INTRODUCTION
Nearly 1 in 1,000 people every year will succumb to an out-of-hospital cardiac arrest (OHCA)Reference Priori, Aliot and Blomstrom-Lundqvist 1 , Reference Kette, Sbrojavacca and Rellini 2 with a mean survival rate at hospital discharge of about 7%.Reference Sasson, Rogers and Dahl 3 , Reference Berdowski, Berg and Tijssen 4 The chance of survival following OHCA depends on the “chain of survival”Reference Cummins, Ornato and Thies 5 concept as well as the steps taken in the first few minutes following the event. With better implementation of the links of this chain, cardiac arrest survival can be improved.Reference Daya, Schmicker and Zive 6 Early and high quality cardiopulmonary resuscitation (CPR) has been shown to greatly improve the survival rate of cardiac arrest victims,Reference Iwami, Kawamura and Hiraide 7 , Reference Rea, Eisenberg and Culley 8 as indicated by American Heart Association (AHA) guidelines changes from 2005 to date. 9 - Reference Kleinman, Brennan and Goldberger 11 For this reason, the 2015 Guidelines for Cardiopulmonary Resuscitation stress the importance of performing high quality CPR immediately after a cardiac arrest. Both laypersons and health care providers, in fact, are recommended to compress the adult chest at a rate of at least 100 compressions per minute (not exceeding 120) with a compression depth of at least 5 cm (not exceeding 6 cm); rescuers should also allow complete chest recoil after each compression and attempt to minimize frequency and duration of interruptions in compressions.Reference Kleinman, Brennan and Goldberger 11 , Reference Perkins, Handley and Koster 12 Many factors contribute to CPR quality: individual factors, training, awareness, technique, and rescuer fatigueReference Wik, Kramer-Johansen and Myklebust 13 ; however, data about laypersons’ CPR quality are scarce. Furthermore, the International Liaison Committee on Resuscitation (ILCOR) 2010 recommendations, in the education knowledge gaps section, underlined the lack of a specific technique to optimize chest recoil,Reference Mancini, Soar and Bhanji 14 and this point remained unsolved in ILCOR 2015 recommendations.Reference Bhanji, Finn and Lockey 15 Instructor assessment of chest compression quality during training has been demonstrated to be not accurate enough.Reference Brennan, McGraw and Brooks 16 For this reason, in the last few years, many types of CPR feedback devices have been developed, and their use has been demonstrated to increase the quality of health care providers’ CPR during both trainingReference Yeung, Meeks and Edelson 17 - Reference Buléon, Delaunay and Parienti 24 and in real-life cardiac arrest scenarios.Reference Kirkbright, Finn and Tohira 25 Recent evidence has also shown that real-time audiovisual feedback used during a real cardiac arrest increases the survival rate and the chances of a favourable outcome following OHCA.Reference Nolan 26 , Reference Bobrow, Vadeboncoeur and Stolz 27 Regarding laypersons, one study demonstrated that CPR quality is improved during the use of feedback devicesReference Buléon, Parienti and Halbout 28 ; however, there are only a few non-randomized studies regarding the use of such devices during laypersons’ training, and their results are controversial.Reference Krasteva, Jekova and Didon 29 - Reference Pavo, Goliasch and Nierscher 31 Moreover, the optimal duration of feedback device use is unknown.Reference Sutton, Donoghue and Myklebust 32 - Reference Lynch, Einspruch and Nichol 34 The aim of this study is to determine whether the use of a CPR feedback device improves laypersons’ CPR quality after the completion of a training course and, secondarily, to determine whether final quality is related to how long the feedback device is used in training.
METHODS
Study design
We performed a randomized, controlled manikin study. Regarding the blinding method, participants and instructors knew the time spent using a feedback device for each participant, but the instructors did not know which were the study endpoints and the statistical analysis were blinded (statisticians did not know which group they were analysing). We submitted the study to a regional ethics committee for medical research that considered it exempt from evaluation, in accordance with Italian law, because the study did not include the use of drugs or medical devices, and it was not directly related to health and illness of the participants. We obtained a written consent for study participation from all participants.
