Bulimia nervosa is a common and disabling disorder seen most frequently in young women. Reference Currin, Schmidt, Treasure and Jick1,Reference de la Rie, Noordenbos and van Furth2 Cognitive–behavioural therapy (CBT) is the treatment of choice. 3 Self-care manuals of CBT for bulimia nervosa exist, which have been evaluated in randomised controlled trials (RCTs). Reference Perkins, Murphy, Schmidt and Williams4,Reference Schmidt, Lee, Beecham, Perkins, Treasure, Yi, Winn, Robinson, Murphy, Keville, Johnson-Sabine, Jenkins, Frost, Dodge, Berelowitz and Eisler5 A stepped care model using self-care as the first step has been recommended for bulimia nervosa Reference Haaga6 and was endorsed by the National Institute for Health and Clinical Excellence (NICE). 3
Computerised CBT interventions (CD–ROM or internet based) may be an alternative to manual-based self-care. Such interventions may have advantages over books, as they are more interactive and individually tailored. Web-based interventions have been used in two RCTs for the prevention of eating disorders, Reference Taylor, Bryson, Luce, Cunning, Doyle, Abascal, Rockwell, Dev, Winzelberg and Wilfley7,Reference Jacobi, Morris, Beckers, Bronisch-Holtze, Winter, Winzelberg and Taylor8 in a non-randomised trial of bulimia nervosa Reference Carrard, Rouget, Fernández-Aranda, Volkart, Damoiseau and Lam9 and in one exploratory RCT in binge eating disorder. Reference Shapiro, Reba-Harrelson, Dymek-Valentine, Woolson, Hamer and Bulik10 We previously piloted a CD–ROM based CBT intervention Reference Williams, Aubin, Cottrell and Harkin11 in individuals with bulimia nervosa Reference Murray, Pombo-Carril, Bara-Carril, Grover, Reid, Langham, Birchall, Williams, Treasure and Schmidt12–Reference Bara-Carril, Williams, Pombo-Carril, Reid, Murray, Aubin, Harkin, Treasure and Schmidt14 with good outcomes and acceptability. As yet, no RCT has addressed the effectiveness of a computerised intervention in the treatment of bulimia nervosa. The aim of the present study was to investigate the effectiveness of an unsupported/unguided CD–ROM based CBT intervention followed by a flexible number of therapist sessions (5 or 15) against 3 months on a waiting list followed by 15 therapist sessions, using a stepped care design in a routine clinical setting. We hypothesised that people receiving the CD–ROM treatment as the first step in treatment would show greater symptomatic improvement compared with those on the waiting list at 3 months, and that at 7 months individuals in both groups would have similar outcomes. We also hypothesised that participants in the CD–ROM group would need fewer therapist sessions than those who did not have the CD–ROM as the first step of treatment.
Method
Participants
Participants were recruited during 2003–2006 from consecutive referrals to the adult Eating Disorders Out-patients Service in the South London and Maudsley National Health Service (NHS) Foundation Trust. This is the main eating disorders service provider for a local population of 2 million people. Individuals are referred by general practitioners. Referrals with bulimia nervosa or eating disorder not otherwise specified (NOS) (bulimic type) as defined by DSM–IV, 15 were eligible for the study and were invited to participate. Diagnosis was confirmed by senior clinicians using a semi-structured interview designed and used within the service as part of the assessment procedure. We included participants with clinically significant levels of compensatory behaviours (purging), but without objective binges. As a minimum frequency for inclusion, participants had to engage in key bulimic behaviours on average once a week over the previous 3 months.
Exclusion criteria were insufficient knowledge of English, insufficient literacy skills, severe intellectual disability, anorexia nervosa, severe depression, acute suicidality, and alcohol or substance dependence. We did not exclude participants on antidepressants, provided they were on a stable dose for at least the preceding 4 weeks.
Eligible individuals were approached for participation at initial clinical assessment and gave written informed consent to participate in the trial. The study was approved by the joint research ethics committee of the Institute of Psychiatry and the South London and Maudsley NHS Foundation Trust. The trial was registered in the ISRCTN register (ISRCTN51564819).
