Background
Alcohol and substance use disorders (AUD and SUD, respectively), as well as non-substance-related psychiatric disorders are known risk factors for early death.Reference Charlson, Baxter, Dua, Degenhardt, Whiteford, Vos, Patel, Chisholm, Dua, Laxminarayan and Medina-Mora1–Reference Chesney, Goodwin and Fazel3 AUD/SUD are among the disorders with the highest standardised mortality ratio (SMR) of all psychiatric disorders.Reference Chesney, Goodwin and Fazel3 Accidental drug overdose and suicide have been found to be leading causes of death among treatment-seeking individuals with illicit drug use in Finland.Reference Onyeka, Beynon, Vohlonen, Tiihonen, Fohr and Ronkainen4,Reference Onyeka, Beynon, Hannila, Tiihonen, Fohr and Tuomola5 Individuals who seek treatment for substance-related issues typically have a severe AUD/SUD and accumulated health-related challenges, as well as social problems.Reference Tuithof, Ten Have, van den Brink, Vollebergh and de Graaf6,7
Non-substance-related psychiatric disorders and AUD/SUD are well-known to be extremely common comorbidities in the general population.Reference Grant, Stinson, Dawson, Chou, Dufour and Compton8,Reference Hasin, Stinson, Ogburn and Grant9 Estimates of comorbidity vary somewhat according to study settings and comorbidity is most common among psychiatric in-patients.Reference Hunt, Malhi, Lai and Cleary10,Reference Hunt, Large, Cleary, Lai and Saunders11 In clinical populations of individuals with illicit drug use, roughly two-thirds have at least one comorbid non-substance-related psychiatric disorder, of which personality, anxiety and mood disorders are the most prevalent.2 Comorbid AUD/SUD is often associated with a more severe course and worse clinical outcomes of psychiatric disorders compared with individuals without AUD/SUD.
Some studies have found psychiatric comorbidities to be important risk factors for premature death among individuals with AUD/SUD.Reference Roerecke and Rehm12–Reference Fridell, Bäckström, Hesse, Krantz, Perrin and Nyhlén14 A recent large population-based study on psychiatric comorbidities and their impact on mortality comprised over 7.5 million people in Denmark. The study found that the largest excess mortality was observed for combinations of psychiatric disorders that included SUD.Reference Plana-Ripoll, Musliner, Dalsgaard, Momen, Weye and Christensen15 Of specific psychiatric disorders, schizophrenia spectrum disorders have been most studied and for example recent results in the Nordics have shown that SMRs are highest for individuals with comorbid schizophrenia spectrum disorders and AUD/SUD compared with either disorder alone.Reference Heiberg, Jacobsen, Nesvåg, Bramness, Reichborn-Kjennerud and Næss16 However, to date only a few studies have sought to understand how different comorbid psychiatric disorders among individuals with AUD/SUD can predict premature death. Further, the recruiting of patient cohorts to study this comorbidity and its sequalae has often been done within psychiatric treatment settings and from the perspective of a psychiatric illness, most often psychotic disorders, and not vice versa.
Aims
Among a Finnish cohort of over 10 000 individuals who had sought treatment for AUD/SUD between 1990 and 2009, we aimed to study the associations of different non-substance-related in-patient psychiatric diagnoses with subsequent all-cause mortality and suicide up to 28 years after entering substance use treatment.
Method
This study used data from a larger register-based follow-up study on criminality, health and taxation of in-patients and out-patients entered into treatment for substance use. The data included the treatment records of 10 901 individuals who had sought treatment for alcohol or substance use at one of the three studied treatment units of the A-Clinic Foundation between 1990 and 2009.
Data regarding education, psychiatric hospital admissions and mortality were retrieved from national registers and combined with this treatment data. Permission was obtained from each respective register as well as the National Institute for Health and Welfare to combine the data-sets. The ethics committee of the A-Clinic Foundation approved the study protocol. The data were anonymised.
Study sample
The study sample comprised individuals who had sought treatment for alcohol or substance use at one of the three studied treatment units of the A-Clinic Foundation between 1990 and 2009. Järvenpää Addiction Hospital (JAH) is a nationally operating hospital specialised in the treatment of AUD and SUD in Finland. It offers a variety of in-patient programmes, including detoxification from alcohol and other substances, and rehabilitation programmes for men and women also with dual diagnoses, a family treatment programme and an opioid substitution treatment (OST) programme. The data included the treatment records of a total of 5287 patients admitted to JAH between 1990 and 2009. All in-patients (n = 4558) and out-patients (n = 95) in the electronic treatment document system from March 1997 to the end of 2009 were included as well as a group of in-patients (n = 634) before the electronic documenting system was implemented.Reference Pitkänen, Kaskela and Levola17 The mean number of days in treatment was 24, ranging from 1 to 280 days.
