference Mongilio2022).
Though head injuries were reported at T1 these were not included due to the temporal ordering of the risk factors below.
Potential risk factors
Risk factors were distinguished across three levels (child, mother, and household) and were assessed via the creation of CRIs (Bronfenbrenner, Reference Bronfenbrenner1977). CRIs refer to the summation of risk factors. That is, each risk factor is dichotomized and then summed to emphasize volume of risk rather than individual relationships of risk factors (Hall et al., Reference Hall, Sammons, Sylva, Melhuish, Taggart, Siraj and Smees2010; Rutter, Reference Rutter1979). The factors included in the CRIs replicate those used previously in the modeling of the bidirectional association between conduct problems and head injuries (Carr et al., Reference Carr, Hall, Eisenbarth and Brandt2023).
At each ecological level, five potential risks for conduct problems and/or head injuries were identified and labeled as either “present” or “high risk” (1), as compared to “absent” or “low risk” (0). The high-risk thresholds were informed by previous literature (see below). These risks were summed to create the three CRIs (score ranging from 0–5 at each level):
Child-level risks. Potential risks included: low birth weight (<2.5 kg) and premature birth (<=252 days gestation (Reijneveld et al., Reference Reijneveld, de Kleine, van Baar, Kollée, Verhaak, Verhulst and Verloove-Vanhorick2006; Whiteside-Mansell et al., Reference Whiteside-Mansell, Bradley, Casey, Fussell and Conners-Burrow2009)), male sex (Fullerton et al., Reference Fullerton, Jackson, Tuvblad, Raine and Baker2019; McKinlay et al., Reference McKinlay, Kyonka, Grace, Horwood, Fergusson and MacFarlane2010), and whether the child’s biological mother smoked or drank alcohol during pregnancy (Van Adrichem et al., Reference Van Adrichem, Huijbregts, Van Der Heijden, Van Goozen and Swaab2020). These were all measured at T1.
Mother-level risks. Potential risks included: unemployment (Van Adrichem et al., Reference Van Adrichem, Huijbregts, Van Der Heijden, Van Goozen and Swaab2020), no high-school qualification (Greitemeyer & Sagioglou, Reference Greitemeyer and Sagioglou2016; Trentacosta et al., Reference Trentacosta, Hyde, Shaw, Dishion, Gardner and Wilson2008; Van Adrichem et al., Reference Van Adrichem, Huijbregts, Van Der Heijden, Van Goozen and Swaab2020), pregnancy before age 18 (McKinlay et al., Reference McKinlay, Kyonka, Grace, Horwood, Fergusson and MacFarlane2010; Trentacosta et al., Reference Trentacosta, Hyde, Shaw, Dishion, Gardner and Wilson2008), low attachment with child (<= 22 on the Condon Maternal Attachment Scale; six 5-point items [1 = “almost all the time”; 5 = “never”] summed; (Condon & Corkindale, Reference Condon and Corkindale1998; Curran et al., Reference Curran, Cryan, Kenny, Dinan, Kearney and Khashan2016), and high maternal psychological distress (>=4 on Rutter Malaise Inventory; nine binary items [0 = “no”; 1 = “yes”] summed (McKinlay et al., Reference McKinlay, Kyonka, Grace, Horwood, Fergusson and MacFarlane2010; Rutter et al., Reference Rutter, Tizard and Whitmore1970)). These were all measured at T1.
Household-level risks. Potential risks included: low household occupational status (semi-skilled or lower; (Greitemeyer & Sagioglou, Reference Greitemeyer and Sagioglou2016), low household income (< 60% of median household income (Northerner et al., Reference Northerner, Trentacosta and McLear2016; Trentacosta et al., Reference Trentacosta, Hyde, Shaw, Dishion, Gardner and Wilson2008)), single parent household (Northerner et al., Reference Northerner, Trentacosta and McLear2016; Trentacosta et al., Reference Trentacosta, Hyde, Shaw, Dishion, Gardner and Wilson2008), household overcrowding (fewer rooms than people (Northerner et al., Reference Northerner, Trentacosta and McLear2016; Trentacosta et al., Reference Trentacosta, Hyde, Shaw, Dishion, Gardner and Wilson2008)), and low-quality home learning environment (bottom quartile of the (early) Home Learning Environment scale [HLE] (Sylva et al., Reference Sylva, Melhuish, Sammons, Siraj-Blatchford and Taggart2004)). The (early) HLE scale was comprised of six items that assessed the frequency of child engagement in early learning activities such as being read to. The items were scored from 0 (not at all) to 7 (every day) and summed (possible range: 0–42). A higher score indicated a higher quality home learning environment. All were measured at T1 except for the (early) HLE, which was measured at T2.
