Introduction
The gold standard insect repellent to keep away biting pests like mosquitoes has for decades been N,N-Diethyl-meta-toluamide (DEET), which remains the safest and most effective repellent among all synthetic or natural repellents (Holzer, Reference Holzer2001; Fradin and Day, Reference Fradin and Day2002; Kongkaew et al., Reference Kongkaew, Sakunrag, Chaiyakunapruk and Tawatsin2011; Rodriguez et al., Reference Rodriguez, Drake, Price, Hammond and Hansen2015). Hundreds of studies on its safety and efficacy (Fradin and Day, Reference Fradin and Day2002; Canadian Paediatric Society, 2003; Frances, Reference Frances, Debboun, Frances and Strickman2007; Chen-Hussey et al., Reference Chen-Hussey, Behrens and Logan2014) and decades of reports covering tens of thousands of exposures confirm that DEET is of low risk and safe to use in any individual over 2 months of age, including pregnant and breastfeeding women (Veltri et al., Reference Veltri, Osimitz, Bradford and Page1994; Bell et al., Reference Bell, Veltri and Page2002; Koren et al., Reference Koren, Matsui and Bailey2003; Fradin, Reference Fradin, Keystone, Kozarsky, Connor, Nothdurft, Mendelson and Leder2019; Mutebi and Gimnig, Reference Mutebi, Gimnig, Brunette and Nemhauser2019). DEET is better tolerated than most plant-based topical repellents such as oil of lemon eucalyptus or citronella, some of which have higher risks of side effects and/or are not recommended for children younger than three years (Temple et al., Reference Temple, Smith and Beasley1991; Goodyer and Behrens, Reference Goodyer and Behrens1998; Woolf, Reference Woolf1999; Pollack et al., Reference Pollack, Kiszewski and Spielman2002; de Groot and Schmidt, Reference de Groot and Schmidt2016; Mutebi and Gimnig, Reference Mutebi, Gimnig, Brunette and Nemhauser2019). Regardless of ingredients, all topical repellents still require transporting containers of liquids or creams, are only effective for a certain amount of time, may leave an undesirable odor or greasy sensation, and may require total coverage of all exposed skin to prevent all bites.
Proposed alternatives vary in their efficacy: insecticide-treated bed nets work, while sonic repellent devices or phone apps do not (Rasnitsyn et al., Reference Rasnitsyn, Alekseev, Gornostaeva, Kupriyanova, Potapov and Razumova1974; Enayati et al., Reference Enayati, Hemingway and Garner2007). Long sought after are systemic repellents: substances that, when consumed or injected, render the entire body unattractive to biting insects (Sherman, Reference Sherman1966). One widely promoted systemic repellent, especially online (Ives and Paskewitz, Reference Ives and Paskewitz2005), is vitamin B1, or thiamine (C12H17N4OS), also spelled ‘thiamin’ and typically sold in its salt form as thiamin[e] [hydro]chloride. [Note that some sources state other vitamins such as B12 are repellent, but this is typically an error (Roessler, Reference Roessler1961).] Discovered in 1897 (Wuest, Reference Wuest1962), thiamine is an essential nutrient found in whole grains, legumes, fish, pork, and yeast. Following its synthesis in 1936, it was enthusiastically adopted as a medicine and food additive to prevent beriberi, at the time a widespread and debilitating disease (Sriram et al., Reference Sriram, Manzanares and Joseph2012). As a repellent, thiamine is touted as a ‘natural’ alternative to DEET (Maia and Moore, Reference Maia and Moore2011; Shelomi, Reference Shelomi2020). The different online sources publicizing thiamine as a repellent all recommend differing dosages and delivery mechanisms, and differ on the number of doses needed to induce effect: some products claim to work almost immediately, while others claim they must be used regularly for days or weeks to become effective (Ives and Paskewitz, Reference Ives and Paskewitz2005).
Is there any truth to these claims? Nothing in mosquito biology suggests they would be particularly repelled by or attracted to thiamine, as thiamine is an essential nutrient for mosquito larvae (Trager and Subbarow, Reference Trager and Subbarow1938; Kleinjan and Dadd, Reference Kleinjan and Dadd1977). No reports link beriberi or genetic defects in thiamine metabolism to increased susceptibility to mosquito bites (Marcé-Grau et al., Reference Marcé-Grau, Martí-Sánchez, Baide-Mairena, Ortigoza-Escobar and Pérez-Dueñas2019). Thiamine is also not without risks. While oral thiamine supplementation has low risks (Scientific Committee on Food, Reference Scientific Committee on Food2006), rare but potentially lethal side effects were reported for parenteral delivery of thiamine at doses above 100 mg (Wrenn et al., Reference Wrenn, Murphy and Slovis1989; Proebstle et al., Reference Proebstle, Gall, Jugert, Merk and Sterry1995). During the 1940's (Laws, Reference Laws1941; Mills, Reference Mills1941; Schiff, Reference Schiff1941; Brown, Reference Brown1944), reports of sensitization and allergic reactions from subcutaneous thiamine injection were noted, including symptoms such as pruritus (itching), nausea, ataxia, anxiety, cyanosis, anaphylactic shock, and death. Although later studies reported lower toxicity and fewer adverse effects (Scientific Committee on Food, Reference Scientific Committee on Food2006), cases of allergic symptoms like pruritis after thiamine injection were still noted (Wrenn et al., Reference Wrenn, Murphy and Slovis1989; Royer-Morrot et al., Reference Royer-Morrot, Zhiri, Paille and Royer1992). Contact dermatitis was also reported from workers at a pharmaceutical plant making injectable thiamine ampoules (Combes and Groopman, Reference Combes and Groopman1950), and from a patient sensitized after thiamine ingestion (Hjorth, Reference Hjorth1958). Beyond these direct risks, using ineffective repellents can also cause indirect harm by providing a false sense of security (Pollack et al., Reference Pollack, Kiszewski and Spielman2002), such that people who use thiamine as their sole prophylactic when traveling to areas with endemic, mosquito-borne pathogens like malaria will be insufficiently protected (Mølle et al., Reference Mølle, Christensen, Hansen, Dragsted, Aarup and Buhl2000). Thus, a rationale exists for a scoping review of the evidence for the concept of systemically repellent thiamine.
