An informal caregiver is someone who provides unpaid care to another person, normally a family member or friend, who requires help due to physical or mental ill health, disability or problems associated with old age (Fowler, Reference Fowler2015; Settineri et al., Reference Settineri, Rizzo, Liotta and Mento2014). Studies of informal caregivers of people with dementia have demonstrated that this role can have a number of negative consequences, including burden, depression, anxiety, stress, irritability, poorer wellbeing and health, sleep disturbances, social isolation, and an increased risk of cardiovascular disease (Del-Pino-Casado & Ordóñez-Urbano, Reference del-Pino-Casado and Ordóñez-Urbano2016; Fowler, Reference Fowler2015; Pearlin et al., Reference Pearlin, Mullan, Semple and Skaf1990; Roepke et al., Reference Roepke, Allison, von Känel, Mausbach, Chattillion, Harmell, Patterson, Dimsdale, Mills, Ziegler, Ancoli-Israel and Grant2012; Zarit et al., Reference Zarit, Reever and Bach-Peterson1980). However, a smaller body of research suggests that being a caregiver can also bring some positive benefits (Kramer, Reference Kramer1997a; Rapp & Chao, Reference Rapp and Chao2000). Rapp and Chao (Reference Rapp and Chao2000), for instance, found that some informal caregivers reported a sense of personal growth and satisfaction, the learning of new skills, and an improved relationship with the care recipient and/or with others. Similarly, Cohen et al. (Reference Cohen, Colantonio and Vernich2002) noted that most caregivers were able to identify at least one positive aspect of their role, the most commonly cited being companionship, feelings of satisfaction and reward, fulfillment, and a sense of duty. These authors also found that positive feelings about caregiving were negatively associated with caregiver burden and depression.
Kramer (Reference Kramer1997a) used the term gain to refer to any positive benefit resulting from the caregiving role and went on to show (Kramer, Reference Kramer1997b) that such gains were negatively predicted by level of education and positively predicted by problem-focused coping and satisfaction with social life. Sanders (Reference Sanders2005) subsequently proposed three main kinds of gain: (a) Spiritual growth and increased faith, described by caregivers as a deepened sense of spirituality or a closer relationship to God; (b) personal growth, such as becoming more patient or mature; and (c) feelings of mastery and accomplishments, associated with the perception of having been successful in the role of caregiver. In a similar vein, Netto et al. (Reference Netto, Jenny and Philip2009) also proposed three kinds of gain: (a) Personal growth, related to increased patience and understanding and a sense of mastery and of having acquired new skills and personal qualities such as resilience or humility; (b) gains in relationships, in the sense of an improved relationship with the care recipient and an increased ability to relate to other older adults; and (c) higher-level gains, such as spiritual growth.
Based on the latter three categories, Yap et al. (Reference Yap, Luo, Ng, Chionh, Lim and Goh2010) developed the Gain in Alzheimer Care Instrument (GAIN) to measure the benefits of caring for a person with dementia. This instrument comprises 10 items, the first four of which refer to personal growth, the following three to gains in relationships, and the final three to higher-level gains. The authors performed an exploratory factor analysis (EFA) and principal components analysis (PCA) and concluded that the GAIN had a unidimensional structure. They also examined correlations between GAIN scores and caregiver burden (measured with the Zarit Burden Interview, ZBI), dementia management strategies (evaluated using the Dementia Management Strategies Scale, DMSS), and positive aspects of caregiving (Positive Aspects of Caregiving scale). This analysis showed that GAIN scores were negatively correlated with burden (ZBI) and criticism (DMSS), and positively correlated with positive aspects of caring and with encouragement (DMSS) and active management (DMSS).