ADHD
ADHD is a risk factor due to its comorbidity with conduct problems (Gnanavel et al., Reference Gnanavel, Sharma, Kaushal and Hussain2019) and sustaining a head injury (Ramos Olazagasti et al., Reference Ramos Olazagasti, Klein, Mannuzza, Belsky, Hutchison, Lashua-Shriftman and Castellanos2013). ADHD was measured by parents reporting if their child had received an ADHD diagnosis between T3 to T6 (age 5–14). A binary variable was created (0 = no diagnosis, 1 = diagnosis of ADHD).
Epilepsy
Epilepsy is a risk factor due to its comorbidity with conduct problems (Lin et al., Reference Lin, Mula and Hermann2012) and sustaining a head injury (Annegers & Coan, Reference Annegers and Coan2000). Epilepsy was measured by parents reporting if their child had received an epilepsy diagnosis between T2 to T6 (ages 3–14). A binary variable was created (0= no diagnosis, 1 = diagnosis of epilepsy).
Negative parenting styles
Negative parenting styles were measured at T3 (age 5) using the Parent-Child Conflict Tactic Scale (Straus et al., Reference Straus, Hamby, Finkelhor, Moore and Runyan1998). This measures how often the mother engages in harsh parenting (smacking, shouting at, and telling off) and withdrawal tactics (ignoring, sending to room, or taking away toys). Mothers were asked to report the frequency of these behaviors on a 5-point Likert scale ranging from 1 (never) to 5 (daily). The three items for each parenting style were summed to create a score (possible range: 3–15). A higher score indicated harsher parenting or greater levels of withdrawal.
Statistical analysis
Analyses were conducted using Mplus v7.4 (Muthén & Muthén, Reference Muthén and Muthén2017). Latent class analysis was used to identify distinct development pathways linking conduct problem symptoms and head injuries from 3 to 17 years. The first step was to identify the optimum number of classes starting with a two-class model and increasing the number of classes until the solution that best fitted the data was found. This was established by comparing model fit indices between competing potential solutions (Weller et al., Reference Weller, Bowen and Faubert2020) and interpretability (see supplementary materials, Appendix B).
Missing data from T2 to T6 were accounted for by using Full Information Maximum Likelihood (FIML).
MCS sample weights from T7 were included (accounting for stratification, nonresponse bias, and attrition) to facilitate generalization of findings to the UK population. ADHD, epilepsy, and three CRIs at the child, mother, and household level were included in the analysis and were tested for their association with an individual’s distinct developmental pathway via multinomial logistic regression. Post hoc analyses further probed if negative parenting styles (harsh parenting or withdrawal tactics) at T3 were associated with class membership (see supplementary materials, Appendix C). Though exclusions were applied to the sample (refer to supplementary materials, Appendix A and Figure S1), additional analysis without these exclusions was completed on the final class solution to ensure the exclusions did not alter the interpretability of the linked pathways identified.
Data availability
The MCS data that support the findings of this study are openly available at the UK Data Service (https://discover.ukdataservice.ac.uk/series/?sn = 2000031). To access the data, one must register to the UK Data Service and submit a data request.
Results
Participants and demographics
Sample characteristics, variable differences between the analytical and excluded sample, and information on missing data can be seen in Table 1. Though there were significant differences between the included and excluded samples these effects were typically small (Cohen’s d effect sizes: −.02–.18; Cramér’s V effect sizes: .03–.10).
