Introduction
Apart from the provision of clean water, vaccines have had a more profound effect on global health, especially children, than any other public health measure (Public Health England, 2014; WHO, 2021; Rodrigues & Plotkin, Reference Rodrigues and Plotkin2020). Despite this, millions of children around the world do not receive the recommended vaccines. In 2020, 23 million children missed out on routine childhood vaccinations, the highest number since 2009 and 3.7 million higher than in 2019 (WHO, 2021; UNICEF, 2022).
Poor vaccination coverage leads to outbreak of diseases (UNICEF, 2019). For example, in January and February 2022, there were over 17 338 cases of measles recorded globally, compared to 9665 cases in the same period in 2021 (WHO, 2022). In England and Wales in 2018, there was a marked increase in confirmed measles cases with 991 cases, compared to 284 cases in 2017 (Public Health England, 2019). These developments led to the UK losing its ‘measles-free’ status with the World Health Organization (WHO) barely three years after the measles virus was eliminated from the country (Wise, Reference Wise2019).
Concern from parents, decision-makers, and the media regarding the safety of recommended immunisations has increased in recent years due to debates regarding the links between vaccines and autism, vaccine ingredients, and the number of injections given during a single office visit or during the first years of life (Miller & Reynolds, Reference Miller and Reynolds2009; Davidson, Reference Davidson2022; Gabis et al., Reference Gabis, Attia, Goldman, Barak, Tefera, Shefer, Shaham and Lerman-Sagie2022). An increasing number of people question the safety of vaccines (Yaqub et al., Reference Yaqub, Castle-Clarke, Sevdalis and Chataway2014; Dubé, et al. Reference Dubé, Vivion and MacDonald2015; Larson et al., Reference Larson, Jarrett, Schulz, Chaudhuri, Zhou, Dube, Schuster, MacDonald and Wilson2015a), seek alternative measures such as natural methods (eg, rigorous hygiene) and antibiotic use (Dempsey et al., Reference Dempsey, Schaffer, Singer, Butchart, Davis and Freed2011; Robison et al., Reference Robison, Groom and Young2012; Popa et al., Reference Popa, Muntean, Muntean and Popa2020) and sometimes delay or refuse vaccination (Gust et al., Reference Gust, Darling, Kennedy and Schwartz2008; Larson et al., Reference Larson, Jarrett, Eckersberger, Smith and Paterson2014a; Larson et al., Reference Larson, Wilson, Hanley, Parys and Paterson2014b). This delay or refusal of vaccination is termed vaccine hesitancy (VH). VH is of grave concern, such that it was listed by the WHO as one of the ten threats to global health in 2019 (WHO, 2019).
VH is determined by a wide range of factors. In the UK, a cross-sectional study of 600 participants including GPs, health visitors, practice nurses and parents of immunised children found that socioeconomic factors, such as high social class and being a first-time parent, were important predictors of delayed childhood vaccination (Macdonald et al., Reference MacDonald, Henderson and Oates2004). Family size and parental education were identified as determinants of under-immunisation in Greece (Danis et al., Reference Danis, Georgakopoulou, Stavrou, Laggas and Panagiotopoulos2010). In Nigeria, maternal availability, lack of knowledge and parental disapproval were associated with partial immunisation (Babalola, Reference Babalola2011). A combination of sociodemographic and socioeconomic factors such as marital status, maternal education and family income influenced parental decision-making in Israel (Stein-Zamir & Israeli, Reference Stein-Zamir and Israeli2017), Saudi Arabia (Alsubaie et al., Reference Alsubaie, Gosadi, Alsaadi, Albacker, Bawazir, Bin-Daud, Almanie, Alsaadi and Alzamil2019), Italy (Giambi et al., Reference Giambi, Fabiani, D’Ancona, Ferrara, Fiacchini, Gallo, Martinelli, Pascucci, Prato, Filia and Bella2018), Australia (Chow et al., Reference Chow, Danchin, Willaby, Pemberton and Leask2017), and USA (Omer et al., Reference Omer, Salmon, Orenstein, deHart and Halsey2009; Rachel et al., Reference Rachel, Minard, Guffey, Swaim, Opel and Boom2018).
Several systematic reviews have investigated factors that influence VH across different populations, with a particular focus on the influence of knowledge, attitudes, and beliefs on vaccination behaviour (Falagas & Zarkadoulia, Reference Falagas and Zarkadoulia2008; Rainey et al., Reference Rainey, Watkins, Ryman, Sandhu, Bo and Banerjee2011; Prematungr et al., Reference Prematunge, Corace, McCarthy, Nair, Pugsley and Garber2012; Trim et al., Reference Trim, Nagji, Elit and Roy2012). While it is important to identify potential determinants of VH, the proportion of parents who are vaccine-hesitant needs to be estimated using widely validated, theory-based psychological scales, to inform researchers and policymakers about the burden of vaccine-preventable diseases (VPDs), which will ultimately help in identifying priorities in healthcare prevention, promotion, practices, and policy (Bloom, Reference Bloom2008; Mahase, Reference Mahase2020). Few studies offer quantitative tools to measure prevalence of VH and even fewer studies have used standardised, widely validated survey instruments, such as the Parent Attitudes about Childhood Vaccinations scale (Opel et al., Reference Opel, Mangione-Smith, Taylor, Korfiatis, Wiese, Catz and Martin2011a; Opel et al., Reference Opel, Taylor, Mangione-Smith, Solomon, Zhao, Catz and Martin2011b), to achieve these objectives.
Few researchers have applied theories of health behaviour to vaccination uptake. The Protection Motivation Theory (PMT) (Rogers, Reference Rogers1975; Rogers, Reference Rogers, Cacioppo and Petty1983; Maddux & Rogers, Reference Maddux and Rogers1983; Rogers & Prentice-Dunn, Reference Rogers, Prentice-Dunn and Gochman1997), developed to understand how people respond to health threats, is one such theory. PMT suggests that people will be likely to protect themselves (eg, by obtaining a vaccine) if they have firm beliefs about the threat posed by the disease itself (severity and vulnerability) (Voeten et al., Reference Voeten, de Zwart, Veldhuijzen, Yuen, Jiang, Elam, Abraham and Brug2009). PMT considers the physical and psychosocial consequences of engaging in a risky behaviour (intrinsic and extrinsic rewards) and the costs (eg, personal resources) involved in avoiding the given health threat (response costs) (Rogers & Prentice-Dunn, Reference Rogers, Prentice-Dunn and Gochman1997), as displayed in Figure 1. In addition, PMT considers people’s beliefs in their own abilities to adopt a protective measure (self-efficacy) as well as the outcomes of their behaviour (response efficacy) (Maddux & Rogers, Reference Maddux and Rogers1983; Rogers & Prentice-Dunn, Reference Rogers, Prentice-Dunn and Gochman1997). PMT thus reliably predicts behavioural intentions based on attitudes and perceptions (de Zwart et al., Reference de Zwart, Veldhuijzen, Elam, Aro, Abraham, Bishop, Voeten, Richardus and Brug2009).

Fig. 1. PMT constructs
Vaccination acceptance is a behavioural outcome that results from a complicated decision-making process that can be impacted by a variety of variables. After considering the diverse factors and the possibility of informing the development of global and country-level VH indicators, the WHO’s Strategic Advisory Group of Experts on Immunization (SAGE) Working Group developed the 3C model of VH (MacDonald, Reference MacDonald2015), which points out three different types of VH determinants: confidence, complacency, and convenience (Figure 2).

Fig. 2. 3C Model of vaccine hesitancy
Confidence is described in the 3C model as strong belief in the efficacy and safety of vaccinations, the system that distributes them, plus the trustworthiness and competency of health services, health systems and health professionals, and what drives the policymakers who determine which vaccines are required (MacDonald, Reference MacDonald2015). People with little or no vaccine confidence have negative views toward immunisations, which influence their actions. The unfavourable attitude is fuelled by misinformation, conspiracy theories, and heightened perceptions of vaccine-related risks (Betsch et al., Reference Betsch, Böhm and Chapman2015).
