Introduction
Bipolar disorders (BDs) are a group of common, complex, and multidimensional mental disorders that affect mood, cognition, and behavior. They are classified into two main types, BD type I and BD type II. BD type I is characterized by the presence of one or more manic episodes, whereas BD type II includes both a hypomanic episode and a major depressive episode. Depressive components of either subgroup are the most prevalent and difficult to treat.Reference McIntyre, Berk and Brietzke1, Reference Rakofsky and Rapaport2 Depression in BD is more likely to be accompanied by atypical symptoms, such as increased sleep and appetite, as well as fatigue.Reference McIntyre, Berk and Brietzke1 The implications for those who are affected by these disorders are significant, as it impacts their physical and mental health while also being inconsistent by nature which complicates both living and treating the disorder. Ideal treatment strategies should address both manic and depressive groups of symptoms, treat acute episodes, prevent relapses and recurrences, restore functioning, and cause no or limited side effects. These goals are not always achieved by individuals living with BD, even with the adoption of evidence-based approaches.Reference SayuriYamagata, Brietzke, Rosenblat, Kakar and McIntyre3
Although frequently referred to as a mood disorder, the mental and behavioral manifestations of BD go far beyond mood. Individuals with BD exhibit widespread dysfunction across multiple central and peripheral systems including abnormalities in arousal, attention, cognition, neuroendocrine function, and even neurostructural changes.Reference McCarthy, Gottlieb and Gonzalez4 Another dimension of BD psychopathology is circadian rhythm disruption, with changes in the sleep–wake cycle being the most replicated.Reference Alloy, Ng, Titone and Boland5-Reference Soreca7 Most individuals with BD exhibit different degrees of circadian desynchronization in different moments of their illness trajectory, resembling “jet lag” via unfavorable side effects such as abnormal sleep, metabolic disturbances, and low energy.Reference Robillard, Naismith and Hickie8 In addition, there is a bi-directional relationship between circadian disruption and manic and depressive symptoms, with sleep deprivation being a trigger for manic symptoms and mood episodes being accompanied by circadian dysfunction.Reference Gold and Sylvia9, Reference Harvey, Soehner and Kaplan10 One of the most robust illness triggers is jet lag itself.Reference Walker, Walton, DeVries and Nelson11
Circadian rhythms are influenced both by the main endogenous biological clock, a distinct group of cells located in the anterior hypothalamus, and by information from both internal and external inputs, via light, sounds, feeding, exercise, and activity scheduling.Reference Steardo, de Filippis, Carbone, Segura-Garcia, Verkhratsky and De Fazio12 Neurobiological underpinnings of this association include but are not restricted to genetic factors, chronotypes, presence of sleep disturbances (eg, obstructive sleep apnea), hormones (eg, melatonin), and immune-inflammatory mediators.Reference Alloy, Ng, Titone and Boland5 The genetic control of circadian rhythm maintenance is composed of a molecular feedback loop of approximately 20 genes, known as “clock genes.”Reference Partch, Green and Takahashi13 Studies have suggested a role for the suprachiasmatic nucleus (SCN) and related genes in emotional regulation.Reference McCarthy, Gottlieb and Gonzalez4 In addition, disruptions in circadian rhythm have been implicated in a variety of adverse health effects, including mood and metabolic disturbances.Reference McCarthy, Gottlieb and Gonzalez4, Reference Pickel and Sung14 Metabolic syndrome is approximately twice as common in BD when compared to the general population and is associated with worsened mood symptoms, reduced treatment efficacy, and an unfavorable clinical course.Reference McIntyre, Danilewitz and Liauw15, Reference Moreira, Jansen and Cardoso16 Further, dysfunctional circadian rhythms have been linked to an increased susceptibility to mood switching and treatment resistance.Reference Lee, Son and Geum17 It is evident that a complex and multi-directional relationship exists between synchrony of circadian clocks, metabolic homeostasis, and mood disorders.
The study of energy intake and expenditure in mood disorders represents a unique opportunity to integrate transdisciplinary lines of research, such as chronobiology and metabolic physiology with the goal of improved patient outcomes.Reference Scaini, Rezin, Carvalho, Streck, Berk and Quevedo18, Reference Morris, Walder and Berk19 The objective of this study is to comprehensively review the clinical and mechanistic findings from different lines of evidence suggesting that imbalances in rhythmic regulation of metabolic processes are involved in the pathophysiology of BD and discuss the implications of these findings for research and clinical care.
The concept of metabolic jet lag
“Metabolic jet lag” is a recently introduced concept in the literature, designating a state of dramatic shift in circadian patterns of energy homeostasis, including but not being restricted to hormone release, adipose tissue function, and immune function which is expressed through behavioral changes including irregular sleep and feeding.Reference Asterholm and Scherer20 Under physiological conditions, metabolic rhythms are related to cyclical changes in biochemical pathways which are integral for the body to respond to the environmental changes that happen during night and day cycles.Reference Asterholm and Scherer20 The existence of such changes is thought to provide organisms with a significant evolutionary advantage, as it allows the body to anticipate nutrient needs and guarantee optimal energetic capacity during the active hours of the day.Reference Sardon Puig, Valera-Alberni, Canto and Pillon21
Metabolic jet lag constitutes a desynchronization between external cues and the temporal order of the main circadian clock and has been linked to a variety of detrimental health outcomes. For example, it is well known that shift workers or individuals consistently traveling between time zones are disproportionately affected by coronary disease, obesity, and metabolic syndrome.Reference Brum, Filho, Schnorr, Bottega and Rodrigues22-Reference Peplonska, Bukowska and Sobala24 Conversely, individuals affected by increased weight and obesity are more prone to circadian rhythmic alterations.Reference Blancas-Velazquez, Mendoza, Garcia and la Fleur25 The bi-directional link between circadian rhythmicity and metabolic health adds to the complexity in understanding the underlying mechanisms.
