1. Introduction
The majority of patients with schizophrenic psychoses experience a prodromal phase with first signs and symptoms, beginning on average 3–4 years before the onset of frank psychosis [Reference Riecher-Rössler, Gschwandtner, Borgwardt, Aston, Pflüger and Rössler1, Reference Häfner, Riecher-Rössler, Maurer, Fätkenheuer and Löffler2]. Based on this evidence, the concept of the clinical high risk (CHR) state for psychosis was developed approximately two decades ago, including specified criteria such as the presence of attenuated psychotic symptoms, short limited psychotic symptoms or genetic risk and functional decline [Reference Yung, Phillips, McGorry, McFarlane, Francey and Harrigan3].
A large body of research has since been conducted to establish and optimize early detection of the early stages of the disorder and to predict transition to frank psychosis. Current meta-analytical evidence indicates that about 20% of CHR patients develop frank psychosis [Reference Fusar-Poli, Cappucciati, Borgwardt, Woods, Addington and Nelson4] and about 35% remit from their CHR state [Reference Simon, Borgwardt, Riecher-Rössler, Velthorst, de Haan and Fusar-Poli5] within two years after initial identification. The speed of psychosis progression tends to plateau from the third year on, reaching a cumulative transition risk of about 35% after 10 years [Reference Kempton, Bonoldi, Valmaggia, McGuire and Fusar-Poli6]. Therefore, most previous studies have focused on the first 2–3 years after initial identification [Reference Riecher-Rössler and McGorry7–Reference Schultze-Lutter, Michel, Schmidt, Schimmelmann, Maric and Salokangas9] and there is only little evidence on the long-term outcome of CHR patients [Reference Michel, Ruhrmann, Schimmelmann, Klosterkötter and Schultze-Lutter10–Reference Beck, Andreou, Studerus, Heitz, Ittig and Leanza15].
Although CHR patients without later transition (CHR-NT patients) make up the majority of CHR samples [Reference Fusar-Poli, Cappucciati, Borgwardt, Woods, Addington and Nelson4, Reference Schultze-Lutter, Michel, Schmidt, Schimmelmann, Maric and Salokangas9], little is known about their clinical and functional long-term outcome. So far, there are only very few studies evaluating non-psychotic clinical and functional outcome of CHR-NT patients with follow-up durations of more than 2 years [Reference Michel, Ruhrmann, Schimmelmann, Klosterkötter and Schultze-Lutter10–Reference Amminger, Schäfer, Schlögelhofer, Klier and McGorry12, Reference Beck, Andreou, Studerus, Heitz, Ittig and Leanza15]. These studies indicate that even CHR patients without transition to frank psychosis experience (subclinical) psychotic symptoms, non-psychotic disorders and psychosocial impairments in the long-term [Reference Michel, Ruhrmann, Schimmelmann, Klosterkötter and Schultze-Lutter10–Reference Amminger, Schäfer, Schlögelhofer, Klier and McGorry12, Reference Beck, Andreou, Studerus, Heitz, Ittig and Leanza15], although most of the comorbid disorders seem to be already present at baseline [Reference Fusar-Poli, Rutigliano, Stahl, Davies, De Micheli and Ramella-Cravaro16, Reference Webb, Addington, Perkins, Bearden, Cadenhead and Cannon17].
However, the existing long-term studies on CHR-NT patients have several methodological limitations. Functional outcome was frequently assessed by the GAF in which the level of functioning is rated based on psychosocial functioning or clinical symptoms, whichever area is more impaired, leading to a conflation of both. Most studies reported rates of remission from the CHR state only for certain points in time. Furthermore, a risk estimate that takes into account the “competing” risk of transition and the usually considerable proportion of drop-outs was rarely provided.
Little is known about how many CHR patients transition to frank psychosis and how many remit from their clinical high risk state in the long term. Furthermore, limited information is available on the clinical and functional outcome of those who do not transition, e.g., regarding subclinical psychotic symptoms, non-psychotic clinical symptoms and diagnoses such as depression and anxiety, psychosocial functioning and overall recovery. Insight into the long-term outcome of CHR-NT patients could inform clinical service planning and future research on the CHR state.
In this study, we therefore thoroughly investigated the ultra-long-term course (up to 16 years) of CHR patients, evaluating transitions to psychosis over the whole follow-up period including late transitions. Furthermore, we assessed the clinical and functional outcome of those without transition, i.e., the rates of remission from the CHR state, clinical symptoms and axis I diagnoses, functional outcome, and the prevalence of full clinical and functional recovery. Moreover, we aimed to investigate predictors of clinical and functional outcome in CHR-NT patients at long-term follow-up as to the best of our knowledge this has not previously been investigated. Based on a systematic review [Reference Beck, Andreou, Studerus, Heitz, Ittig and Leanza15], we expected that most CHR-NT patients do not recover functionally and clinically during several years of follow-up.
