Introduction
While medical innovations and government policies have advanced neonatal health, there remains disproportionately high rates of adverse birth outcomes globally(World Health Organization, 2018). The greatest burden of preterm births (<37 weeks gestation) and low birth weight infants (<2,500 grams) occurs in low-and middle-income countries (LMICs) where more than 80% of preterm births and nearly 91% of low birth weight babies are born promoting a sense of urgency (Blencowe et al., Reference Blencowe, Krasevec, De Onis, Black, An, Stevens, Borghi, Hayashi, Estevez and Cegolon2019; Chawanpaiboon et al., Reference Chawanpaiboon, Vogel, Moller, Lumbiganon, Petzold, Hogan, Landoulsi, Jampathong, Kongwattanakul and Laopaiboon2019). Nearly ten million low birth weight babies (almost half of the global burden) and approximately 9 million preterm infants are born annually in Southern Asia (Blencowe et al., Reference Blencowe, Cousens, Oestergaard, Chou, Moller, Narwal, Adler, Garcia, Rohde and Say2012; Blencowe et al., Reference Blencowe, Krasevec, De Onis, Black, An, Stevens, Borghi, Hayashi, Estevez and Cegolon2019). More specifically, India has the highest number of preterm births worldwide with approximately 3.5 million preterm births and 8 million low birth weight infants born annually (Blencowe et al., Reference Blencowe, Cousens, Oestergaard, Chou, Moller, Narwal, Adler, Garcia, Rohde and Say2012; World Health Organization, 2004). Additionally, the proportions of all births that are preterm (13%) and low birth weight (40%) in India remain among the highest in the world (Chawanpaiboon et al., Reference Chawanpaiboon, Vogel, Moller, Lumbiganon, Petzold, Hogan, Landoulsi, Jampathong, Kongwattanakul and Laopaiboon2019; Lawn et al., Reference Lawn, Blencowe, Oza, You, Lee, Waiswa, Lalli, Bhutta, Barros and Christian2014; World Health Organization, 2004). Consequently, India currently accounts for the highest number of neonatal mortality worldwide, with 779,000 deaths annually (Lawn et al., Reference Lawn, Blencowe, Oza, You, Lee, Waiswa, Lalli, Bhutta, Barros and Christian2014). The neonatal mortality rates in India are even higher in rural areas with 31 neonatal deaths per 1000 live births compared to 15 per 1000 live births in urban areas (Sankar et al., Reference Sankar, Neogi, Sharma, Chauhan, Srivastava, Prabhakar, Khera, Kumar, Zodpey and Paul2016).
Infants born prematurely are vulnerable and are at an increased risk of infections including neonatal sepsis, unconjugated hyperbilirubinemia, respiratory distress syndrome, difficulty in feeding, and poor body temperature regulation (Blencowe et al., Reference Blencowe, Cousens, Chou, Oestergaard, Say, Moller, Kinney and Lawn2013; Moutquin, Reference Moutquin2003; World Health Organization, 2016; World Health Organization, 2018). Preterm birth complications are the leading cause for deaths among children under 5 years of age (Liu et al., Reference Liu, Oza, Hogan, Chu, Perin, Zhu, Lawn, Cousens, Mathers and Black2016). Low birth weight has been associated with acute and chronic health conditions including a lower intelligence quotient, neurological impairments, and stunted growth in childhood (World Health Organization, 2014). Additionally, they are at higher risk for developing hypertension and cardiovascular disease during adulthood (World Health Organization, 2014). Attempts to elucidate the etiology of preterm birth and low birth weight remain unclear but include clinical, biological, behavioral, and sociodemographic factors. Studies suggest that maternal anemia, diabetes, smoking and prior preterm birth are predictors of preterm birth and low birth weight (Andraweera et al., Reference Andraweera, Dekker, Leemaqz, Mccowan, Myers, Kenny, Walker, Poston, Roberts and Consortium2019; Grandi et al., Reference Grandi, Filion, Yoon, Ayele, Doyle, Hutcheon, Smith, Gore, Ray and Nerenberg2019; Liabsuetrakul, Reference Liabsuetrakul2011; Oaks et al., Reference Oaks, Jorgensen, Baldiviez, Adu-Afarwuah, Maleta, Okronipa, Sadalaki, Lartey, Ashorn and Ashorn2019; Parks et al., Reference Parks, Hoffman, Goudar, Patel, Saleem, Ali, Goldenberg, Hibberd, Moore and Wallace2018; Su et al., Reference Su, Samson, Garg, Hanson, Berry, Lin and Qu2018; Vahdaninia, Tavafian and Montazeri, Reference Vahdaninia, Tavafian and Montazeri2008).