Table 1. Sample characteristics and differences between the analytical and excluded samples

If n totals less than 8,600 or 10,186, respectively, this indicates missing data.
a Independent t-test.
b Cohen’s D.
c As measured by the Parent-version of the Strengths and Difficulties Questionnaire Conduct Problem Subscale.
d As measured by parent reports of accidents resulting in a bang to the head with or without a loss of consciousness.
Identification of distinct linked developmental pathways
Upon comparison of latent class models with two-five classes, a 4-class solution appeared to best fit the MCS data based on model fit (see Table 2) and interpretability.
Table 2. Model fit indices of a latent class analysis of conduct problems and head injuries
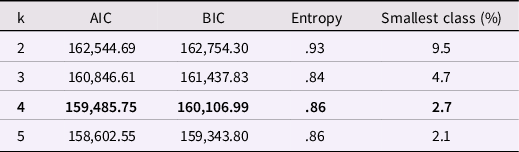
AIC = Akaike’s information criterion; BIC = bayesian information criterion; K = classes.
Bold typeset indicates final class solution.
The 4-class solution identified four distinct and interpretable classes of linked conduct problem symptoms (Fig. 1a) and head injuries (Fig. 1b). The first class (n = 6,422 [74.7%]) was labeled stable low-level conduct problem symptoms and head injuries. Members of this class were characterized by consistent “close to average” levels of conduct problem symptoms as well as low levels of head injuries at all waves. The second class (n = 1,422 [16.5%]) was labeled childhood-only high conduct problem symptoms and head injuries. Members of this class presented with “high” levels of conduct problem symptoms at age 3, which declined into the lower range by age 7. Similarly, levels of head injury were highest at age 3, declining until age 14. The third class (n = 567 [6.6%]) was labeled high adolescent conduct problem symptoms and childhood onward head injuries. Members of this class showed “high” levels of conduct problem symptoms from age 14 to 17 as well as an increase in head injuries from age 11 to 14. The fourth class (n = 189 [2.2%]) was labeled persistent high conduct problem symptoms and childhood-limited head injuries. Members of this class showed persistently “slightly raised” to “very high” levels of conduct problem symptoms and the highest level of head injuries from ages 3 to 17 with a particular increase in head injuries during ages 7 and 11.