2. Methods
2.1 Participants and procedure
Patients with a clinical high risk (CHR) for psychosis were recruited via the prospective Früherkennung von Psychosen (FePsy) study [Reference Riecher-Rössler, Pflueger, Aston, Borgwardt, Brewer and Gschwandtner18, Reference Riecher-Rössler, Gschwandtner, Aston, Borgwardt, Drewe and Fuhr19] and the Bruderholz study (BHS) [Reference Simon, Gradel, Cattapan-Ludewig, Gruber, Ballinari and Roth20]. Both were prospective clinical studies of all consecutive referrals from defined catchment areas to the specialized early detection centers of the counties of Basel city (FePsy) and Basel countryside (BHS). Patients received treatment according to needs, case-management, and supportive psychotherapy during the follow-up. Antipsychotic treatment was only initiated after transition to psychosis had occurred. Further details regarding the characteristics of the studies can be found in Table 1 and in previous publications [Reference Riecher-Rössler, Pflueger, Aston, Borgwardt, Brewer and Gschwandtner18–Reference Simon, Gradel, Cattapan-Ludewig, Gruber, Ballinari and Roth20]. Both studies were approved by the Ethics Committee northwest/central Switzerland (EKNZ) and all participants provided written informed consent. If subjects were under age 18, additional written informed consent was obtained from their parents.
Table 1 Characteristics of the FePsy and Bruderholz studies.
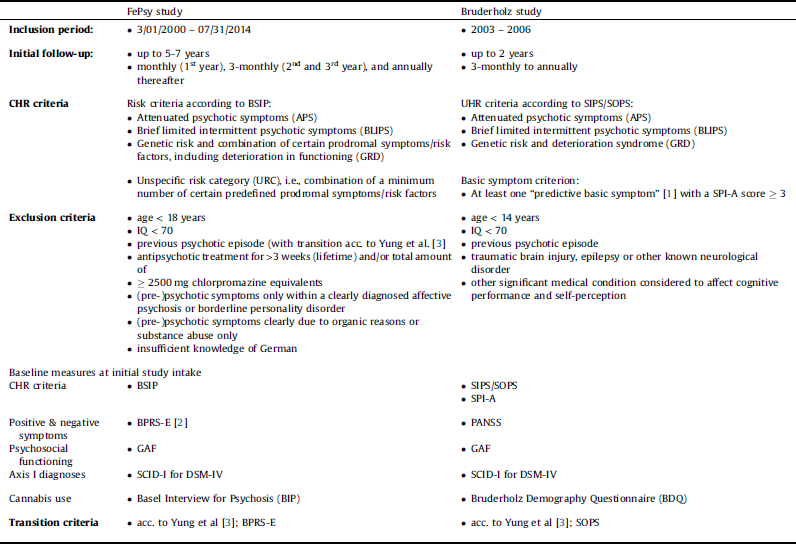
Note: FePsy study = Früherkennung von Psychosen (Basel early detection of psychosis) study; Bruderholz study = Basel countryside early detection of psychosis study; CHR = Clinical high risk for psychosis; SIPS = Structured Interview for Prodromal Symptoms / SOPS = Scale of Prodromal Symptoms (McGlashan et al, 2001([Reference McGlashan, Miller, Woods, Hoffman, Davidson, Miller, Mednick, McGlashan, Libiger and Johannessen24])); BSIP = Basel Screening Instrument for Psychosis (Riecher-Rössler et al [Reference Riecher-Rössler, Aston, Ventura, Merlo, Borgwardt and Gschwandtner42]; Peralta et al (Reference Peralta, Studerus, Andreou, Beck, Ittig and Leanza43)); SIPS = Structured Interview for Prodromal Symptoms; SOPS = Scale of Prodromal Symptoms; SPI-A = Schizophrenia Proneness Instrument, Adult version (Schultze-Lutter et al (Reference Schultze-Lutter, Ruhrmann, Picker, von Reventlow, Brockhaus-Dumke and Klosterkotter44)); PANSS = Positive and Negative Syndrome Scale (Kay, Fiszbein, & Opler (Reference Kay, Fiszbein and Opler45)); BPRS-E = Brief Psychiatric Rating Scale – Expanded (Ventura et al (Reference Ventura, Lukoff, Nuechterlein, Liberman, Green and Shaner23)); GAF = Global Assessment of Functioning scale of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; American Psychiatric Association (Reference American Psychiatric Association28)); SCID-I = Structured Clinical Interview for DSM-IV Axis I Disorders (First & Gibbon [Reference First and Gibbon30]; Wittchen, Gruschwitz & Zaudig (Reference Wittchen, Wunderlich, Gruschwitz, SKID and Strukturiertes Klinisches31)); BIP (Riecher-Rössler et al (Reference Riecher-Rössler, Ackermann, Uttinger, Ittig, Koranyi and Rapp46)).
a According to Klosterkötter et al [Reference Klosterkötter, Hellmich, Steinmeyer and Schultze-Lutter47]: thought interference, thought perseveration, thought pressure, thought blockages, disturbances of receptive language, decreased ability to discriminate between ideas and perception, fantasy and true memory, unstable ideas of reference, derealization, visual and acoustic perception disturbances.
b Positive and negative symptom subscales according to Shafer et al ([Reference Shafer, Dazzi and Ventura21]).