Trial interventions
CD–ROM group
Participants in this group undertook a CD–ROM self-care treatment with no practitioner guidance/support followed by therapist sessions depending on clinical need. ‘Overcoming Bulimia’ Reference Williams, Aubin, Cottrell and Harkin11 is a CD–ROM-based cognitive–behavioural interactive multimedia programme. It consists of eight modules, combining cognitive– behavioural, motivational and educational strategies. The content of the modules is detailed in the Appendix. A central feature is the development of a personalised CBT formulation of individuals' own vicious cycle of bulimia, i.e. the factors maintaining bulimic and compensatory symptoms (Modules 1–3). Strategies for re-learning to eat normally and for interrupting bulimic behaviours are taught early on. Later modules focus on identifying and challenging unhelpful thoughts, particularly in relation to weight, shape and appearance. A range of basic CBT techniques address skills deficits (such as poor problem-solving, low assertiveness) commonly found in bulimia, so as to enable participants to lead fuller, more balanced lives without bulimia. Each module requires about 45 min at the computer. To prevent unstructured browsing and dipping in and out of different modules, these have to be worked through in sequence and a new module can only be accessed once the previous module has been completed. Each module finishes with a set of homework tasks. Eight patient workbooks that contain a condensed version of the module contents accompany each session. Individuals received all workbooks at the beginning of treatment. Self-assessment tools in the programme provide them with printed feedback on their progress, detailing levels of bulimic symptoms, depression and anxiety.
Participants used the CD–ROM package in a private, designated room in the out-patient department of the eating disorders unit. They were introduced to the programme and booked in for further computer appointments by a non-clinical administrator. Participants were asked to complete the programme over 8–12 weeks. No practitioner support or guidance was offered during the time the individual used the CD–ROM, and they organised their appointments and use of sessions by themselves using a paper-based booking system run by an administrator.
Three months later, participants were reviewed by a clinician and offered either shorter or longer face-to-face therapy. The need for further treatment was determined using operational criteria adapted from a study on manual-based self-care in bulimia nervosa. Reference Palmer, Birchall, McGrain and Sullivan16 People with a reduction in key symptoms (bingeing, vomiting, purgatives) of less than 50% were offered full CBT (15 sessions of one-to-one therapy by an eating disorders specialist), whereas those with a reduction in symptoms of more than 50% were given minimal therapist support (5 sessions) to support their continued use of CBT self-care.
Waiting-list control group
Participants allocated to this group had a 3-month wait before they started a full course of one-to-one CBT for bulimia nervosa (15 sessions). This treatment contains key elements of Fairburn's maintenance model of CBT for bulimia Reference Fairburn, Cooper and Shafran17 but also has additional elements. Initially this treatment focuses on the function of bulimia nervosa in the person's life and builds motivation to change. Information about how bulimic symptoms are maintained is introduced, using self-monitoring of thoughts, feelings and behaviours. Problem-solving, goal-setting and behavioural experiments are used to help participants alter vicious cycles of behaviour. A case formulation is developed collaboratively. Towards the end of treatment, relapse prevention is covered. In the penultimate session the therapist writes a goodbye letter. The follow-up sessions focus on relapse prevention. Regular homework accompanies the treatment. Participants in this group did not have access to the computer-based intervention.
Therapists and treatment fidelity
Study treatments were delivered by 16 NHS clinicians working in the eating disorders unit, with training in CBT of eating disorders.
Therapists received routine clinical group supervision for their cases. Written guidance was provided for the therapists as to which treatment elements to include in their intervention and how to sequence and pace these, given the available session number. As this is an effectiveness trial no attempt was made to assess quality or uniformity of and adherence to CBT through the use of tapes.
Randomisation, masking and protection against bias
Following clinical assessment, which checked people's suitability for participation and after giving written consent, participants were contacted by a researcher who conducted the initial research assessment via telephone interview. Thereafter, participants were randomised to one of the two trial interventions.
The randomisation sequence was prepared independently from the rest of the trial team by a statistician (S.L.). Blocks of random sizes between 4 and 10 people were used to assign individuals to one of the two trial arms. Treatment allocation codes were contained in a computerised randomisation database which concealed the sequence until interventions were assigned. Names of consenting participants were entered into the database by the unit administrator and the treatment allocation was conveyed to the assessing clinician. Participants were informed in writing by the clinician of the outcome of randomisation, and those randomised to the CD–ROM treatment were advised to make an appointment with the administrator to start the CD–ROM treatment as soon as possible. The others were informed of the wait for treatment. All participants were asked to re-attend 3 months later to see the clinician for review and immediately prior to this had a telephone assessment with the researcher. This separation of tasks between the clinician and the research assessor was done so as to keep the researcher masked to treatment allocation. Throughout the trial every effort was made to ensure that the assessor remained masked to the treatment condition. The combination of masked assessments and independent prospective data records reduced scope for bias.