Several factors are involved in the pathophysiology of metabolic jet lag. The most relevant are described in the following sections.
Genetic predisposition
It is known that BD is a heritable mood disorder and recently it has been suggested that circadian disruption, a risk factor for BD, may also be heritable.Reference McCarthy, Gottlieb and Gonzalez4 The circadian rhythm is regulated by a variety of transcription and translation pathways, described in detail elsewhere.Reference Asterholm and Scherer20, Reference Maury26 Although specific genetic variation predisposing to metabolic jet lag has yet to be identified, genetic mutations in multiple clock genes are known to result in an array of health effects, including metabolic abnormalities. For example, deletion of the melatonin receptor has been shown to result in systemic insulin resistance, increased fat mass, leptin resistance, and diabetes in mice. In addition, mice lacking BMAL1 or the leptin receptor demonstrated weight gain and a shifted rhythm of food intake.Reference Li, Ma and Yao27 Studies in humans have also outlined multiple clock gene polymorphisms which are linked to obesity and metabolic syndrome including BMAL1, CRY2, and the melatonin receptor.Reference Maury26
It is also possible that a genetic predisposition to metabolic or sleep dysfunction may result in circadian rhythm abnormalities, further exacerbating metabolic jet lag in the afflicted individual. For example, mutations in PER2 have been associated with sleep–wake disorders which are more commonly diagnosed in individuals with BD compared to the general population.Reference Hoang, Yuen and Howe28, Reference Ahmad, Anderson and Watson29 Specifically, delayed sleep–wake phase disorder results in a loss of synchrony between sleep–wake and day–night cycles and is associated with potentiated relapse and the onset of mania.Reference Ahmad, Anderson and Watson29
Irregular eating rhythms
The timing of energy intake is an important peripheral cue, influencing the regulation of circadian function. Adjusting regular meal times can reset peripheral clocks, placing them out of sync with the SCN.Reference Barandas, Landgraf, McCarthy and Welsh30 In fact, a disorganized eating pattern is both an indicator of and contributor to metabolic jet lag which is related to a higher risk of obesity, metabolic syndrome, diabetes mellitus, and even some forms of cancer.Reference Ellingsen, Bener and Gehani31-Reference Van Cauter33
Eating rhythms have been shown to influence body weight and energy metabolism, even when the same amount of food is consumed because energy balance does not promote expenditure during the night hours and therefore calories are stored as fat.Reference Oike, Sakurai, Ippoushi and Kobori34 Weight gain and increased risk of cardiometabolic diseases have been observed regardless of overall food intake when eating patterns were out of sync with the SCN clock.Reference Asterholm and Scherer20, Reference Li, Ma and Yao27, Reference Barandas, Landgraf, McCarthy and Welsh30 Rodent studies have demonstrated that restoring meal timing during the active phase improves metabolic abnormalities associated with jet lag and reduces obesity, indicating a protective effect of routine feeding.Reference Salgado-Delgado, Angeles-Castellanos, Saderi, Buijs and Escobar35
Although exact mechanisms underlying the adverse effects of irregular eating rhythms remain unknown, research indicates that meal timing and physiological processes of the circadian cycle may interact to influence how metabolic systems respond to meals differently over the 24-hour day. For example, human subjects who consumed a high-calorie breakfast showed reduced weight gain, adipose tissue, fasting glucose, triglycerides, and insulin compared to subjects who consumed a high-calorie dinner late in the evening when melatonin levels are highest.Reference Li, Ma and Yao27 Additionally, a cross-sectional study of college-aged individuals demonstrated that participants who consumed most of their calories closer to the onset of melatonin secretion at night had more body fat than individuals who consumed most of their calories in the day.Reference McHill, Phillips and Czeisler36 Furthermore, irregular eating times associated with shift work have been repeatedly linked to obesity, abnormal insulin functioning, and metabolic syndrome in the literature.Reference Brum, Filho, Schnorr, Bottega and Rodrigues22, Reference Guerrero-Vargas, Espitia-Bautista, Buijs and Escobar37-Reference Wang, Zhang and Zhang40
Abnormalities in hunger, satiety, and hedonic aspects
In humans, the behavior of obtaining food and eating is highly complex and requires the integration of multiple systems. For example, it requires the interpretation of interoceptive inputs, such as the sensations of hunger and satiety, which fluctuate dynamically over time based on the energy status.Reference Quigley, Kanoski, Grill, Barrett and Tsakiris41 It also has to be integrated with the hedonic aspects of eating, which are partially independent of the energetic needs.Reference Ferrario, Labouebe and Liu42 Viewed through an evolutionary lens, obtaining food requires activity to facilitate the gathering of food (eg, foraging) and the navigation of associated risks (eg, hunting). Eating according to the socially determined times also requires learning and memory which are at least partially dependent on hippocampal activity, through the integration of past experiences with current signals from exteroception and internal energy balance. The hypothalamus plays an important role in learned control of eating behavior, highlighted by the inability of subjects with bilateral hippocampal damage to interpret interoceptive inputs such as hunger and satiety.Reference Quigley, Kanoski, Grill, Barrett and Tsakiris41 A disconnect between energy requirements and the interpretation of hunger was observed as maintained hunger ratings throughout eating phases. This confirmed that these systems can process independently but require communication to operate effectively. Overall, negative health consequences arise if humans do not receive or interpret energy requirements sufficiently, including metabolic jet lag.Reference Quigley, Kanoski, Grill, Barrett and Tsakiris41
Nutritional content