All CHR patients who did not transition to frank psychosis during the respective initial follow-up periods, including patients who dropped out and did not complete all planned follow-up assessments, were regarded as patients without initial transition (CHR-NT), and were asked to take part in the long-term follow-up assessment of the current study (see Supplementary Materials page 1 for detailed information on the very thorough contact procedure).
Patients who refused to participate in the extensive long-term follow-up examination were asked to participate in a shorter telephone interview instead.
2.2 Measures
2.2.1 Baseline assessment
Baseline parameters and measures are reported in Table 1.
2.2.2 Follow-up assessments
CHR status was re-evaluated at each follow-up visit using the positive symptom items of the Brief Psychiatric Rating Scale – Expanded (BPRS-E) [Reference Lukoff, Nuechterlein and Ventura22, Reference Ventura, Lukoff, Nuechterlein, Liberman, Green and Shaner23] in the FePsy study and the Structured Interview for Prodromal Symptoms/Scale of Prodromal Symptoms (SIPS/SOPS) [Reference McGlashan, Miller, Woods, Hoffman, Davidson, Miller, Mednick, McGlashan, Libiger and Johannessen24, Reference Miller, McGlashan, Woods, Stein, Driesen and Corcoran25] in the Bruderholz study.
Remission from CHR. Remission from CHR was defined as the absence of attenuated psychotic symptoms (APS) or brief limited intermittent psychotic symptoms (BLIPS), i.e., sub-threshold severity scores on all positive symptom items of the BPRS-E (FePsy) or SOPS (BHS) for at least 12 consecutive months preceding the latest follow-up assessment. Thus, in the FePsy study, the four BPRS-E symptoms relevant for this assessment had to be constantly under the following thresholds: suspiciousness ≤ 2, hallucinations ≤ 1, unusual thought content ≤ 2, and formal thought disorder ≤ 2. In the Bruderholz study, the five positive psychotic symptom items of the SOPS had to be constantly ≤ 2. Both sets of criteria are similar to those used by Schlosser et al. [Reference Schlosser, Jacobson, Chen, Sugar, Niendam and Li26]. The date of remission was defined as the date at which the APS/BLIPS-free period lasting at least 12 months started. In those CHR-NT patients who participated in the long-term follow-up assessment, the date of remission was determined retrospectively for the whole follow-up period including the initial follow-up period. In those patients who did not take part in the long-term assessment, remission was evaluated by using all BPRS-E/SOPS positive symptom ratings of the initial follow-up period.
Transition to psychosis according to the criteria by Yung and colleagues [Reference Yung, Phillips, McGorry, McFarlane, Francey and Harrigan3] was also evaluated not only at each follow-up assessment but also retrospectively for the entire follow-up period by considering all available information, including medical records.
Non-remission from CHR. In case neither remission from CHR nor transition to psychosis occurred, patients were considered non-remitted at the time point they were last seen. This was the date of the long-term follow-up visit for patients participating in the long-term follow-up, whereas for patients not participating in the long-term follow-up this was the last visit in the initial follow-up.
Psychosocial functioning in CHR-NT patients at long-term follow-up, referring to the preceding 4 weeks, was evaluated by the Personal and Social Performance scale (PSP) [Reference Morosini, Magliano, Brambilla, Ugolini and Pioli27] which is based on the Social and Occupational Functioning Scale (SOFAS) [Reference American Psychiatric Association28] and has been validated in many languages, including German [Reference Juckel, Schaub, Fuchs, Naumann, Uhl and Witthaus29]. Functioning is assessed in four domains, i.e., occupational functioning, interpersonal relationships, self-care, and presence of disturbing/aggressive behavior. Overall functioning is expressed in a global score. For the current study a global score of ≤ 70 was defined as functional impairment since scores above 70 indicate no or mild dysfunction [Reference Morosini, Magliano, Brambilla, Ugolini and Pioli27].
The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) [Reference First and Gibbon30, Reference Wittchen, Wunderlich, Gruschwitz, SKID and Strukturiertes Klinisches31] was used to assess current axis I diagnoses in CHR-NT patients at long-term follow-up.
Full clinical and functional recovery at long-term follow-up was defined as meeting all of the following criteria: no transition to frank psychosis, remission from CHR, good functional outcome (PSP global score > 70), and the absence of any current axis I disorder in accordance with Rutigliano et al. [Reference Rutigliano, Valmaggia, Landi, Frascarelli, Cappucciati and Sear32].
2.3 Statistical analyses
Statistical analyses were conducted using the R environment for statistical computing [Reference R Core Team and Computing RFfS33]. Analyses were conducted in two different samples: 1) the initial baseline sample of all CHR patients and 2) the sample of CHR patients who participated in the long-term follow-up assessment of the current study and had not transitioned to frank psychosis during the whole follow-up period. To test the representativity of the second sample, we compared those who participated in the long-term follow-up assessment with those who did not regarding various socio-demographic and clinical characteristics – both at baseline and at their last visit of the initial follow-up period.