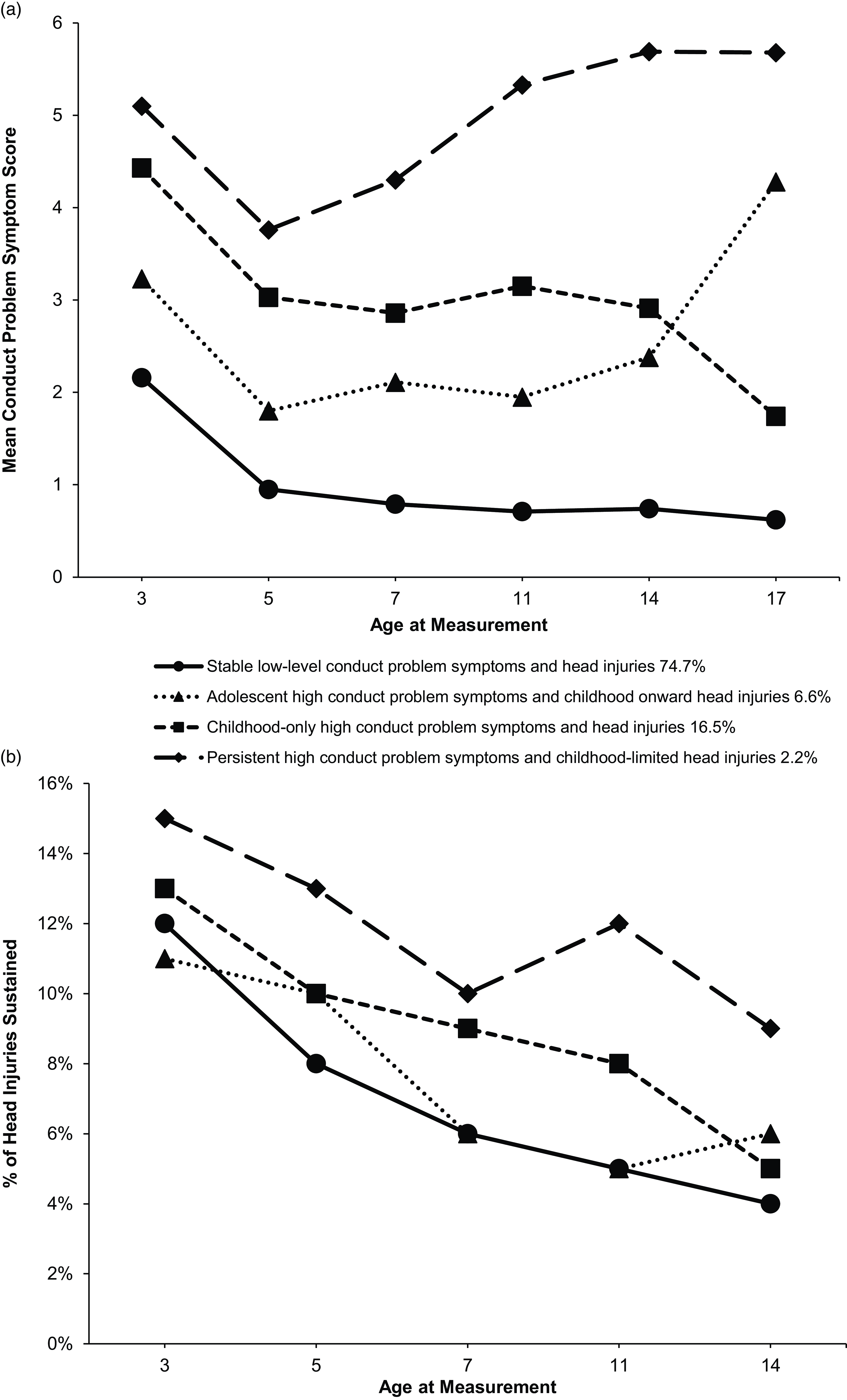
Figure 1. A figure of the linked pathways of mean conduct problem symptoms and head injuries at each timepoint for the 4-class solution. This figure shows the linked pathways of ( a ) mean conduct problem symptoms and ( b ) frequency of head injuries within the 4-class solution where conduct problem symptoms were measured using the conduct problem subscale of the SDQ and head injuries were parent-reported based on a history of a bang on the head with or without a loss of consciousness. The circles represent the “typically developing” group with low levels of conduct problem symptoms and sustained head injuries. The squares represent those with higher early levels of conduct problems symptoms and head injuries, which decline during development. The triangles represent those with low early levels of conduct problem symptoms and head injuries which both begin to rise from late childhood to adolescents. The diamonds represent persistently higher levels of head injuries and conduct problem symptoms.
Classes two to four indicated distinct developmental pathways that were deemed to be "clinically relevant" due to the levels of conduct problem symptoms shown by their members in accordance with the SDQ categorizations (see Methods).
Supplementary analysis identified a similar 4-class solution when no exclusions were applied to the sample (see supplementary materials, Figure S2).
Association between distinct linked developmental pathways and potential risk factors
Multinomial logistic regression showed that higher scores on all three CRIs were generally associated with a greater likelihood of a child belonging to a clinically relevant developmental pathway compared to the stable low-level conduct problem symptoms and head injuries pathway (see Table 3). The only exception being the mother-level, which showed no evidence of an association with the adolescent-onset pathway (class 3).
Table 3. Multinomial logistic regression of the associations with class membership
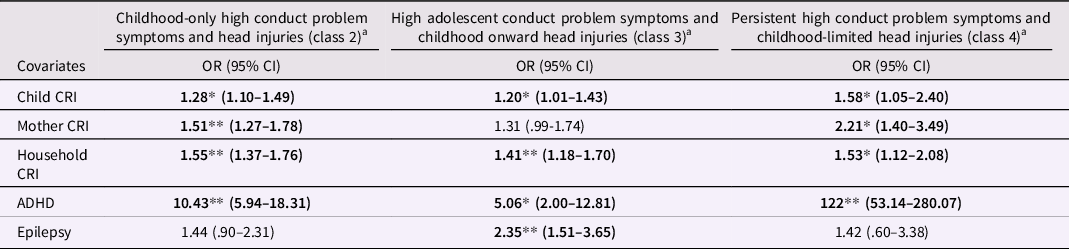
OR = odds ratio; CRI = cumulative risk index.
a versus stable low-level conduct problem symptoms and head injuries (class 1).
