Stunting remains a significant public health problem in low- and middle-income countries, affecting 156 million children under the age of 5 years. Meanwhile, there has been a significant rise in children who are overweight or obese, affecting 42 million children(1,2) . WHO has recognised that this phenomenon has the double burden of malnutrition, not only affecting mortality but also significantly affecting cognitive functioning, reducing physical activity, increasing poor delivery outcomes for those who were stunted during early childhood and increasing the risk of cardiovascular diseases, diabetes and cancer in adults who are overweight during childhood(1,Reference Martorell3,4) . As a result, addressing the double burden of malnutrition has been imperative to Sustainable Development Goals and WHO(4).
Indonesia has made progressive strides in improving rates of malnutrition over the past 5 years(5). However, over 37 % of children under 5 years are still stunted despite advancements in the economy and implementation of social programmes(6). On the other hand, the prevalence of being overweight in children under age 5 years has fluctuated, increasing from 5·6 to 8·5 % in 2000–2007 and then decreasing to 7·5 % in 2014. Meanwhile, the prevalence of being overweight in adults has increased to 33 %(Reference Odoo, Maehara and Rah7). Therefore, identifying other factors associated with diet and malnutrition has been imperative to malnutrition research and solutions.(6)
Efforts to address malnutrition in Indonesia have already included extensive education with the involvement of future mothers on healthy feeding practices and implementation of a national strategic plan incorporating behaviour change communication strategies, which may translate and encourage proper nutrition for their children(5,8) . On the other hand, the efficacy of these policies and/or how they are being implemented has been investigated to a limited extent. For example, the Integrated Health Service Post known as ‘Posyandu’ has provided basic training for village health workers on nutrition counselling to women who do not readily seek prenatal care services. However, research has shown that a lack of professional training and uneven distribution has prevented women in rural areas from receiving proper counselling(Reference Thomas and Yusran9).
Lack of dietary diversity has been associated with child stunting according to a systematic review using data from eleven Demographic and Health Survey (DHS) surveys from low- and middle-income countries(Reference Armond and Ruel10). The Indonesia DHS 2017 survey reported that approximately 40 % of boys and girls aged 6–23 months do not meet the criteria for minimum dietary diversity (MDD, defined as the consumption of four or more food groups out of seven food groups)(11). Of the seven food groups (grain, legumes, dairy, flesh foods, eggs, vitamin A-rich fruits and vegetables, and other fruits and vegetables) included in determining dietary diversity, food made from grains and vitamin A-rich fruits and vegetables was among the most commonly consumed food groups in this age group(11).
More specifically, there were few studies that investigated the association of maternal obstetrical care with dietary diversity in children in Indonesia. One study has shown that children aged 6–23 months who were delivered by traditional birth attendants and in the home had lower prevalence of MDD, compared with those born at a health facility with trained health staff(Reference Ng, Dibley and Agho12). Minimum acceptable diet, a combination of MDD and minimum meal frequency, has also been associated with low number of prenatal visits and delay in postnatal check-up in the same study(Reference Ng, Dibley and Agho12). Other factors such as mode of delivery (vaginal v. C-section) and postnatal check-up provider were not investigated. The association of these factors with individual food group consumption has also not yet been described in the literature, even though animal-source protein or micronutrient-rich foods are particularly important to the growth of young children(Reference Murphy and Allen13).
Pregnancy has been considered a teachable moment by many studies, where women have shown capacity and motivation for health behaviour change and have closer contact with health providers, specifically for maternal weight control and prevention of obesity(Reference Olander, Darwin and Atkinson14,Reference Phelan15) . Several studies have assessed the effect of maternal nutritional education on linear and ponderal growth in children, showing significant benefit alone and when combined with complementary food provision(Reference Imdad, Yakoob and Bhutta16). Determining at which points during obstetrical care that child’s dietary diversity and consumption of food groups are affected may help assess where and when certain food groups are emphasised, identify points of care to target additional maternal nutritional education and overall help to improve future nutrition policies and programmes.
Our study seeks to investigate the association of obstetrical care factors with dietary diversity score, MDD and consumption of individual food groups by secondary data analysis of the Indonesia DHS 2017 to fill existing knowledge gaps and improve future maternal and child nutrition interventions.