Information regarding all out-patients (n = 6514) in two out-patient addiction units in Helsinki from May 1990 to September of 2009 were also included in the study. The first clinic was founded in 1990 and provided treatment services for a variety of addictions. The other clinic provided mainly OST from 1998 onwards. Out-patient treatment consists largely of therapy and counselling for individuals or groups with the overall aim to help patients stop or reduce their substance use, reduce the harm associated with substance use and improve their overall quality of life. The overall data included 900 individuals (8.3% of all 10 901 treatment seeking individuals) who were patients both at one of the two out-patient clinics and at JAH.
Final sample
This study focused on the working-age individuals in the study population in order to evaluate premature mortality related to AUD/SUD and psychiatric comorbidity. Thus, individuals aged <18 and >65 years were excluded from the analyses. Of the 10 901 treatment-seeking individuals, both substance-use treatment data and information regarding psychiatric hospital admissions were available for 10 888 individuals of whom 135 were excluded because of age (<18 or >65 years when first entering treatment). A further 148 were diagnosed with dementia (290, 294.1; F00-F09) during in-patient psychiatric care and thus excluded, leaving us with a final sample of 10 605.
Substance use
Substance use was categorised into three groups by combining treatment and hospital data. The first group (AUD group) included individuals with AUD only (n = 3220). The second group (SUD group) included individuals with one or more SUD or a combination of AUD and SUD (n = 4341). The third group (SU–NAS group) included individuals who had sought treatment from one of the out-patient clinics but did not have recorded diagnoses or any hospital admissions because of AUD/SUD between 1990 and 2009 (n = 3044). This group has been characterised in more detail previously.Reference Pitkänen, Kaskela and Levola17
Psychiatric in-patient care and diagnoses
The National Institute for Health and Welfare maintains a registry of all hospital admissions in Finland. The retrieved data included information on psychiatric hospital admissions and diagnoses of psychiatric disorders from those admissions between 1990 and 2009.
Psychiatric hospital admissions during the study period were extracted from the data. Psychiatric admissions included admissions to specialised psychiatric in-patient care as well as some admissions to JAH for comorbid psychiatric and AUD/SUD between 1998 and 2001. Before and after this period, entering treatment at JAH was not guided to be coded in the national registers as psychiatric hospital admission. Further, information on involuntary admission to psychiatric in-patient care was extracted and dichotomised as yes/no depending on whether the individual had undergone involuntary care for at least 1 day during the study period. Involuntary care is strictly regulated in Finland by legislature and criteria include (a) the presence of a severe mental disorder (mainly psychoses, psychotic mania or psychotic depression), (b) the person presents an imminent danger to themselves or other persons and (c) other, less severe forms of treatment are not suitable. Involuntary care is good as it is always carried out in a specialised psychiatric in-patient setting with extremely rare instances where a somatic emergency requires somatic hospital care. According to regulations governing AUD/SUD treatment, involuntary care is technically also possible for severe AUD/SUD, when an individual has either an imminent risk of death or acts violently, but involuntary care on this basis has been utilised only a handful of times during past decades in Finland.
The patients’ primary diagnosis, as well as two secondary diagnoses were recorded by using ICD-9 or ICD-10 codes. Psychiatric diagnoses were grouped according to their respective ICD-categories: schizophrenia or related psychoses (ICD-9- 295xx, 297xx, 298xx; ICD-10 F20-F29), bipolar disorder (ICD-9 296.xx excluding 296.2 and 296.3; ICD-10 F30-F31), unipolar depression including dysthymia (ICD-9 296.2, 296.3, 300.4, 311; ICD-10 F32-F33, F34.1), anxiety disorder including obsessive–compulsive disorder (ICD-9 300; ICD-10 F40-F42), personality disorder (ICD-9 301; ICD-10 F60-F61) and adjustment reaction including acute stress-related disorder and post-traumatic stress disorder (ICD-9 308, 309; ICD-10 F43).