Study setting and population
The study was conducted at the two IRC-Comunità Training Centers of the nonprofit associations Pavia nel Cuore (Via de Canistris 7, Pavia, Italy) and Robbio nel Cuore (Via Mortara 5, Robbio, Pavia, Italy). Volunteers were recruited during our BLS/AED free courses; the courses were promoted by the local newspaper and on social networks (Facebook, Twitter). Laypersons over 18 years old with no previous training in CPR were eligible for randomization. Each participant was asked to supply demographic data (i.e., gender, age, weight, and height), and body mass index was also calculated for each participant. We informed all of the participants that we would have evaluated their performance for scientific purposes only. No identifying data were collected. Enrolment was conducted from March 2013 to September 2014, and a total of 450 participants were included in the study.
Study protocol
Participants were randomly divided into three groups (Group NF for no feedback, Group SF for short feedback, and Group LF for long feedback) with an allocation ratio of 1:1:1 with a randomization list created with Research Randomizer (Urbaniak G. C. & Plous S., Research Randomizer Version 4.0; www.randomizer.org) using permuted blocks of 6. A CONSORT diagram is displayed in Figure 1.
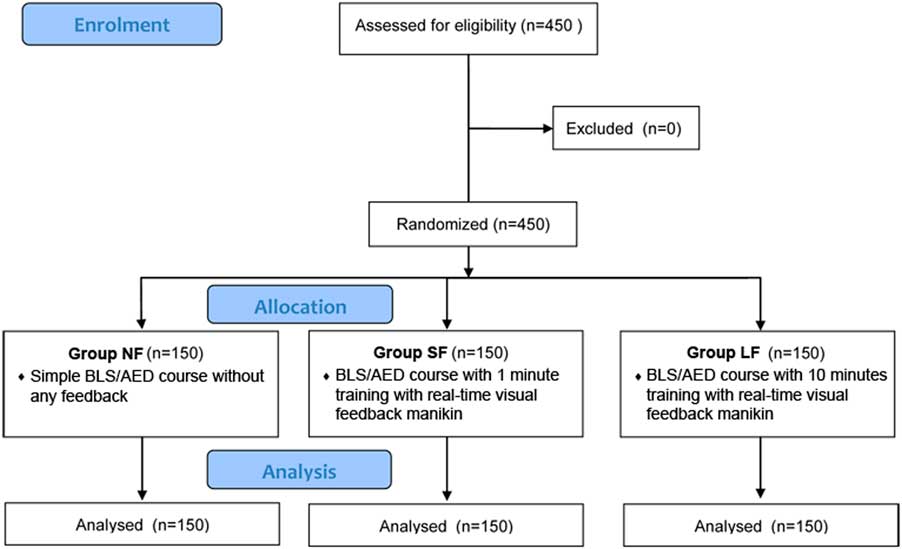
Figure 1 Flow chart of design and recruitment of participants according to 2010 CONSORT statement.
Each group attended one of three different types of 5-hour BLS/AED courses (Group NF attended Course NF, Group SF attended Course SF, and Group LF attended Course LF), and all performed according to the 2010 ILCOR recommendations. Every course consisted of 1 hour of theory and 4 hours of practice with an instructor:attendees:manikin ratio of 1:5:1 and maximum ratio of 1:6:1. The only difference among the courses was the amount of time spent training with feedback, in particular, as follows:
-
− Course NF: simple BLS/AED course without any feedback
-
− Course SF: BLS/AED course with 1 minute of training with real-time visual feedback manikin
-
− Course LF: BLS/AED course with 10 minutes of training with real-time visual feedback manikin
The manikin used for the three courses was Laerdal Little Anne (Laerdal Medical, Inc., AS, Norway). The real-time visual feedback on compression depth, compression rate, chest recoil, and the correct hand position was provided by the Resusci Anne Wireless SkillReporter software, version 1.1.0.20 (Laerdal Medical, Inc., AS, Norway) connected to the Laerdal Resusci Anne Wireless SkillReporter manikin (Laerdal Medical, Inc., AS, Norway), as shown in Figure 2. At the end of each course, we recorded 1 minute of compression-only CPR using the same software and the same manikin, without visual feedback for the attendee. We chose the duration of 1 minute to minimize the deterioration of chest compression quality as a result of fatigue, according to the results from Nishiyama et al.Reference Nishiyama, Iwami and Kawamura 35 To avoid any difference in results, as a result of using different manikins, Group NF and Group SF used the Resusci Anne Wireless SkillReporter manikin without any feedback for 10 and 9 minutes, respectively, during the course. This was done to ensure that all groups used this type of manikin for the same amount of time.