In the first sample we investigated of CHR remission and transition rates over the whole follow-up period using cumulative incidence curves (CIC) which are the competing risks analogs of Kaplan-Meier survival curves [Reference Kleinbaum and Klein34]. We used proportional cause-specific hazards models to investigate baseline predictors for remission from CHR and transition to psychosis, i.e., age and gender, positive symptoms, negative symptoms, psychosocial functioning, and current cannabis use.
In the second sample we conducted 1) logistic and 2) multiple regression analyses to examine the predictive value of the aforementioned baseline socio-demographic and clinical variables regarding 1) remission from CHR and 2) psychosocial functioning at the long-term follow-up assessment. For each predictor variable, a separate model was fitted that additionally included study (FePsy vs. BHS) as covariate.
3. Results
3.1 Initial baseline sample (all CHR patients)
The initial baseline sample consisted of 255 CHR patients. The average follow-up duration (mean ± SD; range) of the whole initial sample was 3.9 ± 4.1 (range: 0–16.6), of those with later transition 2 ± 2.5 (0.01–11.21), and of those without transition 8.2 ± 4.4 (0.1–16.6) years, respectively.
3.2 Ultra-long-term follow-up sample of CHR-NT patients
Forty-seven CHR patients of the initial baseline sample had been detected to have had transitioned to frank psychosis during initial follow-up. Thus, 208 CHR patients without initially detected transition (CHR-NT) were contacted and invited to participate in the ultra-long-term follow-up assessment. Of these, 72 (34.6%) did participate (71 face-to-face interviews, 1 telephone interview), 28 (13.5%) refused to take part, and 108 (51.9%) could not be reached. For two further patients only medical records were available, including information on transition status. Twelve patients participating in the long-term follow-up assessment turned out to have had transitioned in the meantime. Therefore, the long-term sample of CHR-NT patients consisted of 60 participants. Further details on the study sample can be found in Fig. 1 and Table 2.
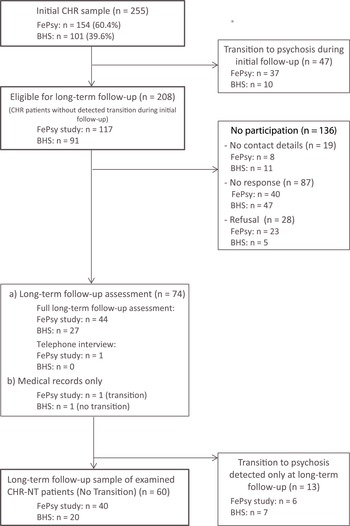
Fig. 1. Flow diagram of the study population.
Table 2 Socio-demographic and clinical characteristics of the CHR-NT patients of the long-term follow-up sample (n = 60) at baseline and long-term follow-up.
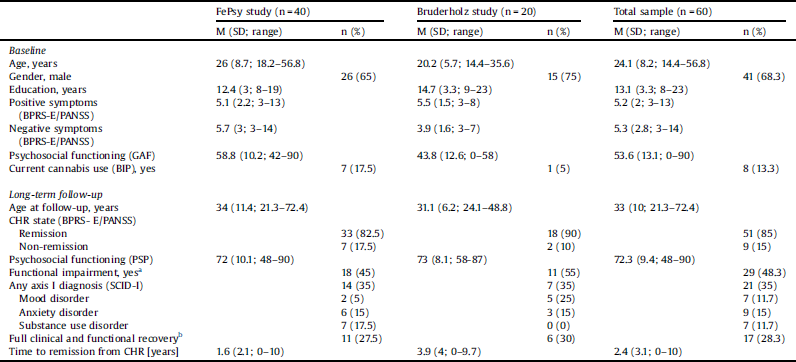
Note: CHR = Clinical high risk for psychosis; GAF = Global Assessment of Functioning scale of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; American Psychiatric Association, [Reference American Psychiatric Association28]); BPRS-E = Brief Psychiatric Rating Scale – Expanded (Ventura et al. [Reference Ventura, Lukoff, Nuechterlein, Liberman, Green and Shaner23]); PANSS = Positive and Negative Syndrome Scale (Kay, Fiszbein, & Opler, [Reference Kay, Fiszbein and Opler45]); PSP = Personal and Social Performance Scale; GAF = Global Assessment of Functioning scale of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; American Psychiatric Association [Reference American Psychiatric Association28],); SCID-I = Structured Clinical Interview for DSM-IV Axis I Disorders (First & Gibbon, [Reference First and Gibbon30]; Wittchen, Gruschwitz & Zaudig, [Reference Wittchen, Wunderlich, Gruschwitz, SKID and Strukturiertes Klinisches31]); BIP (Riecher-Rössler et al [Reference Riecher-Rössler, Ackermann, Uttinger, Ittig, Koranyi and Rapp46]).
a Personal and Social Performance Scale (PSP) total score ≤ 70.
b Remission from CHR and absence of functional impairment and no axis I disorder.
There were no significant group differences between CHR patients who participated in the long-term follow-up assessment (n = 72) and those who did not (n = 183) regarding various sociodemographic and clinical variables (all p-values > 0.05; data available upon request), indicating a high representativity of the long-term follow-up sample.