Although the timing of meals is important to maintaining metabolic synchrony with the circadian clock, studies have also indicated an important role of nutritional content. Specifically, diets with a high content of fat and sugar have been linked to disturbances in circadian rhythms. In animals, 1 week of high-fat diet was sufficient to cause a prolongation of the circadian period compared to a regular diet, an effect that was independent of changes in body weight.Reference Kohsaka, Laposky and Ramsey43 More recently, studies have indicated an underlying mechanism for this observation in which the nutritional content of food has been shown to alter the expression of clock genes. For example, obesity caused by a high-fat diet was shown to alter the expression of clock genes in the liver and kidneys.Reference Li, Ma and Yao27 In addition, disruption of intestinal L cells and pancreatic beta cells was shown in mice following obesogenic feeding, providing some explanation for the development of metabolic abnormalities on a high-fat diet.Reference Martchenko and Brubaker44
Gut microbiome health
The gut microbiome may be a factor whereby diet and meal timing impact metabolic and circadian dysfunction. The composition and functioning of the gut microbiome oscillate with the 24-hour clock. The gut epithelium interacts with different microbes throughout the course of the day and some bacteria are even entrained with melatonin levels.Reference Paulose, Wright, Patel and Cassone45 Furthermore, a bi-directional relationship has been proposed in which the microbiome may also influence clock gene expression in response to diet.Reference Bae, Fang, Rustgi, Zarbl and Androulakis46 In particular, a high-fat diet has been shown to reduce microbial diversity and patterns of metabolite production which in turn modulates clock gene expression in hepatocytes. Conversely, germ-free mice demonstrated impaired clock gene expression on both low- and high-fat diets, even when light and dark signals remained intact.Reference Leone, Gibbons and Martinez47 Therefore, gut microbiota may mediate the effects of dietary content on circadian abnormalities as the microbiome was needed to see the effects of diet on clock function. Overall, it is evident that both meal timing and composition are important factors in maintaining microbial function and, therefore, circadian alignment.
Sedentary lifestyle
Another facet of lifestyle that may predispose an individual to metabolic jet lag includes insufficient exercise or a sedentary lifestyle which has been linked to the desynchrony between metabolism and the circadian cycle. In humans, physical activity exhibits an approximate 24-hour circadian cycle and acts as a zeitgeber to entrain circadian clocks in peripheral tissues such as skeletal muscle, liver, and lungs. This has been confirmed in both animal and human studies.Reference Aoyama and Shibata48 From an evolutionary perspective, energy metabolism is optimized throughout the day–night cycle to allow humans to travel long distances for food during the waking hours. Conversely, limited physical activity may indicate the body is recovering from an injury or sickness and is associated with inflammatory responses.Reference Charansonney and Despres49 Therefore, energy expenditure responds to environmental adversity and is also an important external cue for maintaining circadian synchronization.
Sedentary lifestyles are associated with a variety of unfavorable health effects, including cardiometabolic issues such as worsened glycemic control, blood pressure, and triglyceride levels.Reference Dollet and Zierath50 Sedentary activity is reported to significantly increase glucose and insulin resistance in participants after only 5 days, including a 67% greater insulin response to a glucose load.Reference Hamburg, McMackin and Huang51 Exercise is a promoter of health in humans as well as an important circadian entrainment cue. Therefore, the widespread benefits of physical activity are important to consider in resisting the development of metabolic jet lag.Reference Wang52
Disturbances in mitochondrial metabolism
Mitochondria are organelles responsible for the generation of energy in eukaryotic cells. Dysfunctional mitochondrial function has been consistently demonstrated in several severe mental disorders, including BD. In fact, BD is often conceptualized as a mitochondrial disorder, where mania and depression are considered states of up- and down-regulation of mitochondrial function, respectively.Reference Morris, Walder and McGee53 In addition, the prevalence of BD in mitochondrial diseases is about 20 times higher than in the general population.Reference Kato54 The mitochondria of individuals with BD demonstrate significant differences in morphology and dynamics when compared with healthy individuals.Reference Scaini, Rezin, Carvalho, Streck, Berk and Quevedo18 Early observation of variations of mitochondrial morphology date from 30 years ago, when Uchiyama described that mitochondria from rat hepatocytes changed their tubular structure from the light to dark phase.Reference Uchiyama55 After this, it was demonstrated that mitochondria continuously fuse and divide, move, and are removed, depending on the energetic needs of the cells.Reference Sardon Puig, Valera-Alberni, Canto and Pillon21 The endosymbiotic theory states that mitochondria were once independent bacteria, consumed by an early eukaryotic cell; therefore, it is plausible that these organelles have their own circadian clock.Reference Manella and Asher56
Current evidence suggests that mitochondria are both influenced by circadian rhythm and exert effects on biological rhythms. Circadian factors are known to be critical regulators of mitochondrial function and demonstrate an important role in the maintenance of metabolic health.Reference Morris, Walder and McGee53 Specifically, changes in the clock genes are related to abnormalities in mitochondrial dynamics, but the opposite also happens. Adenosine monophosphate-activated protein kinase (AMPK) is responsive to AMT/ATP ratios and works to maintain energy balance as well as promoting biogenesis.Reference Sardon Puig, Valera-Alberni, Canto and Pillon21 AMPK provides a link between mitochondrial functioning and clock transcription and gene expression, having the power to destabilize circadian functioning should an imbalance occur.Reference Sardon Puig, Valera-Alberni, Canto and Pillon21 Therefore, specific mitochondrial enzymes and proteins may influence metabolic rhythms associated with changing circadian function and could be of interest as a contributing factor in altered energy homeostasis in BD (Table 1).