Psychiatric disorders are highly comorbid. Further, conversion of psychiatric diagnoses, for example from unipolar depression to bipolar disorder over time is quite common. To investigate the role of different non-substance-related psychiatric disorders on mortality, six mutually exclusive hierarchical groups prioritising severity were formed. Individuals were categorised into one of the following groups according to whether they had undergone psychiatric in-patient care during the study period with the following priority order:
(a) schizophrenia or related psychoses;
(b) bipolar disorder;
(c) unipolar depression;
(d) anxiety disorder;
(e) personality disorder; and
(f) adjustment reaction.
Thus, individuals with schizophrenia or related psychoses could also have a diagnosis of bipolar disorder, unipolar depression, anxiety, personality and/or adjustment disorders, but these additional diagnoses are irrelevant to the categorisation as only the highest category was recorded. Participants with for example unipolar depression could also have an anxiety, personality or adjustment disorder (but no schizophrenia or related psychoses, or bipolar disorder) and participants with an adjustment disorder could not have any of the other diagnoses at any time during the study period. Individuals who had not been in psychiatric in-patient care were considered as the reference group.
Individuals who had been in psychiatric in-patient care but were not categorised into any of the above-mentioned diagnostic groups, had been admitted to psychiatric in-patient care for alcohol or substance-related diagnoses only. These individuals were not included in the analyses where diagnostic grouping was used because of the following reasons: (a) the aim was to study the association of non-substance-related psychiatric disorders on all-cause mortality and suicide among treatment-seeking individuals with AUD/SUD and (b) the study population was already known to have sought treatment for AUD/SUD.
Death
Data concerning date and causes of death in the study population were obtained from Statistics Finland up to 31 December 2018. Mortality data was collected up to this date or until the individual turned 65 years, after which they were considered alive. The classifications of causes of death are reported using the 54-group classification of underlying causes of death.18 This classification takes into account data on both underlying and additional causes of death in the risk analysis for alcohol- and other substance-related deaths, as well as suicide. An inquest into the cause of death including an autopsy is routinely carried out in all deaths in Finland where the cause is not evident. In the cases of death, for example, by poisonings, overdoses or falls where suicidal intent is unclear, the deaths are not included in the suicide category.
Background variables
Previous research conducted in this study population and others has found that gender, date of birth, education and urban versus rural living are associated with mortality.Reference Pitkänen, Kaskela and Levola17,Reference Herttua, Mäkelä and Martikainen19,Reference House, Lepkowski, Williams, Mero, Lantz and Robert20 The background variables derived from treatment data (n = 10 605) included gender, decade of birth and living in the urban capital area or in other, more rural, parts of Finland. Additionally, data from the national Register of Completed Education and Degrees were provided by Statistics Finland. Patients were categorised into two groups: no secondary education completed and secondary education (or more) completed corresponding respectively to <12 and ≥12 years of education.
Statistical analyses
Distributions are presented with frequencies and percentages using cross-tabulation. Significance for the differences in frequencies was tested with chi-squared and Fisher's tests. Ages at death are presented with means and standard deviations (s.d.). Mean ages at death were compared with Welch's t-test and one-way ANOVA. Cox regression was used to calculate hazard ratios (HRs) with 95% confidence intervals for all-cause mortality and suicide-specific mortality from the time of first treatment contact for alcohol and/or substance use. As a result of the differences in the baseline hazard for mortality in the AUD, SUD and SU–NAS groups, the proportional hazards assumptions of the Cox models were not satisfied, and they were stratified according to substance use. The HRs for psychiatric in-patient care and involuntary care, as well as the different diagnostic groups were calculated using no psychiatric in-patient care as the reference group. Decade of birth, gender, secondary education and living in the capital were included as covariates. The overall model fit was evaluated with likelihood ratio test. Results were considered statistically significant when P < 0.05. P-values presented are unadjusted for multiple comparisons.
The analyses were performed using SPSS v.26.0.0.0. Figures were drawn using ggadjustedcurves() from R (v.4.0.0) package survminer (v.0.4.8).
Results
Nearly one-third (31.4%; n = 3330) of the study population had died by the end of 2018 or by their 65th birthday (Table 1). More than one in ten (n = 385) of the deceased individuals had died by suicide. The mean age at death was 47.6 years (s.d. 10.7) with suicide occurring at a younger age (mean age at death 40.3 years, s.d. 10.5).