Liew et al. (Reference Liew, Luo, Ng, Chionh, Goh and Yap2010) explored the relationship between caregiving gains and both caregiver and care recipient variables. They found that higher GAIN scores were obtained by caregivers who were not in work, who had been the caregiver for more than three years, who spent at least 60% of their time each week on caregiving tasks, who had daily contact with the care recipient, who had minimal or no financial difficulties, who attended caregiver educational and support programs, and who cared for a person with a more advanced stage of dementia. These authors also examined correlations between GAIN scores and feelings of competence in the caregiver (measured using the Short Sense of Competence Questionnaire, SSCQ), dementia management strategies (evaluated with the DMSS), caregiver burden (ZBI), general mental health problems in the caregiver (assessed using the General Health Questionnaire 28, GHQ–28), and behavior problems in the care recipient (assessed with the Revised Memory and Behavior Problems Checklist, RMBPC). They found that GAIN scores were positively associated with the caregiver’s sense of competence (SSCQ) and with the use of encouragement and active management strategies (DMSS), and negatively correlated with burden (ZBI), mental health problems in the caregiver (GHQ–28), criticism as a management strategy (DMSS), and behavior problems in the care recipient (RMBPC). Regression analysis also showed that active management as a caregiving strategy, mental wellbeing of the caregiver, and participation in educational and support programs were significantly associated with gains, with the strongest predictor being an active management strategy.
Fabà and Villar (Reference Fabà and Villar2013) adapted the GAIN for use in the Spanish population. They analyzed its internal structure by means of EFA and concluded that the Spanish version replicated the single-factor structure of the original instrument. Reliability was assessed using the split-half method and by calculating Cronbach’s alpha coefficient (α = .87). Item homogeneity indices ranged between .46 and .68, and internal consistency was not significantly improved by omitting any of the items. Although the authors also sought to provide validity evidence based on relationships with other variables, this was only explored with respect to sociodemographic variables (age, gender, level of education, marital status, religiosity, caregiver’s perceived health, relationship to the care recipient, time spent as the caregiver, and hours per day and days per week dedicated to the caregiving role), of which only religiosity was significantly associated (in this case, positively) with GAIN scores. More recently, and with the aim of measuring more potential gains than are considered by the GAIN, Fabà et al. (Reference Fabà, Villar and Giuliani2017) developed the 22-item Gain Associated with Caregiving (GAC) scale. However, they did not obtain sufficient evidence of validity based on internal structure, since neither the single-factor model nor multi-factor models showed a good fit to the data. Furthermore, the GAC scale is focused on the Spanish population and it has not been adapted for use in other languages or countries, thus preventing cross-cultural comparisons. Consequently, our analysis here is focused on the GAIN, an instrument that is widely and internationally used.
Despite the important contribution of Fabà and Villar’s (Reference Fabà and Villar2013) study, the internal structure of the Spanish version of the GAIN has yet to be examined by means of confirmatory factor analysis (CFA), and validity evidence based on its relationships with psychological variables is still lacking. In order to address this gap, our aim here was to analyze the psychometric properties of the GAIN in a sample of Spanish informal caregivers of people with dementia. Specifically, we sought, first, to provide new validity evidence based on the internal structure of the instrument, using CFA to test the single-factor structure reported previously. Second, we analyzed the reliability of GAIN scores and examined item homogeneity. Finally, we aimed to provide new validity evidence based on relationships with other variables. The specific variables we considered were burden and mental wellbeing of the caregiver, which were explored when validating the original instrument (Liew et al., Reference Liew, Luo, Ng, Chionh, Goh and Yap2010; Yap et al., Reference Yap, Luo, Ng, Chionh, Lim and Goh2010) but not the Spanish version, and stress, anxiety, depression, and life satisfaction, which have yet to be examined in relation to GAIN scores. We expected to find that GAIN scores were positively associated with life satisfaction and negatively associated with caregiver burden, general mental health problems, stress, anxiety, and depression.
Materials and Methods
Participants
The initial sample comprised 115 informal caregivers of people diagnosed with dementia, of whom 113 (25 male and 88 female) were included in the final analysis. The exclusion of two participants was due to missing values in GAIN scores. As these cases accounted for less than 5% of the total, we opted to analyze only those cases with complete data (Garson, Reference Garson2015). The informal caregivers ranged in age from 35 to 82 years (M = 56, SD = 12.94) and they were recruited through 11 different day centers for people with Alzheimer’s disease and other dementias in the province of Malaga (Spain). To be eligible for participation they had to be over 18, to have spent at least six months as the caregiver of a person with dementia, to have a command of Spanish sufficient for understanding and answering the questionnaires, and to sign informed consent. In addition, the care recipient in each case had to have been diagnosed with dementia and to be attending one of the 11 aforementioned centers. The majority of caregivers were Spanish (97.35%), married (71.68%), lived with the care recipient (78.76%), and were his/her son or daughter (66.37%). Approximately half of the caregivers were in employment (43.36%) and a similar proportion (40.71%) had either no or only elementary school education. The time spent as a caregiver ranged from 1 year to eight years (M = 4.81 years, SD = 3.80).