The goal of this review is to settle, for the 21st century reader, the following research questions: What is the evidence for thiamine in the prevention or treatment of arthropod bites? If this evidence exists, then what is the best way to apply thiamine and at what dosage? If no evidence for efficacy exists, and/or evidence for lack of efficacy exists, then what are the challenges to overcoming incorrect knowledge in the general population?
Materials and methods
This paper is a critical appraisal of all available evidence regarding thiamine and insect biting, spanning nearly 80 years of research worldwide. A scoping review was chosen because the literature on the subject is highly heterogeneous, such that statistical analysis of a systematic review is not feasible, and narrative synthesis is employed (Tricco et al., Reference Tricco, Lillie, Zarin, O'Brien, Colquhoun, Levac, Moher, Peters, Horsley, Weeks, Hempel, Akl, Chang, McGowan, Stewart, Harting, Aldcroft, Wilson, Garritty, Lewin, Godfrey, Macdonald, Langlois, Soares-Weiser, Moriarty, Clifford, Tunçalp and Straus2018). As a scoping review, it follows the PRISMA-Scr checklist, and serves to ‘systematically map the research done in this area, as well as to identify any gaps in knowledge’ (Tricco et al., Reference Tricco, Lillie, Zarin, O'Brien, Colquhoun, Levac, Moher, Peters, Horsley, Weeks, Hempel, Akl, Chang, McGowan, Stewart, Harting, Aldcroft, Wilson, Garritty, Lewin, Godfrey, Macdonald, Langlois, Soares-Weiser, Moriarty, Clifford, Tunçalp and Straus2018). The final protocol is registered with the Open Science Framework and is publicly available (https://osf.io/jm8hq/).
Any references (excluding patents) on Google Scholar or PubMed mentioning thiamin[e] or vitamin[e] B1 and repellency, mosquitoes, fleas, midges, bedbugs, or ticks, as well as the papers cited by these papers and any literature that cited them and contained the relevant terms, were obtained online or through interlibrary loans. This method has been shown to sufficiently cover all relevant studies for literature reviews (Bramer et al., Reference Bramer, Giustini, Kramer and Anderson2013; Gehanno et al., Reference Gehanno, Rollin and Darmoni2013), and in this case the search on PubMed did not reveal any publications Google Scholar missed. Using multiple spellings of the terms ensured older papers and papers of non-English, Roman alphabet languages were included in the review. Review papers, case studies, research papers, letters to the editor, and commentary articles were included, as were government documents and legal documents. Articles from predatory journals were noted but not factored into the analysis of the evidence. Popular science or non-academic books, websites such as blogs or wikis, news media, posters, and advertisements were also excluded. While no prior reviews on thiamine as a repellent exist, this paper also covers past review papers on thiamine sensu lato, and on repellents, arthropod-vectored disease prevention, and insect bite symptom treatment sensu lato, to see whether or not they mentioned repellency or thiamine respectively. The PRISMA flowchart summarizing the data collection process is presented in fig. 1.
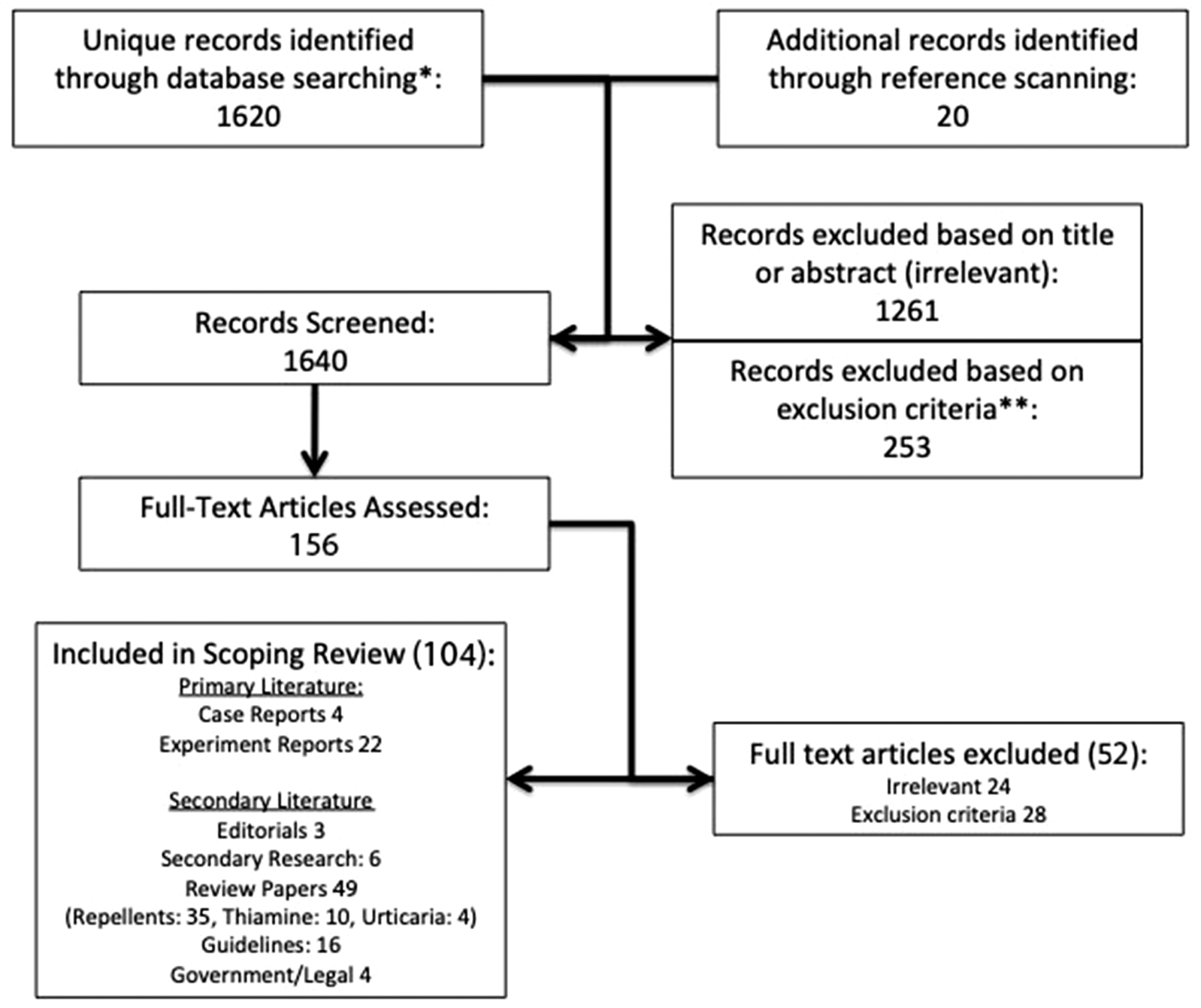
Figure 1. PRISMA flowchart for the scoping review process. *Search performed on 19 November 2020 using the protocol registered with Open Science Framework (https://osf.io/jm8hq/). **Excluded report formats were websites, blogs, news media, advertisements, posters, and articles in predatory journals.