Complacency occurs when the dangers of VPDs are viewed as minimal, and vaccination is not considered a required precautionary measure (MacDonald, Reference MacDonald2015). Complacency about a specific vaccine, or vaccination in general, is determined by several factors, which include other general duties that are deemed more important at the time (Betsch et al., Reference Betsch, Böhm and Chapman2015). When people assess the risks of getting a specific vaccine versus the risks of getting the disease that the vaccine protects against, the success of vaccination programmes can lead to complacency and, ultimately, hesitancy (Schmid et al., Reference Schmid, Rauber, Betsch, Lidolt and Denker2017). The extent to which complacency affects hesitancy is also determined by self-efficacy (an individual’s perceived or real ability to decide whether to be vaccinated or not) (Ernsting et al., Reference Ernsting, Knoll, Schneider and Schwarzer2015).
Convenience is a crucial determinant which might result from sentiments that are neither strongly against nor strongly in favour of vaccination, implying that vaccination is insufficiently important to actively overcome physical or psychosocial barriers (MacDonald, Reference MacDonald2015). For example, access to immunisations may be hampered by geopolitical or economic reasons that affect production and supply reliability (Betsch et al., Reference Betsch, Böhm and Chapman2015). Furthermore, increased vaccine costs may result in a reduction in the frequency with which parents interact with healthcare services (Schmid et al., Reference Schmid, Rauber, Betsch, Lidolt and Denker2017). As a result, when decision-makers face obstacles such as poor access, a high cost, or a long travel time, they opt out of vaccination to avoid these issues (Betsch et al., Reference Betsch, Böhm and Chapman2015).
Grounded in the 3C model and other validated VH and acceptance models (Larson et al., Reference Larson, Jarrett, Eckersberger, Smith and Paterson2014a; Thomson et al., Reference Thomson, Robinson and Vallée-Tourangeau2016), the 5C model captures relevant determinants of vaccination behaviour and links them to psychological theories to explain health behaviour (Betsch et al., Reference Betsch, Schmid, Heinemeier, Korn, Holtmann and Böhm2018). The 5C model retains the terms ‘confidence’ and ‘complacency’, but ‘convenience’ is replaced with ‘constraints’ as it more accurately reflects the physical, structural, and psychological obstacles (eg, access, costs) that serve as gatekeepers, preventing the transition from vaccination intention to vaccination behaviour. Time spent travelling to vaccination centres or enduring unpleasant procedures can also be categorised as constraints (Betsch et al., Reference Betsch, Böhm and Chapman2015).
Calculation, the fourth ‘C’ which applies to both the 4C (Betsch et al., Reference Betsch, Böhm and Chapman2015) and 5C models (Betsch et al., Reference Betsch, Schmid, Heinemeier, Korn, Holtmann and Böhm2018), demonstrates the requirement for significant research and elaboration. People with high calculation tendencies assess the risks of infection and immunisation to make an informed decision. As a result, calculation has been linked with the risk of disease exposure and immunisation (Brewer et al., Reference Brewer, Cuite, Herrington and Weinstein2007). Cost-benefit analysis could indicate a risk-averse mindset, hence a negative correlation with risk attitude (Johnson et al., Reference Johnson, Wilke and Weber2004). The need to avoid risks could be a major incentive to people with high calculation levels, as their conscious thinking patterns suggest (Johnson et al., Reference Johnson, Wilke and Weber2004). These individuals are also known to have a more deliberate logical and cognitive decision-making style (Betsch et al., Reference Betsch, Böhm and Chapman2015) and to rely less on superstitious beliefs (Wiseman & Watt, Reference Wiseman and Watt2004).
Collective responsibility refers to a person’s willingness to safeguard others through herd immunity (Fine et al., Reference Fine, Eames and Heymann2011). The notion includes the societal benefits of vaccination, such as the fact that most immunisations protect unvaccinated individuals owing to herd immunity. The desire to free-ride when enough people are vaccinated is the opposite effect (Fine et al., Reference Fine, Eames and Heymann2011; Betsch et al., Reference Betsch, Böhm and Korn2013; Betsch et al., Reference Betsch, Böhm, Korn and Holtmann2017). Collectivism, communal attitude, and empathy have been associated with collective responsibility (Clark et al., Reference Clark, Oullette, Powell and Milberg1987; Shulruf et al., Reference Shulruf, Hattie and Dixon2007; Betsch et al., Reference Betsch, Böhm, Korn and Holtmann2017). Because collective responsibility has a negative correlation with individualism (Shulruf et al., Reference Shulruf, Hattie and Dixon2007), those with a high sense of collective responsibility are likely to vaccinate in the interests of others. Low levels may suggest that a person is unaware of herd immunity, is unconcerned about it, or refuses to vaccinate in the interest of others (Betsch et al., Reference Betsch, Böhm and Chapman2015).
Examining psychological variables is critical for understanding vaccination intention and informing effective interventions (Schmid et al., Reference Schmid, Rauber, Betsch, Lidolt and Denker2017). A more comprehensive knowledge and understanding of the underlying psychology of vaccine-hesitant groups can improve the effectiveness of public health messages aimed at these populations.
This systematic review uses the PMT and the WHO’s SAGE Working Group model as comprehensive theoretical frameworks for understanding VH and its drivers. The models served as useful tools for predicting the intention of parents to adopt protective behaviours, such as getting their children vaccinated. The physical, psychological, contextual, and sociodemographic barriers to vaccination will be identified and clustered using these theoretical models. The hesitancy profiles of the identified risk group (parents) were discussed using the 5C model, and the findings were integrated at the macro- and micro-level.
This paper examined VH from a global perspective and then narrowed its focus to the UK. The purpose is to understand parental childhood VH and inform gaps in research and interventions in the UK and, importantly, consider the wider determinants of VH as no single intervention exists to eliminate VH (WHO, 2021; Danabal et al., Reference Danabal, Magesh, Saravanan and Gopichandran2021; Wiysonge et al., Reference Wiysonge, Ndwandwe, Ryan, Jaca, Batouré, Anya and Cooper2022).
Methods
Objectives
This systematic review will achieve the following specific objectives:
-
(1) Identify relevant quantitative research on parental childhood VH with vaccine uptake and vaccination intention being relevant outcomes;
-
(2) Identify context-specific causes, behaviour, and impact of VH in the UK; and
-
(3) Map the gaps in knowledge on VH to develop suggestions for further research and to guide interventions in this field.
Search strategy
To reflect the diverse range of subject areas covered by VH, databases in medicine, nursing, public health, biological and social sciences, behavioural sciences, and psychology were used in this review. The search was also extended to relevant internet sites including Google Scholar and WHO’s Global Literature on Coronavirus Disease. The database search (see Table 1) was supplemented by a manual search of the reference lists of the included studies, as well as the cited references. The search strategy incorporated MeSH or equivalent terms.
Table 1. Selected databases

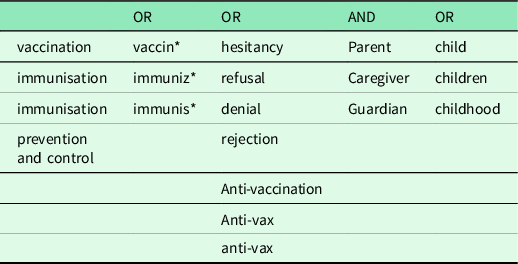
Multiple search terms were first developed and then these were combined using the Boolean operators ‘OR’ and ‘AND’. The search for data involved keywords, related terms, variants, or the same meaning for the terminologies (see Table 2).
Table 2. Keywords used in search strategy

From the identified search terms, a broad search string was first developed for MEDLINE and then adapted to all other databases. The core search around the concepts of vaccination and hesitancy is shown in Table 3.