Instruments
Caregiver gains
Gains were assessed with the Gain in Alzheimer Care Instrument (GAIN; Yap et al., Reference Yap, Luo, Ng, Chionh, Lim and Goh2010), in its Spanish version (Fabà & Villar, Reference Fabà and Villar2013; APA 2015). This is a 10-item scale with a five-point Likert-type response format (0 = disagree a lot, 4 = agree a lot), and higher total scores indicate a higher level of perceived gains. Exploratory factor analysis has shown that both the Spanish and the original version have a single-factor structure.
Caregiver Burden
Caregiver burden was assessed using the Spanish version (Martín et al., Reference Martín, Salvadó, Nadal, Miji, Rico, Lanz and Taussig1996) of the Zarit Burden Interview (ZBI; Zarit et al., Reference Zarit, Reever and Bach-Peterson1980). This self-report scale comprises 22 items (e.g., Do you feel that your relative asks for more help than he/she needs?) that are rated using a five-point Likert-type scale (1 = never; 5 = almost always). A higher total score indicates a greater level of perceived burden. Cronbach’s alpha in the present sample was .94.
General Mental Health
The general mental health of caregivers was assessed using the Spanish version (Rocha et al., Reference Rocha, Pérez, Rodríguez-Sanz, Borrell and Obiols2011) of the General Health Questionnaire 12 (GHQ–12; Goldberg & Williams, Reference Goldberg and Williams1988). The GHQ–12 is a unidimensional questionnaire used to screen for psychiatric problems, and each of its 12 items is rated on a four-point Likert-type scale (‘less than usual’, ‘no more than usual’, rather more than usual, and ‘much more than usual’). Because the GHQ–12 comprises both positive and negatively worded items (e.g., Have you recently been able to face up to your problems? Have you recently been feeling unhappy and depressed?), these response options are arranged so that no reverse scoring is necessary, and consequently higher total scores indicate poorer mental health. Cronbach’s alpha coefficient in the present sample was .90.
Depression, Anxiety, and Stress
The Spanish version (Daza et al., Reference Daza, Novy, Stanley and Averill2002) of the Depression Anxiety Stress Scales (DASS–21; Lovibond & Lovibond, Reference Lovibond and Lovibond1995a, Reference Lovibond and Lovibond1995b) comprises 21 items distributed equally across three subscales, corresponding to depression, anxiety, and stress. Each item is rated on a four-point Likert-type scale (from 0 = did not apply to me at all, to 3 = applied to me very much or most of the time; the time frame for responses is the past week), and higher scores on each subscale indicate a higher level of the respective variable. Example items are: I couldn’t seem to experience any positive feeling at all (depression), I experienced breathing difficulty (anxiety), and I found it difficult to relax (stress). Cronbach’s alpha coefficients in the present sample were .87, .85, and .88 for the depression, anxiety, and stress subscales, respectively.
Life Satisfaction
Life satisfaction was measured with the Spanish version (Vázquez et al., Reference Vázquez, Duque and Hervás2013) of the Satisfaction With Life Scale (SWLS; Diener et al., Reference Diener, Emmons, Larsen and Griffin1985). This is a unidimensional instrument and each of its five items (e.g., In most ways my life is close to my ideal) is rated on a seven-point Likert-type scale (1 = strongly disagree; 7 = strongly agree). Higher total scores indicate a higher level of life satisfaction. Cronbach’s alpha coefficient in the present sample was .88.
Procedure
We began by contacting the managers of various day centers for people with Alzheimer’s disease and other dementias in the province of Malaga, informing them about the study objectives and procedures. In those day centers that agreed to participate, the caregivers of center users were informed by managers about the study and invited to take part. Those who agreed and who signed informed consent for anonymized data collection and analysis were then given the aforementioned questionnaires to complete. The study was carried out in accordance with the Declaration of Helsinki and it was approved by the Experimentation Ethics Committee of the University of Malaga.
Data Analysis
We first conducted a descriptive analysis of GAIN item scores, calculating the mean, the standard deviation, and skewness and kurtosis coefficients.