Results
Statistics
Excluding duplicates, a total of 1620 citations were identified from searches of electronic databases, and 20 more from reference lists of other literature. Based on the title and abstract, 1261 were excluded, and another 253 excluded for being in excluded literature categories. In total 156 full-text articles were retrieved and assessed for eligibility. Of these, 24 were excluded for being irrelevant, and 28 for being websites, news media, articles in predatory journals, or other excluded literature.
Of the remaining 104 references (Supplementary table 1), four were case reports or anecdotes from medical doctors, of which three suggested thiamine is effective and one stated conflicting reports [Such papers' conclusions will be described as ‘ambivalent’ henceforth and in Supplementary table 1]. Of the research papers, 22 were replication studies testing thiamine as a repellent, although several used reduction of bite symptoms as a proxy for repellency. Of these, four examined effects on lab animals, 15 on humans, and three on both. Relatively few, most of which were uncontrolled studies, had positive conclusions, while the majority found thiamine ineffective.
This review also considered other reviews and ‘secondary literature,’ here defined as papers that cite the ‘primary literature’ generating new data about thiamine, but not generating new data about thiamine themselves. Of the 49 review or synthesis papers, 35 were reviews of insect repellents in general or ways to prevent insect bites or insect-vectored diseases, of which three made no mention of thiamine, five were ambivalent as to whether or not thiamine is repellent, and 27 explicitly stating it is not an effective repellent. Ten were reviews of thiamine itself, of which seven made no mention of its purported repellence, one was ambivalent, and two explicitly dismissed this as false. Four reviews were found in medical literature discussing urticaria, of which one from 1944 claimed oral thiamine caused urticaria symptoms (Brown, Reference Brown1944), two claimed thiamine has no positive or negative effect, and one made no mention of thiamine. Also found were six ‘secondary’ research papers studying the repellents recommended by doctors or used by patients or travelers, all of which referred to thiamine as an ineffective repellent. Of the 16 published guidelines on avoiding biting arthropods or preventing insect-vectored disease found, the oldest claimed thiamine worked, the next two oldest were ambivalent, and the rest claimed thiamine is ineffective. Three editorials or commentary articles and four government documents or legal documents found all claimed thiamine is not repellent (Supplementary table 1).
Case reports
The origin of the thiamine-as-systemic-repellent idea is a paper from 1943 by Minnesota pediatrician W Ray Shannon (Reference Shannon1943). Shannon's ‘preliminary report’ describes ten cases in which he used thiamine to control itching symptoms from mosquito bites in children ‘prone to bites’ from 8.5 months to seven years old, plus three adults of unspecified age. This derives from a prior report by Shannon where he claims thiamine is a general anti-itching medication (Shannon, Reference Shannon1942). Doses were oral or, in one case, subcutaneous, and ranged from 10–120 mg delivered 1–4 times a day, typically with a larger loading dose on the first day and smaller doses thereafter for one day up to two months. While initial treatments were likely done in his office, subsequent treatment and reporting of symptoms was done by at home by the adult patients or the children's caregivers. While the thiamine was prescribed as an anti-pruritic, nine of these reports mentioned that the patients obtained ‘complete protection [from mosquitoes] for the rest of the summer,’ leading Shannon to state that oral or injected thiamine causes ‘susceptible persons to become not only tolerant but actually repellent to mosquitoes.’ He also noted that a topical ointment of thiamine did not repel mosquitoes.
In 1945, California physician Howard L Eder gave ‘a large number’ of pediatrics patients thiamine specifically to repel fleas. The treatments were typically two to four doses of 10 mg thiamine daily for a few days followed by one 10 mg dose daily, and, after several weeks, ‘apparently gave complete protection against flea bites’ (Eder, Reference Eder1945). From his description, the possibility exists that Eder mistook outdoor chiggers (mites of the family Trombiculidae) for predominantly indoor fleas. Both flea and chigger bites are typically seasonal and their bites always resolve within weeks, so there is no evidence from Eder's data that thiamine was related to his patients' reported improvement over weeks of time. Nonetheless, by 1949, oral thiamine was being used as a flea repellent across California for humans and animals, with reported results ranging from ‘100 percent effective’ to ‘completely worthless’ (Lunsford, Reference Lunsford1949; Perlman, Reference Perlman1962; Marks, Reference Marks1969).