Table 3. Search string for selected databases

The publication dates of interest were limited to the period between 1 January 1998 and 31 December 2020. The starting year was chosen as it was the year of publication of the now-retracted Andrew Wakefield’s article that linked measles, mumps and rubella (MMR) vaccine with the occurrence of autism and behavioural abnormalities in children (Wakefield et al., Reference Wakefield, Murch, Anthony, Linnell, Casson, Malik, Berelowitz, Dhillon, Thomson, Harvey and Valentine1998). The controversy fuelled the anti-vaccination movement (Balakrishnan, Reference Balakrishnan2019; Glasper, Reference Glasper2022). The initial search was conducted from 31 December 2020 to 21 January 2021. The search process and resulting analysis followed the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-analyses) approach (Page et al., Reference Page, McKenzie, Bossuyt, Boutron, Hoffmann, Mulrow, Shamseer, Tetzlaff, Akl, Brennan and Chou2021).
After the removal of duplicates, the remaining articles were screened by title and abstract. Articles were then excluded using a set of exclusion criteria (Table 4). As this review focused on parental childhood VH with vaccine uptake and vaccination intention being relevant outcomes, articles were excluded for the following reasons: not addressing human vaccines; studies that measured hesitancy indicators on vaccines unrelated to childhood immunisation including adolescent vaccines (Human papillomavirus, Diphtheria-Tetanus-Pertussis booster) and adult vaccines (herpes zoster vaccine); studies not related to determinants of general VH (eg, studies about vaccine efficacy); studies with determinants not linked to a behavioural outcome; modelling studies and intervention studies. Studies without full texts were also excluded. Preprints, grey literature, including dissertations/theses, government publications and articles on mandates were excluded, as these are not peer-reviewed. Other systematic reviews, meta-analysis and review articles were excluded to avoid duplication of studies. Only articles written in English were considered.
Table 4. Exclusion criteria

Filters were provided by most databases for elements of the exclusion criteria, including publication dates (1998–2020), language (English), and type of publication (peer-reviewed journal article). These filters were used during the initial search, when applicable.
Data extraction
Included studies were coded by publication year, country, WHO region, vaccine, outcome variable (intention or behaviour), and population, among other variables. The predictors of childhood vaccine uptake or intention (P-value <0.05) as well as the prevalence rates of parental childhood VH were extracted from the selected studies and documented.
Quality assessment
To assess the quality of included studies, the Joanna Briggs Institute (JBI) critical appraisal checklist for studies reporting prevalence data was used (Munn et al., Reference Munn, Moola, Lisy, Riitano and Tufanaru2015) (see Supplementary Material 1). This is a standard, recommended and widely used tool with a higher methodological rigour compared to other appraisal methods (Ma et al., Reference Ma, Wang, Yang, Huang, Weng and Zeng2020; Migliavacaa et al., Reference Migliavacaa, Stein, Colpanib, Munn and Falavignaa2020). The 34 included studies met all the JBI criteria.
Data synthesis
Thematic analysis was used for the synthesis, analysis, and interpretation of the patterns of meanings, attributes, and findings from the selected quantitative studies (Braun & Clarke, Reference Braun and Clarke2006; Guest et al., Reference Guest, MacQueen and Namey2012). A meta-analysis of numerical data was considered inappropriate for this review as the included studies are heterogeneous, clinically diverse, with different metrics or outcomes evaluated, and as such too dissimilar to combine the results (Higgins et al., Reference Higgins, Thomas, Chandler, Cumpston, Li, Page and Welch2021).
Results
Identified literature
In total, 335 262 records (all languages) were identified from the databases using the search strategy previously described (Table 2). An additional 1734 articles were added from other sources (relevant internet sites including Google Scholar and WHO’s Global Literature on Coronavirus Disease, and studies obtained from manual search of the reference lists of the included studies, as well as the cited references). After the removal of duplicates, 335 842 records were shortlisted for screening by title and abstract (Figure 3). A total of 276 474 papers were removed according to the exclusion criteria (Table 4). In all, 37 914 articles were eligible for the full-text assessment. After full-text analysis, 37 880 articles were removed. The remaining articles were considered for descriptive analysis and synthesis (n = 34).

Fig. 3. PRISMA flow diagram
A total of 30 articles assessed the prevalence of parental childhood VH in various populations, while four evaluated the intention of parents to vaccinate their children against VPDs (see Supplementary Material 2).
Descriptive analysis of articles
Study setting, design, and sampling
Relevant research about VH was found across all WHO regions. Twelve articles in the current review present findings from the Americas (USA, Canada, Guatemala). From 1998, nine studies came from Europe (Italy, France, UK, Netherlands, Slovenia, Kyrgyzstan), five from Western Pacific (Malaysia, China), two from East Mediterranean (Pakistan, Saudi Arabia), one from South-East Asia (India), one from Africa (Ghana), and four from cross-national comparisons of countries across different regions. Only two studies were conducted in the UK (two further studies included participants from the UK).
The majority of articles present data derived from cross-sectional (72.5%; n = 29) study designs. Longitudinal (n = 2) and mixed methods (n = 3) made up the remaining 15% of study designs used by the selected studies. The articles covered diverse ethnic backgrounds of sample populations. Nearly half (15/34) of the studies examined a multi-ethnic sample. Nineteen studies reported no information on race/ethnicity.
There was an increase in research on parental childhood VH across all WHO regions over the period 1998–2020. There was particular interest shown in pandemic influenza and seasonal influenza vaccines and the newly introduced COVID-19 vaccines. The main outcome variable in most studies (30/34) was actual vaccine behaviour, while the intention to vaccinate against COVID-19 or any new VPD was assessed in 4 of the 34 studies. Childhood vaccines remained a primary focus in Africa, South-Eastern Asia, and East Mediterranean regions. Studies from the Americas, Europe, and Western Pacific considered all age groups, with a tendency to shift to adolescent and adult vaccines. The introduction of COVID-19 vaccines oversaw an increase in published literature on VH with a shift in focus to the adult population. This research boost reflects the extent of the challenges surrounding uptake of the COVID-19 vaccines and the broader implications for vaccine confidence (Bell et al., Reference Bell, Clarke, Mounier-Jack, Walker and Paterson2020; Goldman et al., Reference Goldman, Yan, Seiler, Cotanda, Brown, Klein, Hoeffe, Gelernter, Hall, Davis and Griffiths2020).
Focus on specific vaccines
The majority of the selected studies (24/34) considered vaccines in general and were not focused on a specific vaccine. Studies that were specific to one vaccine looked at influenza, MMR, or COVID-19 vaccine, and this was more common in the Americas, Europe, and South-East Asia. Of the 34 articles reviewed, parents or primary caregivers were the focal point, offering their perspectives on the factors influencing their intention to recommend vaccines.
Use of theoretical models
Only a few of the studies expanded the field of VH research using novel approaches drawn from the core concepts of social cognitive models. For example, a cross-sectional study in the Netherlands was conducted to determine parental attitudes towards future childhood immunisations (Hak et al., Reference Hak, Schönbeck, De Melker, Van Essen and Sanders2005). Guided by the Health Belief Model (HBM), the authors developed a questionnaire for distribution to 800 highly educated parents of children <5 years of age attending day-care centres. With a response rate of 35% and less than half (46%) of participants expressing desire to vaccinate their children against diseases, this study highlighted the need for continuous health education to ensure the success of vaccination programmes. The low predictive capability of HBM variables was evident in this research, given the lack of depth of the questions used to assess and predict behaviour change among the respondents. For example, while questions related to perceived barriers and perceived benefits were strong predictors, questions about perceived severity were weakly correlated.
In Canada, Dubé et al. (Reference Dubé, Gagnon, Ouakki, Bettinger, Witteman, MacDonald, Fisher, Saini and Greyson2018) explored VH among parents and examined factors associated with their intention to vaccinate their children. Informed by the Theory of Planned Behaviour (TPB), this cross-sectional study assessed the relationships between knowledge, attitudes, and beliefs of 2013 parents and their intention to present their children for future vaccinations. Despite the importance of this study, the applied model did not comprehensively cover the influence of broader contextual factors. Even the authors acknowledged that ‘…the predictive power of TPB could be further increased by integrating concepts of risk perception, past behaviour, knowledge, and experience into the model’ (Dubé et al., Reference Dubé, Gagnon, Ouakki, Bettinger, Witteman, MacDonald, Fisher, Saini and Greyson2018:547).