Assessments and measures
All outcome assessments were carried out over the telephone by researchers trained in their administration (S.P., O.D., S.R.) and masked to the treatment allocation of the participant. Previous studies have found excellent agreement between diagnostic interviews administered by telephone or face to face. Reference Rohde, Lewinsohn and Seeley18
Three months following the baseline research assessments, participants were contacted by the researcher for their second research assessment. Following this, information about the participant's key bulimic symptoms was given to the clinician conducting the 3-month clinical review with the participant. The aims of this review meeting were to gain further information on the participant's progress since initial assessment, to maintain contact with participants and to report back to the individual regarding their forthcoming out-patient therapy. Participants randomised to the waiting-list control group were then offered 15 sessions of out-patient CBT treatment. At 7 months following initial assessment, participants were subject to a final research assessment.
Measures included a widely used interview-based assessment of bulimic symptomatology, the Eating Disorder Examination (EDE). Reference Cooper, Cooper and Fairburn19 The primary outcomes were the EDE–Global score (EDE–G) and frequencies of the two key bulimic symptoms, bingeing and vomiting at 3 and 7 months. Additional outcomes were EDE sub-scale scores, proportion of participants in remission or abstinence from bingeing, vomiting and laxatives, and treatment adherence. Remission was defined as being below the DSM–IV threshold (i.e. bingeing, vomiting and laxative misuse present less than twice a week) over the previous 28 days. Abstinence was defined as being free of bingeing vomiting and laxative misuse over the previous 28 days. Participants also completed several questionnaires (to be reported elsewhere).
Proposed sample size
At the time when the trial started we did not have pilot data using the EDE as an outcome measure after CD–ROM treatment. Thus, the power calculation was based on remission rates from self-induced vomiting in our pilot study. Reference Bara-Carril, Williams, Pombo-Carril, Reid, Murray, Aubin, Harkin, Treasure and Schmidt14 We assumed that 69% in the CD–ROM treatment group (as in our pilot study) and 29.8% in the waiting-list group Reference Bara-Carril, Williams, Pombo-Carril, Reid, Murray, Aubin, Harkin, Treasure and Schmidt14 would be in remission from vomiting at 3 months. To detect such an effect with a power of 90% a sample size of 33 people per group would be required using a two-sided chi-squared test at a significance level of 5%. Applying an attrition correction factor of 1/(1–a), where the attrition to follow-up rate is a=0.30, a total of 94 people would be needed.
Statistical analysis
Descriptive statistics were used to summarise the baseline variables namely current diagnosis, gender, ethnicity, age, body mass index (BMI) and antidepressant medication, and the eating disorders outcome variables from the EDE.
Since there was an attrition rate of 38.1% from baseline to the 7-month follow-up time point, the drop-out mechanism was studied (by drop-out we refer here to non-participation in research assessments). Logistic regression was used to determine whether the individuals' baseline characteristics (age, diagnosis, ethnicity, illness duration, antidepressant medication and BMI) were predictive of the probability of drop-out by the 7-month time point. In addition, participants at time ‘t’ were divided into those who supplied data to time point t+1 and those who did not (dropped out) to assess whether earlier values of an outcome variable predicted later drop-out. To minimise assumptions regarding the drop-out mechanisms, a random intercepts model was fitted using maximum likelihood which provides valid estimates under the less restrictive assumption that the drop-out process is missing at random (MAR). Specifically, drop-out was allowed to depend on earlier values of the outcome variable and explanatory variables that were included in the model.
Formal statistical analyses were carried out to assess the effect of the two interventions at the two post-intervention time points on the outcome variables: EDE–G score, objective binge episodes and episodes of self-induced vomiting. The analysis models contained baseline values of the outcome variable, time points, groups and the interaction between time and group as explanatory variables. The analyses further contained random intercepts for individuals to take account of the correlations between their measures at 3- and 7-month time points.
For the EDE–G score, a random intercept model was fitted using the Stata 9 command ‘xtreg’. The regression model contained contrasts for the time factor (3-month v. 7-month time points), the main effect of group (CD–ROM v. waiting list) and the group × time interaction. The interaction effect was initially tested to assess whether the groups differed significantly at 3- and 7-month time points. If the interaction was not significant then only the main effects were included in the model.
In order to decide whether any baseline characteristics (current diagnosis, gender, ethnicity, age, illness duration, BMI and antidepressant medication) should be included in the analysis model as further predictor variables, such variables were added to the analysis model one by one and significance tests carried out to assess whether they explained post-intervention variability in the outcome measure on top of what could be explained by baseline variability.
The same procedure was used to analyse the outcome variables ‘objective binge episodes’ and ‘episodes of vomiting’. However, since these variables are of a count nature (number of episodes during the previous month) a normal distribution could not be assumed. Instead, the variables were assumed to follow a Poisson distribution and be linearly related to the predictor variables on the log scale. The corresponding generalised linear mixed models were fitted using the Stata command ‘xtpoisson’.