In order to obtain validity evidence based on the internal structure of the GAIN we performed a CFA, testing a single-factor model using EQS 6.4 (Bentler, Reference Bentler2006). Because GAIN items are scored using a Likert-type scale, the analysis was based on the polychoric correlation matrix, using robust maximum likelihood estimators. We computed the Satorra-Bentler chi-square (S-B χ2), along with the following goodness-of-fit indices (Bentler, Reference Bentler2006): The comparative fit index (CFI; Bentler, Reference Bentler1990), the non-normed fit index (NNFI; Bentler & Bonett, Reference Bentler and Bonett1980), and the root mean square error of approximation (RMSEA; Browne & Cudeck, Reference Browne, Cudeck, Bollen and Long1993; Steiger, Reference Steiger2000). Values of the CFI and the NNFI approaching .95 indicate an acceptable fit (Bentler, Reference Bentler1992; Bentler & Bonett, Reference Bentler and Bonett1980; Hu & Bentler, Reference Hu and Bentler1999; McDonald & Ho, Reference McDonald and Ho2002), while a value of .95 or higher indicates good fit (Hu & Bentler, Reference Hu and Bentler1999); RMSEA values above .08 indicate poor model fit, those between .06 and .08 a reasonable fit (Browne & Cudeck, Reference Browne, Cudeck, Bollen and Long1993; MacCallum et al., Reference MacCallum, Browne and Sugawara1996), and those below .06 a good fit (Hu & Bentler, Reference Hu and Bentler1999).
The reliability of test scores was examined by calculating McDonald’s omega coefficient. Values of .70 or higher are considered acceptable (Campo-Arias & Oviedo, Reference Campo-Arias and Oviedo2008; Ventura-León & Caycho-Rodríguez, Reference Ventura-León and Caycho-Rodríguez2017; Viladrich et al., Reference Viladrich, Angulo-Brunet and Doval2017).
For the item analysis we computed corrected item-total correlation coefficients, which indicate the correlation between a given item and the total test score when that item is omitted. Values above .30 are considered satisfactory (De Vaus, Reference De Vaus2002; Traub, Reference Traub1994).