A more recent cross-sectional study in China evaluated parental VH and identified risk factors associated with the intention of mothers to vaccinate their children (Hu et al., Reference Hu, Chen, Wang and Liang2019). Of the 770 mothers of children aged 24–35 months surveyed in Zhejiang province, 79.6% had positive attitudes towards vaccination. Like the Canadian study, this research used the TPB constructs to predict behaviour change among the sample population, and thus had similar shortcomings.
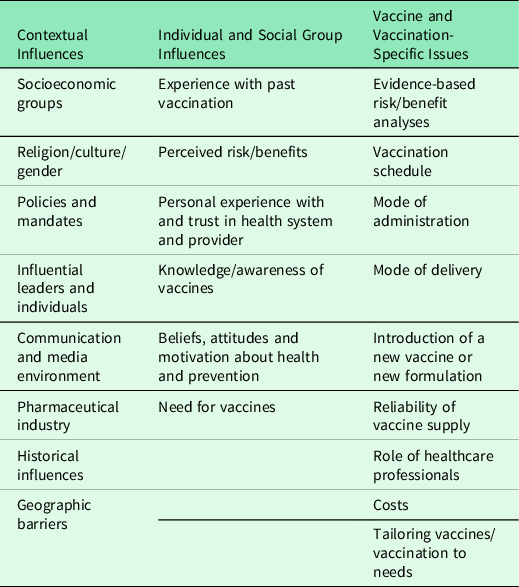
Analysis of factors (determinants of VH)
The 34 studies recognised the complex nature of VH, evidenced by the range of factors identified as determinants of vaccination behaviour (Table 5). These factors clustered around the core concepts of commonly used social cognitive models such as the HBM, Theory of Reasoned Action, TPB, Social Cognitive Theory, Health Action Process Approach, and the PMT. With respect to the objectives of this review, these findings validate the determinants of VH outlined in the SAGE WG model (MacDonald, Reference MacDonald2015). These themes will be adopted for the analysis of factors identified in the selected studies.
Table 5. Determinants of vaccine hesitancy

Contextual influences
Socioeconomic Factors
Socioeconomic status (SES) was recognised as a significant determinant of VH in nine of the included studies. In Netherlands (Hak et al., Reference Hak, Schönbeck, De Melker, Van Essen and Sanders2005), Malaysia (Azizi et al., Reference Azizi, Kew and Moy2017), France (Bocquier et al., Reference Bocquier, Fressard and Cortaredona2018), and China (Hu et al., Reference Hu, Chen, Wang and Liang2019), low SES was identified as a promoter/enabler of vaccination, while high SES was found to be a barrier. Another study in Malaysia (Kalok et al., Reference Kalok, Loh, Chew, Aziz, Shah, Ahmad, Ismail and Mahdy2020) indicated low SES as a barrier to vaccination, whereas high SES was considered a promoter. This finding was corroborated by studies in India (Dasgupta et al., Reference Dasgupta, Bhattacherjee, Mukherjee and Dasgupta2018) and Pakistan (Khattak et al., Reference Khattak, Rehman, Shahzad, Arif, Ullah, Kibria, Arshad, Afaq, Ibrahimzai and ul Haq2021). In China, although caregivers with high SES accepted vaccines with doubts, they did not delay or refuse vaccines for their children (Fanxing et al., Reference Fanxing, Chantler, Francis, Sun, Zhang, Han, Rodewald, Yu, Tu, Larson and Hou2020). The varying results obtained by different studies reflect the multidimensional nature of VH, especially in the context of socioeconomic and health disparities existing among nations (Bocquier et al., Reference Bocquier, Fressard and Cortaredona2018). Thus, it would be counterproductive to consider individual factors in isolation as multiple influences are at play (Larson et al., Reference Larson, Jarrett, Schulz, Chaudhuri, Zhou, Dube, Schuster, MacDonald and Wilson2015a; Larson et al., Reference Larson, Schulz, Tucker and Smith2015b).
Communication and media environment
The mass media remains a regular source of information about vaccination and vaccine-related issues. Constant exposure to vaccination stories could serve as a promoter of, or barrier to, vaccination (Larson et al., Reference Larson, Schulz, Tucker and Smith2015b). Previous studies in Nigeria (Antai, Reference Antai2009; Babalola & Lawan, Reference Babalola and Lawan2009; Babalola, Reference Babalola2011), India (Patra, Reference Patra2012), and Bangladesh (Rahman & Obaida-Nasrin, Reference Rahman and Obaida-Nasrin2010) highlighted the positive association between the media and the promotion of vaccination. In this review, however, negative news stories acted as a barrier to vaccination, as seen in studies from the UK (Campbell et al., Reference Campbell, Edwards, Letley, Bedford, Ramsay and Yarwood2017), Canada (Greenberg et al., Reference Greenberg, Dubé and Driedger2017; Dubé et al., Reference Dubé, Gagnon, Ouakki, Bettinger, Witteman, MacDonald, Fisher, Saini and Greyson2018), France (Bocquier et al., Reference Bocquier, Fressard and Cortaredona2018), Italy (Napolitano et al., Reference Napolitano, D’Alessandro and Angelillo2018; Bianco et al., Reference Bianco, Mascaro, Zucco and Pavia2019), Slovenia (Ucakar et al., Reference Učakar, Fafangel and Kraigher2018), Malaysia (Azizi et al., Reference Azizi, Kew and Moy2017; Musa et al., Reference Musa, Nordin, Cheong and Soni2019; Kalok et al., Reference Kalok, Loh, Chew, Aziz, Shah, Ahmad, Ismail and Mahdy2020), Pakistan (Khattak et al., Reference Khattak, Rehman, Shahzad, Arif, Ullah, Kibria, Arshad, Afaq, Ibrahimzai and ul Haq2021), Saudi Arabia (Alsubaie et al., Reference Alsubaie, Gosadi, Alsaadi, Albacker, Bawazir, Bin-Daud, Almanie, Alsaadi and Alzamil2019), and China (Hu et al., Reference Hu, Chen, Wang and Liang2019; Fanxing et al., Reference Fanxing, Chantler, Francis, Sun, Zhang, Han, Rodewald, Yu, Tu, Larson and Hou2020).
Trust in pharmaceutical companies
In nine of the included studies, parents had a mistrust of pharmaceutical industries, believing that economic interests influenced vaccination policy (Gilkey et al., Reference Gilkey, McRee, Magnus, Reiter, Dempsey and Brewer2016; Greenberg et al., Reference Greenberg, Dubé and Driedger2017; Bocquier et al., Reference Bocquier, Fressard and Cortaredona2018; Domek et al., Reference Domek, O’Leary, Bull, Bronsert, Contreras-Roldan, Ventura, Kempe and Asturias2018; Dubé et al., Reference Dubé, Gagnon, Ouakki, Bettinger, Witteman, MacDonald, Fisher, Saini and Greyson2018; Giambi et al., Reference Giambi, Fabiani, D’Ancona, Ferrara, Fiacchini, Gallo, Martinelli, Pascucci, Prato, Filia and Bella2018; Bianco et al., Reference Bianco, Mascaro, Zucco and Pavia2019; Alsubaie et al., Reference Alsubaie, Gosadi, Alsaadi, Albacker, Bawazir, Bin-Daud, Almanie, Alsaadi and Alzamil2019; Musa et al., Reference Musa, Nordin, Cheong and Soni2019). Parents felt the pharmaceutical sector should act in the public’s best interest. Lack of trust in pharmaceutical companies was thus considered a barrier to vaccination.