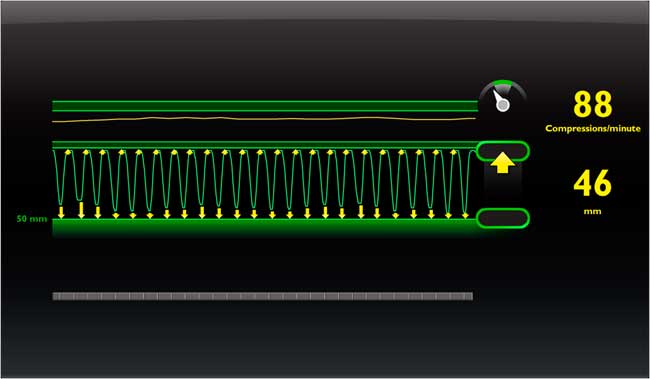
Figure 2 Screenshot representing the real-time visual given by the Resusci Anne Wireless SkillReporter software: the yellow arrows reveal inadequate depth or incomplete chest recoil, whilst, in the top, the compression rate is represented by both a number and a continuous line.
Measurements
For each participant, we analysed the percentage of compressions with correct depth (50 mm–60 mm), the percentage of correctly released compressions, the percentage of compressions with the correct hand position, the number of compressions, and the Total CPR Score. Total CPR Score is a comprehensive scoring algorithm developed by Laerdal in close collaboration with members of the AHA Emergency Cardiovascular Care Subcommittees and co-authors of the 2013 AHA Consensus Statement on CPR Quality. This score ranges from 0% to 100% and reflects the adherence to guidelines; the score decreases gradually as the performance deviates from the guidelines.
The primary end point was the difference in the percentage of compressions with correct depth (50 mm–60 mm) among the groups. Secondary end points were the differences in the percentage of correctly released compressions, in the percentage of compressions with correct hand position, in the compression rate, and in the Total CPR Score among the groups.
Data analysis
All data were entered in anonymous form into a database (Microsoft Excel 2010) and then analysed with SPSS 19.0 Windows version (SPSS Inc., Armonk, New York). We evaluated differences among the groups using the analysis of variance (ANOVA) with the Fisher’s least significant difference (LSD) correction for the post-hoc comparison. All continuous variables are expressed as means with their 95% confidence intervals. A p-value<0.05 was defined as statistically significant. The sample size calculation was based on the comparison of the primary end point in the three groups; we did not perform earlier studies that would have been useful as a basis for a sample size calculation; therefore, based on previous studies,Reference Field, Soar and Davies 36 - Reference Kramer-Johansen, Myklebust and Wik 38 we wanted to adequately detect a mean paired difference of 0.7 times the standard deviation. Based on an alpha=0.05 and a power of 80%, a sample size of 37 study participants per group was needed. The enrolment of the participants was easier than expected, and we had no logistic problems in increasing the number of our study population. Therefore, we decided to reach the number of 450 participants to improve the power of our study. We also performed an analysis on the first 37 laypersons enrolled for each group (111 participants) to verify whether our primary end point was satisfied finding a statistically significant difference in the percentage of compressions with correct depth (overall p=0.017). We performed all of the analyses shown in the results on the entire sample (n=450).
RESULTS
Demographic characteristics of the population
We compared the demographic variables of the three groups to verify whether there were any differences that could influence the results. As shown in Table 1, there were no differences among the three groups.
Table 1 Comparison of the demographic characteristics of the three groups
CI=confidence interval; LF=long feedback; NF=no feedback; SF=short feedback.