Results
Participant flow through the study
Figure 1 shows the flow of people through the study. Treatment uptake was similar in both groups with about two-thirds of individuals taking up CD–ROM or therapist sessions (after being on the waiting list). One individual in the waiting-list group died from a non-eating-disorder-related cause after the 3-month assessment and therefore did not take up therapy. In people who started the CD–ROM, the median number of CD–ROM sessions attended at 3 months was 3 (range 1–8) and at 7 months was 6.5 (range 1–8). In people who started therapist sessions, the median number of therapist sessions attended at 7 months was 5 (range 1–15) in the CD–ROM group compared with 8.5 (range 1–17) in the waiting-list group. This difference is significant (Mann–Whitney U=666.5, P=0.03).
Baseline characteristics
Overall, 97 people participated in this study with 61.9% diagnosed with bulimia nervosa and 38.1% with eating disorder NOS. Most participants were female (96.9 %) and were from a White British background (73.3%). The mean age of individuals was 27.1 years (s.d.=7.6); their mean BMI was 23.6 kg/m2 (s.d.=5.2); and 33.7% were on antidepressant medication. Forty-nine people (50.5%) were randomised to the CD–ROM group and 48 (49.5%) to the waiting list. The participant characteristics by group are given in Table 1. It also demonstrates that randomisation led to similar baseline characteristics in the two groups.
Table 1 Baseline demographic and clinical data
| Characteristic | CD—ROM group (n=49) | Waiting-list group (n=48) | Total (n=97) |
|---|---|---|---|
| Current diagnosis, n (%) | |||
| Bulimia nervosa | 33/49 (67.3) | 27/48 (56.2) | 60/97 (61.9) |
| Eating disorder NOS | 16/49 (32.7) | 21/48 (43.8) | 37/97 (38.1) |
| Gender, n (%) | |||
| Female | 49/49 (100) | 44/48 (91.7) | 93/97 (96.9) |
| Ethnicity, n (%) | |||
| White British | 27/38 (71.1) | 28/37 (75.7) | 55/75 (73.3) |
| Other | 11/38 (28.9) | 9/37 (24.3) | 20/75 (26.7) |
| Age, years: mean (s.d.) | 25.6 (6.2) | 28.7 (8.6) | 27.1 (7.6) |
| Body mass index, kg/m2: mean (s.d.) | 24.3 (6.2) | 22.8 (3.8) | 23.6 (5.2) |
| On antidepressant medication, n (%) | 12/43 (27.9) | 17/41 (41.5) | 29/84 (34.5) |
| Duration, years: median (min, max) | 6.0 (0.5, 30.0) | 9.5 (0.5, 32.0) | 8.0 (0.5, 32.0) |
Description of outcome variables
Online Tables DS1–DS3 show medians with interquartile ranges and means with standard deviations of EDE variables for the two randomisation groups. The number of participants decreased over the study period with 60 people out of 97 (61.9%) contributing assessments at all three time points. The tables show that average values of all variables and in both groups decreased over time. This table provides summaries by group but it is important to note that these summary statistics may not provide unbiased estimators, rather they may be subject to selection biases if the drop-out mechanism is not missing completely at random (MCAR).
Drop-out mechanism
To assess this issue the drop-out mechanism was studied to find out whether baseline variables (current diagnosis, ethnicity, age, illness duration, BMI and antidepressant medication) predicted the drop-out. Logistic regression analyses did not detect any significant relationships between the baseline variables and drop-out by the follow-up time point (all P-values >0.05). In addition, means and 95% confidence intervals (CIs) were constructed for the EDE–G score by groups of later drop-outs and non-drop-outs (Fig. 2). Although the figure shows that the mean EDE–G score of participants that later drop-out tend to be higher than of those that do not, there was no evidence of a significant relationship since the CIs for the drop-out and non-drop-out groups were widely overlapping. We therefore found no evidence that the drop-out mechanism was not MCAR but nevertheless decided to use analyses that only assume MAR to err on the side of caution.

Fig. 1 Flowchart of design. a. One of these participants died.
Formal randomisation group comparison
The outcome variables EDE–G score, objective binge episodes and vomiting were subject to formal statistical analysis. Table 2 shows the results of fitting random intercept models (EDE–G) and Poisson regressions with random intercepts (bingeing, vomiting) to these outcome variables.