* p < .05.
**p < .001.
Compared to the stable low-level conduct problem symptoms and head injuries pathway, ADHD had a strong association with all the clinically relevant classes (see Table 3), while epilepsy was only significantly associated with the adolescent-onset class (see Table 3).
Association between distinct linked developmental pathways and maternal negative parenting styles
Post hoc multinomial logistic regression revealed that both greater use of maternal withdrawal tactics and harsh parenting at age 5 was significantly associated with a child’s membership to all three clinically relevant developmental pathways compared to the stable low-level conduct problem symptoms and head injuries pathway. Maternal withdrawal tactics and harsh parenting were most strongly associated with the persistent pathway (OR = 1.33, 95% CI: 1.14–1.54; OR = 1.38, 95%CI: 1.22–1.56, respectively) followed by the child-limited pathway (OR = 1.28, 95% CI: 1.20–1.35; OR = 1.26, 95%CI: 1.19–1.34, respectively) and most weakly associated with the adolescent-onset pathway (OR = 1.09, 95% CI: 1.01–1.17; OR = 1.16, 95%CI: 1.09–1.24, respectively).
Discussion
This study identified four distinct developmental pathways linking conduct problem symptoms and head injuries between early childhood and adolescence (between 3 and 17 years). As expected, the majority of the sample (75%) displayed low levels of conduct problem symptoms and a low likelihood for head injuries from 3 to 17 years (class 1). However, three clinically relevant pathways were identified. Seventeen percent displayed clinically relevant levels of conduct problem symptoms and an elevated risk for head injuries in childhood, but both declined after childhood (child-limited; class 2). A further 6% developed clinically relevant levels of conduct problem symptoms in adolescence and showed an elevated risk of head injuries from ages 11 to 14 (adolescent-onset; class 3). The final 2% displayed consistently high levels of conduct problem symptoms across development and displayed the highest rates of head injury with a particular sharp increase during ages 7–11 (persistent; class 4). The three developmental pathways show patterns of clinically relevant conduct problem symptoms that are consistent with the DSM-5’s conduct disorder classifications (Diagnostic and statistical manual of mental disorders, 2013) and conduct disorder pathways previously identified within the MCS dataset (Gutman et al., Reference Gutman, Joshi and Schoon2019). These results, however, provide new insight into how such developmental pathways of conduct problem symptoms link with pathways of head injuries. It teases apart the previously identified bidirectional association between conduct problems and head injuries (Carr et al., Reference Carr, Hall, Eisenbarth and Brandt2023) and suggests that this bidirectional association may not be relevant to all individuals but to specific subsets of individuals at different periods from early childhood to adolescence.
Though three clinically relevant pathways were identified, emphasis should be placed on the linked pathways of classes 3 (adolescent-onset) and 4 (persistent). These are the only two classes to display increasing levels of conduct problem symptoms in adolescents and increasing levels of head injuries during development. These characteristics are associated with an increased risk for adolescent delinquency (Kennedy et al., Reference Kennedy, Heron and Munafò2017; Mongilio, Reference Mongilio2022) and greater odds of problematic behaviors in adulthood (Bevilacqua et al., Reference Bevilacqua, Hale, Barker and Viner2018). Taken together, these features, thus, suggest the need for prevention work to stop individuals from entering these clinically relevant developmental pathways.
Such preventions may target risk factors associated with membership of these pathways. ADHD was highly associated with all clinically relevant pathways and most strongly with the class displaying persistent conduct problem symptoms (class 4). This finding is unsurprising due to ADHD’s strong association with conduct problems (particularly persistent or child-onset conduct problems (Fairchild et al., Reference Fairchild, Hawes, Frick, Copeland, Odgers, Franke, Freitag and De Brito2019; Silberg et al., Reference Silberg, Moore and Rutter2015)) and head injuries (Ramos Olazagasti et al., Reference Ramos Olazagasti, Klein, Mannuzza, Belsky, Hutchison, Lashua-Shriftman and Castellanos2013), as well as interactions between ADHD and harsh parenting (Golm & Brandt, Reference Golm and Brandt2023). The strength of the association provides further support for the relevance of interventions to manage conduct disorder with comorbid ADHD, e.g., psychosocial intervention for the conduct disorder symptoms and stimulant medication for the ADHD symptoms (Fairchild et al., Reference Fairchild, Hawes, Frick, Copeland, Odgers, Franke, Freitag and De Brito2019). By doing so, such interventions may also inadvertently reduce the risk of sustaining a head injury during development and the associated implications of this.