Methods
Study population
A total of 5113 children aged 6–23 months were analysed using data from the Indonesia DHS 2017. The detailed sampling structure and other survey specific methods of the Indonesia DHS 2017 are described elsewhere(11). Briefly, the sampling scheme was done using two-stage stratified sampling, the first using census blocks (primary sampling unit) that were ordered by wealth index and the second by selecting twenty-five households among those census blocks using systematic sampling. A total of 1970 census blocks in twenty-four provinces were represented in the sample for a total of 25 400 and 23 950 households in urban and rural areas, respectively. A total of 49 627 women were interviewed. Data used for the current study were from the Children’s Recode (KR) data set, which includes a record for each child born in the previous 5 years to each woman interviewed. This data set includes information regarding immunization, vitamin A supplementation and recent illness or childhood diseases, with the unit of analysis being children of women born in the last 5 years (0–59 months)(11).
Independent variables
The following characteristics were selected as potential predictor variables for the outcomes of interest: number of antenatal care visits (≥4 or 0–3), location of delivery (home v. health facility), mode of delivery (vaginal v. C-section), delivery provider (professionally trained v. non-professionally trained), timing of postnatal visit (2 d after delivery v. >2 d after delivery) and postnatal visit provider (physician, nurse/midwife and other). Professionally trained delivery providers included physicians, nurses and midwives. Non-professionally trained providers included traditional birth attendants and all others, including none at all. Independent variables were chosen through literature review of similar prior studies in Tanzania and five South Asian countries (including Bangladesh, India, Nepal, Sri Lanka and Pakistan) that have investigated these independent variables separately(Reference Ogbo, Ogeleka and Awosemo17,Reference Senarath, Godakandage and Jayawickrama18) . A prior study using data from Indonesia DHS 2007 also investigated the association of delivery attendant, place of delivery and use of antenatal care as separate predicting indicators for minimum acceptable diet and dietary diversity(Reference Ng, Dibley and Agho12). In the current study, correlations between these predictor variables were all <0·6 (see online supplementary material, Supplemental Table S5).
Antenatal visits were set as a dichotomous variable of whether children met the minimum recommended number of antenatal care visits (≥4 antenatal visits) v. those who did not (≤3 antenatal visits) set by WHO standards(19). The timing of postnatal visit was generated as a dichotomous variable of <2 d after delivery v. no postnatal check or postnatal check more than 2 d after delivery based on WHO guidelines(20). A total of 4915 children aged 6–23 months had data on the postnatal provider(11).
Dependent variables
Dietary diversity score and MDD were the main outcomes of interest. Dietary diversity score was calculated using the seven food groups: (i) grains, (ii) lentils and nut, (iii) flesh, (iv) egg, (v) dairy, (vi) vitamin A-rich fruits and vegetables and (vii) other fruits and vegetables. MDD was defined, according to the WHO Infant and Young Child Feeding Practices, as consuming four or more out of seven food groups within the past 24 h within children aged 6–23 months(21). Data on food group consumed were collected from children born in the last 2–3 years preceding the survey and whom were living with their mother. Diet was measured based on food and liquid consumption on ‘the day or night preceding the survey’.(11)
Covariate variables
The covariate variables included residence (rural v. urban), wealth quintile, maternal education (primary, secondary or higher), maternal occupation (agriculture, non-agriculture or not working) and maternal age (25–34, 14–24 and 35–49 years of age) based on a previous study(Reference Ng, Dibley and Agho12). Wealth index was constructed based on a number of characteristics including household goods owned, water source, toilet facility and flooring, which are used to create score via a principal component analysis(11). These variables were later used for adjustment in our analysis.
Statistical analysis
A total of 5113 children aged 6–23 months who had MDD information were included in the data analysis, whereas only 3340 children aged 6–23 months were included in the data analysis as the number of children who had data on the timing of postnatal visit. All independent and dependent variables were presented as weighted percentages as dichotomous or categorical variables. The consumption of seven food groups was presented as a bar graph.
Within each of our predictor variables for children 6–23 months of age, unadjusted (univariate) linear regression was conducted to examine the associations between independent variables and child’s dietary diversity score. Unadjusted logistic regression was done for the associations between independent variables, MDD and consumption of each food group for children 6–23 months of age. Next, the linear or logistic regression of the same outcome variables for each predictor variable was adjusted with maternal age, maternal occupation and household wealth quintile. Independent variables that showed a significance (P < 0·05) in the adjusted regression analysis were considered determinants for the outcome of interest. Lastly, we explored a linear and logistic regression of our independent variables on dietary diversity score and MDD, stratifying by urban v. rural residence. Adjusted associations between the consumption of seven food groups and dependent variables were presented via forest plots. All analysis considered the sampling design and sampling weight of the original survey. Statistical analysis was performed using Stata version 15. Forest plots were generated using Prism 8.4.
Ethics of human subject participation: The current study was deemed to be exempt from IRB review, as the current study involved secondary data analyses using publicly available data from the DHS.