The majority of studies that have identified risk factors for preterm birth and low birth weight have used multivariable analyses (Apte et al., Reference Apte, Patil, Lele, Choudhari, Bhattacharjee, Bavdekar and Juvekar2019; Hidalgo-Lopezosa et al., Reference Hidalgo-Lopezosa, Jiménez-Ruz, Carmona-Torres, Hidalgo-Maestre, Rodríguez-Borrego and López-Soto2019; Rai et al., Reference Rai, Sudfeld, Barik, Fawzi and Chowdhury2019). While these approaches can identify risk factors, they fail to examine the co-occurrence of risk factors that may further exacerbate adverse birth outcomes (Hendryx et al., Reference Hendryx, Luo, Knox, Zullig, Cottrell, Hamilton, John and Mullett2014; Jobe-Shields et al., Reference Jobe-Shields, Andrews Iii, Parra and Williams2015). Person-centered approaches such as latent class analysis (LCA) identify and classify homogeneous unobserved sub-groups characterized by individuals with similar co-occurring risks (Lanza et al., Reference Lanza, Dziak, Huang, Xu and Collins2018). The majority of the studies have employed LCA on either low birth weight or preterm birth distinctly and in high-income countries such as the US and Australia and have explored risk factors including behavioral risk factors, sociodemographic indicators and chronic diseases (Hendryx, Chojenta and Byles, Reference Hendryx, Chojenta and Byles2020; Hendryx et al., Reference Hendryx, Luo, Knox, Zullig, Cottrell, Hamilton, John and Mullett2014; Shaw, Herbers and Cutuli, Reference Shaw, Herbers and Cutuli2019; Tian et al., Reference Tian, Holzman, Slaughter-Acey, Margerison-Zilko, Luo and Todem2018). However, the complexity of sociodemographic factors and maternal obstetric outcomes has not been explored in LMICs using LCA, which remains critical since preterm and low birth weight births largely occur in these settings. Further, no studies have examined the impact of sociodemographic factors and clinical variables using LCA among rural and tribal populations in rural India. Therefore, the objective of this study was to utilize LCA to identify sociodemographic patterns and assess the association of these patterns on preterm delivery and/or low birth weight among pregnant women in rural Mysore District, India.
Methods
Study Setting
According to the 2011 census, Mysore District had a total population of 3,001,027 of which 1,489,527 were females (Census 2011). Majority of the residents (58.5%) lived in rural villages. The male literacy rate (78.5%) was higher than the female literacy rate (67.1%) (Census 2011). Nearly 87.7% of the population self-identified as Hindu, 9.7% as Muslim, and 1.3% as others (Census 2011). The scheduled caste population comprised 17.9% of the population, while the scheduled tribes were 11% of the total population. The languages commonly spoken in Mysore are Kannada (81.2%), Urdu (8.6%), and Telugu (3.3%) (Census 2011). In 2016, Mysore, the third largest district in the South Indian state of Karnataka, had an infant mortality rate of 33 per 1,000 live births in rural regions of the state, while the state of Karnataka had an infant mortality rate of 28 per 1,000 live births (International Institute of Population Health Sciences, 2016).
Study Population and Design
The original study was a prospective cohort study conducted among 1820 women between 2011 and 2014 to examine the feasibility of integrated antenatal care and HIV testing using mobile clinics in rural Mysore District. The project was called the Saving Children Improving Lives (SCIL) project and is described in the protocol by Kojima et al (Kojima et al., Reference Kojima, Krupp, Ravi, Gowda, Jaykrishna, Leonardson-Placek, Siddhaiah, Bristow, Arun and Klausner2017). The protocol for the study was reviewed and approved by the Institutional Review Boards of Florida International University and Public Health Research Institute of India (PHRII).
Utilizing mobile medical clinics, the women were provided with integrated antenatal care and HIV testing. During the visit, the women were offered educational and awareness information on antenatal care, institutional deliveries and importance of birth preparedness. After the visit, the women were informed of the study and were screened for eligibility. The eligibility criteria included pregnant women living in the Mysore sub-district for more than six months. If the women met the eligibility criteria and elected to participate in the study, the women underwent an informed consent in the local language of Kannada. Trained research staff of PHRII completed an interviewer-administered questionnaire comprised of sociodemographic, medical, and obstetric history. The staff also conducted a detailed physical exam with routine antenatal laboratory examinations of urine and blood. The lab evaluations were performed by trained laboratory technicians from PHRII.