We also analyzed the relationship between GAIN scores and other variables by calculating Pearson correlation coefficients, which we interpreted according to Cohen’s (Reference Cohen1988) criteria: Around |.10| indicates a small correlation, around |.30| a moderate correlation, and |.50| or higher a strong correlation. The other variables considered here were caregiver burden, general mental health problems, stress, anxiety, depression, and life satisfaction.
Finally, having confirmed that the instrument has adequate psychometric properties, we calculated the mean and standard deviation for GAIN scores in the present sample of informal caregivers. All these analyses were performed using IBM SPSS.
Results
Descriptive Item Analysis
Table 1 shows the descriptive analysis of item scores. Most of the skewness and kurtosis indices indicate deviations from the normal curve, which justifies the use of the robust maximum likelihood method for the CFA.
Table 1. Descriptive Statistics for Item Scores: Mean (M), standard deviation (SD), skewness, and kurtosis
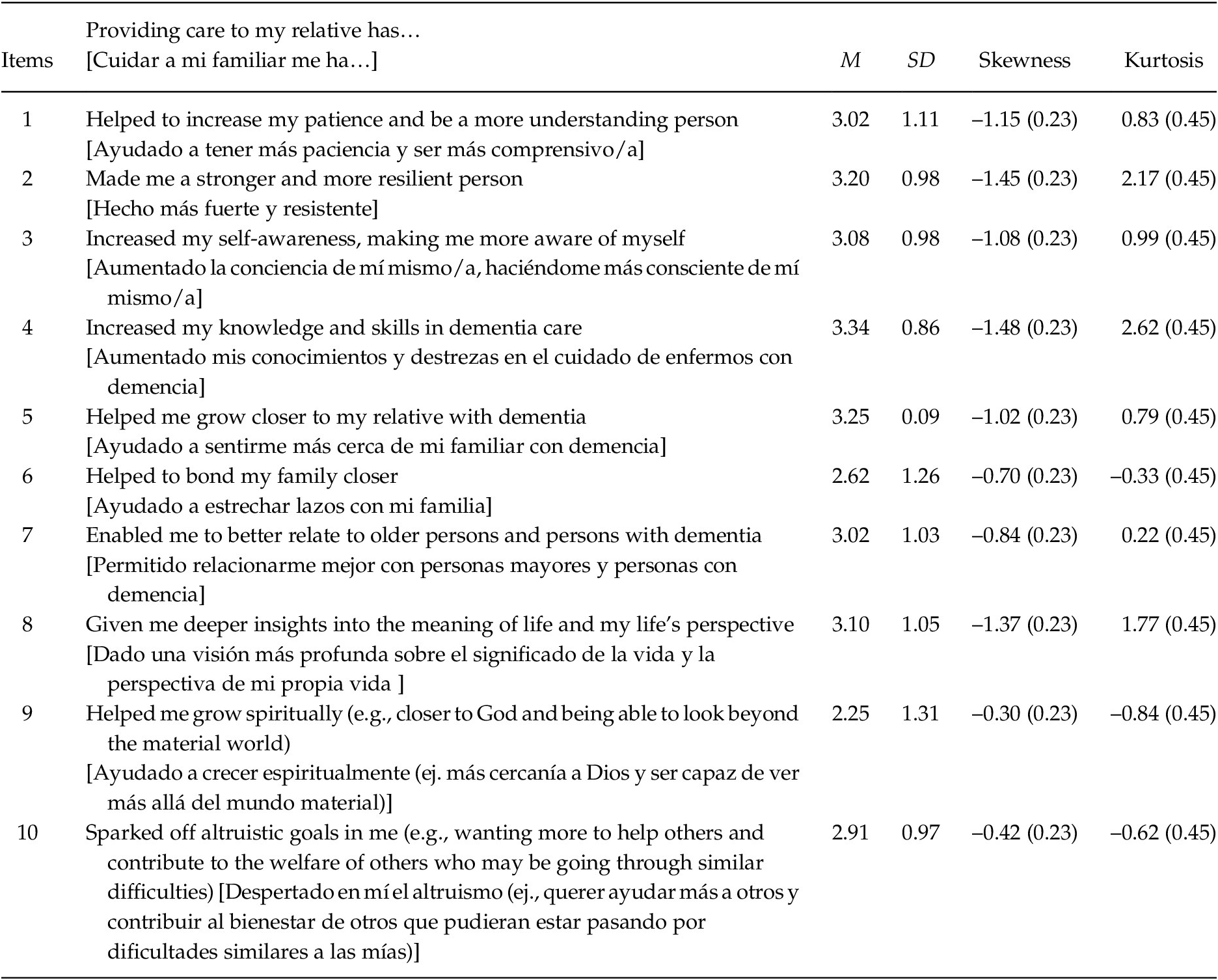
Note. N = 113.
Validity Evidence Based on Internal Structure
The fit indices for the single-factor model of the GAIN (Table 2) indicated satisfactory (CFI and NNFI) and reasonable (RMSEA) model fit. Although the upper bound of the confidence interval for the RMSEA was above .08, this may be an estimation error caused by the small sample size. At all events, and as Jöreskog and Sörbom (Reference Jöreskog and Sörbom2003) recommend, the fit of a model should be decided on the basis of the goodness-of-fit indices as a whole. Consequently, and given the values obtained, we found no reason to reject the hypothesis that the model reproduces the sample covariance matrix. The standardized coefficients are shown in Figure 1, and they are all statistically significant.