Results
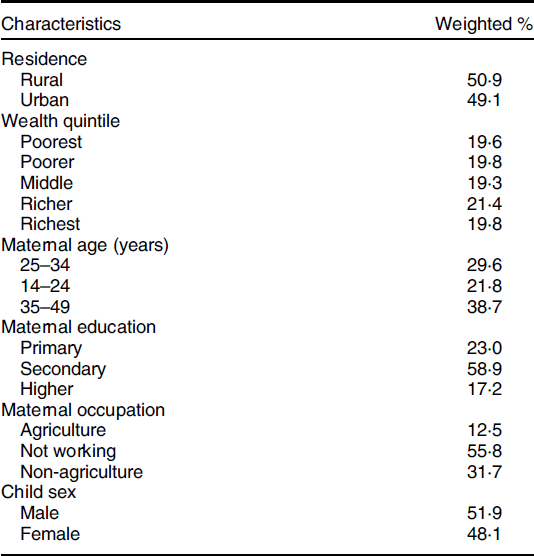
Half of the children aged 6–23 months in the survey were males (51·9 %) and lived in rural areas (50·9 %). Most mothers were aged 35–49 years (38·7 %) and 25–34 years (29·6 %), and half of them received a secondary education (58·9 %) (Table 1).
Table 1. General characteristics of children 6–23 months of age at household, maternal and child level in Indonesia, DHS 2017 (n 5113)
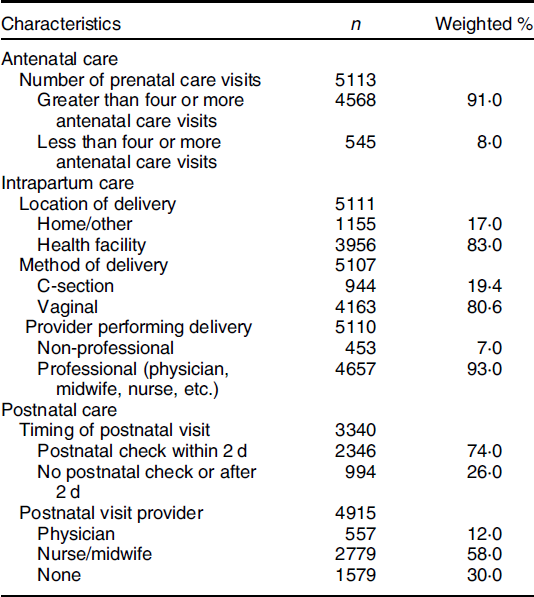
The majority of mothers had four or more antenatal care visits (91·0 %) and delivered at a health facility (83 %). Most mothers delivered their child via vaginal delivery (80·6 %) with the assistance of a professionally trained provider (93·0 %) such as a physician, nurse or midwife (Table 2). Only 3340 mothers had data on the timing of postnatal visit; out of them, most mothers received a postnatal check within 2 d after delivery (74·0 %) which was mostly conducted by a nurse/midwife (58·0 %).
Table 2 General characteristics of maternal care during pregnancy and delivery among mothers of children 6–23 months of age in Indonesia, DHS 2017
The mean dietary diversity score was 3·87 (se 0·03) among children aged 6–23 months with 59·7 % of them achieving MDD. According to the 24-h recall, most children consumed grains (93·6 %) followed by vitamin A-rich fruits and vegetables (78·2 %). Largely, half of the children consumed animal-source nutrient-rich foods such as meat/fish/poultry (57·1 %), eggs (51·0 %) and dairy food (49·3 %). The consumption of legumes and other type of fruits and vegetables than vitamin A-rich ones was less common (30·6 and 26·9 %, respectively) (Fig. 1)
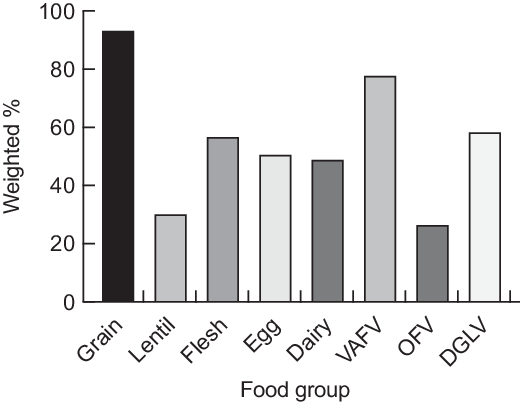
Fig. 1 Weighted percentage of food group consumption among mothers of children 6–23 months of age in Indonesia, DHS 2017 (n 5113). VAFV, vitamin A-rich fruits and vegetables; OFV, other fruits and vegetables
Antenatal and delivery-related determinants for minimum dietary diversity
Four or more antenatal care visits were associated with higher dietary diversity score among children (adjusted β 0·23, 95 % CI (0·06, 0·40)), compared with 0–3 visits, but not associated with achieving MDD (adjusted OR (AOR) 1·23, 95 % CI 0·95, 1·60) (Table 3). Also, four or more antenatal care visits showed higher odds of consuming lentils (AOR 1·66, 95 % CI 1·23, 2·25), eggs (AOR 1·28, 95 % CI 1·01, 1·63 and other fruits and vegetables (AOR 1·70, 95 % CI 1·23, 2·35) among children, compared with less than four visits (Fig. 2).