This study was a cross-sectional analysis nested within the parent study, the SCIL project. The predictor measures were collected at baseline (at enrollment into the study), and the study outcomes were collected during the first follow-up (within 15 days after delivery). Women aged 18 years and older, and those who had a singleton live birth were included in the analysis. In the study, 40 individuals were excluded due to missing date of last menstrual period or missing dates on deliveries and 98 individuals who had a fetal death. The total number of participants included in the study were 1,540.
Outcome and Predictor Variables
Outcomes
The outcomes in the study were preterm birth and low birth weight. Low birth weight was defined as an infant born weighing less than 2500 grams(World Health Organization, 2004). Preterm births were defined as live births before 37 weeks of gestation based on the last menstrual period (World Health Organization, 2018).
Predictor Variables
The variables included pregnant woman’s education, partner’s education, household income, age at marriage, primigravida, and living children in the household. Education was categorized as primary education or less (≤ 8 years), secondary education (9-10 years) and upper secondary education (>10 years). Household income was categorized as low income ≤ 4,000 Indian Rupees (INR) (approximately USD 54.7 with 1 USD = 58.9 INR during the data collection period), middle income as 4001-10,000 INR, and high income as ≥ 10,000 INR. Age at marriage was categorized into <18 years old, or ≥ 18 years old. Living children in the household was dichotomized as yes or no. Covariates included age, delivery location categorized as home, public health institution (sub-center/primary health center/district health) and private institution (maternity hospital/private nursing home). These measures were selected based on prior literature on maternal obstetric factors. (Blencowe et al., Reference Blencowe, Cousens, Chou, Oestergaard, Say, Moller, Kinney and Lawn2013) Age was categorized as <20 years, 20-24 years and ≥ 25 years. Maternal obstetric factors included baseline sexually transmitted infections (STIs) (binary variable with “yes” or “no”), previous stillbirth or neonatal losses (binary variable with “yes” or “no”), history of spontaneous abortion (binary variable with “yes” or “no”), history of induced abortion (binary variable with “yes” or “no”), exposure to passive smoking indoors (binary variable with “yes” or “no”), and history of hypertension (binary variable with “yes” or “no”). Anemia status levels were labeled as normal, mild, and moderate/severe based on the hemoglobin levels of 11.0g/dl or higher, 10-10.9 g/dl, and ≤ 10.0 g/dl respectively. Hypertension categories were based on blood pressure levels as follows: normal (<120/80 mm Hg), pre-hypertension (120-139 mm Hg systolic or 80-89 mm Hg diastolic) and hypertensive categories (≥140 mm Hg systolic or ≥90 mm Hg diastolic).
Statistical Analysis
Latent Class Analysis (LCA) was conducted using the SAS/STATv14.2 software, PROC LCA to identify and classify homogeneous unobserved sub-groups of pregnant women based on a chosen set of sociodemographic indicators including pregnant woman’s education, partner’s education, age at marriage, primigravida status, living children in the household, and total monthly household income (Fig 1) (Lanza et al., Reference Lanza, Dziak, Huang, Xu and Collins2018; Nylund-Gibson and Choi, Reference Nylund-Gibson and Choi2018). Given the unique set of sociodemographic factors identified from the literature review, these variables were selected for the latent classes (Blencowe et al., Reference Blencowe, Cousens, Chou, Oestergaard, Say, Moller, Kinney and Lawn2013). LCA was advantageous compared to multinomial regression as this analytical approach examines and identifies distinct high-risk groups of women for preterm birth and low birth weight based on latent patterns of sociodemographic factors. This approach can simultaneously assess combinations of individuals with similar attributes and identify distinct latent patterns that would not be identified through the use of multinomial regression. On the other hand, multinomial regression focuses on individual variables while adjusting of other variables.

Figure 1. Latent Class Schematic Model.