Table 1 Background information, psychiatric admissions and mortality of treatment-seeking individuals for alcohol and/or substance use between 1990–2009. Differences between groups (χ2-test) alive versus deceased and all-cause mortality versus suicide (decade of birth not included), differences between age at death (Welch's t-test, one-way ANOVA)
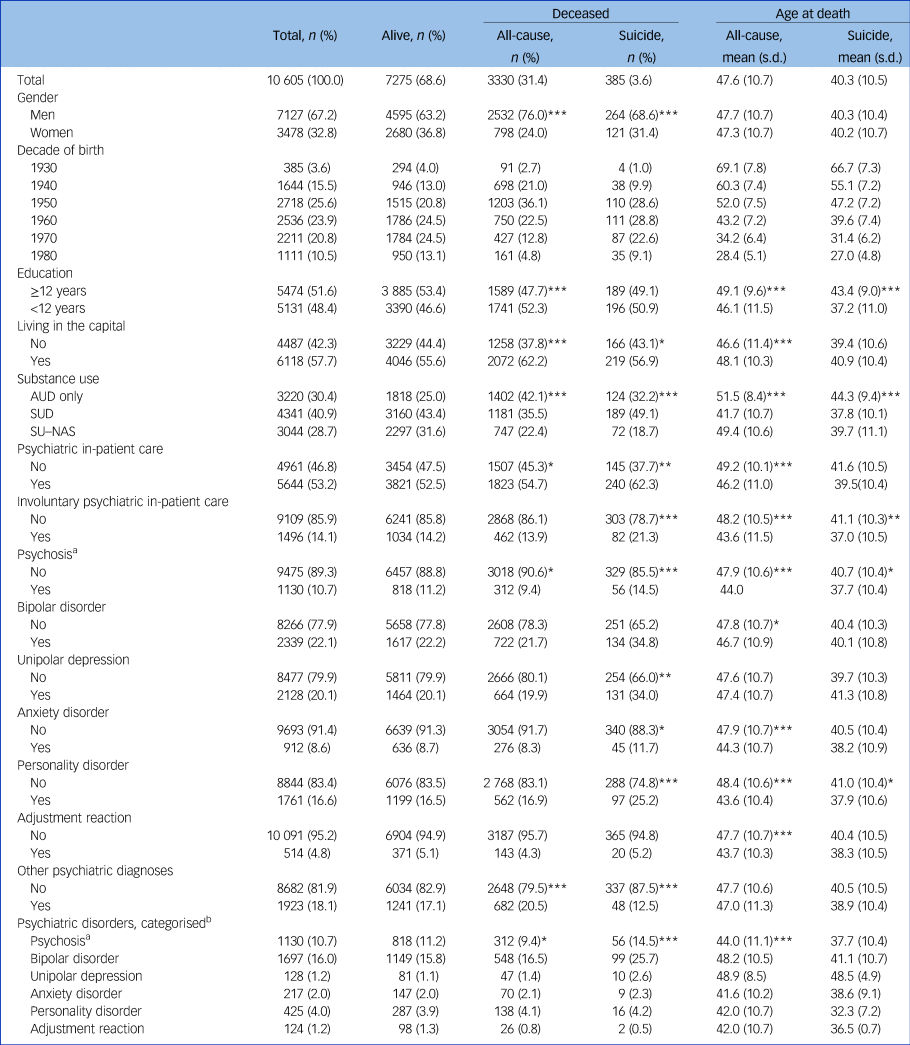
AUD, alcohol use disorder; SUD, substance-use disorder; SU–NAS, individuals who did not have recorded diagnoses or any hospital admissions because of AUD/SUD.
a. Schizophrenia or related psychoses; psychotic mania and psychotic depression included in the bipolar disorder and unipolar depression categories, respectively.
b. Six mutually exclusive hierarchical groups of non-substance-related psychiatric disorders prioritising severity; all differences between groups not analysed because of small cell size.
***P < 0.001, **P < 0.01, *P < 0.05.
Causes of death differed according to gender, age group and history of psychiatric in-patient care (Table 2). Alcohol-related diseases and poisonings were the more common among older men and women compared with younger adults. Suicides accounted for on average a little over a tenth of all deaths, however, there was much variation in suicide rates. Suicides comprised 7.6% of all deaths among older males without a history of psychiatric in-patient care but were the leading cause of death among younger women who had undergone psychiatric in-patient care (35.3%).