In 1958, European physician Dieter Müting reported taking four 50 mg doses of thiamine daily along with his wife while vacationing in Lapland, and experiencing no mosquito bites by the third day (Müting, Reference Müting1958). One notes how the necessary dosage and time to effect has increased greatly since the time of Shannon and Eder, when effective daily doses could be as low as 5 mg. Müting also reported a ‘discharge’ attempt where mosquitoes returned to bite the couple shortly after they ceased thiamine therapy. As the study is uncontrolled and the Mütings' intake of dietary thiamine and of thiamine-reducing substances such as coffee or alcohol is unreported during this time, the value of this self-experimentation is low: it could easily have been biased by a placebo effect, or ‘nocebo’ effect in the case of discharge, as well as daily variation in activity levels, bathing, clothing exposure, or location within Lapland that could affect exposure to mosquitoes. Müting also hypothesized that either thiamine or a breakdown product thereof excreted through the skin after 2–3 days is responsible for the repellency effect, although this was already known to be false at the time of his writing (Cornbleet et al., Reference Cornbleet, Kirch, Bergeim and Solomon1943; Tennent and Silber, Reference Tennent and Silber1943).
Experiment reports
Of the 22 experimental reports found, four studies expressed ‘positive’ results. One was a study with cat fleas on humans fed or injected with thiamine, which paradoxically concluded that the fleas are repelled despite the data actually showing fleas eagerly feeding at first (Lunsford, Reference Lunsford1950). The second was an uncontrolled study with an unknown number of humans given 200 mg thiamine orally, which reported that mosquitoes would approach and land but not probe or feed (Velasco and Varela, Reference Velasco and Varela1965). The third was an uncontrolled study from Mexico on papular urticaria (‘insect prurigo’ in Spanish) that found improvement of symptoms in most subjects orally taking 200–300 mg of thiamine daily (Ruiz-Maldonado and Tamayo, Reference Ruiz-Maldonado and Tamayo1973). The authors did not measure repellency, but concluded the observed reduction in symptoms was due to thiamine's repellency despite insect prurigo being known to resolve spontaneously. A recent, uncontrolled study on eight humans in Egypt tested repeated, topical applications of 2–5 mg thiamine on arms put into cages with mosquitoes (Badawi et al., Reference Badawi, El Halawany and Latif2020). The number of bites on the treated arms decreased after each dose, so the authors concluded thiamine is repellent, but lack of a negative control meant they did not account for the possibility that individual mosquitoes were sated after biting and were simply less likely to bite over time.
All 18 other experimental studies by doctors and entomologists alike (Goldman, Reference Goldman1950), notably including all the well-controlled studies, found thiamine unambiguously ineffective as a repellent. In the 1940's the USA Naval Medical Research Institute attempted to replicate Shannon's findings (Wilson et al., Reference Wilson, Mathieson and Jachowski1944). Using Aedes aegypti (Diptera: Culicidae) mosquitoes, they compared three subjects that took 30 mg four times a day for three days compared to three controls, and found that mosquito biting rate and the subjects' reactions to the bites in the two groups did not differ. In the same year when Müting called for verification of his attempts, a study in Switzerland of four men and three women exposed under controlled conditions to bites on a prescribed area of skin found that ingestion of pills from 250 to 1000 mg of thiamine did not provide any repellent effect, although they did provide partial relief of local irritation (Rahm, Reference Rahm1958). A Norwegian study found that 100 mg oral tablets given twice or thrice a day for six days did not reduce the incidence of mosquito bites (Brunn, Reference Brunn1964; Udjus, Reference Udjus1965). An experiment in Liberia compared oral thiamine supplementation with blood thiamine levels and attractiveness to Culex pipiens fatigans (Diptera: Culicidae) and Anopheles gambiae (Diptera: Culicidae), and found no effect (Maasch, Reference Maasch1973). Observational studies also reported negative results (Smith, Reference Smith1970). In one, the attractiveness of hospitalized patients to mosquitoes was measured in an attempt to identify a drug or disease that induces systemic unattractiveness. None were found, with vitamin B1 specifically mentioned as ineffective (Strauss et al., Reference Strauss, Maibach and Khan1968). In another, 51 Brazilian military personnel stationed in the Amazon were surveyed about their use of repellents. Two stated they used vitamin B1, and both found it ineffective (Ribas and Carreño, Reference Ribas and Carreño2010). Replication research by dermatologists and entomologists alike using larger sample sizes, multiple mosquito species, and more robust controls consistently found no effect of oral thiamine supplementation on the attractiveness of humans or their volatile skin extracts (Ives and Paskewitz, Reference Ives and Paskewitz2005).
Controlled veterinary studies reached the same negative conclusions, including bioassays on laboratory mice using thiamine topically (Lal et al., Reference Lal, Ginocchio and Hawrylewicz1963) and orally (Silva et al., Reference Silva, Braz, Martins, Di Pietro and Mazzucati1995). Tests with thiamine and Brewer's yeast on dogs found it unable to repel or kill fleas (Halliwell, Reference Halliwell1982; Baker and Farver, Reference Baker and Farver1983). A large experimental study from the Ontario Veterinary College tested not only thiamine, but also an extensive range of ‘all available substances which might reveal possibilities as orally-administered repellents,’ delivered at various doses to ‘guinea pigs, rabbits, rats, mice, hamsters and occasionally man’ for two days each, after which the subjects were exposed to Ae. aegypti mosquitoes (Kingscote, Reference Kingscote1958). The effects of age, sex, pregnancy, diet, and blood sugar levels of the subjects as well as the temperature, humidity, health, age, and other related factors regarding the mosquitoes were all investigated, with all experiments replicated and with position correction factors considered. All results were negative.