Table 2. Fit Indices for the Single-factor Model of the GAIN, as Tested in the CFA
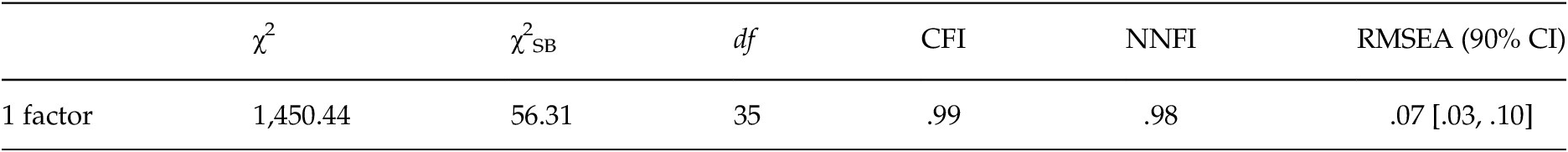
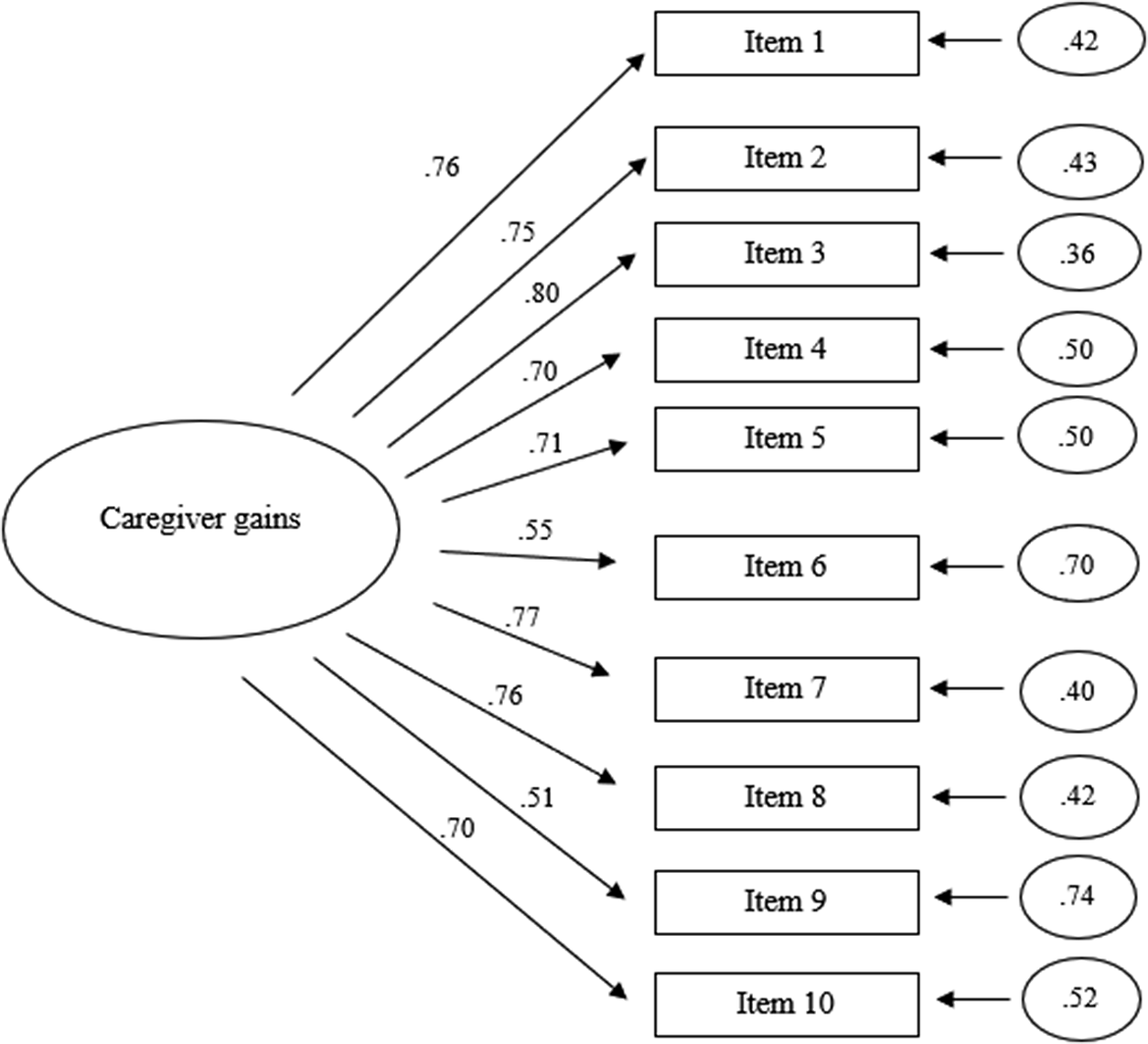
Figure 1. Single-factor model for the GAIN, with standardized parameter values.
Note. N = 113. χ2 = chi-squared statistic, χ2SB = Satorra-Bentler chi-squared, df = degrees of freedom, CFI = comparative fit index, NNFI = non-normed fit index, RMSEA = root mean square error of approximation, with a 90% confidence interval.
Reliability and Item Analysis
The value obtained for McDonald’s omega coefficient was .91, which indicates satisfactory reliability of test scores. The corrected item-total correlations ranged between .45 and .72, indicating adequate homogeneity indices for all items (Table 3).