Table 3 Association between four or more prenatal visits, delivery at a health facility, mode of delivery and timing of postnatal visit with dietary diversity score and minimum dietary diversity among mothers of children 6–23 months of age in Indonesia, DHS 2017
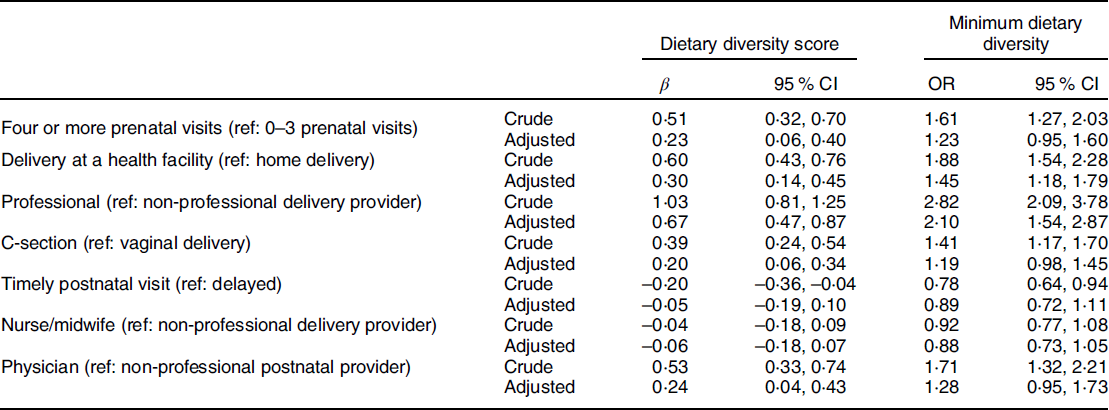
Adjustment was made for maternal wealth quintile, occupation and maternal age.
Table 4 Association between four or more prenatal visits, delivery at a health facility, mode of delivery and timing of postnatal visit with dietary diversity score and minimum dietary diversity in urban residences among mothers of children 6–23 months of age in Indonesia, DHS 2017

Adjustment was made for maternal wealth quintile, occupation and maternal age.
Table 5 Association between four or more prenatal visits, delivery at a health facility, mode of delivery and timing of postnatal visit with dietary diversity score and minimum dietary diversity in rural residences among mothers of children 6–23 months of age in Indonesia, DHS 2017
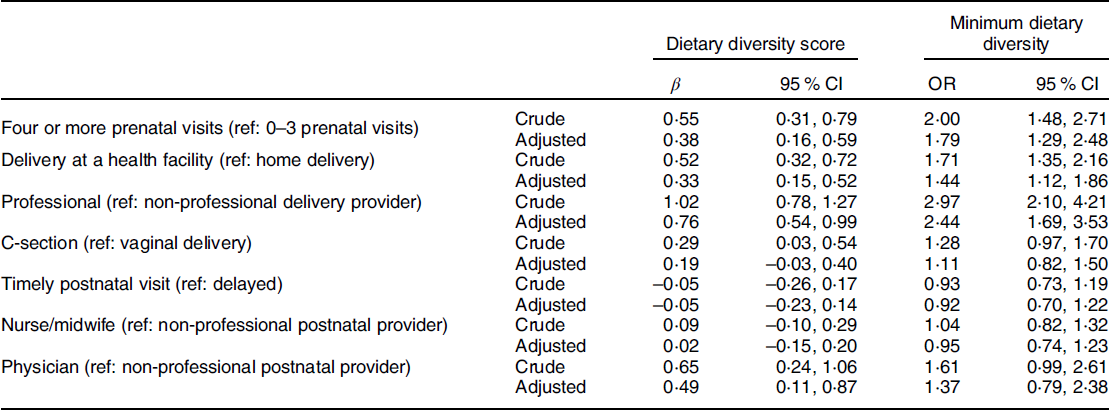
Adjustment was made for maternal wealth quintile, occupation and maternal age.