Table 2 Underlying causes of deatha of treatment-seeking individuals with alcohol and/or substance use according to gender and age group. Differences (Fisher's exact test) in distribution between causes of death by psychiatric in-patient status
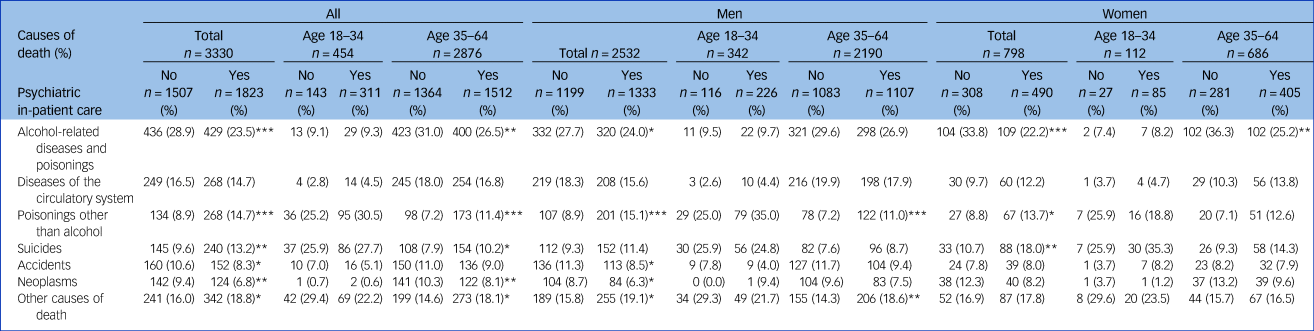
a. Official Statistics of Finland. Causes of death 2020; 2021.18
***P < 0.001, **P < 0.01, *P < 0.05.
Psychiatric in-patient care and diagnoses
Of the 10 605 individuals who had sought treatment for AUD/SUD, 53.2% (n = 5644) had been admitted to psychiatric in-patient care during the study period. Of these, 569 individuals had undergone psychiatric in-patient care in a dual diagnosis setting at JAH only. A total of 14.1% (n = 1496) individuals had undergone involuntary psychiatric in-patient treatment for at least 1 day. Bipolar disorder was the most common diagnosis category (16.0%; n = 1697/10 605) according to the hierarchical diagnostic grouping (Table 1).
All-cause mortality and death because of suicide overall according to psychiatric in-patient care status and psychiatric disorder grouping are presented in Fig. 1. The survival rates in Fig. 1 have been marginally adjusted for gender, decade of birth and the stratification of substance use grouping.
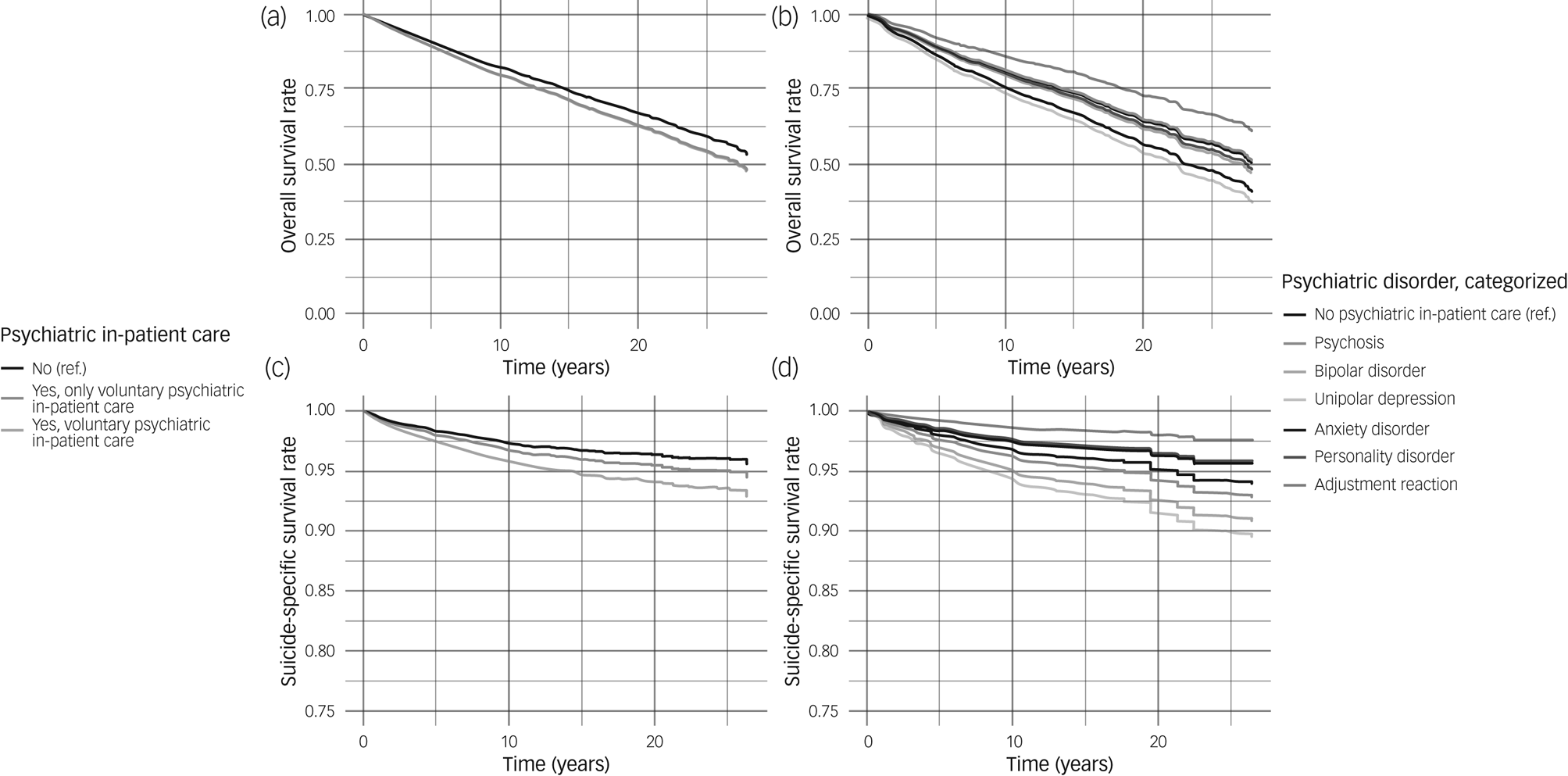
Fig. 1 Estimated overall and suicide-specific survival rates according to psychiatric in-patient care status and psychiatric disorder. Overall survival rate ((a) and (b)) for psychiatric in-patient care status and psychiatric disorder categorisation, respectively. Suicide-specific survival rate ((c) and (d)) for psychiatric in-patient care status and psychiatric disorder categorisation, respectively.