Parents questioning the intentions of pharmaceutical companies may result in weak public acceptance of vaccines (Alsubaie et al., Reference Alsubaie, Gosadi, Alsaadi, Albacker, Bawazir, Bin-Daud, Almanie, Alsaadi and Alzamil2019). Therefore, it is important to consider how parents view the pharmaceutical sector as a major factor in the mistrust that leads to vaccine refusal.
Individual and social group influences
Past experiences
Negative past experiences with vaccination services, such as side effects, poor continuity of care or lack of compassionate or comprehensive care, were significant predictors of VH among parents in twelve of the studies reviewed. These studies were split across the USA (Henrikson et al., Reference Henrikson, Anderson, Opel, Dunn, Marcuse and Grossman2017), Canada (Dubé et al., Reference Dubé, Gagnon, Ouakki, Bettinger, Witteman, MacDonald, Fisher, Saini and Greyson2018), Italy (Giambi et al., Reference Giambi, Fabiani, D’Ancona, Ferrara, Fiacchini, Gallo, Martinelli, Pascucci, Prato, Filia and Bella2018, Napolitano et al., Reference Napolitano, D’Alessandro and Angelillo2018), Bianco et al., Reference Bianco, Mascaro, Zucco and Pavia2019), China (Hu et al., Reference Hu, Chen, Wang and Liang2019; Fanxing et al., Reference Fanxing, Chantler, Francis, Sun, Zhang, Han, Rodewald, Yu, Tu, Larson and Hou2020), Malaysia (Musa et al., Reference Musa, Nordin, Cheong and Soni2019), and Ghana (Wallace et al., Reference Wallace, Wannemuehler, Bonsu, Wardle, Nyaku, Amponsah, Dadzie, Sarpong, Orenstein, Rosenberg and Omer2019). Three multinational studies also reported these findings (Bakhache et al., Reference Bakhache, Rodrigo, Davie, Ahuja, Sudovar, Crudup and Rose2013; Larson et al., Reference Larson, Schulz, Tucker and Smith2015b; Goldman et al., Reference Goldman, Yan, Seiler, Cotanda, Brown, Klein, Hoeffe, Gelernter, Hall, Davis and Griffiths2020).
Beliefs and attitudes
The importance of beliefs about vaccine safety and efficacy, and general attitudes and trust were noted by all 34 studies reviewed. These factors were significantly associated with the vaccination status of children. Having a positive attitude towards vaccination and a belief in the scientific efficacy of vaccines were identified as promoters of vaccination (Opel et al., Reference Opel, Taylor, Mangione-Smith, Solomon, Zhao, Catz and Martin2011b; Opel et al., Reference Opel, Taylor, Zhou, Catz, Myaing and Mangione-Smith2013; Strelitz et al., Reference Strelitz, Gritton, Klein, Bradford, Follmer, Zerr, Englund and Opel2015; Azizi et al., Reference Azizi, Kew and Moy2017; Campbell et al., Reference Campbell, Edwards, Letley, Bedford, Ramsay and Yarwood2017; Henrikson et al., Reference Henrikson, Anderson, Opel, Dunn, Marcuse and Grossman2017; Bocquier et al., Reference Bocquier, Fressard and Cortaredona2018; Dubé et al., Reference Dubé, Gagnon, Ouakki, Bettinger, Witteman, MacDonald, Fisher, Saini and Greyson2018; Napolitano et al., Reference Napolitano, D’Alessandro and Angelillo2018; Rachel et al., Reference Rachel, Minard, Guffey, Swaim, Opel and Boom2018; Bianco et al., Reference Bianco, Mascaro, Zucco and Pavia2019; Dubé et al., Reference Dubé, Farrands, Lemaitre, Boulianne, Sauvageau, Boucher, Tapiero, Quach, Ouakki, Gosselin and Gagnon2019; Musa et al., Reference Musa, Nordin, Cheong and Soni2019; Kalok et al., Reference Kalok, Loh, Chew, Aziz, Shah, Ahmad, Ismail and Mahdy2020). On the other hand, anti-vaccination behaviours, preference for alternative health approaches, and a belief in myths, rumours, or conspiracy theories acted as barriers to vaccination (Larson et al., Reference Larson, Schulz, Tucker and Smith2015b; Azizi et al., Reference Azizi, Kew and Moy2017; Greenberg et al., Reference Greenberg, Dubé and Driedger2017; Bocquier et al., Reference Bocquier, Fressard and Cortaredona2018; Dubé et al., Reference Dubé, Gagnon, Ouakki, Bettinger, Witteman, MacDonald, Fisher, Saini and Greyson2018; Napolitano et al., Reference Napolitano, D’Alessandro and Angelillo2018; Ucakar et al., Reference Učakar, Fafangel and Kraigher2018; Alsubaie et al., Reference Alsubaie, Gosadi, Alsaadi, Albacker, Bawazir, Bin-Daud, Almanie, Alsaadi and Alzamil2019; Bianco et al., Reference Bianco, Mascaro, Zucco and Pavia2019; Hu et al., Reference Hu, Chen, Wang and Liang2019; Musa et al., Reference Musa, Nordin, Cheong and Soni2019; Fanxing et al., Reference Fanxing, Chantler, Francis, Sun, Zhang, Han, Rodewald, Yu, Tu, Larson and Hou2020; Kalok et al., Reference Kalok, Loh, Chew, Aziz, Shah, Ahmad, Ismail and Mahdy2020; Khattak et al., Reference Khattak, Rehman, Shahzad, Arif, Ullah, Kibria, Arshad, Afaq, Ibrahimzai and ul Haq2021).
Knowledge and awareness
Knowledge about the severity of a disease and awareness of disease susceptibility were important determinants of the vaccination status of children in the UK (Campbell et al., Reference Campbell, Edwards, Letley, Bedford, Ramsay and Yarwood2017; Bell et al., Reference Bell, Clarke, Mounier-Jack, Walker and Paterson2020), USA (Opel Reference Opel, Taylor, Mangione-Smith, Solomon, Zhao, Catz and Martin2011b; Strelitz et al., Reference Strelitz, Gritton, Klein, Bradford, Follmer, Zerr, Englund and Opel2015; Henrikson et al., Reference Henrikson, Anderson, Opel, Dunn, Marcuse and Grossman2017), Canada (Greenberg et al., Reference Greenberg, Dubé and Driedger2017; Dubé et al., Reference Dubé, Farrands, Lemaitre, Boulianne, Sauvageau, Boucher, Tapiero, Quach, Ouakki, Gosselin and Gagnon2019), Italy (Napolitano et al., Reference Napolitano, D’Alessandro and Angelillo2018), Saudi Arabia (Alsubaie et al., Reference Alsubaie, Gosadi, Alsaadi, Albacker, Bawazir, Bin-Daud, Almanie, Alsaadi and Alzamil2019), Malaysia (Azizi et al., Reference Azizi, Kew and Moy2017; Musa et al., Reference Musa, Nordin, Cheong and Soni2019; Kalok et al., Reference Kalok, Loh, Chew, Aziz, Shah, Ahmad, Ismail and Mahdy2020), and Ghana (Wallace et al., Reference Wallace, Wannemuehler, Bonsu, Wardle, Nyaku, Amponsah, Dadzie, Sarpong, Orenstein, Rosenberg and Omer2019).