Table 2 Comparison between groups (waiting-list and CD–Rom) at 3- and 7-month time points
| Outcome variable | Estimated group difference (score) | z score | P | 95% CI |
|---|---|---|---|---|
| EDE—G | 0.18 | 0.78 | 0.43 | -0.26 to 0.61 |
| Objective binge episodes | ||||
| 3-month assessment | 0.72a | -1.15 | 0.25 | 0.41 to 1.26 |
| 7-month assessment | 1.51a | 1.40 | 0.16 | 0.85 to 2.69 |
| Vomiting | ||||
| 3-month assessment | 0.97a | -0.10 | 0.92 | 0.53 to 1.77 |
| 7-month assessment | 1.77a | 1.83 | 0.07 | 0.96 to 3.27 |
For EDE–G the predictive effect of baseline scores on later scores was confirmed empirically (z=8.21, P<0.001). The interaction between post-intervention time and randomisation group was not statistically significant (χ2=2.06, d.f.=1, P=0.15) indicating similar group differences at both 3- and 7-month time points. Hence, the interaction term was removed from the model and main effects of group and time were tested. At the 5% level there was no evidence for a significant main effect of group for this outcome measure (P=0.43, Table 2) nor was there any evidence of change between the 3- and 7-month time points (z=1.48, P=0.14). However, we found that ethnicity predicted the EDE–G score with White British participants having significantly lower scores than ethnic minority participants (95% CI for the difference 0.06–1.07, z=2.2, P=0.03). None of the other participant characteristics (age, diagnosis, duration, antidepressant medication and BMI) was predictive (all P-values above 0.05).
For bingeing and vomiting episodes baseline values were also found to be predictive (bingeing: z=3.41, P=0.001; vomiting: z=3.87, P<0.001). For both bingeing and vomiting the interaction was statistically significant (bingeing: χ2=34.4, d.f.=1, P<0.001; vomiting: χ2=32.7, d.f.=1, P<0.001) indicating that the group differences significantly differed between 3- and 7-month time points. Table 2 shows separate post hoc group comparisons at the 3- and 7-month time points. Because Poisson regression has been used here, group effects are measured by incidence rate ratios (IRR). The table shows that the IRRs are not significantly different from 1 at any time point, that is we cannot prove a specific treatment effect at a given time for either intervention. The nature of the interactions is such that bingeing and vomiting rates in the CD–ROM group are decreased compared with the waiting-list group at the 3-month time point, whereas by 7 months the reverse is true. The interaction for the bingeing outcome is also demonstrated in Fig. 3. Finally, none of the participant characteristics was found to provide extra predictive power for either bingeing or vomiting outcomes (all P>0.05).
Moderator analysis
The moderator effects of eating disorder diagnosis (bulimia nervosa, eating disorder NOS) and antidepressant on the CD–ROM group were tested and were not significant for any of the three outcome variables (all P>0.05).
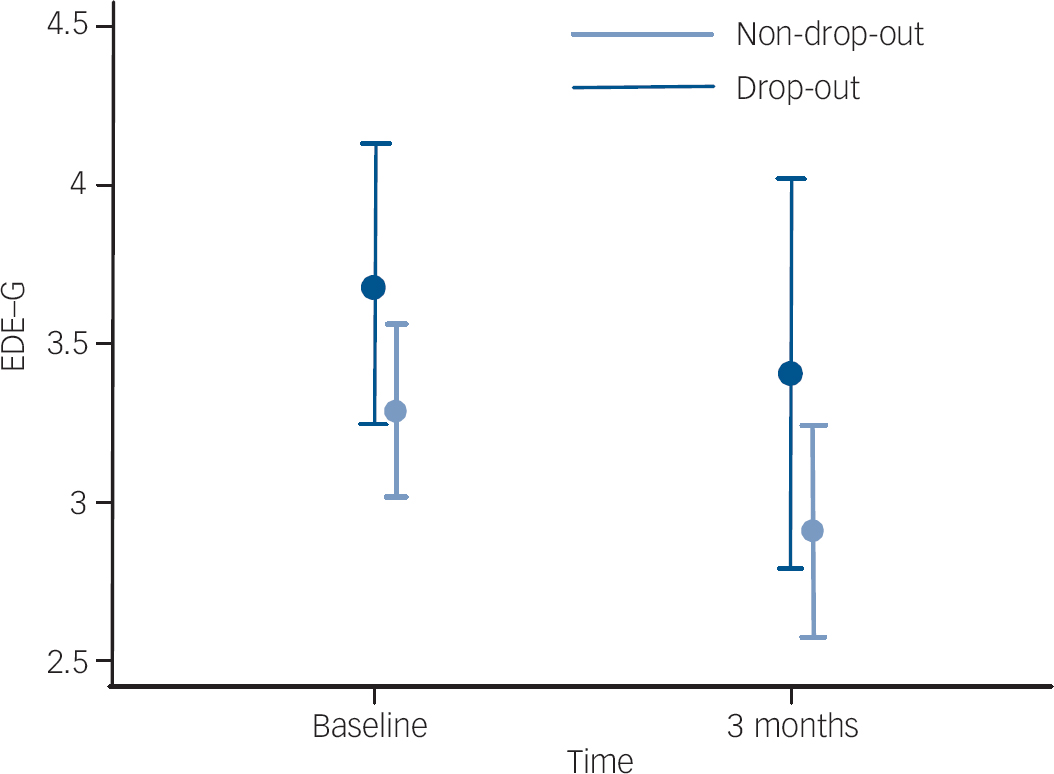
Fig. 2 Mean Eating Disorder Examination–Global (EDE–G) score and 95% CI for participants who dropped out from the study at the next time point (drop-out) and those who did not.