Estimates have been marginally adjusted for gender, decade of birth and the stratification of substance use grouping. Ref., reference.
In the fully adjusted models, involuntary psychiatric in-patient care was associated with a 40% increase in risk of suicide (HR 1.42, 95% CI 1.05–1.94), but no significant association was found for all-cause mortality (Table 3). Bipolar disorder and unipolar depression were associated with a 57% (HR 1.57, 95% CI 1.18–2.10) and 132% (HR 2.32, 95% CI 1.21–4.46) increase in risk of suicide, respectively. Of the different psychiatric diagnoses, schizophrenia and related psychoses were associated with a slight decrease in all-cause mortality (HR 0.87, 95% CI 0.76–0.99). After adjustment for confounding variables, the association between depression and all-cause mortality attenuated to statistically non-significant.
Table 3 Hazard ratios (HR) for all-cause and suicide-specific mortality separately according to psychiatric hospital admission (model 1) and psychiatric diagnostic groups (model 2), Cox proportional hazards model stratified by substance-use grouping (n = 10 605)
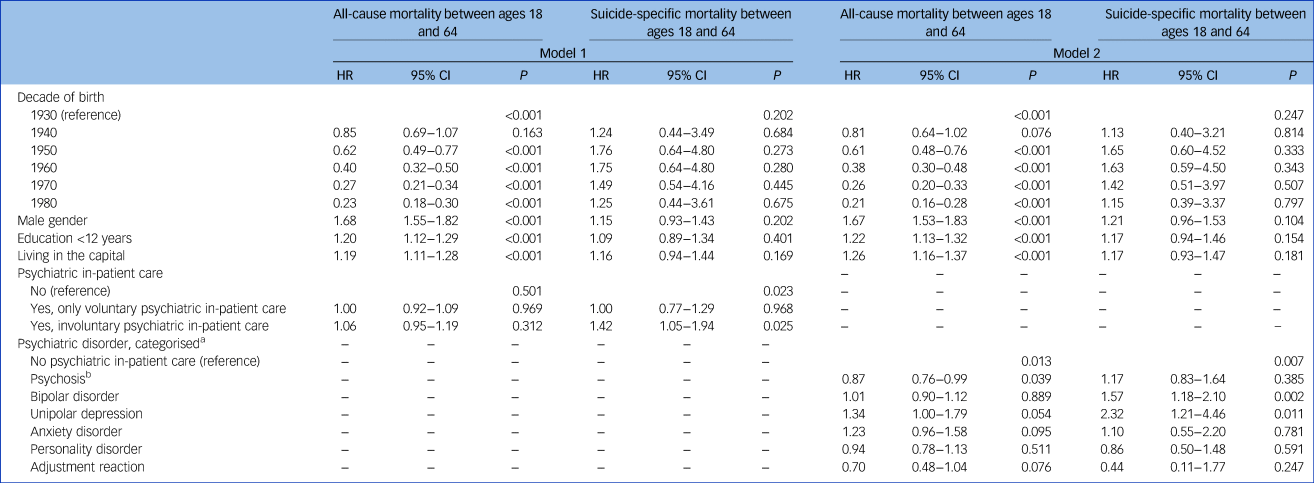
a. Six mutually exclusive hierarchal groups of non-substance-related psychiatric disorders prioritising severity, no psychiatric in-patient care during the study period used as reference.