3.3 Clinical outcome of the total initial CHR sample (n = 255)
3.3.1 Rates of transition to psychosis
Overall, 60 patients had transitioned to frank psychosis. At 2-, 3-, 4-, and 5-year follow-up the estimated transition rates were 18.7%, 23.1%, 25.9%, and 30.8%, respectively. Ten and 15 years after baseline the rates were 34.9% and 38.2%, respectively (for the proportions of transitions for each year see Fig. 2 and Table S2).
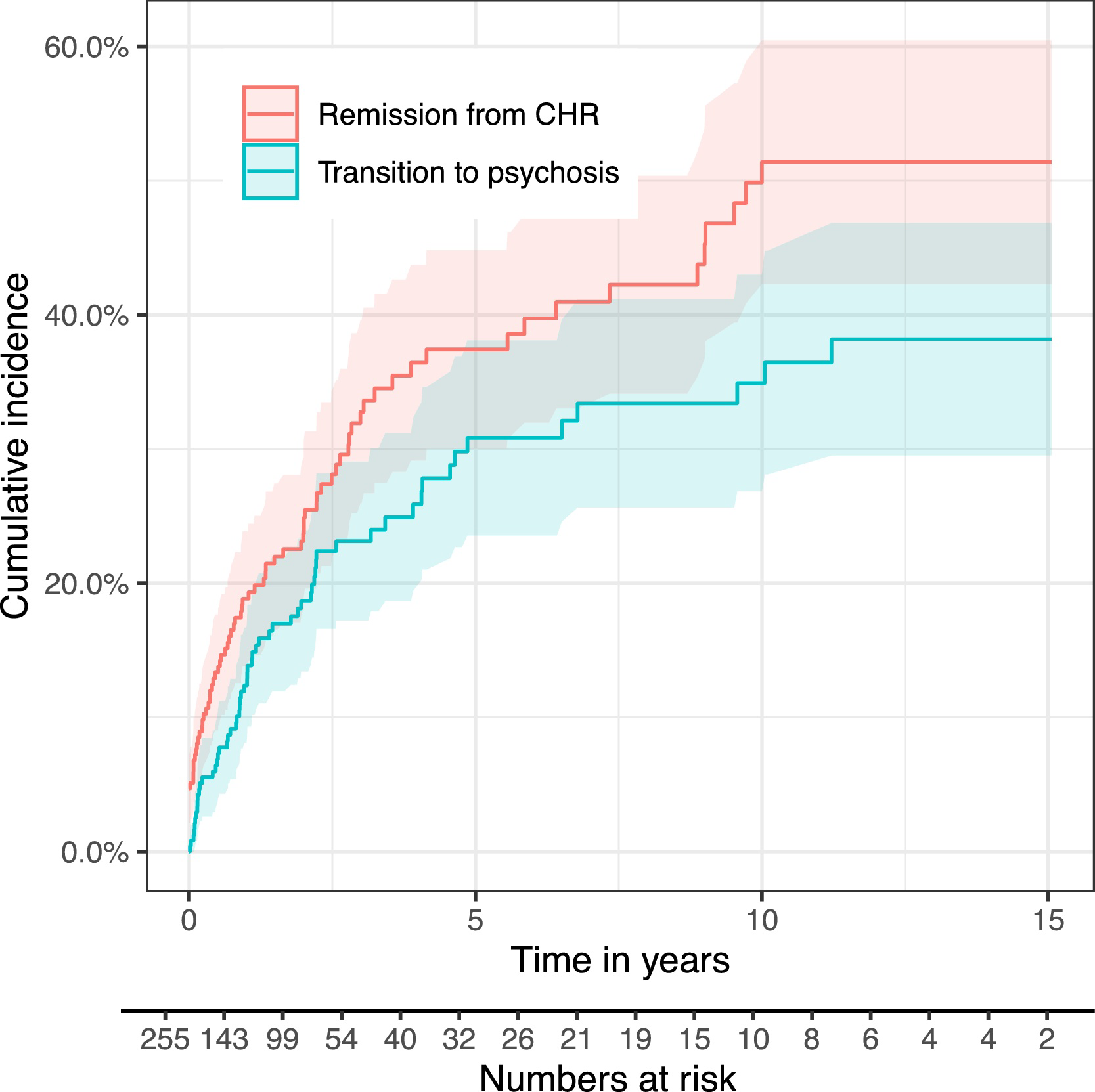
Fig. 2. Cumulative incidence curves.
Note: Estimated risks of remission from CHR and transition to frank psychosis over the whole follow-up period. Numbers at risk indicate CHR patients who are still in follow-up at this time point and neither remitted from their CHR nor transitioned.
3.3.2 Rates of remission from CHR
The proportion of patients with a remission from CHR within the first 2, 3, 4, and 5 years of follow-up was estimated with the cumulative incidence curve as 23.7%, 32.8%, 36.4%, and 37.4%, respectively. Ten years after initial baseline an estimated proportion of 51.4% had remitted, with no further remissions after that time point (for the rates of remissions at each year after initial baseline, see Fig. 2 and Table S2).
3.3.3 Baseline predictors of remission from CHR
In the overall CHR sample, better psychosocial functioning at baseline was associated with a higher likelihood of remission from CHR during follow-up (p = 0.003). Age, sex, positive and negative symptoms as well as cannabis use were not significantly associated with remission (see Table 3).