Adherence to CD–ROM sessions and outcome
Given that a significant proportion of people who had enrolled in the study did not take up the CD–ROM intervention or had only attended a small number of CD–ROM sessions at 3-month assessment, we wanted to know whether outcome at 3 months depended on the use of the CD–ROM. We divided those who had been randomised to the CD–ROM into two groups, i.e. those who attended 0–4 sessions (low adherence) and those who attended 4–8 sessions (high adherence) by the 3-month assessment. Five of eight individuals (62.5%) in the high-adherence group compared with 11 of 33 (33%) in the low-adherence group were in remission from bingeing, vomiting and laxative misuse at 3 months.
Discussion
Key findings in relation to hypotheses
The aim of this study was to investigate the effectiveness of a CD–ROM-based intervention in bulimia nervosa and eating disorder NOS in a routine clinical setting using a stepped care design. We hypothesised that participants receiving the CD–ROM treatment would show greater symptomatic improvement compared with those on the waiting list at 3 months, and that by 7 months these differences would have disappeared. This hypothesis was partially confirmed, in that there was a significant group × time interaction on the outcome variables objective binge episodes and vomiting favouring CD–ROM at 3 months, whereas the reverse was true at 7 months. As post hoc comparisons of group differences on bingeing and vomiting at the 3- and 7-month time points showed no significant differences we cannot prove a specific treatment effect at a given time.
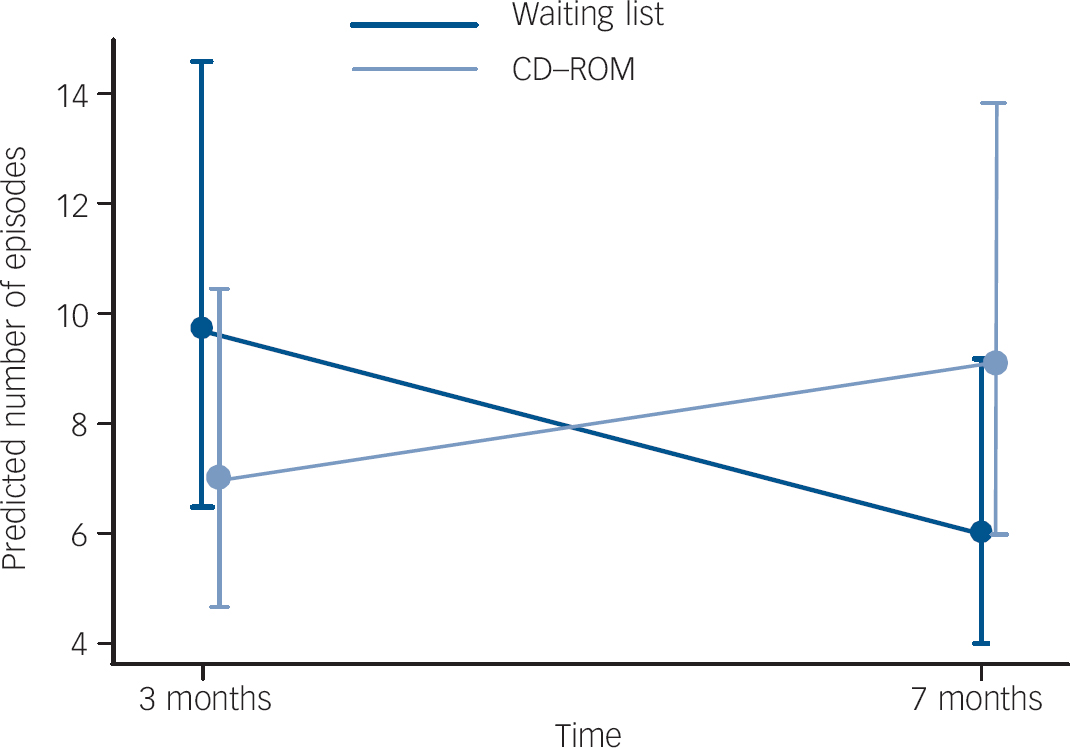
Fig. 3 Predicted mean and 95% CI for objective binge episodes at 3- and 7-month time points (baseline bingeing is adjusted to its sample mean).