The first clinical trial, pointedly titled ‘Vitamin B1 is not a systemic mosquito repellent in man’ describes several studies (Khan et al., Reference Khan, Maibach, Strauss and Fenley1969). The first used adults aged 30–50 given 3 × 50 mg doses for three days and measured the time until mosquito probing and a number of mosquitoes feeding until engorged, and found that mosquitoes probed sooner on thiamine-fed subjects. The second was a paired, double-blinded, placebo-controlled experiment of 3 × 200 mg thiamine over two days where a treated and control person would sit in a room with 100 hungry female Ae. aegypti as an observer collected mosquitoes feeding on the subjects. The thiamine group was bitten more frequently, albeit not statistically significantly. ‘In neither experiment was there evidence of less attraction in thiamine treated subjects’ (Khan et al., Reference Khan, Maibach, Strauss and Fenley1969). The authors also tested topical thiamine, and measured the effects of thiamine on itching and wheal formation, and found no effect (Khan et al., Reference Khan, Maibach, Strauss and Fenley1969). The paper also contains possibly the first controlled test of a thiamine-based product marketed as a ‘natural’ pest repellent, Tixtak (AB Cernelle, Vegeholm, Sweden). Khan et al. (Reference Khan, Maibach, Strauss and Fenley1969) tested it on guinea pigs at four tablets [dose unknown] per kilogram, with un-dosed animals as the control, and found mosquitoes bit the dosed animals ‘as avidly as the control’ (Khan et al., Reference Khan, Maibach, Strauss and Fenley1969). [AB Cernelle, which had previously been sued in the United States for false advertisement (US Senate, Reference US Senate1963), still exists today, but Tixtak is no longer sold.]
Secondary literature
Over time, review papers on insect repellents and on insect bite prevention were less ambivalent and increasingly noted the difference in quality between the papers claiming thiamine was repellent and those demonstrating through controlled experiment that it was not (Hocking, Reference Hocking1952, Reference Hocking1963; Beales and Kouznetsov, Reference Beales, Kouznetsov, Steffen, Lobel, Haworth and Bradley1989). Most review papers on mosquito repellents from the 1990's onward either make no mention of thiamine supplementation (Moore and Debboun, Reference Moore, Debboun, Debboun, Frances and Strickman2007; Paluch et al., Reference Paluch, Bartholomay and Coats2010), or refer to it and/or other oral repellents like garlic and Brewer's yeast as unambiguously ineffective (Fradin, Reference Fradin1998; Holzer, Reference Holzer2001; Fradin and Day, Reference Fradin and Day2002; Canadian Paediatric Society, 2003; Miller, Reference Miller2004; Rudin, Reference Rudin2005; Goad, Reference Goad2006; Sturchler, Reference Sturchler and Schlagenhauf-Lawlor2008; Goodyer et al., Reference Goodyer, Croft, Frances, Hill, Moore, Onyango and Debboun2010; Singh et al., Reference Singh, Singh and Mohanty2012; Croft, Reference Croft2014; Onyett and Canadian Paediatric Society Infectious Diseases and Immunization Committee, Reference Onyett2014; Ramírez-Galván and Palacios-López, Reference Ramírez-Galván and Palacios-López2019). Veterinary research has reached similar conclusions: Scientific review papers on flea repellents in animals have examined thiamine, yeast, B-complex, sulfur, and ultrasonic-based repellents, and found them all equally ineffective (Dryden and Rust, Reference Dryden and Rust1994; Dryden et al., Reference Dryden, Payne and Smith2000; Case et al., Reference Case, Daristotle, Hayek and Raasch2013).
Also worth mentioning are review papers on thiamine itself, such as its biochemistry and clinical or therapeutic uses. By the 21st century, such reviews typically make no mention at all of thiamine as a repellent, nor do they mention any sulfurous metabolic degradation products or any thiamine involvement whatsoever in the skin or sweat (Lonsdale, Reference Lonsdale2006, Reference Lonsdale and Eskin2018; Ang et al., Reference Ang, Alviar, Dans, Bautista-Velez, Villaruz-Sulit, Tan, Co, Bautista and Roxas2008; Fattal-Valevski, Reference Fattal-Valevski2011; Manzetti et al., Reference Manzetti, Zhang and van der Spoel2014). This includes reviews published in evidence-based complementary and alternative medicine journals (Lonsdale, Reference Lonsdale2006; Fattal-Valevski, Reference Fattal-Valevski2011). One review (Zbinden, Reference Zbinden1962) dismissed most medicinal uses of thiamine outside of treating thiamine deficiency due to both evidence of absence (meaning documented evidence from controlled experiments that thiamine is not effective) and absence of evidence (meaning no documented evidence from controlled experiments that thiamine could be effective). These reviews on thiamine written by leading authorities on thiamine thus provide no evidence that oral thiamine is a systemic repellent, nor do they provide any plausible mechanism from its pharmacology for how it could theoretically function as one.
Similarly, nearly all academic or government-published guidelines on avoiding insect bites from around the world state definitively that vitamins are not oral repellents (Rustad, Reference Rustad1992; Holzer, Reference Holzer1993; Cooper and Francis, Reference Cooper and Francis2002; Whelan, Reference Whelan2003; Boulanger, Reference Boulanger2007; Schofield and Plourde, Reference Schofield and Plourde2012; Juckett, Reference Juckett2013; Chiodini et al., Reference Chiodini, Field, Whitty and Lalloo2014; McGregor, Reference McGregor2014; Parpillewar, Reference Parpillewar2018; Delaigue et al., Reference Delaigue, Signolet, Consigny, de Gentile, D'ortenzio, Gautret, Sorge, Strady and Bouchaud2020). The exceptions are older papers that only imply oral thiamine is ‘sometimes useful’ (Kennedy, Reference Kennedy1965) or ‘might be worth a try’ (Kennedy, Reference Kennedy1965; Honig, Reference Honig1986), and a German guidebook for travel medicine that recommended both DEET and oral thiamine at 300–1500 mg a day for mosquito bite prevention while admitting the latter is not based on controlled studies and is controversial (Steffen, Reference Steffen1984). Question-and-answer columns in British (no author, 1965) and American (no author, 1977) medical journals answered the thiamine-repellency question in the negative. The results summarized are that not only have most individuals and organizations primarily interested in protecting citizens from insect bites and reducing the burden of nuisance bites and vector-borne pathogens rejected the notion that oral thiamine is a systemic repellent, but also that this notion has been widespread enough among the general public from the 1960s until today that these authors deemed it prudent to address and explicitly refute it.