First, employing a model comparison approach to test unconditional models without covariates in the LCA. The model fit was assessed using a series of 2 through 6 latent classes. Second, the appropriate number of latent classes were selected based on the Bayesian Information Criterion (BIC), Adjusted Bayesian Information Criterion (aBIC), Adjusted Information Criterion (AIC), entropy values and the interpretability of latent classes. Lower BIC, aBIC, and AIC indicated a better model fit (Nylund, Asparouhov and Muthén, Reference Nylund, Asparouhov and Muthén2007). An entropy value closer to 1.0 represented a better distinction of the latent classes (Lanza et al., Reference Lanza, Dziak, Huang, Xu and Collins2018).
After, the final class was chosen based on BIC, aBIC, AIC, every individual was assigned to the latent class based on the highest posterior probability of membership. Subsequently, descriptive statistics were generated for the explanatory variables used in the LCA and the latent classes. Univariate analyses were conducted using chi-square tests to examine the associations between latent classes and the covariates. Finally, binary logistic regression was applied to estimate the association between latent classes and the outcome measures (i.e. preterm birth and low birth weight) while controlling for maternal obstetric covariates. The results were presented as odds ratios and associated 95% confidence intervals.
Results
Sample Characteristics
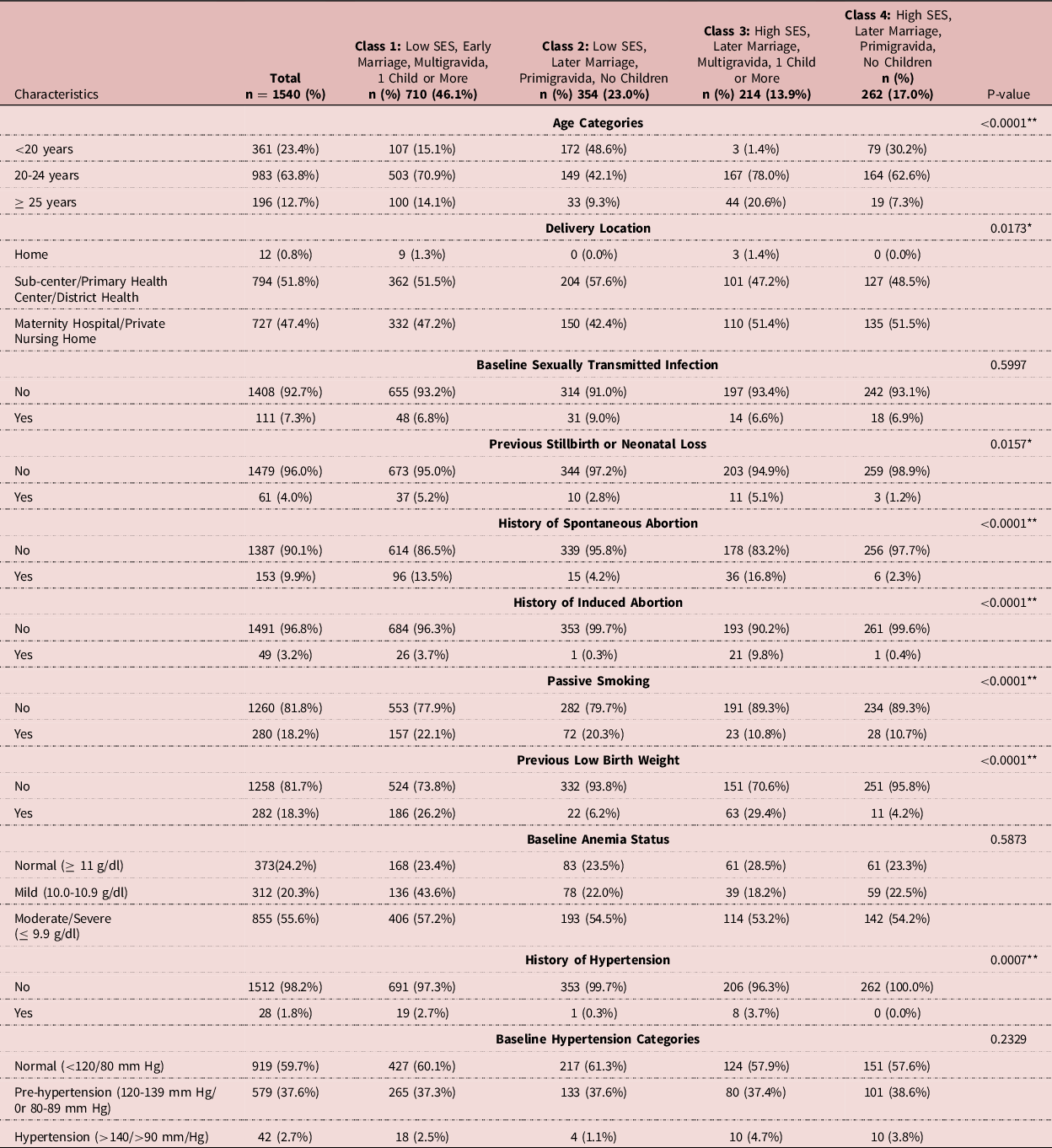
Table 1 displays the characteristics of the participants. Approximately 23.4% of the pregnant women were aged <20 years, 63.8% were aged 20-24 years, and 12.7% were aged 25 years and older. Nearly 40% of the pregnant women had received a primary education or less, while more than half (53.1%) of their partners had primary education or less. Nearly 37% of the women were primigravida, and more than half of the participants had living children in the household. Approximately a third of the women reported that the total household income was less than 4000 Indian Rupees (INR). The majority of the births were institutional deliveries with 51.8% of the women giving birth at a sub-center/primary health center/district health and 47.2% giving birth at a maternity hospital/private nursing home; only 0.8% of births were at the women’s home. Nearly 7.3% (95% confidence intervals (CI): 6.0%-8.2%) of the women were diagnosed as having a baseline STI. Approximately 10% of the participants reported a history of spontaneous abortion, and 3.2% reported a history of induced abortion. Almost 20% were exposed to passive smoking in the house, and 18.3% reported having delivered a previous low birth weight infant. More than 75% of the women were diagnosed with anemia (20.3% mild and 55.6% moderate/severe). Nearly 2% of the women reported a history of hypertension during their last pregnancy. In addition, 37.6% of the women were diagnosed with blood pressure considered pre-hypertensive, and 2.7% had hypertensive levels at baseline. Low birthweight occurred in nearly 13.8% (95% CI: 12.1%-15.7%) of deliveries, while preterm birth occurred in 12.1% (95% CI: 10.6%-13.9%) deliveries. Approximately 26.3% of low birth weight babies comprised of preterm births.