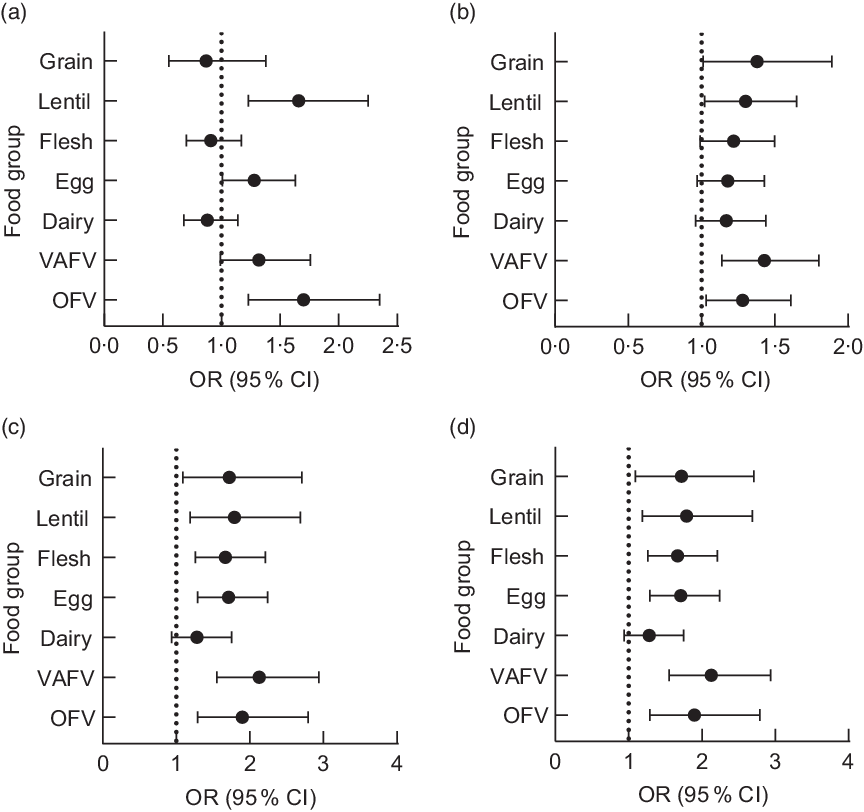
Fig. 2 Association between (a) four or more prenatal visits, (b) delivery at a health facility, (c) mode of delivery (vaginal v. C-section) and (d) professional v. non-professional delivery attendant with food group consumption among mothers of children 6–23 months of age in Indonesia, DHS 2017. VAFV, vitamin A-rich fruits and vegetables; OFV, other fruits and vegetables; MDD, minimum dietary diversity. Adjustment was made for maternal wealth quintile, occupation and maternal age
Delivery at health facility was associated with higher dietary diversity scores (adjusted β 0·30, 95 % CI (0·14, 0·45)) and 1·45 times higher odds of MDD (AOR 1·45, 95 % CI (1·18, 1·79) than children who were delivered in the home (Table 3). Children aged 6–23 months who were delivered at a health facility had 1·30 times higher odds of consuming lentils (AOR 1·30, 95 % CI 1·02, 1·65), 1·43 times higher odds for vitamin A-rich fruits and vegetables (AOR 1·43, 95 % CI 1·14, 1·80) and 1·23 times higher odds for other fruits and vegetables (AOR 1·23, 95 % CI 1·03, 1·61), as compared with children born at home (see Fig. 2 and online supplementary material, Supplemental Table S1).
Children, whose delivery was assisted by a professional medical provider such as a physician, nurse or midwife, had significantly higher dietary diversity scores (adjusted β 0·67, 95 % CI 0·47, 0·87) and 2·10 times higher odds of MDD (AOR 2·10, 95 % CI 1·54, 2·87) than children delivered by a non-professionally trained delivery provider (Table 3). Delivery by a trained professional had higher odds (AOR 1·72, 95 % CI 1·09, 2·71; AOR 1·79, 95 % CI 1·19, 2·69; AOR 1·67, 95 % CI 1·26, 2·21; AOR 1·71, 95 % CI 1·29, 2·24; AOR 2·13, 95 % CI 1·55, 2·94; AOR 1·90, 95 % CI 1·29, 2·79) of consumption of all food groups, except in dairy, compared with non-professional delivery attendants (see Fig. 2 and online supplementary material, Supplemental Table S2). Mothers who delivered by C-section had children with higher dietary diversity score compared with those delivered vaginally (adjusted β 0·20, 95 % CI 0·06, 0·34). Adjusted analysis showed no significant difference between C-section and vaginal delivery in MDD (see Fig. 2 and online supplementary material, Supplemental Table S3). Children who were delivered by C-section had significantly 1·39 times higher odds of diary consumption compared with those who delivered vaginally (AOR 1·39, 95 % CI 1·14, 1·70).