Table 1. Factors Contributing to the Pathophysiology of Metabolic Jet Lag
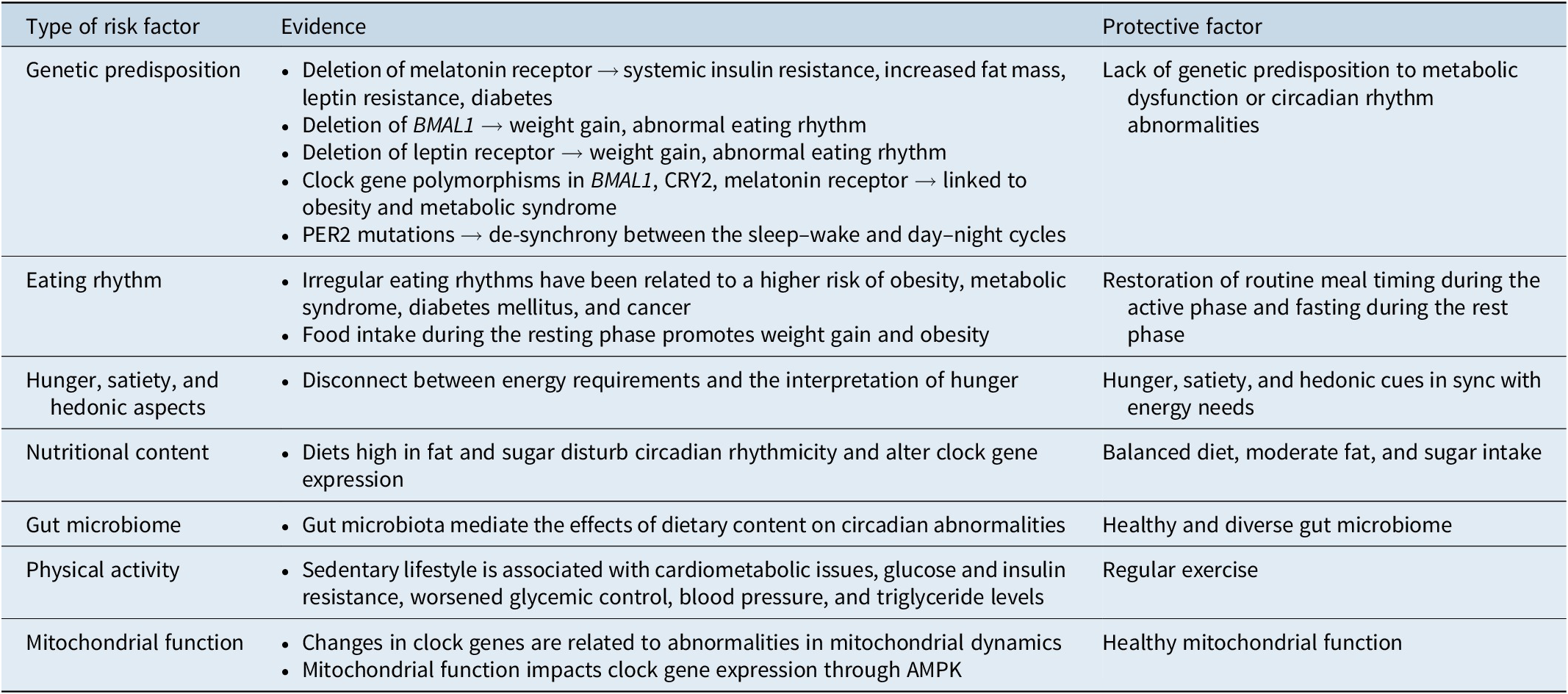
Abbreviation: AMPK, adenosine monophosphate activated protein kinase.
BD as a dysregulated energy expenditure illness
A high prevalence of metabolic abnormalities in individuals with BD, especially in those with multiple mood episodes, is well documented.Reference Vancampfort, Vansteelandt and Correll57 Metabolic abnormalities are frequent in the mood disorder population, with approximately 50% of patients having obesity, diabetes mellitus, and/or insulin resistance.Reference Cairns, McCarvill, Ruzickova and Calkin58, Reference Fagiolini, Chengappa, Soreca and Chang59 Although there is a well-documented influence of iatrogenic and lifestyle factors on metabolic dysfunction in BD, they do not account for all the differences observed.Reference Mansur and Brietzke60 For example, individuals with BD exhibit severe metabolic abnormalities even in the absence of pharmacotherapy.Reference Allison, Newcomer and Dunn61, Reference Birkenaes, Opjordsmoen and Brunborg62 It is believed that metabolic dysfunction is a core component of disease pathophysiology and contributes significantly to mortality in individuals with BD, including increased rates of death due to cardiovascular disease when compared with the general population.Reference Fagiolini, Chengappa, Soreca and Chang59 Understanding the etiology of metabolic abnormalities will allow for the prevention of further disease progression, limiting mortality in these individuals.