A ‘turning point’ (Proctor, Reference Proctor2012) in the general recognition of the scientific consensus on thiamine as a systemic insect repellent can arguably be dated to 1985, when the USA Food and Drug Administration evaluated the evidence and issued a final rule declaring that all oral insect repellents including thiamine ‘are not generally recognized as safe and effective’ (Food and Drug Administration, 1985). Labeling an oral thiamine-based product as having repellency properties is thus considered ‘misbranding’ and a violation of US law. Demonstrative of this consensus, researchers today use thiamine explicitly as an example of an ineffective repellent, as in survey-based studies on whether travelers or military personnel are taking adequate precautions against insect-vectored pathogens (Mølle et al., Reference Mølle, Christensen, Hansen, Dragsted, Aarup and Buhl2000; Chen et al., Reference Chen, Wilson and Schlagenhauf2006; Schoepke et al., Reference Schoepke, Steffen and Gratz2006; Kodkani et al., Reference Kodkani, Jenkins and Hatz2008; Piyaphanee et al., Reference Piyaphanee, Wattanagoon, Silachamroon, Mansanguan, Wichianprasat and Walker2009). Thiamine is not recommended in a good practices document commissioned by the French High Health Authority (Legros et al., Reference Legros, Ancelle, Caumes, Dardé, Delmont, Descloitres, Imbert, De Gentile, Migliani, Ouvrard, Robert, Duvallet, Boulanger, Chandre, de Verdière, Consigny, Delaunay, Depaquit, Doudier, Franc, Moulin, Pagès, Prangé, Quatresous, Robert, Saviuc, Auvin, Carsuzza, Cochet, Darriet, Demantké, Elefant, Failloux, de Gentile, Lagneau, La Ruche, Pecquet, Sorge, Tarantola, Vauzelle, Ajana, Armengaud, Boutin, Chevaillier, Gagnon, Genty, Girod, Godineau, Guiguen, Hatchuel, Hengy, Izri, Jean, Jourdain, Lamaury, Marchou, Masson, Minodier, Pérignon, Piccoli, Quinet, Yébakima, Santi-Rocca and Smith2011), the Brazilian National Sanitary Surveillance Agency is mentioned as not approving of thiamine's use as a repellent (Duarte et al., Reference Duarte, Moron, Timerman, Fernandes, Mariani Neto, Almeida Filho, Werner Junior, Santo, Steibel and Bortoletti Filho2017), and thiamine is explicitly mentioned as ineffective in the Canadian Recommendations for the Prevention and Treatment of Malaria Among International Travelers (Boggild et al., Reference Boggild, Brophy, Charlebois, Crockett, Geduld, Ghesquiere, McDonald, Plourde, Teitelbaum and Tepper2014). The results suggest that at a point no later than the 1980s, the confluence of diverse forms of scientific evidence ‘prompted health and medical authorities throughout the world to publicly acknowledge’ that oral thiamine is not a safe and effective repellent and should not be used as such (Proctor, Reference Proctor2012).
Note that a scientific consensus does not imply unanimous acceptance or awareness (Proctor, Reference Proctor2012). A 2008 study of Swiss pharmacists found that up to 20% still recommended vitamin B1 to patients traveling in malaria-endemic areas (Kodkani et al., Reference Kodkani, Jenkins and Hatz2008). A 2020 study of Australian pharmacists found that 27% think thiamine repels mosquitoes, and only 77% selected ‘clinically justifiable’ chemoprophylaxis for malaria (Heslop et al., Reference Heslop, Speare, Bellingan and Glass2020). A 2002 vaccine study in Mexico by the same team that used thiamine to treat papular urticaria (Ruiz-Maldonado and Tamayo, Reference Ruiz-Maldonado and Tamayo1973) mentioned using 150 mg daily of thiamine as a repellent ‘in accordance with the Ethics Committee instructions’ (Giraldi et al., Reference Giraldi, Ruiz-Maldonado, Tamayo and Sosa-de-Martínez2002). Since this review was performed, the same pharmacist authors of the uncontrolled study in Egypt claiming thiamine is a repellent (Badawi et al., Reference Badawi, El Halawany and Latif2020) cited that paper to justify an uncontrolled experiment of a topical formulation consisting of thiamine-loaded pullulan acetate nanospheres in a pluronic hydrogel (Halawany et al., Reference Halawany, Latif and Badawi2021). They concluded the thiamine hydrogel is as repellent as DEET, but because the study lacked a negative control, the possibility remains that the hydrogel without thiamine would have been equally repellent. In addition to peer-reviewed journals; non-scientific, pseudoscientific (Williams, Reference Williams2003), and predatory publications still publish papers claiming vitamins are repellent. The German Mesotherapy Society claims, without evidence, that it can prevent mosquito bites using subcutaneous injections of thiamine, among other demonstrably false claims associated with the pseudoscience of mesotherapy (Rotunda and Kolodney, Reference Rotunda and Kolodney2006). Due to the aforementioned legal restrictions on falsely branding oral thiamine as a repellent, thiamine retailers are re-formulating the product into transdermal patches that claim to introduce thiamine into the body non-orally while repelling insects. Several extremely low-quality papers published in non-peer-reviewed, predatory journals claimed that transdermal thiamine products are effective (Kalita et al., Reference Kalita, Bora and Sharma2013; Naseem et al., Reference Naseem, Malik and Munir2016), however controlled experiments of several mosquito patch products containing 300 mg thiamine found them ineffective (Revay et al., Reference Revay, Junnila, Xue, Kline, Bernier, Kravchenko, Qualls, Ghattas and Müller2013; Rodriguez et al., Reference Rodriguez, Drake, Price, Hammond and Hansen2015).