Receiving a postnatal visit 2 d after delivery was not associated with dietary diversity score, MDD and consumption of food groups among children (Table 3). Receiving a postnatal visit from a nurse/midwife or a physician was not associated with meeting MDD or consumption of grain, flesh or egg among children, compared with receiving a postnatal visit from a non-professional or not at all (see Fig. 3, Table 3 and see online supplementary material, Supplemental Table S4). Children who received a postnatal visit from a physician had a higher dietary diversity score than those who received a postnatal visit from a non-professional or not at all (adjusted β 0·24, 95 % CI 0·04, 0·43). Receiving a postnatal visit from a physician had 1·51 times higher odds of consumption of dairy food (AOR 1·51, 95 % CI 1·14, 1·99) and 1·49 times higher odds for vitamin A-rich fruits and vegetables (AOR 1·49, 95 % CI 1·06, 2·08) among children, compared with receiving their postnatal visit from a non-professional.
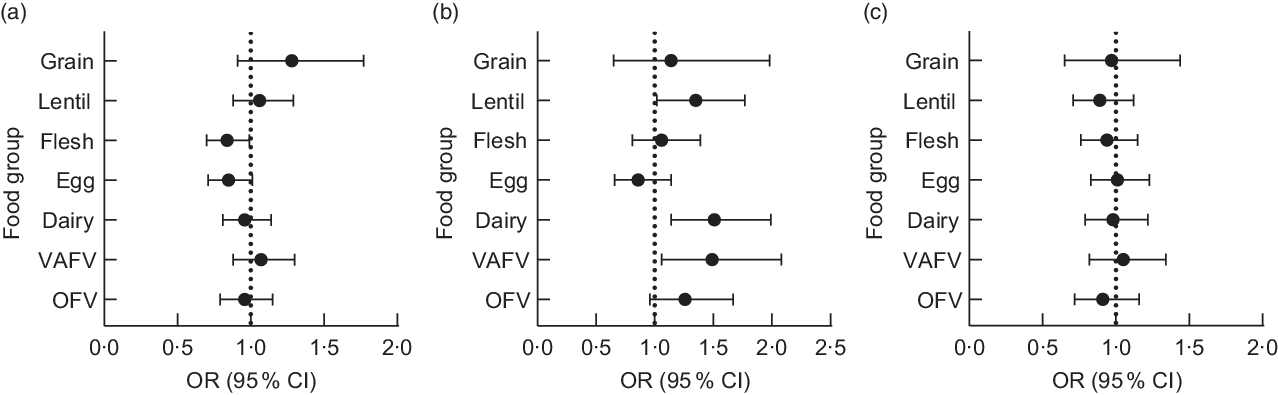
Fig. 3 Association between (a) nurse/midwife v. non-professional postnatal provider (b) physician v. non-professional postnatal provider, (c) timing of postnatal visit with food group consumption among mothers of children 6–23 months of age in Indonesia, DHS 2017. VAFV, vitamin A-rich fruits and vegetables; OFV, other fruits and vegetables; MDD, minimum dietary diversity. Adjustment was made for maternal wealth quintile, occupation and maternal age
Having a caesarean delivery was associated with a higher dietary diversity score in children living in urban areas (adjusted β 0·19, 95 % CI 0·01, 0·37). Four or more prenatal care visits, delivery at a health facility, having a professionally trained delivery attendant and a physician as a postnatal care provider were associated with higher dietary diversity score in children living in rural areas (adjusted β 0·38, 95 % CI 0·16, 0·59; adjusted β 0·19, 95 % CI 0·01, 0·37; adjusted β 0·19, 95 % CI 0·01, 0·37; adjusted β 0·19, 95 % CI 0·01, 0·37). Four or more prenatal care visits, delivery at a health facility, a professionally trained delivery attendant, caesarean delivery, postnatal visit within 2 d and a professionally trained (either nurse or physician) postnatal provider were associated with higher odds of MDD in children living in urban areas (AOR 0·61, 95 % CI 0·39, 0·94; AOR 1·34, 95 % CI 0·91, 1·98; AOR 1·16, 95 % CI 0·63, 2·14; AOR 0·89, 95 % CI 0·64, 1·25; AOR 0·78, 95 % CI 0·61, 1·02; AOR 1·16, 95 % CI 0·82, 1·65). Four or more prenatal care visits, delivery at a health facility, a professionally trained delivery attendant, caesarean delivery, postnatal visit within 2 d and a professionally trained (either nurse or physician) postnatal provider had significantly higher odds of MDD in children living in rural areas (AOR 1·79, 95 % CI 1·29, 2·48; AOR 1·44, 95 % CI 1·12, 1·86; AOR 2·44, 95 % CI 1·69, 3·53; AOR 1·11, 95 % CI 0·82, 1·50; AOR 0·92, 95 % CI 0·70, 1·22; AOR 0·95, 95 % CI 0·74, 1·23; AOR 1·37, 95 % CI 0·79, 2·38).