Taking these data together, it is not unexpected that replicated evidence indicates that energy metabolism plays a critical role in both normal and abnormal brain function.Reference Mansur and Brietzke60 The human brain constitutes 2% of the body mass yet consumes 25% of the energy substrates,Reference Mergenthaler, Lindauer, Dienel and Meisel63 suggesting that changes in energy regulation significantly affect neural function. In addition, evidence indicates that brain energy metabolism plays an important role in human behavior, through the control of both energy intake and expenditure.Reference Roh, Song and Kim64 Certain neural networks including dopamine transmission in cortico-striatal pathways are considered to be a potential mechanism explaining this finding as well as indicators of energy status, such as glucose and insulin. In fact, studies have linked disrupted insulin signaling in the brain with reduced dopamine transmission and disordered mood symptoms.Reference Kleinridders, Cai and Cappellucci65
Research has repeatedly demonstrated that individuals with mood disorders exhibit abnormal brain energy metabolism.Reference Mansur and Brietzke60, Reference Mansur, Lee, McIntyre and Brietzke66, Reference Frey, Stanley, Nicoletti, Hatch and Soares67 For example, markers of dysfunctional energy regulation have been identified in individuals with mood disorders including increased lactate and lower pH,Reference Dogan, Yuksel, Du, Chouinard and Ongur68 as well as oscillating energy generation in which body temperature is higher in mania and lower in depression.Reference Pflug, Johnsson and Ekse69 In addition, reduced cerebral glucose metabolic rates during depressive episodes have been identified in both major depressive disorder and BD.Reference Mah, Zarate and Singh70
As a result of dysfunctional energy metabolism in mood disorders, evidence indicates that molecular and cellular pathways mediating energy expenditure are downregulated.Reference Hino, Sakamoto and Nagaoka71 Behaviorally, this has been expressed as reduced physical activity during depressive episodes, revealed through accelerometry studies.Reference Wielopolski, Reich and Clepce72 In addition, individuals with mood disorders exhibit a reduced willingness to expend physical effort for rewards when compared with healthy controls, indicating motivational changes and reward system dysfunction.Reference Satterthwaite, Kable and Vandekar73 Recent work has associated this finding with altered peripheral insulin signaling in individuals with depression, although more work is needed to identify a mechanistic link.Reference Stouffer, Woods and Patel74, Reference Kleinridders and Pothos75 According to the “selfish brain” theory, glucose utilization is prioritized for use by the brain through the inhibition of insulin secretion from the pancreas. This mechanism enhances the uptake of glucose to the central nervous system which is an insulin-independent process.Reference Mansur and Brietzke60 Therefore, reduced physical activity in individuals with altered brain energy regulation may signify another compensatory mechanism acting to conserve energy in states of homeostatic imbalance such as those observed in mood disorders.
Insulin is a key hormone involved in the regulation of brain energy metabolism, mediating food intake, energy expenditure, adipose tissue accumulation, and peripheral metabolism.Reference Frayn76-Reference Kullmann, Kleinridders and Small78 Brain insulin signaling has also been implicated in the mesolimbic dopamine system and influences brain activity related to reward behavior.Reference Martin, Bullich, Guiard and Fioramonti79 Therefore, the actions of insulin demonstrate high relevance to the study of mood disorder etiology.Reference Rawlinson and Andrews80, Reference McIntyre81 In fact, brain insulin resistance has already been described as a potential mechanism for abnormalities in mood.Reference Ghasemi, Dargahi, Haeri, Moosavi, Mohamed and Ahmadiani82 Despite this evidence, to our knowledge, no study has yet to evaluate the relationship between brain insulin signaling and energy expenditure in individuals with BD.
BD as an illness of metabolic let lag
Historically, circadian rhythms of energy regulation have allowed our human ancestors to allocate metabolic resources according to the occurrence of activities across the day and night cycle. The influence of metabolic jet lag is becoming increasingly relevant to humans as we continue to adopt social and personal habits that stray from the daylight cycle and protrude into the resting period. Misalignment between internal physiology and behavior is detrimental to many aspects of human health. The high prevalence and impact of metabolic dysfunction in individuals with BD support the view that metabolic jet lag may be a key aspect of the pathophysiology and disease progression.Reference Cribbet, Logan and Edwards83
Metabolic abnormalities are significantly higher in BD compared to the general population and have been linked to unfavorable illness trajectories.Reference McIntyre, Danilewitz and Liauw15 Specifically, laboratory markers indicate elevated serum triglycerides and glycosylated hemoglobin, hyperinsulinemia, insulin resistance, and lowered HDL, compared with healthy controls.Reference Soska84 These increased blood markers of metabolic syndrome have been associated with decreased treatment efficacy and worsened disease course in BD.Reference Cuperfain, Kennedy and Goncalves85 Individuals with BD also demonstrate a greater prevalence of obesity when compared with the general population. Obese BD individuals are more likely to have major depressive episodes, accumulate medical conditions, and become treatment resistant.Reference Goldstein, Liu, Schaffer, Sala and Blanco86 Studies have revealed evidence of structural and neurobiological changes associated with obesity that may contribute to the progression of BD, although more work is needed to identify the exact underlying mechanisms responsible.Reference Kuswanto, Sum, Yang, Nowinski, McIntyre and Sim87
Abnormalities in insulin and glucose regulation are also routinely observed in individuals with BD, linked to worsened mood symptoms, and reduced therapeutic efficacy of lithium.Reference Cairns, McCarvill, Ruzickova and Calkin58, Reference Calkin, Ruzickova and Uher88 In fact, a diagnosis of type II diabetes mellitus is three times as common in individuals with BD compared to healthy individuals.Reference Cuperfain, Kennedy and Goncalves85 As a hormone that acts within brain regions such as the amygdala, hypothalamus, and hippocampus, altered insulin signaling may disrupt the healthy functioning of neural tissues. Specifically, it is thought that reduced insulin sensitivity may lead to neurodegeneration in the aforementioned regions.Reference Arnold, Arvanitakis and Macauley-Rambach89, Reference Brietzke, Kapczinski, Grassi-Oliveira, Grande, Vieta and McIntyre90 Cognitive impairment has also been linked to insulin resistance in individuals with BD, further supporting this point.Reference Cuperfain, Kennedy and Goncalves85
A less-studied circadian somatic change in BD is related to appetite, which can widely differ in hypomanic, manic, and depressive episodes, similar to sleep–wake cycle abnormalities. Recent work has identified circadian desynchronized eating behavior as a prominent subgroup of BD, associated with more severe metabolic comorbidities and mood symptoms.Reference Koning, Vorstman, McIntyre and Brietzke91 Under physiological conditions, most of us exhibit a rhythmic pattern in eating behaviors. However, patients with BD frequently describe oscillations or abnormalities in their appetite and eating habits, but most of these abnormalities have not been sufficiently explored.Reference Buyukkurt, Bourguignon and Antinora92 Few studies have investigated eating rhythms in individuals with mental disorders, other than anorexia and bulimia, and very few of them were conducted in populations with BD.Reference Haynes, Gengler and Kelly93 The regular timing of meals is an important external cue for the circadian system; therefore, appetite changes may promote adverse effects along with circadian misalignment, as depicted in Figure 1.