It must be noted that whilst ADHD was strongly associated with group membership it is important to acknowledge potential sex differences. That is, males have a stronger association with both conduct disorder and co-morbid ADHD (Fairchild et al., Reference Fairchild, Hawes, Frick, Copeland, Odgers, Franke, Freitag and De Brito2019; Konrad et al., Reference Konrad, Kohls, Baumann, Bernhard, Martinelli, Ackermann, Smaragdi, Gonzalez-Madruga, Wells, Rogers, Pauli, Clanton, Baker, Kersten, Prätzlich, Oldenhof, Jansen, Kleeven, Bigorra and Freitag2022). These sex differences could play a role in the associations that ADHD shares with these linked developmental pathways and the development of the pathways themselves. Whilst for the purpose of this research, we aimed to provide a novel understanding of how head injuries and conduct problem symptoms co-occur across development irrespective of sex (and other potential confounders), future research may wish to look at how the identified linked developmental pathways differ between males and females and how sex may influence potential risk factors associated with pathway membership (particularly with reference to the role of ADHD). This could provide important findings that will further aid the development of such interventions as those proposed above and their appropriate target population.
Our findings further suggest that early (by age 3) accumulation of risk at the child, mother, and household-level (Carr et al., Reference Carr, Hall, Eisenbarth and Brandt2023) are associated with membership to the clinically relevant classes, again replicating that of previous literature (Gutman et al., Reference Gutman, Joshi and Schoon2019). For the persistent pathway (class 4), the strongest association of cumulative risk was at the mother-level. This supports previous literature, which identifies mother-level risk as strongly associated with a risk for both persistent conduct problems (Gutman et al., Reference Gutman, Joshi and Schoon2019) and head injuries (McKinlay et al., Reference McKinlay, Kyonka, Grace, Horwood, Fergusson and MacFarlane2010). Thus, preventions that might reduce the likelihood of individuals entering this development pathway might aim to primarily reduce undesired maternal unemployment, (potential future) mothers leaving high school with no qualifications, pregnancies before 18 years, low mother attachment with child, and high maternal psychological distress. Future research might determine which of these risk factors are particularly important, in order to develop targeted interventions, such as early support for mother-child attachment for mothers experiencing mental health difficulties.
While the mother-level was the strongest accumulated risk for the persistent pathway, there was no evidence for an association between the mother-level and the adolescent-onset pathway (class 3). This is not in line with previously identified association between mother-level factors (e.g., maternal depression) and an increased risk of head injury by adolescence (McKinlay et al., Reference McKinlay, Kyonka, Grace, Horwood, Fergusson and MacFarlane2010). However, only early mother-level risk factors (by age 3) were taken into account in our study, and it is possible that mother-level risk later in development is more relevant to this adolescent-onset pathway that links head injury and conduct problem symptoms. The adolescent-onset pathway was instead most strongly associated with household risk factors, i.e., low household income, single parent household, household overcrowding, and low-quality home learning environment. This continues to support previous literature, which has shown this pathway of conduct problems to be most strongly associated with socioeconomic status (SES (Gutman et al., Reference Gutman, Joshi and Schoon2019)). This also provides further support for the hypothesis that there are potential latency effects from child and household accumulative risk to later emerging conduct problem symptoms (Gutman et al., Reference Gutman, Joshi and Schoon2019; Schoon et al., Reference Schoon, Sacker and Bartley2003) and its associated higher levels of late childhood head injuries. Thus, preventative measures might aim to primarily reduce household risk factors, or provide effective interventions that are appropriate for families from a low SES background (Leijten et al., Reference Leijten, Raaijmakers, Orobio de Castro, van den Ban and Matthys2017). It could further provide interventions to improve the early home learning environment, such as improving the interaction between preschool staff and parents particular those with a low SES (Kuger et al., Reference Kuger, Marcus and Spiess2019).