Our subsidiary analysis of the relationship between individuals' attendance at the CD–ROM sessions and outcome suggests that the small group of people who attended the majority of CD–ROM sessions within 3 months had much higher remission rates at 3 months than those who attended fewer sessions (five of eight individuals in the high-adherence group (62.5%) v. 11 of 33 in the low adherence group (33%)). This mirrors the findings from an earlier study by our group Reference Troop, Schmidt, Tiller, Todd, Keilen and Treasure20 that examined adherence to a manual-based self-help intervention for bulimia nervosa. This earlier study also found better outcomes in those who adhered to the intervention. It is of course entirely possible that this could be because of the characteristics of such (adherent) individuals rather than the effects of the CD–ROM.
Our second hypothesis that people receiving CD–ROM as the first step in treatment would have fewer therapist sessions thereafter was also confirmed. The number of therapist sessions offered to individuals in the CD–ROM group depended on their rate of improvement at 3 months. However, it may be that offering five sessions only to those who had a reduction in key symptoms of more than 50% at 3 months was simply ‘too little too late’ and may have been responsible for the waning of the CD–ROM group's earlier therapeutic gains at 7 months.
Other findings
Global EDE scores were found to be higher in ethnic minority participants compared with those of their White British counterparts. There could be many reasons for this. For example, general practitioners may have a higher threshold for referring people from ethnic minorities to eating disorder services because of beliefs that eating disorders predominantly affect White middle-class women or these differences may relate to socio-economic differences between these groups or levels of support available to them. This deserves further study in future.
Strengths and limitations
This is the first RCT of computerised CBT in bulimia nervosa in a clinical setting. It is of reasonable size and uses a gold-standard interview assessment procedure. The one other existing RCT on CD–ROM-based CBT for binge eating disorder (a related condition) is limited, because it includes volunteers rather than patients, does not have an interview-based outcome assessment and has very poor follow-up rates. Reference Shapiro, Reba-Harrelson, Dymek-Valentine, Woolson, Hamer and Bulik10 The present study addresses one of the research recommendations made in the NICE guidelines on eating disorders, 3 namely that effectiveness trials of bulimia nervosa are urgently needed, to see how effective treatment, i.e. CBT for bulimia nervosa, can be translated into routine clinical practice.
As for the limitations of the study, about a third of participants had not completed a full course of treatment at 7 months, but resource constraints prevented us from conducting a further follow-up assessment at 1 year. To understand better how participants utilise the CD–ROM intervention it would have been desirable not just to measure session attendance as an indicator of treatment adherence, but also ask about use of accompanying workbooks.
Uptake and retention
Uptake of both interventions was sub-optimal in that about a third of participants in each group failed to attend any treatment. This is characteristic of people referred to London eating disorders services Reference Waller, Schmidt, Treasure, Murray, Alenya, Emanuelli, Crockett and Yeomans21 and eating disorder services in other inner-city areas (e.g. New York City). Reference Agras, Walsh, Fairburn, Wilson and Kraemer22 This perhaps reflects the transient urban population served. A recent study of the care pathways of nearly 1900 local people referred to our unit and the other large eating disorders unit (St George's Hospital) covering South London found that of the original referrals, approximately 35% were never seen, only half entered treatment, and only a quarter reached the end of treatment. Reference Welch and Fairburn23
Several practical factors affected the outcomes of this study. All participants in the present study had long periods of waiting for assessment and treatment. The first bottleneck was the time between general practitioner referral and specialist assessment in our unit, where people usually had to wait several months for this to happen. Those allocated to the waiting-list group then had a further wait of 3 months and even after that instant therapy could not be guaranteed for a proportion of cases, owing to lack of therapist availability. Thus, it is unsurprising that this would have negatively affected motivation for treatment and willingness to cooperate with research procedures.
Participants had to attend the eating disorders clinic to access the CD–ROM. This was done as a safety precaution, as it is known that a significant proportion of people with bulimia nervosa suffer from depression and suicidality. Reference Gellatly, Bower, Hennessy, Richards, Gilbody and Lovell24 However, given that all our participants had a careful clinical assessment prior to starting the CD–ROM programme, major risk issues did not arise over the course of the study. Accessing the CD–ROM in clinic limited individuals' flexibility of its use, in that appointments could only be made during working hours and one of our clinic sites only operated on a part-time basis.