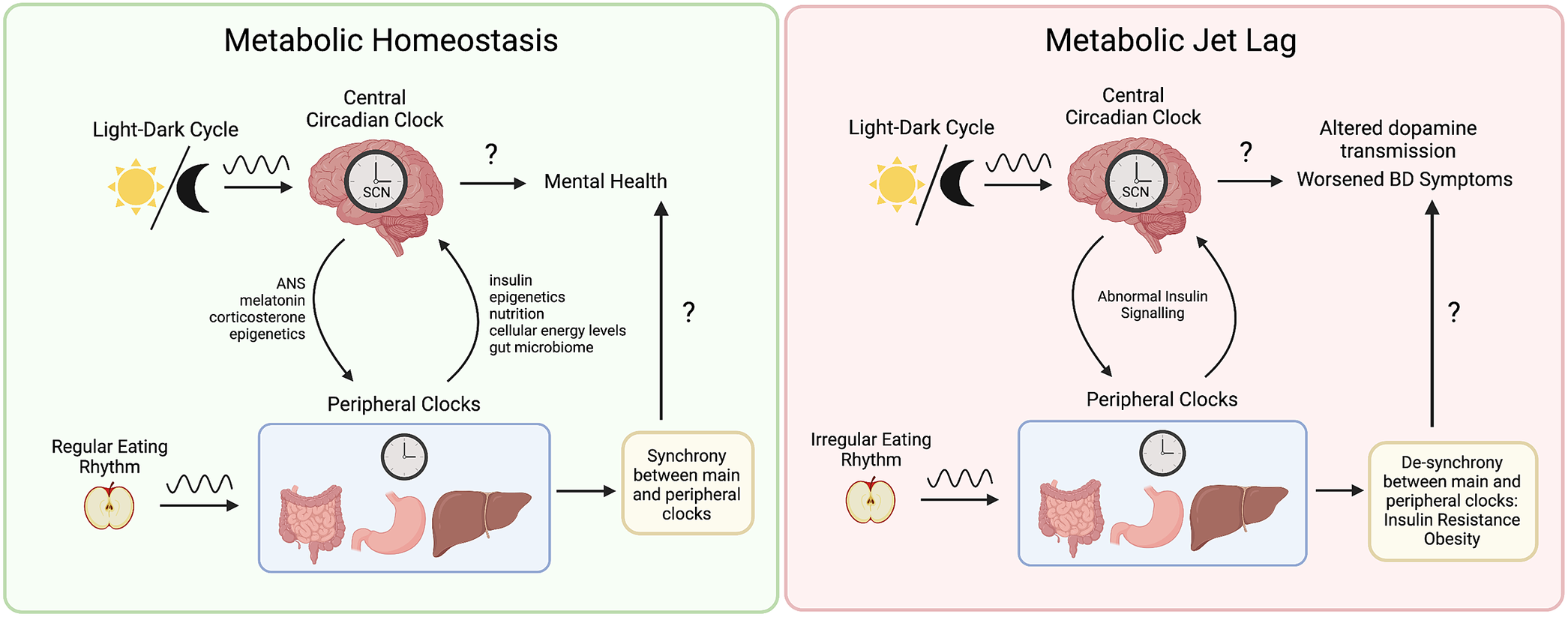
Figure 1. Metabolic jet lag as a core component of bipolar disorder (BD) pathophysiology. Synchrony between central and peripheral clocks is maintained by external cues such as the light–dark cycle and regular patterns of eating. The central circadian clock influences peripheral tissues through the autonomic nervous system, neurohormones such as melatonin and corticosterone, as well as epigenetic mechanisms such as control of metabolic enzyme gene expression. Conversely, metabolic function also influences the central circadian clock through insulin signaling, control of clock gene expression, mitochondrial function, energy expenditure, nutritional content, cellular energy levels, and via the gut–brain axis. Eating rhythms that are irregular and do not align with the light–dark cycle contribute to a variety of metabolic dysfunctions including insulin resistance and obesity. As a result, abnormal insulin signaling has been related to neurobiological changes including altered dopamine transmission. Ultimately, metabolic jet lag contributes to a worsened clinical course in BD including reduced quality of life and treatment efficacy, more frequent mood episodes, and shortened life span. The exact mechanisms underlying metabolic jet lag and worsened symptoms of BD remain unknown.