Risk-benefit perception (perceived threat vs perceived rewards)
Several studies (22/34) highlighted the influence that perceived risks and benefits have on vaccination behaviour. Eight of these studies came from the Americas (Opel et al., Reference Opel, Taylor, Mangione-Smith, Solomon, Zhao, Catz and Martin2011b; Frew et al., Reference Frew, Fisher, Basket, Chung, Schamel, Weiner, Mullen, Omer and Orenstein2016; Gilkey et al., Reference Gilkey, McRee, Magnus, Reiter, Dempsey and Brewer2016; Greenberg et al., Reference Greenberg, Dubé and Driedger2017; Rachel et al., Reference Rachel, Minard, Guffey, Swaim, Opel and Boom2018; Domek et al., Reference Domek, O’Leary, Bull, Bronsert, Contreras-Roldan, Ventura, Kempe and Asturias2018; Dubé et al., Reference Dubé, Gagnon, Ouakki, Bettinger, Witteman, MacDonald, Fisher, Saini and Greyson2018; Dubé et al., Reference Dubé, Farrands, Lemaitre, Boulianne, Sauvageau, Boucher, Tapiero, Quach, Ouakki, Gosselin and Gagnon2019), six from Europe (Hak et al., Reference Hak, Schönbeck, De Melker, Van Essen and Sanders2005; Akmatov et al., Reference Akmatov, Mikolajczyk, Kretzschmar and Kramer2009; Bocquier et al., Reference Bocquier, Fressard and Cortaredona2018; Napolitano et al., Reference Napolitano, D’Alessandro and Angelillo2018; Bianco et al., Reference Bianco, Mascaro, Zucco and Pavia2019; Bell et al., Reference Bell, Clarke, Mounier-Jack, Walker and Paterson2020), four from Western Pacific (Azizi et al., Reference Azizi, Kew and Moy2017; Hu et al., Reference Hu, Chen, Wang and Liang2019; Musa et al., Reference Musa, Nordin, Cheong and Soni2019; Fanxing et al., Reference Fanxing, Chantler, Francis, Sun, Zhang, Han, Rodewald, Yu, Tu, Larson and Hou2020), two from East Mediterranean (Alsubaie et al., Reference Alsubaie, Gosadi, Alsaadi, Albacker, Bawazir, Bin-Daud, Almanie, Alsaadi and Alzamil2019; Khattak et al., Reference Khattak, Rehman, Shahzad, Arif, Ullah, Kibria, Arshad, Afaq, Ibrahimzai and ul Haq2021), one from Southeast Asia (Dasgupta et al., Reference Dasgupta, Bhattacherjee, Mukherjee and Dasgupta2018), and one from Africa (Wallace et al., Reference Wallace, Wannemuehler, Bonsu, Wardle, Nyaku, Amponsah, Dadzie, Sarpong, Orenstein, Rosenberg and Omer2019). Parents who intend to have their children vaccinated had a lower perceived risk of vaccination and vice versa. If parents perceive the risk of a VPD to be lower than the risk from vaccines, they are likely to doubt the relevance of the vaccines and become vaccine-hesitant. These determinants are in line with the Threat Appraisal Pathway of the PMT: Perceived Threat (Severity, Vulnerability), and Perceived Rewards (Intrinsic Rewards, Extrinsic Rewards).
Vaccination as a social norm
Vaccine uptake was influenced by the presence of peers or relatives that are in support of vaccination, as reflected in studies carried out in the USA (Rachel et al., Reference Rachel, Minard, Guffey, Swaim, Opel and Boom2018; Henrikson et al., Reference Henrikson, Anderson, Opel, Dunn, Marcuse and Grossman2017), Canada (Dubé et al., Reference Dubé, Gagnon, Ouakki, Bettinger, Witteman, MacDonald, Fisher, Saini and Greyson2018), Italy (Bianco et al., Reference Bianco, Mascaro, Zucco and Pavia2019), Netherlands (Hak et al., Reference Hak, Schönbeck, De Melker, Van Essen and Sanders2005), Malaysia (Musa et al., Reference Musa, Nordin, Cheong and Soni2019; Kalok et al., Reference Kalok, Loh, Chew, Aziz, Shah, Ahmad, Ismail and Mahdy2020), and Ghana (Wallace et al., Reference Wallace, Wannemuehler, Bonsu, Wardle, Nyaku, Amponsah, Dadzie, Sarpong, Orenstein, Rosenberg and Omer2019). These studies found that parents who view immunisation as a social responsibility and consider the importance of herd immunity are less likely to be vaccine-hesitant. The need to protect others from harm is a behavioural outcome reflected in the Coping Appraisal Pathway of the PMT.
Vaccine and vaccination-specific issues
Accessibility
Time, distance, and cost (including cost of transport to a vaccine provider and the cost of self-paid vaccines) were identified as barriers to vaccination in five of the studies reviewed (Larson et al., Reference Larson, Schulz, Tucker and Smith2015b; Dasgupta et al., Reference Dasgupta, Bhattacherjee, Mukherjee and Dasgupta2018; Domek et al., Reference Domek, O’Leary, Bull, Bronsert, Contreras-Roldan, Ventura, Kempe and Asturias2018; Musa et al., Reference Musa, Nordin, Cheong and Soni2019; Fanxing et al., Reference Fanxing, Chantler, Francis, Sun, Zhang, Han, Rodewald, Yu, Tu, Larson and Hou2020). In Guatemala (Domek et al., Reference Domek, O’Leary, Bull, Bronsert, Contreras-Roldan, Ventura, Kempe and Asturias2018), perceived cost (another component of the Coping Appraisal Pathway of the PMT) was more important in urban areas than rural areas. Only in Pakistan (Khattak et al., Reference Khattak, Rehman, Shahzad, Arif, Ullah, Kibria, Arshad, Afaq, Ibrahimzai and ul Haq2021) did time, distance to clinic and cost not deter parents from accessing vaccination services.
Introduction to a new vaccine
Parental concern about new vaccines carrying more risk than older vaccines had a negative association with the intention to vaccinate in the USA (Allred et al., Reference Allred, Shaw, Santibanez, Rickert and Santoli2005), Netherlands (Hak et al., Reference Hak, Schönbeck, De Melker, Van Essen and Sanders2005), Italy (Giambi et al., Reference Giambi, Fabiani, D’Ancona, Ferrara, Fiacchini, Gallo, Martinelli, Pascucci, Prato, Filia and Bella2018), Guatemala (Domek et al., Reference Domek, O’Leary, Bull, Bronsert, Contreras-Roldan, Ventura, Kempe and Asturias2018), Malaysia (Musa et al., Reference Musa, Nordin, Cheong and Soni2019), India (Dasgupta et al., Reference Dasgupta, Bhattacherjee, Mukherjee and Dasgupta2018), Saudi Arabia (Alsubaie et al., Reference Alsubaie, Gosadi, Alsaadi, Albacker, Bawazir, Bin-Daud, Almanie, Alsaadi and Alzamil2019), and Pakistan (Khattak et al., Reference Khattak, Rehman, Shahzad, Arif, Ullah, Kibria, Arshad, Afaq, Ibrahimzai and ul Haq2021). However, a multinational survey of seven countries (UK, Canada, Australia, France, Spain, Germany, and Sweden) reported that parents would welcome the introduction of new vaccines, even if it requires additional clinic visits or coadministration with current vaccines (Bakhache et al., Reference Bakhache, Rodrigo, Davie, Ahuja, Sudovar, Crudup and Rose2013).
Role of healthcare professionals
All 34 studies acknowledged that advice or recommendation from health professionals could be an important determinant of vaccine acceptance. Parents who do not trust healthcare personnel or have little faith in the health system are more likely to be vaccine-hesitant. The studies suggest the need for healthcare providers to use their privileged position to address parental concerns about vaccinations, as this could influence the decision-making process.
Discussion
For the period under review (1998–2020), relevant studies about VH were found across all WHO regions, with the majority from the Americas and Europe. This does not necessarily suggest an increased prevalence of VH and issues related to vaccine acceptance in these regions, as focus may not be on vaccination, but on treatment of VPDs (eg, influenza, measles, mumps, varicella, pertussis, and meningococcal disease). However, as most of the world’s population lives in other regions, it is difficult to make inferences about the scarcity of available research in those parts.