Table 1. Description of sociodemographic characteristics of rural pregnant women in Mysore District that were used to determine class membership overall and by class (n = 1540)

**-<0.0001 **-<0.05.
Latent Class Analysis
Based on the model fit parameters, the model with four latent classes was selected as the best fitting and most parsimonious model with lowest BIC (445.41), adjusted BIC (321.52), and AIC (237.17) and distinct class separation based on entropy value of 0.75. While the 3-class model offered greater entropy, no major differences were observed between the 3-class and 4-class entropy values at 0.80 and 0.75, respectively. Sensitivity analysis was also performed comparing the 3-class and 4-class models, and similar findings were observed. Moreover, adding classes beyond the 4-class model conferred minor improvements in accuracy and model fit. Hence, a 4-class model was chosen based on its model fit statistics and the interpretability of classes.
Class 1 (46.0%), the largest class in the study, was labeled as “low socioeconomic (SES)/early Marriage/Multigravida/1 Child or More”. Class 1 was characterized by the majority of pregnant women and their respective partners having primary education or less, more likely to have a monthly household income <4000 INR, marriage <18 years of age, multigravida, and more likely to have children (Table 1). Class 2 (23.0%) was labeled as “low SES/later marriage/primigravida/no children.” This class was characterized by the majority of pregnant women and their respective partners having primary education or less, more likely to have a monthly household income of < 4000 INR, more likely to be married after 18 years of age, primigravida and no children. Class 3 (13.9%) was labeled as “high SES/later marriage/multigravida/1 child or more.” Class 3 was characterized by the majority of pregnant women and their respective partners having at least an “upper secondary education”, more likely to have a monthly household income of ≥ 4000 INR, more likely to be married after 18 years of age, multigravida and living children in the household. Class 4 (17.0%) was labeled as “high SES/later marriage/primigravida/no children”. Class 4 was characterized by the majority of pregnant women and their respective partners having upper secondary education, more likely to have a monthly household income of ≥ 4000 INR, more likely to be married after 18 years of age, primigravida and no children. Class 4 was used as the referent group.