Preliminary investigations using simple questionnaires suggest that eating rhythm dysfunction is present in BD during acute episodes and euthymia. This has been associated with symptom severity and poor quality of life.Reference Allega, Leng and Vaccarino94, Reference Giglio, Magalhaes, Kapczinski, Walz and Kapczinski95 Giglio et al.Reference Giglio, Magalhaes, Kapczinski, Walz and Kapczinski95 showed that, although sleep disturbance is prevalent in BD, the disruption of eating rhythms is more strongly associated with executive functioning than with sleep rhythms in the interepisodic period.Reference Buyukkurt, Bourguignon and Antinora92 Additionally, Allega et al.Reference Allega, Leng and Vaccarino94 used a self-report questionnaire to assess this biological disturbance during euthymia in BD, demonstrating that rhythms related to sleep, eating, and social activity are independent predictors of functioning and quality of life.Reference Koning, Vorstman, McIntyre and Brietzke91 Additionally, Mondin et al.Reference Mondin, Cardoso and Souza96 showed that disrupted eating patterns are linked to obesity, diabetes, and cardiovascular disease and provided evidence that biological rhythm disruption may be a trait marker for mood disorders. More recently, a relationship between irregular eating patterns and mood instability has been proposed by Buyukkurt et al.Reference Buyukkurt, Bourguignon and Antinora92 in which the temporal order of eating correlated with hypomanic symptoms. Overall, the alignment of internal and external cues is important to assess in individuals with BD and the role of eating rhythms and metabolic jet lag needs to be further understood.
Implications for research and clinical care
Considerations of metabolic jet lag and its role in the pathophysiology of BD are an important avenue for further research. Clinically, incorporating the assessment of eating rhythms is an important step for individuals with BD, especially considering common comorbidities which impact eating behavior, such as sleep–wake disorders, substance use disorders, and eating disorders.Reference DeSocio97-Reference Serrano-Serrano, Marquez-Arrico, Navarro, Martinez-Nicolas and Adan99
Improvements in the clinical assessment of eating rhythms
Currently available studies use very simple assessments in the evaluation of eating rhythms, including food diaries, 24-hour recalls, and food frequency questionnaires.Reference Pendergast, Ridgers, Worsley and McNaughton100 Food diaries are often tedious, posing a high burden to both the participant and researcher as well as challenging long-term compliance. Additionally, 24-hour recalls are often confounded by aspects of episodic memory and data interpretation with recall bias causing a significant threat to the accuracy of results. Finally, food frequency questionnaires are unable to fully assess eating patterns due to a lack of contextual information. Technological advances such as data entry apps and food tracking websites have reduced some of the burden associated with manual food tracking, although participant engagement is still required.
The use of ecological momentary assessment
The aforementioned methods contrast with the development of more sophisticated tools used to evaluate eating and nutrition, especially considering the current availability of smartphone apps which can be used for both active and passive monitoring of lifestyle factors, as part of a digital phenotyping approach. For example, ecological momentary assessment (EMA) is an active monitoring method in which human behavior is measured in a participant’s natural environment, such as through a mobile phone. This method allows for real-time assessment of behaviors such as eating patterns over a certain period, possibly aiding in the early identification of abnormalities.Reference Moskowitz and Young101 EMA requires little effort on behalf of the participant and avoids the effects of recall bias that are associated with other self-reporting methods, making it more effective than the standard food diary.Reference Pentikainen, Tanner, Karhunen, Kolehmainen, Poutanen and Pennanen102
EMA has been used in a variety of contexts, such as to identify the effects of fasting in eating disorders and the underlying cognitive aspects that may explain eating disorder behavior, as described by Levinson et al.Reference Levinson, Sala, Fewell, Brosof, Fournier and Lenze103. Additionally, McHill et al. used time-stamped pictures from a mobile phone app to record feeding, demonstrating that food intake during the resting phase contributes to weight gain independent of dietary content or energy expenditure.Reference McHill, Phillips and Czeisler36 EMA has also demonstrated feasibility in the study of autoimmune disorders,Reference Nap-van der Vlist, Houtveen and Dalmeijer104 mood disorders,Reference Wenze and Miller105 alcohol abuse,Reference Freisthler, Lipperman-Kreda, Bersamin and Gruenewald106 and other illnesses.Reference Mundi, Lorentz, Grothe, Kellogg and Collazo-Clavell107 However, to our knowledge, there is not yet a study implementing EMA in the assessment of metabolic jet lag in individuals with BD. In addition, the optimal length of time to record with EMA for a reliable view of individuals’ eating rhythms is yet to be determined and studies have collected data over a range of different time periods.
Digital phenotyping also encompasses methods to collect data in a passive manner, that is, not requiring active input from the user such as with EMA. These methods typically use an individual’s personal device, sometimes in conjunction with wearable sensors. This method of assessment utilizes data streams related to social activity, movement, and biological rhythms to identify human behavioral phenotypes.Reference Jagesar, Vorstman and Kas108 Digital phenotyping demonstrates significant potential for capturing intra-individual differences over time, as well as improving the early detection of mood disorders and predicting health outcomes following clinical intervention.Reference Brietzke, Hawken, Idzikowski, Pong, Kennedy and Soares109 Overall, more work is needed to determine the optimal technology for measuring biological rhythms such as eating, as well as implement their use in the clinical assessment of BD.
The integration of chronobiology in the study of mitochondrial dysfunction in BD
Although mitochondrial function and dysfunction have been previously investigated in BD,Reference Gimenez-Palomo, Dodd and Anmella110 to the best of our knowledge, no study has incorporated a chronobiological approach. It would be very helpful to understand if circadian lifestyle factors such as time of meals, exercise, and sleep are able to beneficially modulate mitochondrial function in BD and, in extension, if they can also be beneficial for general medical comorbidities.