Discussion
To summarize the results of this review (Supplementary table 1): in controlled experiments, thiamine does not appear to repel biting insects of any species, in humans or animals, at any dose, over any period of time, and in any formulation: topical, oral, subcutaneous, or transdermal. This statement is accepted by the majority of the medical, veterinary, or entomological community at this time, such that all statements by relevant authorities worldwide since the 1990s disadvise its use as an oral repellent. However, some medical practitioners still prescribe oral thiamine as a repellent, and low-quality papers with insufficient references describing uncontrolled experiments testing parenteral thiamine as a repellent are still being published. The remaining question therefore is, how did the myth of thiamine as an oral repellent arise, and why does it persist?
Early papers alleging thiamine's repellency were not controlled experiments, but instead frequently based on second-hand reporting of subjective impressions of biting or on improvement in symptoms post-bite. After Shannon's papers, later publications would provide a better understanding of the physiology of insect bite reactions that explained most of his findings (Mellanby, Reference Mellanby1946; Gordon and Crewe, Reference Gordon and Crewe1948). Attractiveness to mosquitoes and the intensity of the reaction to mosquito bites are uncorrelated and each affected by multiple factors, meaning the individuals who attract the most mosquitoes are not necessarily those with the most bites, and vice versa (Téllez, Reference Téllez2005). Mosquito bite reactions consist of two parts: an immediate reaction that appears within minutes and improves within two hours, and a delayed reaction that emerges after 20–24 h and lasts for days. Whether or not one experiences the immediate or delayed reactions also changes with repeated exposure to mosquitoes, until eventually one has no response at all (Mellanby, Reference Mellanby1946; Oka and Ohtaki, Reference Oka and Ohtaki1989; Tatsuno et al., Reference Tatsuno, Fujiyama, Matsuoka, Shimauchi, Ito and Tokura2016). The alleged immediate effects of thiamine on mosquito bite symptoms may be the inevitable vanishing of the immediate reaction, while the reported decreased reactions over longer periods of time may thus be due to reduced sensitivity to the mosquito allergen, matching an anecdotal belief in certain countries that bite reactions are bigger at the onset of mosquito season and become weaker as the summer progresses (Reunala et al., Reference Reunala, Brummer-korvenkontio and Palosuo1994). Thus, in the early case reports that used symptoms as a proxy for biting, a natural progression in patients' bite reactions may have been mistaken for repellency.
Our knowledge of thiamine has also improved greatly since its discovery (Lonsdale, Reference Lonsdale2006; Sriram et al., Reference Sriram, Manzanares and Joseph2012). Thiamine is actively absorbed in the upper small intestine until saturated and passively thereafter, though absorption declines rapidly at oral doses above 5 mg. Excess thiamine is actively excreted in the urine, such that higher doses do not significantly raise plasma levels of thiamine, and such that diuretics lead to thiamine deficiency (Sriram et al., Reference Sriram, Manzanares and Joseph2012; Pacei et al., Reference Pacei, Tesone, Laudi, Laudi, Cretti, Pnini, Varesco and Colombo2020). Alcohol is notorious for causing thiamine deficiency in affluent nations by interfering with thiamine intake, absorption, and cellular utilization (Martin et al., Reference Martin, Singleton and Hiller-Sturmhöfel2003). Other foods or drugs that can reduce thiamine concentrations in the body due to the presence of thiamine antagonists and thiaminases include tea, coffee, betel nut, raw fish, and certain edible insects (Nishimune et al., Reference Nishimune, Watanabe, Okazaki and Akai2000; Ehigie et al., Reference Ehigie, Emuebie and Ehigie2013; Pacei et al., Reference Pacei, Tesone, Laudi, Laudi, Cretti, Pnini, Varesco and Colombo2020). While primarily excreted in the urine, free thiamine is also secreted in the sweat (Cornbleet et al., Reference Cornbleet, Kirch, Bergeim and Solomon1943), with approximately 8% of ingested thiamine secreted through the skin (Alexander and Landwehr, Reference Alexander and Landwehr1946). The amount of thiamine in the sweat increases by an order of magnitude when subjects are given large oral doses, but the amount is still so small (<1 μg per 1 ml sweat) as to be insignificantly different (Cornbleet et al., Reference Cornbleet, Kirch, Bergeim and Solomon1943; Tennent and Silber, Reference Tennent and Silber1943), while thiamine excretion in urine greatly increases with such oral dosing. Thiamine in sweat seems to have no impact on skin bacteria, and vice versa (Cornbleet et al., Reference Cornbleet, Kirch, Bergeim and Solomon1943). Thiamine is poorly stored, mostly as protein-bound thiamine diphosphate in the liver, heart, kidneys, and brain, and only for 1–3 weeks. Its blood plasma levels are tightly regulated, with excretion of excess complete in four to six hours post-ingestion of an oral dose, such that the total vitamin B1 content of the average human is maintained at approximately 30 mg (van Snippenburg et al., Reference van Snippenburg, Reijnders, Hofhuis, de Vos, Kamphuis and Spronk2017). The elimination half-life is either between 1–12 h (Pacei et al., Reference Pacei, Tesone, Laudi, Laudi, Cretti, Pnini, Varesco and Colombo2020) or approximately 1.8 days (Scientific Committee on Food, Reference Scientific Committee on Food2006). At no point does the sulfur moiety of the molecule leave thiamine or its phosphates during any metabolic stages between normal consumption and excretion (Cornbleet et al., Reference Cornbleet, Kirch, Bergeim and Solomon1943; Tennent and Silber, Reference Tennent and Silber1943). To summarize: nothing in the chemistry of thiamine metabolism would explain how thiamine could be repellent, nor does it justify the extremely high doses typically used in the above papers, most of which would not even be absorbed. Thiamine as systemic repellent is pharmacologically highly implausible.