b. Schizophrenia or related psychoses; psychotic mania and psychotic depression included in the bipolar disorder and unipolar depression categories, respectively.
Discussion
Main findings and interpretation of our findings
AUD/SUD are significant risk factors for premature death, including death by suicide and significant premature mortality among treatment-seeking individuals with AUD/SUD was also observed in this study. Despite the marked risk of death, specifically violent death, associated with AUD/SUD in previous literature, in this study, a history of involuntary psychiatric in-patient care and hospital admissions because of bipolar disorder or unipolar depression were associated with an even further elevated risk of suicide.
Suicides were, not perhaps surprisingly, more common among men than women in this population when addressing the number of deaths. However, it is to be noted, that the ratio of deaths because of suicide was disproportionately large among younger women who had undergone psychiatric in-patient care (35.3%) compared with other groups. Previous literature has demonstrated that the mortality hazard ratio due to alcohol and substance use is stronger for women compared with men.Reference Kendler, Ohlsson, Sundquist and Sundquist21,Reference Kendler, Ohlsson, Sundquist and Sundquist22 It is to be noted that AUD/SUD are more prevalent among men than women, whereas other psychiatric disorders are often more common among women. However, younger, poorly educated men with serious mental illness have been shown to be at risk to go untreated which may be reflected in a disproportionately small number of hospitalizations.Reference Bijl, de Graaf, Hiripi, Kessler, Kohn and Offord23 While this possible bias is to be taken into consideration in the interpretation of these results, a question about the interaction of age, gender and psychiatric morbidity on the risk of suicide among individuals with substance use can be raised.
Psychiatric hospital admissions were extremely common in this population, most of which were for non-substance-related issues, and a need for involuntary psychiatric care was also relatively frequent. Unipolar depression was quite common as one in five individuals had been admitted to hospital with a diagnosis of unipolar depression (20.1%). However, unipolar depression appeared to transition into or be accompanied by more severe mood disorders or psychotic disorders, as stratification of diagnoses according to severity showed, that only 1.2% had in fact been in psychiatric in-patient care for unipolar depression but never for bipolar disorder or schizophrenia or related psychoses. This is in keeping with the fact that bipolar disorder is often diagnosed with considerable delay and bipolar depression may have been mistakenly identified as unipolar. Personality disorders were relatively common diagnoses (16.6%), but when stratifying psychiatric disorders hierarchically, only 4.0% had hospital admissions with a diagnosis of personality disorder, but without a more severe diagnosis of schizophrenia or related psychoses or mood disorder.
A history of in-patient psychiatric care in not directly indicative of the prevalence of comorbid non-substance-use-related psychiatric disorders in this study population. Rather, a history of in-patient psychiatric care can be viewed as a proxy for the severity of the comorbid psychiatric disorder. Psychiatric hospital beds were cut rapidly in Finland in the 1990s because of a major recession and subsequent cuts to healthcare. Thus, the threshold for psychiatric hospital admissions has shifted, even within the study period, and more often out-patient care is used in situations where in-patient care would have been prioritised. Nowadays, the treatment of psychiatric disorders happens more predominately in out-patient settings.