Exploration of eating rhythms as a target for intervention
Additional research is required to identify more effective intervention strategies for the management of BD, especially for patients displaying circadian desynchronized eating. Further, the potential for adverse effects of pharmacotherapy on energy balance supports the need for adjunctive approaches for the prevention and management of metabolic comorbidities. Non-pharmaceutical interventions, especially those related to lifestyle choices, could support positive changes for those afflicted with this serious issue that impacts more people than is reported.Reference Sarris, O’Neil, Coulson, Schweitzer and Berk111 For example, interpersonal and social rhythm therapies have been shown to improve mood symptoms and prevent relapse in BD by helping patients establish routines to stabilize their circadian rhythms.Reference Bellivier, Geoffroy, Etain and Scott6, Reference Crowe, Beaglehole and Inder112, Reference Gold and Kinrys113
Time-restricted eating (TRE) refers to the restriction of the daytime feeding window to 12–20 hours and demonstrates benefit to multiple aspects of human physiology, including the potential to counteract metabolic jet lag.Reference Currenti, Godos and Castellano114 Although few studies of TRE have been conducted in humans, there is evidence that brain function and peripheral energy metabolism can be optimized with this method, including the promotion of ketone body synthesis. The role of ketone bodies in the brain has been linked to enhanced energy metabolism and ketosis is an increasingly attractive therapeutic target in BD.Reference Jensen, Wodschow, Nilsson and Rungby115-Reference Morris, Puri, Maes, Olive, Berk and Carvalho117 Further, TRE allows for regulation of fat metabolism through hormones implicated in mood, such as leptin, adiponectin, and ghrelin.Reference Zarouna, Wozniak and Papachristou118 TRE may be used to counteract certain metabolic abnormalities which have been linked to worsened mood disorder symptoms and the limited eating window allows a means to overcome circadian desynchronized eating.
Recently, Guerrero-Vargas et al.Reference Guerrero-Vargas, Zarate-Mozo, Guzman-Ruiz, Cardenas-Rivera and Escobar119 demonstrated successful prevention of depressive- and anxiety-like behaviors in animal models of shift work upon adoption of a TRE window. Although there have been limited observational studies in humans, there is evidence that short-term calorie restriction similar to TRE may induce antidepressant effects in individuals with depression through a variety of molecular pathways.Reference Zhang, Liu, Zhao, Zhang, Li and Cui120 Additionally, a recent cross-sectional study concluded that individuals over the age of 70 that have a feeding window of 8 hours are less likely to show signs of mental health distress, compared to those with no restriction on their feeding time.Reference Currenti, Godos and Castellano114 Overall, more research is needed to delineate the role of TRE in the management of mood disorders, but current evidence is promising.
Conclusion
Disruptions in circadian rhythm adversely affect metabolic processes, and this is relevant to those with BD. Sleep–wake and feeding-fasting cycles are both affected by circadian rhythm disruption and are altered as features of BD, but it remains unclear whether the disruption is a result of physiological differences in those with BD, or if it is a contributing factor to the related disturbances. This review has explored important findings related to BD and the prevalence of metabolic dysfunction in this patient population, suggesting that altered energy regulation is a key contributing factor to disease pathophysiology.
Individuals with BD routinely exhibit signs of metabolic jet lag, and more work is needed to determine the link between biological rhythms such as meal timing and disease progression. Furthermore, it may be possible to limit unfavorable disease progression with interventions such as TRE, which improve the synchronization between energy metabolism and the circadian clock. As an emerging field in medicine, chrononutritional approaches to psychiatry show potential for improving BD symptoms, especially considering the unpredictable nature of pharmacological interventions and associated treatment resistance. As a 24-hour society, further research is needed to delineate the role of rhythm disruption in psychiatric illness. The incorporation of biological rhythm assessment in routine clinical care will allow the significant influence of lifestyle factors such as metabolic jet lag to be taken into consideration, a step toward improved treatment and patient outcomes.
Acknowledgments
This work was supported by the 2021 Department of Psychiatry Internal Faculty Grant and a Dean’s Doctoral Award, Queen’s University. Dr. Michael Berk was supported by a NHMRC Senior Principal Research Fellowship (1156072).
Author Contributions
Conceptualization: E.B.; Formal analysis: E.K.; Funding acquisition: E.B.; Investigation: E.K., A.M., A.B., F.A.G. J.V., M.B., R.B.M., E.B.; Methodology: F.A.G., J.V.; Project administration: E.K., E.B.; Supervision: E.B.; Writing—original draft: E.K., A.M., A.B., F.A.G., J.V., M.B., J.F., R.S.M., R.B.M., E.B.; Writing—review & editing: E.K., A.M., A.B., F.A.G., J.V., M.B., J.F., R.S.M., R.M., R.B.M., E.B.
Disclosures
Dr. Roger S. McIntyre has received research grant support from CIHR/GACD/National Natural Science Research Foundation of China (NSFC) and the Milken Institute; speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Boehringer Ingelheim, Sage, Biogen, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axosome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Viatris, Atai Life Sciences and Abbvie. Dr. Roger S. McIntyre is a CEO of Braxia Scientific Corp. Dr. Fabiano A. Gomes reports personal fees as a speaker/consultant from Abbott, Allergen, Aspen, Libbs, and Lundbeck, as well as grants from the BBRF Foundation (NARSAD Young Investigator Award/P&S Fund Investigator) and the Canadian Menopausal Society/Pfizer Research Award, outside the submitted work. Dr. Elisa Brietzke reports personal fees as a speaker/consultant from Janssen and Daiichi-Sankyo, as well as grants from the Queen’s University Faculty of Health Science and SEAMO, outside the present work.