Our findings identify a further opportunity for preventions to reduce the likelihood of a child entering these developmental pathways of conduct problems and head injuries via provision of greater support to mothers to prevent the emergence of negative parenting styles with children through to age 5. Mother’s negative parenting styles were associated with all clinically relevant pathways. It must be noted that while the mother-level cumulative risk was not associated with the adolescent-onset pathway, mother’s negative parenting styles were. Though this effect was small for this pathway, adolescent head injuries have been previously associated with negative parenting styles (McKinlay et al., Reference McKinlay, Kyonka, Grace, Horwood, Fergusson and MacFarlane2010). Efforts to prevent the emergence of maternal withdrawal tactics and harsh parenting (Speyer et al., Reference Speyer, Hang, Hall and Murray2022) should therefore be addressed to reduce both conduct problem symptoms and head injuries in all clinically relevant pathways. Such interventions could include parent feedback and coaching (McConnell et al., Reference McConnell, Closson, Morse, Wurster, Flykt, Sarche and Biringen2020) and/or parental well-being courses (Tapp et al., Reference Tapp, Gandy, Fogliati, Karin, Fogliati, Newall, McLellan, Titov and Dear2018).
Strengths and limitations
A key strength of this study is that it is the first to reveal multiple distinct pathways linking conduct problems and head injuries from 3 to 17 years of age. This will have important implications for when interventions should be administered and to whom. This study benefits from its analysis of data belonging to a large population representative national cohort study, which aids statistical power and generalizability.
The study, however, also has limitations. Note that we refer to ‘clinically relevant’ levels of conduct problems symptoms. The SDQ is not a diagnostic measure of conduct problems. Therefore, the described developmental pathways can only infer clinically relevant symptoms. Such use of parent-report measures may also lead to social desirability bias in the reporting of both key variables (Bornstein et al., Reference Bornstein, Putnick, Lansford, Pastorelli, Skinner, Sorbring, Tapanya, Uribe Tirado, Zelli, Alampay, Al-Hassan, Bacchini, Bombi, Chang, Deater-Deckard, Di Giunta, Dodge, Malone and Oburu2015). Future research may use health and clinical records, for example, to remove such potential bias from the results. Further, the measure of harsh parenting used in the MCS omits the severe harsh parenting items included in the original scale. This may explain why only a small effect is evident. Further research may wish to investigate this association further outside of the MCS where the more severe harsh parenting items can be explored. Finally, we encourage follow-up of this epidemiological research with smaller-scale neurological investigation to uncover possible neurological mechanisms at play between the distinct developmental pathways found in this paper.
Conclusions
This study identifies four distinct developmental pathways that link conduct problems and head injuries between 3 and 17 years of age. Two of these pathways showed a tendency toward clinically relevant levels of conduct problem symptoms and increasing levels of head injuries at some point during this period. Children were more likely to exhibit one of these pathways in the presence of negative parenting styles through to age 5 years or alongside diagnosed ADHD. Cumulative risk at various ecological levels had unique associations with these pathways and should also be utilzed in early interventions to prevent membership to clinically relevant pathways of linked head injuries and conduct problems. Such interventions are necessary to prevent subsequent outcomes associated with these pathways including delinquency and criminality.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0954579423001062.
Acknowledgments
We are grateful to the Centre for Longitudinal Studies (CLS), UCL Social Research Institute, for the use of the MCS dataset and to the UK Data Service for making them available. Neither CLS nor the UK Data Service bear any responsibility for the analysis or interpretation of these data. We are also very grateful to the families who have taken part in the MCS study and to the MCS team.
HC had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
No funding was received toward this work, but HC has received PhD funding from the Economic and Social Research Council South Coast Doctoral Training Partnership (Grant Number ES/P000673/1) and would like to thank them for the research opportunity. The authors report no competing interests.
Funding statement
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Competing interests
None.