Several determinants of VH were identified by the studies included in this review. No single algorithm was applicable to all studies as each factor was independent and varied across time, place, and vaccines, reflecting the complex interplay of other variables and the context-specific nature of VH (Clark & Sanderson, Reference Clark and Sanderson2009; Larson et al., Reference Larson, Jarrett, Schulz, Chaudhuri, Zhou, Dube, Schuster, MacDonald and Wilson2015a, Reference Larson, Schulz, Tucker and Smith2015b). Even in parts of the world where research was readily available, only few studies examined the different levels of interactions that exist between factors influencing VH. Different research methods were applied, and most of the studies were cross-sectional, thus making it difficult to draw conclusions about the influence of single or multiple determinants of vaccine acceptance at the individual or collective level. Future research should consider qualitative studies to help fill these gaps and contribute to existing knowledge and understanding of the many factors that influence parental decision-making.
The quantitative studies considered in this review examined the determinants of vaccine acceptance such as lack of vaccination awareness, fear of side effects, mistrust in the healthcare system and health professionals, poor perception of vaccine value, and negative past experiences with vaccine services, among others. However, it is difficult to make inferences about the relative strength of influence of these determinants because the studies were rarely based on theoretical models. While these findings do not rule out the significance of identified factors, they do highlight the shortcomings in such approaches.
Most studies showed that sociodemographic factors are important drivers of VH. It is crucial to emphasise, however, that most sociodemographic factors play a minor role in explaining individual VH. In the sociodemographic variables section, for example, inconsistent results were commonly reported. Furthermore, sociodemographic characteristics are at best a collection of plausible causes and can never fully define a particular behaviour without additional analysis (Schmid et al., Reference Schmid, Rauber, Betsch, Lidolt and Denker2017). Several studies, for example, suggested a link between a study population’s race/ethnicity, sex distribution, and vaccination intention (Allred et al., Reference Allred, Shaw, Santibanez, Rickert and Santoli2005; Strelitz et al., Reference Strelitz, Gritton, Klein, Bradford, Follmer, Zerr, Englund and Opel2015; Gilkey et al., Reference Gilkey, McRee, Magnus, Reiter, Dempsey and Brewer2016; Musa et al., Reference Musa, Nordin, Cheong and Soni2019; Bell et al., Reference Bell, Clarke, Mounier-Jack, Walker and Paterson2020; Kalok et al., Reference Kalok, Loh, Chew, Aziz, Shah, Ahmad, Ismail and Mahdy2020; Khattak et al., Reference Khattak, Rehman, Shahzad, Arif, Ullah, Kibria, Arshad, Afaq, Ibrahimzai and ul Haq2021). These associations could be accounted for by other factors such as family size (Luyten et al., Reference Luyten, Bruyneel and van Hoek2019), access to healthcare facilities (Lockyer et al., Reference Lockyer, Islam, Rahman, Dickerson, Pickett, Sheldon, Wright, McEachan and Sheard2021), healthcare provider discrimination (Woolf et al., Reference Woolf, McManus, Martin, Nellums, Guyatt, Melbourne, Bryant, Gogoi, Wobi, Al-Oraibi and Hassan2021), misinformation on social media (Broadbent, Reference Broadbent2019), trust in government and/or health authorities (Trent et al., Reference Trent, Seale, Chughtai, Salmon and MacIntyre2022), attitudes towards vaccination (Gravelle et al., Reference Gravelle, Phillips, Reifler and Scotto2022), and the fear of vaccine side effects (Karafillakis et al., Reference Karafillakis, Dinca, Apfel, Cecconi, Wűrz, Takacs, Suk, Celentano, Kramarz and Larson2016). As a result, sociodemographic variables such as ethnicity, race, and gender are only carrier variables, not explanatory variables (Schmid et al., Reference Schmid, Rauber, Betsch, Lidolt and Denker2017). This suggests that these variables could be confounders of the variables that actually cause VH. While such factors may be associated with VH, they cannot explain the development or severity of the situation. Most significantly, they are unhelpful in informing decisions to overcome hesitancy if psychological determinants are ignored. While these carrier variables may be useful in identifying target groups for intervention programmes, they should not be used to design the intervention (Schmid et al., Reference Schmid, Rauber, Betsch, Lidolt and Denker2017).
Across the target demographics, all the explanations for not being vaccinated as stated by the 5C model were recognised as major barriers to vaccine acceptance. Constraints and calculation, however, were less significant drivers. For pandemic influenza, the most common reasons for apprehension were a loss of faith in authorities and a diminished perception of the vaccine’s safety, as well as complacency, largely caused by low perceived risk and fear about the infection. The most common causes of VH for seasonal influenza vaccination were a lack of faith in authority, low vaccine effectiveness, low vaccine safety perceptions, vaccine misconceptions, and a negative attitude toward vaccines. A loss of confidence due to low perceived vaccination efficacy was commonly noted for both flu strains. COVID-19 immunisation intention was most significantly linked to confidence and collective responsibility.
The benefits of using the 5C model to design interventions can be seen in the distinctions between disease types in terms of their psychological profile of vaccine denial in target populations. The model serves as a framework for identifying, developing, and implementing effective solutions to the VH crisis (Betsch et al., Reference Betsch, Böhm and Chapman2015). If one wants to enhance COVID-19 vaccine uptake in the hospital environment, for example, the findings of this review show that tackling confidence issues (by dispelling myths and making people understand the ethical and professional need to get vaccinated) is a viable mechanism. Low confidence has been demonstrated to respond well to informational interventions such as instructional initiatives (Betsch et al., Reference Betsch, Böhm and Chapman2015). It has also been demonstrated that structural interventions such as compulsory vaccinations, which are effective in overcoming complacency, should be approached with caution, as negative attitudes regarding immunisation are substantial obstacles that can lead to reactance after structural intervention efforts (Betsch et al., Reference Betsch, Böhm and Chapman2015). When the findings of this systematic review are integrated with conceptual frameworks such as the 5C model, important revelations about modifiable behaviours can emerge.
Campaigns aimed at raising parental vaccination intention would most likely be effective if they emphasise building confidence and collective responsibility while reducing complacency. Other factors, such as constraints and calculation, had smaller negative correlations with vaccination intention. When developing solutions, the psychological characteristics that underpin these motivations should be considered. Vaccination intention is influenced by variations in levels of confidence, which are driven by the perceived risk and safety profiles of vaccines. Because parents who believe vaccines have greater risks than benefits have lower levels of confidence, the importance of faith in the government and health officials in clarifying vaccine intentions is vital. Parents that have less faith in these institutions have lower confidence levels, which leads to a lower intention to get vaccinated. Vaccination intention is also influenced by the extent to which family members and friends express their need to get vaccinated.
Complacency sets in when the perceived dangers of VPDs are low, and vaccination is not considered an essential preventive measure (MacDonald, Reference MacDonald2015). Individuals who are unconcerned about communicable diseases do not feel threatened by them and hence do not feel compelled to change their preventative habits (Schwarzer & Fuchs, Reference Schwarzer and Fuchs1996). Because of the low level of involvement, the affected people do not see the need to actively seek information and increase their knowledge and awareness of prevailing issues (Fischer et al., Reference Fischer, Kastenmüller, Greitemeyer, Fischer, Frey and Crelley2011). Preventive behaviour is also not perceived as a descriptive or injunctive norm in society; therefore, it is regarded as separate from subjective norms (Askelson et al., Reference Askelson, Campo, Lowe, Smith, Dennis and Andsager2010). However, complacency should be linked to a poor perception of disease risks (Brewer et al., Reference Brewer, Cuite, Herrington and Weinstein2007).
Because prevention is a future-oriented behaviour, it is expected to have a negative relationship with the consideration of future repercussions (Petrocelli, Reference Petrocelli2003). Individuals with a high level of complacency should also have a favourable risk perception, showing a propensity for risk-taking behaviours, because future repercussions are irrelevant (Johnson et al., Reference Johnson, Wilke and Weber2004). This may be linked to perceptions of invulnerability as well as a positive subjective personal health status (Lapsley & Hill, Reference Lapsley and Hill2010).