ANOVA among the groups and Fisher’s LSD post-hoc comparisons for the primary end point
We found a statistically significant difference among the three groups for the percentage of compressions with correct depth (overall p=0.012), for the percentage of compressions with complete chest recoil (overall p<0.001), for the percentage of compressions with correct hand position (overall p<0.001), and for Total CPR Score (overall p<0.001). We did not find any difference among the three groups for the compression rate (overall p=0.529). The Fisher’s LSD post-hoc comparisons among the three groups for the percentage of compressions with correct depth showed a statistically significant difference between groups NF and SF (p=0.005) and between groups NF and LF (p=0.022), but not between groups SF and LF (p=0.601) (Table 2).
Table 2 Comparison of the percentage of compressions with correct depth, the percentage of compressions with complete chest recoil, the percentage of compressions with correct hand position, the compression rate, and Total CPR Score among the groups
ANOVA=analysis of variance; CI=confidence interval; LF=long feedback; NF=no feedback; SF=short feedback.
a LSD corrected p-values are given.
DISCUSSION
Current evidences about the feedback devices
It has been well demonstrated that feedback devices improve health care providers’ CPR quality during both trainingReference Yeung, Meeks and Edelson 17 - Reference Buléon, Delaunay and Parienti 24 and in real-life scenarios.Reference Kirkbright, Finn and Tohira 25 ILCOR 2015 recommendations pointed out the importance of high-quality CPR performed not only by health care providers but also by laypersons, who are often the first bystanders in the setting of OHCA.Reference Bhanji, Finn and Lockey 15 However, teaching high-quality CPR to laypersons is often a considerable challenge for an emergency medical services (EMS) medical director and BLS/AED course instructor, probably mainly because laypersons have had no experience of CPR prior to the course. Moreover, as demonstrated by Brennan et al.,Reference Brennan, McGraw and Brooks 16 it is difficult for the instructors to be accurate during an assessment of chest compression quality, and feedback devices can serve as a helpful tool. In literature, studies regarding the use of feedback devices by laypersons are scarce, and their results are controversial. Krasteva et al.Reference Krasteva, Jekova and Didon 29 in 2011 and González-Salvado et al.Reference González-Salvado, Fernández-Méndez and Barcala-Furelos 30 in 2016 demonstrated that these devices can help improve the CPR performance of laypersons while training on a manikin; their results, however, were not confirmed by Pavo et al.Reference Pavo, Goliasch and Nierscher 31 who showed that human feedback and feedback by audiovisual devices are equal in effectiveness. Therefore, the utility of feedback devices over human feedback in teaching CPR to laypersons is currently unclear, and there are no randomized studies on this topic. Our present study describes an intervention that may improve the quality of CPR by layperson bystanders, which, in turn, may be a life-saving method for someone who experiences an OHCA.
Discussion of the study results
There was a statistically significant improvement in all of the parameters, except for compression rate, in the groups receiving real-time visual feedback during BLS/AED training compared to the group not receiving real-time visual feedback (see Table 2). Regarding compression rate, it is interesting to notice that it does not seem to be affected by the incorporation of real-time visual feedback because all of the groups, including the NF group, reached the compression rate suggested by the guidelines (i.e., between 100 and 120 per minute). It is possible that a standard BLS/AED course is sufficient to achieve the correct compression rate and that feedback is not necessary to improve this parameter. Our study showed no significant differences between Group SF and Group LF in all of the parameters. Regarding methodology, it is important to point out that only a small group of well-trained IRC-Comunità-certified BLS/AED instructors was involved in this study, and all of the BLS/AED courses were performed using the same methodology (i.e., same slides, same syllabus), in the same place (i.e., the headquarters of the two associations), and at the same time of the day (weekend mornings) to minimize any teaching bias. Furthermore, we chose the duration of 1 minute to verify CPR quality after the course because, according to our reference,Reference Nishiyama, Iwami and Kawamura 35 a longer duration (i.e., 4 minutes, which is the mean arrival time of BLS provider with AED in the United States) could tire the participants unnecessarily considering that the goal of the study was only to verify whether the use of feedback devices could improve CPR quality after a course. Given that the main difference among the courses was the use of feedback devices and how long they were used for, we infer that the differences in CPR performance among the three groups are the result of the real-time visual feedback. According to our results, we can also assume that just 1 minute per participant of real-time visual feedback is sufficient to improve CPR quality and, in the majority of the participants, to achieve the values established by the guidelines.