Table 3 Baseline predictors of remission from CHR in the whole sample (n = 255).
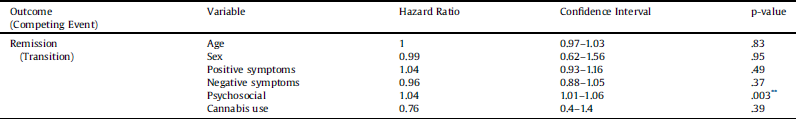
* p ≤.05.
** p ≤.01.
3.4 Clinical and functional outcome of the CHR-NT long-term follow-up sample (n = 60)
The mean follow-up duration of the CHR-NT long-term follow-up sample was 8.2 ± 4.4 (range: 0.1–16.6) years. The average follow-up duration was 7.1 ± 4.3 (1.2–16.6) years of those with later remission from the CHR state and 2.5 ± 3.2 (0–15.1) years of those who neither remitted nor transitioned, respectively.
Of the 60 CHR-NT patients of the long-term follow-up sample, 51 (85%) had remitted from their high risk status (CHR), 39 (65%) had not any axis I diagnosis, 31 (51.7%) showed good psychosocial functioning. All in all, only 17 (28.3%) had fully recovered clinically and functionally. For further characteristics of the long-term follow-up sample see Table 2 and Fig. 3.
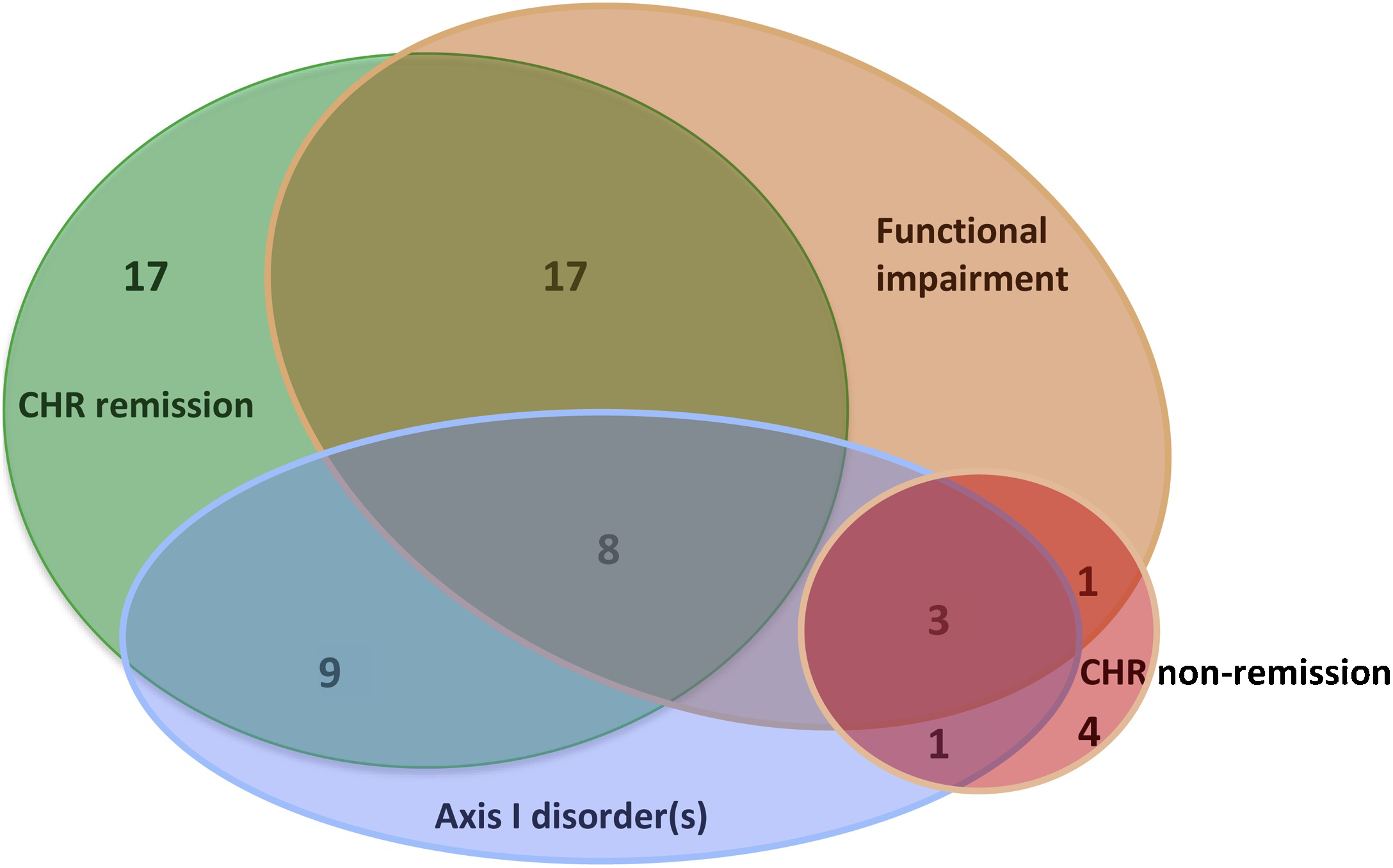
Fig. 3. Clinical and functional outcome of CHR patients without transition to frank psychosis at ultra-long-term follow-up (n = 60).