Table 3. Corrected Item-total Correlation Coefficients
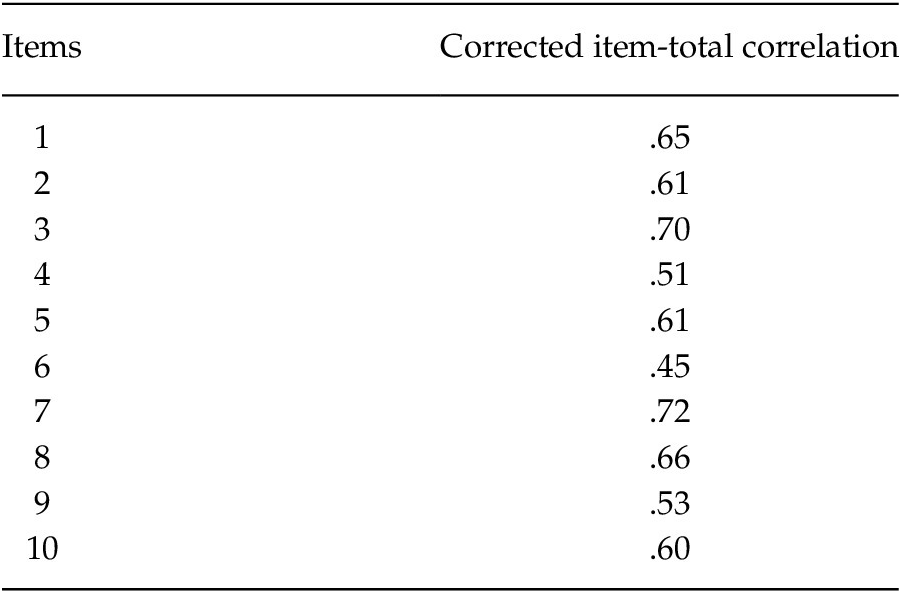
Note. N = 113.
Validity Evidence Based on Relationships with Other Variables
GAIN scores were positively and significantly correlated with life satisfaction, and negatively and significantly correlated with caregiver burden, general mental health problems, stress, anxiety, and depression (Table 4). In terms of effect size, the associations between GAIN scores and burden, stress, depression, and life satisfaction were moderate, whereas the associations with general mental health problems and anxiety were of small magnitude.
Table 4. Correlations between GAIN Scores and Caregiver Burden, General Mental Health Problems, Stress, Anxiety, Depression, and Life Satisfaction

Note. N = 113.
*p < .05. **p < .01.
Interpretation of Scores
The total score on the GAIN is obtained by summing the item scores (each scored from 0 to 4) and hence it ranges between 0 and 40, with higher scores indicating greater perceived gains from caregiving. In the present sample the minimum and maximum scores obtained were 8 and 40, respectively, with a mean of 29.78 (SD = 7.17) and a median of 30. These are relatively high values and indicate that our participants generally perceive positive benefits associated with their caregiving role.
Discussion
The aim of this study was to analyze the psychometric properties of the GAIN in a sample of Spanish informal caregivers of persons with dementia. To this end, we began by conducting a CFA in order to obtain new validity evidence based on the internal structure of the instrument. We then analyzed the reliability of GAIN scores and examined item homogeneity. Finally, we sought to provide new validity evidence based on relationships with other variables, specifically, caregiver burden, general mental health problems, stress, anxiety, depression, and life satisfaction.
The results of the CFA indicated that the GAIN has a single-factor structure. The fit indices were satisfactory, although the upper bound of the confidence interval for the RMSEA was above .08, suggesting that the model could be improved. However, as Kenny et al. (Reference Kenny, Kaniskan and McCoach2015) point out, this index is highly sensitive to sample size and may be inflated with small samples, such as that used in the present study. These authors therefore recommend using other indices such as the CFI or NNFI in models with few degrees of freedom. Based on the values obtained with the other fit indices we consider that the single-factor model shows a satisfactory fit to the data. This single-factor structure is consistent with that reported in previous studies, and as such the results of the CFA support those obtained through EFA (Fabà & Villar, Reference Fabà and Villar2013; Yap et al., Reference Yap, Luo, Ng, Chionh, Lim and Goh2010). This structure also supports the use of the total test score, with higher scores indicating greater perceived benefits of caregiving.