Discussion
We explored the association of obstetrical care factors with dietary diversity score and MDD among young children in Indonesia using data from DHS 2017. The results suggest that obstetrical care factors including four or more prenatal visits, delivery at a health facility, delivery by caesarean section and delivery by a professionally trained birth attendant are positive determinants of child’s dietary diversity score. The association between delivery by caesarean section and high dietary diversity might be due to earlier cessation of exclusive breast-feeding associated with caesarean delivery(Reference Hobbs, Mannion and McDonald22,Reference Chien and Tai23) . Delivery at a health facility and having a professionally trained delivery assistant were associated positively with meeting child’s MDD. Our stratified analysis by the place of residence did not significantly change the associations shown in the pooled sample. This is inconsistent with prior DHS analyses in Indonesia that have shown rural residence was associated with significantly lower dietary diversity(Reference Ng, Dibley and Agho12). This is may be because women who are still able to access care in rural areas may still be able to receive counselling on dietary diversity regardless of their residence status.
A prior secondary analysis using Indonesia DHS 2007 data showed that delivery at a health facility and having a professionally trained delivery attendant were associated with the higher prevalence of dietary diversity among children(Reference Ng, Dibley and Agho12). Other studies investigating determinants for MDD in Tanzania, Nepal and Sri Lanka have seen a positive association between delivering at a health facility and having a professionally trained delivery assistant with higher dietary diversity in children(Reference Chien and Tai23–Reference Nabahan, Hasan and Marthias26).
We did not see a significant association of minimum or above number of prenatal visits or caesarean delivery with child’s MDD. This is inconsistent with other studies, including a study based on an Indonesia DHS 2007 analysis, which showed that not attending prenatal care visits was associated with lower minimum acceptable diet(Reference Ng, Dibley and Agho12). Studies using DHS data from Sri Lanka and Nepal have also shown that delivery by C-section and attending prenatal care visits were positively associated with MDD(Reference Senarath, Godakandage and Jayawickrama18,Reference Joshi, Agho and Dibley25) . These studies categorised prenatal care visits using different criteria from our study, comparing MDD among women who did not seek prenatal care with those who had 1–3 visits and those who had greater than four visits, which may account for these contrasting findings. We chose to use a minimum of four or more prenatal visits, based on WHO recommendations at the time the DHS was conducted(19). According to a study on the use of maternal care services in Indonesia, rates of caesarean delivery have increased over the past several years for women who deliver at a health facility(Reference Nabahan, Hasan and Marthias26). Likewise, the use of prenatal care services has increased over the past several years, with a decreasing gap in access across socio-economic strata(Reference Nabahan, Hasan and Marthias26). It is plausible that along with the increase in prenatal services and caesarean deliveries, the quality of antenatal care has also increased to address challenges such as MDD.
It is notable that our study revealed that the timing of postnatal check and postnatal check provider was not associated with dietary diversity score or MDD. It is likely that prenatal visits are better, compared with postnatal care, at improving dietary quality of children. Studies in other low- and middle-income countries have shown mixed results when assessing the association of the timing of postnatal visits with child’s dietary quality. Studies in Tanzania, Sri Lanka and Nepal showed that delayed or less frequent postnatal visits were significantly associated with lower odds of MDD, yet one study in Malawi showed that attending postnatal visits was negatively associated with minimum acceptable diet likely due to the low quality of postnatal care(Reference Senarath, Godakandage and Jayawickrama18,Reference Victor, Baine and Agho24,Reference Joshi, Agho and Dibley25,Reference Walters, Rakotomanana and Komakech27) . When assessing the use of postnatal care services in Indonesia, one study found that 67 % of women in their cohort accessed postnatal care, with the majority attending in the first week of the newborns life(Reference Titaley, Dibley and Roberts28). Barriers to attending postnatal care services included living in rural areas, lower wealth quintiles and lower education(Reference Titaley, Dibley and Roberts28). Most women in our cohort accessed postnatal services within the first 2 d, and it is possible that dietary diversity is not being addressed during these visits.