3.4.1 Baseline predictors of remission from CHR and psychosocial functioning at long-term follow-up (n = 60)
There were no significant associations between any of the baseline variables and remission from CHR at long-term follow-up (all p-values > 0.05; see Table S3). However, higher age (p = 0.06) and less negative symptoms (p = 0.09) at baseline were associated with better psychosocial functioning at long-term follow-up at a trend level (see Table S4).
4. Discussion
We evaluated rates of transition and remission from the clinical high risk state and their predictors in a large sample of CHR patients over a follow-up period of up to 16 years. At the latest follow-up time, an estimated 38% of the overall sample of 255 patients had transitioned to frank psychosis, 51% had remitted from their CHR state, and 11% continued to experience subclinical psychotic symptoms. A higher level of psychosocial functioning at baseline was associated with a higher likelihood of remission from the CHR state during the follow-up.
Of the 60 CHR patients who participated in our direct, personal long-term follow-up assessments (i.e., at an average of 8 years after baseline) and had not transitioned to psychosis, 85% had remitted from their CHR state, 35% presented with at least one axis I diagnosis (apart from the CHR state), 48% showed poor functional outcome, and overall, only 28% had fully recovered clinically and functionally. This suggests that the majority of CHR-NT patients continue to experience clinical symptoms or functional impairments, even many years after initial identification. In this sample of CHR-NT patients, higher age and less negative symptoms at baseline were associated, at a trend level of significance, with better functional outcome at long-term follow-up.
4.1 Transition to psychosis
The present study estimated rates of transition for up to 16 years after initial referral, which – to our knowledge - is the longest time period that has ever been reported. Overall, we estimated that 26% of CHR patients had developed frank psychosis after 3 years, 31% after 5 years, 35% after 10 years, and 38% after 16 years. Our estimated transition rates in the first 4 years of the follow-up are very similar to those reported in the most recent meta-analyses [Reference Fusar-Poli, Cappucciati, Borgwardt, Woods, Addington and Nelson4, Reference Schultze-Lutter, Michel, Schmidt, Schimmelmann, Maric and Salokangas9]. As expected [Reference Fusar-Poli, Cappucciati, Borgwardt, Woods, Addington and Nelson4], most transitions occurred during the first 2–3 years of follow-up. However, several of our CHR patients had experienced a “late transition” 4 or more years after initial identification.
So far, only very few studies have estimated cumulative transitions rates for periods longer than 4 years [Reference Nelson, Yuen, Wood, Lin, Spiliotacopoulos and Bruxner35, Reference Fusar-Poli, Nelson, Valmaggia, Yung and McGuire36]. In line with our results, the study by Nelson et al [Reference Nelson, Yuen, Wood, Lin, Spiliotacopoulos and Bruxner35] on 416 CHR patients revealed cumulative transition rates of 28% and 35% after 4 and 10 years, respectively. In contrast, the study by Fusar-Poli et al [Reference Fusar-Poli, Nelson, Valmaggia, Yung and McGuire36] on 509 CHR patients detected only few transitions after more than 4 years. However, they might have missed some late transitions as their follow-up was limited to 10 years and they had a relatively high rate of drop-outs.
The multiple late transitions revealed in our study and that of Nelson et al [Reference Nelson, Yuen, Wood, Lin, Spiliotacopoulos and Bruxner35] support the importance of follow-up durations longer than three years. This is not only important to estimate the true rates of transitions but also to evaluate the outcome of CHR patients without transition to psychosis. The fact that there is quite a number of late transitions also challenges many studies on risk prediction, as most prediction models were developed based on samples with short follow-up durations and can therefore only make accurate predictions regarding the short term.
4.2 Remission from CHR
In the whole sample of CHR patients, including those who transitioned, we estimated that 24% of CHR patients had remitted from their CHR state after 2 years, 32% after 3 years, 36% after 5 years, and 50% after 10 and 16 years, indicating that a considerable number of CHR patients experience subclinical psychotic symptoms even many years after initial identification. The only other study that has estimated cumulative remission rates using competing risk survival analysis estimated 36% remissions after two years [Reference Schlosser, Jacobson, Chen, Sugar, Niendam and Li26]. Our results are also similar to those of the meta-analysis of Simon et al. [Reference Simon, Borgwardt, Riecher-Rössler, Velthorst, de Haan and Fusar-Poli5], which found a remission rate of 35% after two years.
Of the CHR patients without transition that participated in our direct long-term follow-up assessments 85% had remitted from their CHR state. This is about 10% higher than in other studies [Reference Simon, Borgwardt, Riecher-Rössler, Velthorst, de Haan and Fusar-Poli5, Reference Michel, Ruhrmann, Schimmelmann, Klosterkötter and Schultze-Lutter10, Reference Lin, Wood, Nelson, Beavan, McGorry and Yung11, Reference Beck, Andreou, Studerus, Heitz, Ittig and Leanza37] which might be explained by the shorter average follow-up durations of most of these studies compared to the on average 8 years of follow-up in our sample.