Since starting the present study, a web-based version of the ‘Overcoming Bulimia’ programme has become available. Delivering the intervention over the web has the advantage of increasing flexibility of access in that people can use it at a time that suits them.
Therapist guidance
Previous studies of manual-based self-care in bulimia nervosa have found that guidance from a therapist helps with programme adherence and improves outcomes. Reference Perkins, Murphy, Schmidt and Williams4 A recent meta-analysis of self-help interventions in depression also found clear evidence that guided self-help is more effective than unguided self-help and helps those with low motivation to keep on track. Reference Gellatly, Bower, Hennessy, Richards, Gilbody and Lovell24 In the present study no guidance was given during the 3 months while participants worked through the CD–ROM. At 3 months when people had their clinical review assessment many hadn't completed the CD–ROM, but with one-off encouragement from the clinician they then attended further CD–ROM sessions. This significantly increased the median number of sessions of the package completed from 3 to 6.5.
In one of our previous pilot studies on the CD–ROM intervention we found that adding limited face-to-face support (three times for 20 min) from a trainee psychologist during CD–ROM treatment did not improve outcomes. Reference Murray, Schmidt, Pombo-Carril, Grover, Alenya, Treasure and Williams13 It is possible that this study may have been underpowered. Moreover, if support was given by experienced clinicians this may have a more positive impact. In this context, it is of interest that in the treatment of anorexia nervosa a supportive treatment delivered by experienced clinicians was more effective than other interventions. Reference McIntosh, Jordan, Carter, Luty, McKenzie, Bulik, Frampton and Joyce25 Future studies should consider giving this intervention with specialist guidance to improve outcomes and retention in treatment.
It is government policy to advocate self-care interventions for common mental disorders where possible Reference Lewis, Anderson, Araya, Elgie, Harrison, Proudfoot, Schmidt, Sharp, Weightman and Williams26 but our findings suggest that we need to learn a lot more about how best to utilise and support these kinds of interventions with which kinds of individuals and in what settings. All in all, this computerised intervention does seem to have promise as a first step in treatment of bulimia nervosa. However, by the time individuals have been referred for specialist treatment and have waited for a considerable time it is difficult to mobilise people into following a self-care programme. Several factors may contribute to making this intervention more effective and improve uptake and adherence. First, it may be more fruitful to deliver this intervention over the web rather than offer it in a clinic setting. Second, it may be preferable to deliver this intervention to people at an earlier stage of their disorder, i.e. target young people in schools or universities or offer this intervention in the voluntary sector and/or to individuals who are actively interested in pursuing self-care treatments. Finally, as research in depression has confirmed the benefits of providing support/guidance for the use of CBT self-help, this should be incorporated into future research. Studies exploring these options are currently under way.
| Description of sessions on CD—ROM | ||
|---|---|---|
| Session | Title | Session content |
| Session 1 | What is bulimia? | Bulimia and its physical and emotional consequences |
| The vicious cycle of bulimia | ||
| Session 2 | Understanding why I have bulimia | Why people develop eating disorders |
| How food, shape and weight are seen in our society | ||
| Increasing motivation to change | ||
| Session 3 | How do I change? | How to break the vicious cycle |
| The rules of healthy eating | ||
| How to fight food cravings | ||
| Session 4 | The role of thoughts in bulimia | Role of thoughts in bingeing |
| Unhelpful ways of thinking | ||
| How to change extreme and unhelpful thoughts | ||
| Session 5 | Assertiveness and a ‘bigger life’ | Activity scheduling |
| How to be assertive | ||
| Session 6 | Problem-solving | The role of thinking and coping in the face of practical difficulties |
| Session 7 | Living life to the full | How to face up to your fears |
| How to build your confidence and enjoy life more | ||
| Start doing things you stopped doing | ||
| How to use a daily activity diary to increase feelings of pleasure and achievement in life | ||
| Session 8 | Planning for the future and review of what I have learned | Review of previous sessions |
| Relapse prevention: plan for the future and write a personal plan to cope | ||
Acknowledgements
The study was supported by a Psychiatry Research Trust grant to U.S., C.W., S.L., M.G. and J.T. We thank Dr Rudolf Uher, Ms Barbara Pavlova and Mr Peter Musiat for their helpful comments on the manuscript. We also thank all the therapists of the eating disorders unit who participated in the study.









eLetters
No eLetters have been published for this article.