Parents who believe the risk of VPDs in their surroundings is minimal have a decreased intention to vaccinate their children, owing to a reduced desire to safeguard others. Furthermore, personality plays a key role in understanding how vaccination is viewed as a social responsibility. Psychopathic qualities, which are linked to antisocial behaviour caused by a lack of empathy, emotion, and self-control (Jones & Paulhus, Reference Jones and Paulhus2014), have a negative relationship with collective responsibility and, as a result, with vaccination intentions. Likewise, parents with more humane characteristics, such as those who feel greater sympathy for others and wish to help those in need, have a stronger intention to vaccinate their children because they have a larger sense of community duty.
Research suggests that attempting to boost both confidence and collective responsibility at the same time will be beneficial, as interventions that target multiple underlying factors have proved to be more effective (Frew & Lutz, Reference Frew and Lutz2017). The results of this study suggest that is critical to target vaccine safety and efficacy when addressing confidence. Concerns regarding safety, vaccine side effects, speed of development, and the desire for the vaccine to be shown efficient and safe over a longer period were the most common reasons given in this review for COVID-19 VH. Confidence levels in the vaccine can be boosted by debunking myths about the vaccine and offering real information on issues such as why the vaccine was produced so quickly, for example. Nevertheless, it is critical to consider the way this information is communicated, and the personnel involved, because a correction of information could backfire and lead to even more polarised sentiments among those who already have strong opinions (Glaeser & Sunstein, Reference Glaeser and Sunstein2014). Because in this study, poor confidence was linked to a distrust of government and healthcare agencies, safety, and efficacy information should best be presented by people who are not in typical positions of authority. A viable approach would be to use people who are considered as reputable by the target audience but are not expected to give this knowledge (Glaeser & Sunstein, Reference Glaeser and Sunstein2014). Campaigns involving peers or celebrities, for example, could be used to reach parents.
In this study, parents’ collective responsibility was shown to significantly predict COVID-19 vaccine uptake. The potential threat of COVID-19 for other family members in a household environment indirectly influences parental vaccination intention. The presence of family members who are susceptible to COVID-19, such as those with underlying medical conditions, could motivate parents to get their children vaccinated, thus safeguarding the people around them. Vaccination programmes focused on parents may thus be more effective if they highlight the hazards to individuals in the immediate vicinity of the parents. Vaccination is an effective way to explain what herd immunity is about (Betsch et al., Reference Betsch, Böhm, Korn and Holtmann2017). When deciding whether to vaccinate their children, parents can and should be made aware that they are making a collective decision, not simply an individual one. To raise awareness, campaigns could address the reasons why certain people cannot get vaccinated (eg, those who have had an adverse reaction to immunisations, have autoimmune diseases, or have other illnesses).
Because parents with less altruistic, assertive, and gregarious personalities are less likely to feel communal responsibility, it will be difficult, if not impossible, to influence these personality traits. However, because these parents have less empathy for others, campaigns emphasising the vaccine’s prosocial effects may not be enough to sway certain groups and may even compound the free-rider problem (Ibuka et al., Reference Ibuka, Li, Vietri, Chapman and Galvani2014). As a result, it is critical to keep expressing the personal hazards of COVID-19 to parents, such as the possibility of long-term negative effects of COVID-19 (Mahase, Reference Mahase2020).
Descriptive norms can influence vaccination intention indirectly through confidence and complacency, just as they can influence the decision-making process directly. These norms have been shown to be powerful motivators of behaviour, particularly in uncertain times (Cialdini, Reference Cialdini2009). Vaccination campaigns may be more effective if they emphasise the importance of vaccination among parents by emphasising that most families plan to get vaccinated.
When family members have already been vaccinated, the level of collective responsibility may be reduced due to a lower perceived risk of VPDs for others. As a result, it is critical that parent-focused efforts begin early on, when the importance of vaccination is most apparent, and thus, positive attitudes can be formed. According to studies, once a sufficient decision has been made to get vaccinated, it is more likely to be followed through (Auslander et al., Reference Auslander, Meers, Short, Zimet and Rosenthal2019). In terms of policy, the process of getting vaccinated should be simple, quick, and free of avoidable constraints to accelerate the shift from intention to behaviour (DaCosta DiBonaventura & Chapman, Reference DaCosta DiBonaventura and Chapman2005).
Limitations, directions for future research, and conclusions
Limitations
Rather than obtaining a comparison of the individual determinants of vaccine acceptance, this systematic review analysed the spectrum of parental childhood VH and its drivers. Studies that investigated the different barriers but found no significant connections are not reported or considered since they were outside the scope of the research. A meta-analytic technique is required to assess the cumulative outcome measures of relevant barriers and their respective significance. However, meta-analytic approaches to addressing VH have significant challenges because the outcome measures are not frequently based on the constructs of theoretical models and their use varies widely among researchers.
Most of the VH studies were undertaken in the United States and Europe. All other jurisdictions were relatively poorly represented. Even though research for the target populations has increased in number over time, the number of studies focusing on children has remained comparatively low. As a result of the scarcity of data, the results of this review must be confined to the locations and populations that are accessible.
The review had other limitations, including the exclusion of databases that had articles not written in English, which may have affected the sensitivity of searches in other languages, and the exclusion of government publications and articles on mandates, which may have influenced findings around the impact of health policies and practices.
Notwithstanding the shortcomings, this research offers governments and public health experts the necessary tools for understanding the key drivers of vaccination behaviour and vaccination intention among parents. Considering the fluctuating rates of vaccine acceptance in the studies reviewed, it is hoped that the findings of this study will aid in the development and enhancement of public health interventions to improve vaccine compliance above the proportions required for herd immunity.
Directions for future research
Underserved regions where only limited studies were found on parental childhood VH and demographics (eg, parents of children aged 0–6 years) should be the focus of future studies. From the results of this research, the UK is one of those regions that requires further investigations. More research will provide further evidence to design interventions across the UK and all WHO regions and for all groups at risk of VPDs.
Studies should not only concentrate on regions and demographics but also on measurable outcomes. Psychological variables can help researchers further comprehend why some people reject vaccinations while others do not. These variables are not studied regularly. Psychological principles are rarely employed in the measurement of study outcomes, and the tools used to evaluate the constructs differ significantly between investigations. Furthermore, risk perception variables are hardly distinguished and used interchangeably throughout and even within articles.
Theory-based psychological scales should be adopted for use in research to obtain accurate results and allow the scientific community to compare findings across publications. This approach will ensure scientific advancement in the relatively new field of VH research and raise the standard of future investigations.
Conclusions
The emergence of VH has been central to the understanding of the wider concept of vaccine acceptance. This review showed that unfavourable dispositions towards vaccinations and behavioural attitudes such as a reduced perception of vaccine effectiveness and mistrust of health authorities were the most often cited barriers to vaccine uptake. Other evaluations include concerns about vaccine safety, low perceived severity of VPDs, and low perceived disease susceptibility.
Confidence and complacency, according to available evidence, are major determinants of VH. Anxiety, low perceived risk, and low disease severity were the most common signs of complacency. Doubts about vaccine safety and effectiveness, as well as lack of faith in health officials and the assumption that vaccines can cause the diseases they were meant to prevent, all contributed to a lack of confidence.
The constructs of relevant theoretical models have provided further context to the evolution of VH determinants, emphasising the need for parents and stakeholders to be actively engaged in the decision-making process from an early stage. It is clear, however, that additional information sources are needed to ensure these models adequately account for the influence of broader contextual factors, particularly in regions with limited peer-reviewed literature.
Theoretical approaches to quantifying VH will continue to strengthen the body of knowledge needed to develop successful evidence-based interventions. The efficacy of vaccine advocacy campaigns could be increased and the burden of VPDs could be lowered by adopting clinical, patient-centred techniques to measure and overcome VH. A combination of local, regional, and universally driven initiatives will be critical in the early detection of parental concerns.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1463423622000512
Acknowledgements
The authors thank all students and staff of the University of Sunderland.
Financial support
The authors received no funding or grant from any agency or body.
Conflict(s) of interest
None.