Persistence of attenuated psychotic symptoms might indicate an ongoing risk of transition to psychosis [Reference Nelson, Amminger and McGorry38]. Recurrent symptoms might also point towards a moderate disposition to react to stress with subclinical psychotic symptomatology, but not full psychosis due to, e.g., comparably low vulnerability and/or good protective factors. Subclinical psychotic symptoms might also indicate other diagnoses such as affective disorder, posttraumatic stress disorder and borderline personality disorder.
4.3 Baseline predictors for remission from CHR
In the whole sample of CHR patients we found better psychosocial functioning at baseline to be associated with a higher remission rate. Not predictive were age, sex, positive symptoms, negative symptoms, or cannabis use. A similar study of Schlosser et al [Reference Schlosser, Jacobson, Chen, Sugar, Niendam and Li26] found not only baseline psychosocial functioning but also lower levels of negative symptoms to increase the likelihood of remission. This discrepancy might be due to the large difference in the follow-duration (up to 2 vs. 16 years) and different measures of negative symptoms (i.e., SOPS vs. BPRS/PANSS).
Poor psychosocial functioning is closely associated with (emerging) psychosis and might be a more stable marker for vulnerability to psychosis, i.e., non-remission from CHR, than positive symptoms at baseline [Reference Riecher-Rössler and McGorry39]. A subgroup of CHR patients might not be predisposed to psychosis but might suffer from non-psychotic disorders associated with decreased psychosocial functioning and subclinical psychotic symptoms. CHR patients with better psychosocial functioning at baseline might have a higher resilience, including more internal and external resources such as a good social network and support, and a stable school or work environment. Those protective factors might contribute to their remission from CHR.
If only the CHR-NT patients that participated in our direct long-term follow-up assessments were considered, no significant associations between baseline predictors and remission from CHR were found. This is in line with a study of Ziermans et al [Reference Ziermans, Schothorst, Sprong and van Engeland40]. However thismight also be due to a lack of statistical power as only few patients had not remitted from their CHR state (n = 9).
4.4 Clinical and functional ultra-long-term outcome of CHR-NT patients
The relatively high proportion of CHR patients without transition to psychosis diagnosed with clinical axis I diagnoses and/or showing poor psychosocial functioning at long-term follow-up is consistent with our recent review [Reference Beck, Andreou, Studerus, Heitz, Ittig and Leanza15]. It suggests that most patients still require clinical attention and should be further examined. Despite the relatively large proportions of CHR-NT patients presenting with non-psychotic disorders at long-term follow-up, recent studies have shown that the clinical high risk state for psychosis is not predictive for non-psychotic diagnoses [Reference Webb, Addington, Perkins, Bearden, Cadenhead and Cannon17, Reference Woods, Powers, Taylor, Davidson, Johannesen and Addington41]. The large number of comorbidities in CHR-P patients could at least partially be due to clinicians using other diagnosis as a substitute for a CHR diagnosis as the latter is not yet included in the DSM or ICD.
4.5 Limitations
We included patients from two different studies with slightly different study designs. While the FePsy study evaluated CHR patients aged 18 years or older, the Bruderholz study also included adolescents who made up almost half of its sample. Furthermore, the FePsy study used the BSIP for assessing CHR criteria, whereas the Bruderholz study used the SIPS. In addition, the initial follow-up duration was longer in the FePsy study (5–7 years) than in the Bruderholz study (2 years). Moreover, positive and negative symptoms were assessed with the BPRS-E in the FePsy study and the PANSS in the Bruderholz study. The small number of non-remitted patients in the CHR-NT sample possibly limits the statistical power of the analyses of predictors of remission from CHR. Nevertheless, our study is one of the first to extensively evaluate outcome of CHR patients over such a long follow-up duration, using an advanced methodological approach to estimate remission and transition rates for a large sample.
4.6 Conclusions
By investigating a relatively large sample of CHR patients over a very long follow-up duration of up to 16 years, we could demonstrate that several patients still transition to psychosis after the usual time period assessed in most previous studies. We also found that only a minority of CHR-NT patients had fully functionally and clinically recovered at long-term follow-up. So far, we have obviously underestimated the rate of late transitions as well as the long-term prevalence of clinical symptoms and functional impairments in CHR patients without transition. One implication of our study is that existing prediction models, which are mostly based on samples with short follow-up duration, can predict transition to psychosis only at short-term. Our study reinforces the need for longer follow-ups of patients at clinical high risk for psychosis to provide adequate clinical care and inform future research.
Funding
This work was supported by the Swiss National Science Foundation [grant number 32003B_159554].
Declaration of Competing Interest
None.
Acknowledgements
We thank all patients who participated in the study and shared their experience with us. Without them this research project would not have been possible. Furthermore, we thank the specialists who initially referred the patients.
Appendix A Supplementary data
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.eurpsy.2019.08.005.









Comments
No Comments have been published for this article.