Table 2 displays the results of univariate analyses and comparisons between the maternal obstetric covariates and the latent classes. Maternal obstetric covariates were significantly associated with the latent classes except for anemia status and hypertension. The proportion of women reporting prior adverse maternal obstetric outcomes i.e. previous still birth or neonatal loss, prior history of spontaneous abortion, prior history of induced abortion, anemia, exposure to passive smoking indoors, prior low birth weight was highest among women in Class 1. Women in class 1 were also characterized with the highest proportion among women aged 20-24 years old. The proportion of women reporting baseline STI levels was highest in Class 2. In addition, the majority of these women was younger than 20 years old. The proportion of women reporting both prior adverse maternal obstetric outcomes and chronic diseases including moderate or severe levels of anemia and history of hypertension was highest in Class 3. Moreover, these women were likely to be 25 years and older. The proportion of women with prior and current adverse maternal obstetric outcomes and chronic diseases was lowest in Class 4.
Table 2. Description of maternal obstetric covariates among rural pregnant women in Mysore District overall and by class membership (n=1540)

**-<0.0001 **-<0.05.
Table 3 displays the crude and adjusted odds ratio (OR) and 95% CI for the relationship between latent classes and preterm birth and low birth weight. When compared with women in Class 4, women in Class 1 had higher crude odds for preterm birth (OR: 1.79, 95% CI: 1.10-2.91). After adjusting for the covariates, women in Class 1 had higher odds for preterm birth (adjusted OR [aOR]: 1.77, 95% CI: 1.05-2.97) compared with women in Class 4. In addition, women less than 20 years old were twice as likely to have a preterm birth (aOR: 2.00, 95% CI: 1.08-3.71). Moreover, hypertension (>140/>90 mm/Hg) was also a significant determinant of preterm birth (aOR: 2.28, 95% CI: 1.02-5.07). Women with mild anemia at baseline also had significantly lower odds of preterm birth compared to those with normal hemoglobin levels (aOR: 0.58, 95% CI: 0.33-0.98).
Table 3. Crude Odds Ratio and Adjusted Odds Ratio of Preterm Birth and Low Birth Weight by characteristics of rural pregnant women in Mysore District obtained from binary logistic regression

CI, confidence intervals; OR, odds ratio.
* Significance.
The final model for preterm birth and low birth weight was adjusted for the latent classes, age, delivery location, baseline STI, history of neonatal loss or still birth, history of spontaneous abortion, history of induced abortion, passive smoking, previous low birth weight, anemia, history of hypertension and hypertension
When compared with women in Class 4, women in Class 1 (OR:1.75, 95% CI: 1.08-2.84) and Class 2 (OR: 2.83 95% CI: 1.71-4.71) had higher crude odds for low birth weight. Moreover, pregnant women with history of neonatal loss or still birth (OR: 1.92, 95% CI: 1.04-3.54) and passive smoking exposure had higher crude odds for low birth weight (OR: 1.40, 95% CI: 1.03-2.07). The multivariable model showed that women in Class 2 had higher odds of low birth weight (aOR: 2.50, 95% CI: 1.49-4.21) compared to women in Class 4 (Table 3). Moreover, pregnant women with a previous low birth weight had higher odds of low birth weight (aOR: 2.15, 95% CI: 1.40-3.29) compared to women without any previous low birth weight. There was no significant association with baseline anemia.
Discussion
This study employed LCA to identify sociodemographic patterns and assessed the role of these patterns in determining preterm delivery and/or low birth weight among pregnant women in South India. The LCA identified four subgroups of women characterized by distinct sociodemographic profiles, with approximately 46% representing “low SES/early marriage/multigravida/1 child or more”. Women belonging to Class 1 “low SES/early marriage/multigravida/1 child or more” had higher odds of a preterm delivery compared to the referent class 4 “high SES/later marriage/primigravida/no children”. In addition, women belonging to Class 2 “low SES/later marriage/primigravida/no children” had higher odds of delivering a low birth weight baby compared to Class 4. Women with a history of having delivered a previous infant with low birth weight also had greater odds of delivering a subsequent infant with low birth weight.