While thiamine is not repellent, the possibility exists that its effects on bite symptoms may not just be a placebo effect (Obermayer and Frost, Reference Obermayer and Frost1945). A few authors tested for this possibility (Ruiz-Maldonado and Tamayo, Reference Ruiz-Maldonado and Tamayo1973), including Khan et al. (Reference Khan, Maibach, Strauss and Fenley1969), whose controlled experiments found thiamine ineffective, and Lunsford (Reference Lunsford1950) and Rahm (Reference Rahm1958), whose uncontrolled experiments found it possibly reduced local symptoms. Fewer researchers have studied thiamine as an anti-pruritic than as a repellent, and any such papers face the problem that itch response can vary widely in the same individual for both physiological and psychological reasons (Nakao & Barsky, Reference Nakao and Barsky2007; Ogden & Zoukas, Reference Ogden and Zoukas2009; Colloca & Miller, Reference Colloca and Miller2011; Papoiu et al., Reference Papoiu, Wang, Coghill, Chan and Yosipovitch2011; Lloyd et al., Reference Lloyd, Hall, Hall and McGlone2013; Sukan & Maner, Reference Sukan and Maner2015). However, unlike systemic repellency, thiamine as post-bite treatment is pharmacologically plausible. Thiamine has been noted as an anti-inflammatory agent before (Manzetti et al., Reference Manzetti, Zhang and van der Spoel2014), and thiamine deficiency is a known cause of peripheral neuropathy and neuritis (Ang et al., Reference Ang, Alviar, Dans, Bautista-Velez, Villaruz-Sulit, Tan, Co, Bautista and Roxas2008). Vitamin B complex was recommended in the 1940s for allergic dermatoses, although the mode of action was unknown (Obermayer and Frost, Reference Obermayer and Frost1945), and shows potential in treating multiple different types of pain (Jurna, Reference Jurna1998; Lonsdale, Reference Lonsdale and Eskin2018). Thiamine injection was also reported as useful against chronic urticaria when injected into acupuncture points (Tong and Song, Reference Tong and Song1986), although neither thiamine nor acupuncture has been systematically confirmed as effective for pain in controlled studies (Chen and Yu, Reference Chen and Yu1998). In recent reviews of treatment for urticaria, including that caused by insects, vitamins are not listed as a treatment, valid or invalid (Schaefer, Reference Schaefer2017; Antia et al., Reference Antia, Baquerizo, Korman, Alikhan and Bernstein2018). It is therefore plausible, albeit not probable based on a scoping review of the literature, that thiamine supplementation, oral or parenteral, can reduce symptoms of insect bites.
The persistence of the myth that thiamine is repellent is easier to explain. A medical myth, ‘even if it is never fully published, discussed, and examined by other scientists… may become regarded as common knowledge and eventually be referred to even in the scientific literature’ (Winkler and Anderson, Reference Winkler and Anderson1990). Pseudo-scientific articles promoting thiamine as a repellent are pervasive throughout non-academic media such as news, popular science and health websites, and wellness blogs. The myth of thiamine's repellency appears often enough in the media that it may be an assumption that scientists entering the field already hold before starting their literature review, and which they can only shed upon accumulating sufficient knowledge. Unfortunately, the literature that debunks the myth of thiamine's repellency is typically behind a pay-wall in subscription-only journals, if it is online at all, while the lowest quality research is easily available in open access, predatory journals. Thus, inaccurate ideas in online, unreviewed papers purporting to have legitimate scientific authority are more easily available than facts in the actual scientific literature. In addition, positive publication bias (Mlinarić et al., Reference Mlinarić, Horvat and Šupak Smolčić2017), combined with the persistent prevalence of inappropriately designed experimental studies in both high and low impact factor journals (Masic and Jankovic, Reference Masic and Jankovic2020), means high quality, controlled studies or review papers claiming a nutraceutical does not work may be less likely to be published (Song et al., Reference Song, Parekh, Hooper, Loke, Ryder, Sutton, Hing, Kwok, Pang and Harvey2010) and cited (Duyx et al., Reference Duyx, Urlings, Swaen, Bouter and Zeegers2017) than low quality, uncontrolled studies claiming it does. These issues are linked to the reproducibility crisis in science (Bizzarri and Monti, Reference Bizzarri and Monti2019; Ioannidis, Reference Ioannidis2019), partially explaining how those who promote ineffective, thiamine-based repellents are still publishing papers today.
Just as it took time for doctors to alert patients that cigarettes cause cancer despite the existence of a scientific consensus (Proctor, Reference Proctor2012), doctors are not yet completely aware that thiamine-based and/or systemic repellents do not work. Entomologists and vector-borne disease prevention experts have been in consensus for decades that thiamine is not a mosquito repellent in any dose or by any route of administration, yet ignorance of this consensus is leading to wasted research resources and unprotected consumers at increased risk of illness. One hopes that this review, the most comprehensive ever on the subject of thiamine and arthropod bite prevention and treatment, will increase awareness of the problem. Combined with broader laws against the marketing and production of ineffective remedies, this awareness of ineffective prophylaxis can better protect people from biting insects and consumer fraud alike.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0007485321001176.
Data
The final protocol is registered with the Open Science Framework and is publicly available (https://osf.io/jm8hq/).
Acknowledgements
None.
Author contribution
MS conceived and designed the study, conducted data gathering, and wrote the article.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
The authors declare there are no conflicts of interest.
Ethical standards
Not applicable.