The results for item homogeneity and reliability based on internal consistency were also satisfactory. The value of McDonald’s omega (.91) was similar to the alpha coefficient reported by Yap et al. (Reference Yap, Luo, Ng, Chionh, Lim and Goh2010) for the original version of the instrument (.89) and to that obtained by Fabà and Villar (Reference Fabà and Villar2013) when developing the Spanish adaptation of the GAIN (.87).
As regards validity evidence based on relationships with other psychological variables, the analysis showed that GAIN scores were positively and significantly correlated with life satisfaction and negatively and significantly correlated with caregiver burden, general mental health problems, stress, anxiety, and depression. Based on Cohen’s (Reference Cohen1988) criteria, most of these associations were of moderate magnitude, the exceptions being the small correlations obtained with respect to general mental health problems and anxiety. These results indicate that informal caregivers who perceive greater benefits from caregiving also report higher life satisfaction and lower levels of the following: Burden, general mental health problems, stress, anxiety, and depression. This is in line with previous studies which found that burden and mental health problems were negatively and significantly associated with caregiving gains (Liew et al., Reference Liew, Luo, Ng, Chionh, Goh and Yap2010; Yap et al., Reference Yap, Luo, Ng, Chionh, Lim and Goh2010), and it constitutes further empirical evidence of the relationship between GAIN scores and other measures of psychological wellbeing. Our findings are also consistent with those reported when using different instruments to measure caregiving gains, which likewise showed a positive relationship with life satisfaction and a negative association with depression and burden (Fabà et al., Reference Fabà, Villar and Giuliani2017). Overall, these results suggest that interventions aimed at enhancing the perceived gains of caregiving could have a positive impact on the caregiver’s psychological health.
Despite providing new evidence for the validity and reliability of the GAIN, this study has a number of limitations that need to be acknowledged. First, all the data were obtained using self-report measures. Second, participants were recruited through day centers for people with dementia in the province of Malaga (southern Spain), which may limit the generalizability of results. Third, relationships between variables were examined using a correlational analysis, and hence no causality can be inferred. Finally, the sample size may be small, due to the difficulty of recruiting participants in settings such as this. Empirical evidence has shown that several factors affect sample size requirements, including number of indicators and factors, magnitude of factor loadings, and amount of missing data (Wolf et al., Reference Wolf, Harrington, Clark and Miller2013). Overall, the analysis of complex models requires more sample size than that of a simpler model (Kline, Reference Kline2011) as the one tested here. For example, Wolf et al. (Reference Wolf, Harrington, Clark and Miller2013) found that the eight-indicator single-factor model with loadings of .50 were associated with a minimum sample size of 90. In any event, in order to extend knowledge, the present study should be replicated with larger samples in future research.
Although the GAC scale (Fabà et al., Reference Fabà, Villar and Giuliani2017) is also designed to measure gains associated with caregiving in the Spanish population, there are two reasons why we consider the GAIN to be a more suitable instrument overall. The first is that the GAC scale is focused on this population, whereas the GAIN is widely and internationally used, thus enabling cross-cultural comparisons. In addition, despite the important contribution of Fabà et al.’s (Reference Fabà, Villar and Giuliani2017) study, further research is needed to clarify the internal structure of the GAC, whereas there is already empirical evidence from different cultural contexts supporting a clear structure for the GAIN.
In summary, we sought in this study to provide new validity evidence for the Spanish version of the GAIN, analyzing its psychometric properties in a sample of informal caregivers of people with dementia. We began by conducting a CFA to examine its internal structure, and then analyzed item homogeneity and the reliability of item scores. Finally, we explored the relationship between GAIN scores and other psychological variables, specifically, caregiver burden, general mental health problems, stress, anxiety, depression, and life satisfaction. The results obtained were satisfactory and indicated a good fit of the single-factor model to the data. Reliability of scores and item homogeneity were both satisfactory, and significant associations were found between GAIN scores and scores on all the other variables considered. The instrument is quick and easy to apply and given the association between GAIN scores and other variables, it may be used to provide information about a caregiver’s psychological health status.
We thank the day centers for people with Alzheimer’s disease and other dementias in Málaga for their help in recruiting participants for this study.