The study findings indicate that low SES conveyed significant risk to preterm birth and low birth weight among rural pregnant women. The most notable differences observed among Class 1, Class 2 and Class 4 are low SES compared to high SES. Several studies have corroborated that sociodemographic factors stemming from low maternal education, and low household wealth are determinants of adverse birth outcomes (Apte et al., Reference Apte, Patil, Lele, Choudhari, Bhattacharjee, Bavdekar and Juvekar2019; Blumenshine et al., Reference Blumenshine, Egerter, Barclay, Cubbin and Braveman2010; Hidalgo-Lopezosa et al., Reference Hidalgo-Lopezosa, Jiménez-Ruz, Carmona-Torres, Hidalgo-Maestre, Rodríguez-Borrego and López-Soto2019; Kader and Perera, Reference Kader and Perera2014; Rai et al., Reference Rai, Sudfeld, Barik, Fawzi and Chowdhury2019; Tian et al., Reference Tian, Holzman, Slaughter-Acey, Margerison-Zilko, Luo and Todem2018). Overall findings highlight that all the classes that comprised primarily of women with low SES had higher crude odds of preterm birth and low birth weight. After controlling for maternal obstetric characteristics, Class 1 and Class 2 remained statistically significant for preterm birth and low birth weight respectively. Previous LCA studies have established socioeconomic characteristics as determinants of either low birth weight or preterm birth in high-income settings (Hendryx, Chojenta and Byles, Reference Hendryx, Chojenta and Byles2020; Hendryx et al., Reference Hendryx, Luo, Knox, Zullig, Cottrell, Hamilton, John and Mullett2014; Shaw, Herbers and Cutuli, Reference Shaw, Herbers and Cutuli2019; Tian et al., Reference Tian, Holzman, Slaughter-Acey, Margerison-Zilko, Luo and Todem2018). A systematic review conducted by Blumenshine and colleagues noted that socioeconomic disparities remained the most significant predictor of adverse perinatal outcomes including preterm birth, low birth weight and small for gestational age (Blumenshine et al., Reference Blumenshine, Egerter, Barclay, Cubbin and Braveman2010). It is speculated that pregnant women with high SES have reduced odds of delivering babies born with adverse birth outcomes due to increased access to antenatal care, improved health literacy, and nutritional behavior (Blumenshine et al., Reference Blumenshine, Egerter, Barclay, Cubbin and Braveman2010).
In addition, the women characterized in Class 2, married over the age of 18 years old and were primigravida. It is possible that these women who are pregnant for the first time have unknown underlying factors. Additionally, these women may not be connected with antenatal care services and may lack prior pregnancy experience compared to multigravida women. Earlier studies have supported the finding that primigravida is associated with low birth weight (Ahankari et al., Reference Ahankari, Bapat, Myles, Fogarty and Tata2017; Kamala et al., Reference Kamala, Mgaya, Ngarina and Kidanto2018). A case-control study in Southern India indicated that primigravida was associated with increased odds of low birth weight (Johnson et al., Reference Johnson, Abraham, Stephenson and Jehangir2016). More importantly, the compounding of risks in Class 2 of low SES, primigravida and later marriage has been shown to further exacerbate low birth weight. Notably, Class 1 was significant in the adjusted models for preterm birth among women belonging to low SES and marrying early. A distinct characteristic is that the women in Class 1 were multigravida, and not pregnant for the first time. While these women may have been connected to antenatal services during previous pregnancies, women in Class 1 reported the highest prior adverse maternal obstetric outcomes among the classes. These study findings have confirmed that multigravida, specifically multigravida with previous adverse birth outcomes, may be a risk factor to preterm birth (Blencowe et al., Reference Blencowe, Cousens, Chou, Oestergaard, Say, Moller, Kinney and Lawn2013; Heaman et al., Reference Heaman, Kingston, Chalmers, Sauve, Lee and Young2013).