Finland, like most other European countries and for example, Japan, India, Australia, Argentina and Brazil has a universal healthcare system, where healthcare is provided for all citizens. In Finland, substance-use-related issues have typically been treated separately from other mental health disorders. There have been times when individuals have been denied access to specialised psychiatric care for diagnostic evaluation or treatment of, for example, bipolar disorder or severe depression because of having a comorbid AUD/SUD. They have been treated in addiction settings often administratively under Social Services, where insufficient knowhow on diagnosing and treating mental disorders has resulted in these individuals receiving substandard or in some cases no care at all for their mental health disorders. Integrated care perspectives for comorbid psychiatric and substance-related issues have only recently begun to gain ground.
The finding that schizophrenia or related psychoses were associated with a slight decrease in mortality, may reflect the fact that individuals with the most severe psychiatric disorders are for the most part in specialised psychiatric care and should thus receive rigorous treatment for their non-substance-related psychiatric illness. However, unipolar depressive disorders are often treated in primary care or, in the case of our study population, most likely in the context of substance-use treatment settings. Only in the most severe cases will an individual with unipolar depression and a comorbid AUD/SUD be admitted to psychiatric in-patient care, which is reflected in the relatively low number of individuals who had undergone psychiatric in-patient care because of unipolar depression in this study (1.2%).
The individuals with AUD only were generally older and more educated than the other treatment-seeking individuals and had sought treatment from the studied units at an older age. A significant proportion of the treatment-seeking individuals included in this study did not have a diagnosis of AUD or SUD at any time during the study period. The individuals in the SU–NAS group had sought treatment at an out-patient clinic, where walk-in policies were applied, i.e. anyone could walk in or make an appointment without a referral. Especially in past decades, alcohol- and substance-use treatment services were carried out in the context of Social Services where systematic diagnostic evaluation was not implemented. The SU–NAS group in this study most resembled the AUD-only group in terms of year of birth and age at death, but their all-cause and specifically suicide rates were lower compared with the AUD-only group. None of the individuals in the SU–NAS group had any admissions to hospital with diagnoses of AUD/SUD. Previous research evidence suggests that disorder severity is strongly related to treatment seekingReference Bijl, de Graaf, Hiripi, Kessler, Kohn and Offord23 and it is plausible that the differences in mortality risk in this group is explained by a milder course of AUD/SUD.
Strengths and limitations
This research has several strengths. We were able to utilise large national treatment data on individuals seeking treatment for alcohol/substance-related issues. Further, Finnish registries are comprehensive and provide excellent opportunities to study, for example, mortality and hospital admissions with little missing information. An autopsy is carried out in Finland in all cases where there are individuals where the cause of death is unclear and the Finnish death register and the methods for determining the underlying cause of death are comprehensive. Combining treatment data and data from different registers is reliable using the personal social security number each Finnish individual is given. However, a limitation is that only hospital data were available, which precluded the use of data on out-patient psychiatric diagnoses. The use of a hierarchical psychiatric outcome variable may underestimate the latter outcomes such as personality disorder due to loss of cases.
Implications
This research underscores the fact that severe, non-substance-related psychiatric comorbidities requiring in-patient psychiatric care are extremely common among individuals seeking treatment for AUD/SUD. It is not acceptable that individuals do not receive adequate psychiatric treatment for their mental health disorders if they have a comorbid AUD/SUD, and this study shows that these individuals actually frequently require robust psychiatric care in the form of in-patient or even involuntary treatment, regardless. This calls into question the rationale for segregated treatment delivery of AUD/SUD and other psychiatric non-alcohol/substance-related disorders. Knowledge and knowhow on providing integrated care for comorbid disorders is acutely needed.
The already high suicide mortality associated with AUD/SUD is even higher among individuals who have undergone involuntary psychiatric in-patient treatment and among those with comorbid depression and bipolar disorder. The proportion of suicides was highest among young adult women who had undergone psychiatric in-patient treatment. Much more research on treatment strategies for co-occurring disorders is needed to diminish this risk.
Data availability
The data that support the findings of this study are available on request from the corresponding author, J.L. The data are not publicly available due to their containing information that could compromise the privacy of research participants.
Author contributions
J.L. formulated the research question, J.L., R.L. and T.P. designed the study and carried it out. T.P. was responsible for managing and R.L. for analysing the data. J.L. wrote the first draft of the article, to which R.L. and T.P. made a substantial contribution. All authors approved the final version of the article.
Funding
This work was supported by the Finnish Foundation for Alcohol Studies (personal grant J.L.).
Declaration of interest
None.








eLetters
No eLetters have been published for this article.