Our study is the first to address the association of obstetrical care factors with individual food group consumption in Indonesia. Four or more antenatal visits, delivery at a health facility and having a professional delivery attendant were associated with higher odds of consumption of other fruits and vegetables than vitamin A-rich ones. Having a professional delivery attendant was associated with higher odds of consumption of grains, flesh and eggs. Studies in Indonesia have previously investigated the consumption of individual food groups across different economic strata showing that higher socio-economic status was significantly associated with the increased consumption of dairy products and other fruits and vegetables(Reference Santika, Februhartanty and Ariawan29). Our study adjusted for wealth quintile and maternal occupation, suggesting that obstetrical care may be an opportunity to address the gaps in the consumption of certain food groups. A study among some Indonesian communities investigating health education initiatives for infant feeding based on ethnographic studies described it is a common practice for mothers to feed infants bananas and rice with milk(Reference Wiryo30). More importantly, many of these mothers had been advised of these feeding practices by spiritual leaders and traditional birth attendants(Reference Wiryo30,Reference Tasnim, Mwanri and Dasvarma31) . It is possible that feeding infants rice and fruits is being given similar value in the hospital setting and/or mothers are seeking advice from multiple health providers in child nutrition. Another review of maternal feeding preferences and beliefs shared that fruits and vegetables were useful for ‘preventing vomiting and disease’ in Indonesia, which could also explain our observations(Reference Kavle and Landry32). Alternatively, these findings could represent the overall increasing trend in the consumption of meat over the years and the continued dominance of traditional Indonesian diet that is rich in grains and plants both in rural and urban areas(Reference Colozza and Avendano33). Future research should continue to look at obstetrical care and its impact on food group consumption in order to best inform future policies and programmes.
Strengths and limitations
First, our data were cross-sectional in nature; thus, the results do not demonstrate the causal relation between obstetrical care and child’s dietary diversity. Likewise, data were collected using the WHO standard method for the food groups that were consumed by children, which may or may not represent the typical diet of the child. However, the large and nationally representative sample size may mitigate the limitations encountered with a one-time dietary assessment. Second, our study did not control for maternal education in adjusted regression, as this characteristic has a strong correlation with wealth quintiles and our regression outputs including or excluding education were consistent. It is possible that mothers, who are receiving nutrition education and counselling during their obstetrical care by hospital facilities and staff, might be indirectly benefitting the child. Studies have shown that maternal education during pregnancy is crucial to promoting health behaviour change to address health issues such as obesity(Reference Phelan15). Third, it is possible that other components could have influenced the associations but not assessed at DHS survey. Obstetrical history or pregnancy-related complications, including baseline BMI of all members of the household, were not included in the DHS and may or may not influence child feeding practices. Although we adjusted for many socio-economic variables, there may also be other similar variables that were not measured in the DHS that could be associated with obstetrical care and dietary diversity. Finally, it is difficult to assess the practical applications for the changes in dietary diversity score according to each independent variable, and it is important to consider that our large sample size may have led to the observation of significant differences with such small changes.
Conclusion
Our study suggests that mothers who receive obstetrical care from a health facility, specifically prenatal care and intrapartum care, are associated with higher child’s dietary diversity. Our study suggests that obstetrical care may be a good opportunity for strengthening counselling of maternal and child feeding practices and addressing malnutrition challenges. Indonesia’s National Strategic Plan to address malnutrition has incorporated health behaviour change strategies within education regarding maternal healthy feeding practices(5,8) . Policymakers can consider not only enforcing nutritional education in mothers but also extending the national strategic plan for nutritional education to incorporate advice in child feeding while women seek obstetrical care. While Posyandu has provided nationwide village health worker training, there has been an unequal distribution of this training, particularly in rural areas where it was difficult for women to receive proper nutritional counselling(Reference Thomas and Yusran9). We suggest that nutritional educational policies be implemented with more contextualisation, specifically in communities where women seek care outside of a health facility. This can include training local health workers to provide these initiatives in their communities. Lastly, our study showed no association with postnatal visits and child’s dietary diversity. Further investigation into the quality of care of postnatal visits in Indonesia should be considered in addition to implementing stronger nutritional education initiatives during postnatal visits. Implementing these changes might address the existing gaps in addressing the double burden of malnutrition in Indonesia.
Acknowledgements
Acknowledgements: None. Financial support: The current study was made possible by the Johns Hopkins Institute for Clinical and Translational Research which is funded in part by grant no. TL1 TR003100 from the National Center for Advancing Translational Sciences, a component of the National Institutes of Health, and National Institutes of Health Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the Johns Hopkins Institute for Clinical and Translational Research, National Center for Advancing Translational Sciences or National Institutes of Health. Conflict of interest: The authors have no conflicts of interest. Authorship: A.M.P.Y. and Y.K. designed the study. A.M.P.Y. conducted data analysis and wrote the initial draft. Y.K. contributed to the interpretation of the results. Both authors provided revision to the draft and approved the final manuscript.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980020002396