Having a previous low birth weight infant conferred a greater than two-fold risk to have a recurrent low birth weight infant. Recent studies have supported that previous low birth weight is the strongest indicator for subsequent delivery of low birth weight infant (Shaw, Herbers and Cutuli, Reference Shaw, Herbers and Cutuli2019; Smid et al., Reference Smid, Ahmed, Stoner, Vwalika, Stringer and Stringer2017). Additionally, previous low birth weight may further exacerbate the risk of other adverse perinatal outcomes including small-for-gestational age (Smid et al., Reference Smid, Ahmed, Stoner, Vwalika, Stringer and Stringer2017). In a previous study in Karnataka State, India, prior low birthweight was a predictor for preterm birth and low birth weight (Basha, Shivalinga Swamy and Noor Mohamed, Reference Basha, Shivalinga Swamy and Noor Mohamed2015). Moreover, poor maternal obstetric characteristics can increase the likelihood of having a low birth weight or preterm birth. In the study, a history of neonatal loss or still birth was also found to be a significant predictor in the unadjusted analysis. Similarly, previous studies have supported that prior maternal obstetric outcomes can influence subsequent birth outcomes (Basha, Shivalinga Swamy and Noor Mohamed, Reference Basha, Shivalinga Swamy and Noor Mohamed2015; Shaw, Herbers and Cutuli, Reference Shaw, Herbers and Cutuli2019). In addition, passive smoking exposure was also determined to be a predictor of low birth weight in the unadjusted analysis. However, these findings were not observed in the multivariate analysis. Prior studies have corroborated that exposure to passive smoking may substantially increase adverse birth outcomes (Hendryx, Chojenta and Byles, Reference Hendryx, Chojenta and Byles2020; Xi et al., Reference Xi, Luo, Wang, Wang, Wang, Guo and Lu2020). Moreover, current maternal obstetric characteristics including hypertension (>140/>90 mm Hg) was a significant predictor in preterm birth. Previous studies have confirmed the relationship between hypertension and preterm birth (Mulualem, Wondim and Woretaw, Reference Mulualem, Wondim and Woretaw2019; Wagura et al., Reference Wagura, Wasunna, Laving and Wamalwa2018). Surprisingly, mild anemia (assessed at the baseline visit) was associated with lower risk of preterm birth. It could be explained that all women received iron supplements after the baseline visit that could explain the unexpected relationship. Therefore, prior and current maternal obstetric history are significant determining factors in predicting adverse birth outcomes.
This study has several limitations worth noting. Given the cross-sectional study design, no causal relationship can be established between the latent classes and the outcomes. The data are derived from rural Mysore; therefore, it is difficult to extrapolate the findings to other regions in India since the study results may have limited generalizability. Gestational age was based on last menstrual period, and this may result in some degree of inaccuracy because there were no clinical records to ascertain as the study was done in a rural region. Previous low-birth weight was self-reported and this may result in inaccurate estimates. Measures such as short interpregnancy intervals were not included in the survey and may be a potential confounder in the analysis. In addition, blood pressure was only assessed once during the baseline visit only so hypertension during pregnancy may not be well-documented. Self-reported variables including exposure to passive smoking indoors may be subject to social desirability bias due to the nature of the interviewer-administered survey. Lastly, utilizing LCA assigns individuals based on their probability however, the exact percentage cannot be classified. Nevertheless, this study has some strengths. This is the first study that utilizes LCA to examine both preterm birth and low birth weight among pregnant women in rural India. Previous LCA studies have been documented in high resource settings hence it is valid and reliable approach. Further, this study utilized a large sample size from a rural region within India and data was collected prospectively, allowing us to establish the exposure prior to the outcome of interest.
Conclusion
The identification of at-risk women based on multiple characteristics is critical for healthcare providers to tailor interventions for pregnant women to prevent future adverse birth outcomes. The study findings highlighted the importance of utilizing multiple co-occurring risk factors and the impact of compounding risks in determining preterm birth and low birth weight. Women belonging to low socioeconomic status latent classes, despite obstetric measures, were more likely to have preterm birth and low birth weight. While these birth outcomes are often intertwined, our study revealed two high-risk classes. Women characterized by co-occurring risks of low SES, early marriage, multigravida, and having more than one child were at an increased risk of preterm delivery whereas women characterized by low SES, later marriage, primigravida, and no children were at an increased risk of delivering a low birth weight infant. Thus, the combination of prior maternal obstetric measures and lower SES may need to be identified before pregnancy or early during pregnancy, monitored and treated for pregnancy complications and infections to prevent subsequent adverse birth outcomes. Targeted policies in addressing socioeconomic status need to be implemented to reduce the disproportionate differences between individuals of high and low SES. Therefore, government policies and programs are crucial in reducing inequalities in addressing preterm birth and low birth weight in rural Mysore, India.
Ethical Approval
The protocol for the study was reviewed and approved by the Institutional Review Boards of Florida International University and Public Health Research Institute of India. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Conflicts of Interest
The authors have no conflicts of interest to declare.
Source of Funding
This study was supported by the Positive Action for Children Fund [to PM]; National Institutes of Health (NIAID grant R15AI28714-01; FIC/NHLBI/NINDS Award Number D43 TW010540 [to PM]); National Institute on Minority Health and Health Disparities of the National Institutes of Health Under Award Number NIMHD (U54MD012393 [to ZBT and MJT]); the Global Health Equity Scholars Fellowship (NIH FIC/NHLBI/NINDS Award Number D43 TW010540 to [to KK]).