We think that many elements could be responsible for this improvement; real-time visual feedback allows laypersons not only to comprehend what the parameters established by the guidelines actually are, but also how to leverage their physical potential to achieve them. We also believe that participants could consider real-time visual feedback a challenge, motivating them to improve their performance and, therefore, reach the correct cut-off values. Moreover, one of our most interesting results is that this type of feedback considerably improves the percentage of compressions performed with complete chest recoil, filling in one of the knowledge gaps established by ILCOR 2010 recommendations,Reference Mancini, Soar and Bhanji 14 which remained unsolved in the ILCOR 2015 recommendations.Reference Bhanji, Finn and Lockey 15 Another point favouring these devices is that they are simple to use and that they do not require any specific skills other than those that a BLS/AED instructor already has besides basic knowledge of the software provided with the manikin.
In summary, our study is the largest randomized controlled manikin study regarding the use of real-time visual feedback during CPR training for laypersons carried out to date. Our results show that the use of such devices during BLS/AED courses improves the majority of measurable parameters of CPR and, therefore, the capability of laypersons to reach a high-quality CPR at the end of the course. This could have wide-ranging implications for EMS medical directors, BLS/AED course instructors, and coordinators involved in training laypersons in CPR who might consider to incorporate at least 1 minute of real-time visual feedback for all of the participants in their classes (if this technology is available) to help attendees achieve the goals emphasized by ILCOR 2015 recommendations.
Nonetheless, further investigations into the use of feedback in retraining and into the long-term efficacy of using such devices during CPR training are required. If further studies confirm that this CPR quality improvement is retained 6 months and 1 year after a course, this intervention could be a simple and inexpensive way to improve bystander chest compression quality, which subsequently may lead to an improvement in OHCA survival, if widely adopted.
STUDY LIMITATIONS
The principal limitation of this study is that it was conducted using manikins; there is no direct evidence that the use of real-time visual feedback during CPR courses for laypersons improves patient outcome after OHCA. Nonetheless, it has been proved that high-quality CPR improves the survival rate of cardiac arrest victims,Reference Iwami, Kawamura and Hiraide 7 and that training of health care providers with feedback devices improves survival rates after OHCA.Reference Truszewski, Szarpak and Kurowski 23 , Reference Buléon, Delaunay and Parienti 24 We can therefore assume that better training of laypersons using feedback devices may positively affect survival rates after OHCA.
Another weakness of our study is that we did not collect long-term follow-up data about the participants’ CPR quality over the subsequent weeks to months. Further investigations are required to estimate the permanence of the effect of such devices during CPR training.
CONCLUSION
The use of real-time visual feedback in BLS/AED courses for laypersons improves the CPR quality of the participants and their adherence to guidelines. In particular, 1 minute of real-time visual feedback seems to be sufficient for laypersons to reach a better CPR quality. Although further study is needed, it is reasonable to consider the use of feedback devices in all BLS/AED courses for laypersons.
Acknowledgements
We would like to thank all of the volunteers of the nonprofit associations Pavia nel Cuore and Robbio nel Cuore for their irreplaceable work in organizing BLS/AED courses for free. We offer a special thanks to Dr. Silvia Bassi, Dr. Gianluca Borio, Dr. Sara Fratino, and Dr. Gianpaolo Toscano for their help in data collection and to Ziggy Kennell for working on the English revision. Clinical trial registration information can be found at http://www.umin.ac.jp/ctr/ (Unique Identifier: UMIN000017851).
Competing interests: None declared.
SUPPLEMENTARY MATERIAL
To view supplementary material for this article, please visit http://dx.doi.org/10.1017/cem.2016.410