In December 2019, a series of unexplained pneumonia cases emerged in Wuhan, Hubei Province of China. Reference Huang, Wang and Li1 The cause was later identified as a novel RNA β-coronavirus by deep sequencing analysis, Reference Lu, Zhao and Li2 and it has been named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) by the International Committee on Taxonomy of Viruses. Reference Zhu, Zhang and Wang3 On February 11, 2020, the World Health Organization (WHO) officially named the disease caused by SARS-CoV-2 coronavirus disease 2019 (COVID-19).
COVID-19 has become a worldwide public health challenge. As of September 28, 2020, SARS-CoV-2 has affected 235 countries, causing >30 million infections and 991,224 deaths. 4 Given the immediacy and widespread nature of the COVID-19 pandemic, healthcare workers (HCWs) around the world are facing increasing challenges and higher infection risks. A recent meta-analysis showed that among all COVID-19 patients in different countries, HCWs accounted for 4.2%–17.8% of cases. Reference Sahu, Amrithanand, Mathew, Aggarwal, Nayer and Bhoi5 As of February 11, 2020, a report from the Chinese Centers for Disease Control and Prevention indicated that 1,716 HCWs were confirmed to be infected by SARS-CoV-2 in China. 6 As of April 9, 2020, >5,000 HCWs have been infected in Italy 7 and nearly 9,300 in the United States. 8
To reduce the number of infections among HCWs and to achieve early identification and management, it is crucial to determine the epidemiological and clinical characteristics of these infections. However, studies on this issue are scarce thus far. Additionally, under the current context of heavy workload and continuing psychological stress placed on frontline HCWs, Reference Chen, Liang and Li9,Reference Wu, Fang and Guan10 the critical question that needs to be addressed is whether there are differences in signs, symptoms, and case fatality rates between HCWs and other occupational groups. We conducted this study to address these questions.
Methods
Study design, data source, and study population
The participants in this study were all cases identified through epidemiological investigation in Hubei Province as of February 27, 2020, who were followed until March 7, 2020. Individuals were classified as HCWs or “other” occupational cases based on their occupation. 6 Specifically, HCW refers to medical and health professionals who are directly involved in patient care. These occupations include reception, screening, inspection, testing, transfer, treatment, nursing, epidemiological investigation and medical observation, as well as medical and health professionals who directly perform case specimen collection, pathogen detection, pathological examination, and pathological anatomy. The others are defined as other occupational cases. After excluding suspected or clinically diagnosed cases and those who had a missing value recorded for their occupation, 43,126 cases remained in the data set. First, we included HCWs only, and we analyzed the epidemiological and clinical characteristics of the subgroup of HCWs with COVID-19 (Fig. 1). Second, to compare the differences in signs and symptoms between HCWs and other occupational cases, we further excluded those with a missing value for the onset of symptoms variable. From the initial 43,126 cases, this left 1,013 HCWs and 17,972 other occupational cases. We then matched 2,026 other occupational cases based on sex, age, address and the date of symptom onset (Fig. 1). Third, for these 43,126 cases, and we analyzed the association between occupation and the risk of COVID-19 mortality (Fig. 1).

Fig. 1. The flowchart of subjects.
Variables
Demographic characteristics and clinical features were collected using a case questionnaire at the time of diagnosis and were then input into the infectious disease information system by local epidemiologists or public health professionals. The case questionnaire contains basic demographic or epidemiological information (eg, sex, birthdate, present address, occupation, Wuhan-related exposure and confirmed cases exposure) and clinical information (eg, symptom onset, the date of symptom onset, blood cell count). We computed the age of each case using the date of symptom onset and birthdate. According to the present address, all of the records were further classed as residents in Wuhan or elsewhere. The severity of symptoms variable was categorized as asymptomatic, mild, common, severe, or critical. Our diagnostic criteria on clinical severity followed the Chinese clinical guidance for COVID-19 pneumonia diagnosis and treatment. 11 All of the confirmed HCWs were diagnosed based on positive viral nucleic acid test results from throat swab samples. 6 The date of symptom onset in asymptomatic cases was based on the date of the positive nucleic acid test results.
Statistical analyses
Categorical variables were expressed as counts (alongside percentages), and continuous variables were expressed as medians (alongside interquartile ranges). All statistical analyses were performed using R version 3.5.3 software (R Foundation for Statistical Computing, Vienna, Austria). A 2-tailed P value <.05 was considered statistically significant.
To describe the epidemiological characteristics and clinical features of SARS-CoV-2 infection among HCWs, we classified the date of symptom onset into 4 categories: before January 23, 2020 (the lockdown date in Wuhan city), January 24–February 3, February 4–13, and February 14–27. Moreover, an epidemic curve for the distribution of case severity was constructed to show the progression of illness among HCWs involved in the outbreak over time.
To include controls in our study, we matched 1,013 HCWs and 2,026 other occupational cases based on sex, age, address, and the date of symptom onset, and we compared the differences in clinical signs or symptoms. The Wilcoxon signed-rank test was used to compare continuous variables with skewed distribution, and the χ2 test or the Fisher exact test was used to compare categorical variables.
A logistic regression model was performed to analyze the association between occupation and the risk of COVID-19 mortality. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated for the output. The potential confounders were ascertained based on prior publications Reference Leung, Hedley and Ho12,Reference Zhou, Yu and Du13 and these included age range (20–29, 30–39, 40–49, 50–59, and 60+ years), sex (male or female), disease severity (severe or nonsevere), address (Wuhan city or elsewhere), and the date of symptom onset (before January 24–February 3, February 4–13, or February 14–27).
Results
Epidemiological and clinical characteristics of HCWs stratified by the date of symptom onset
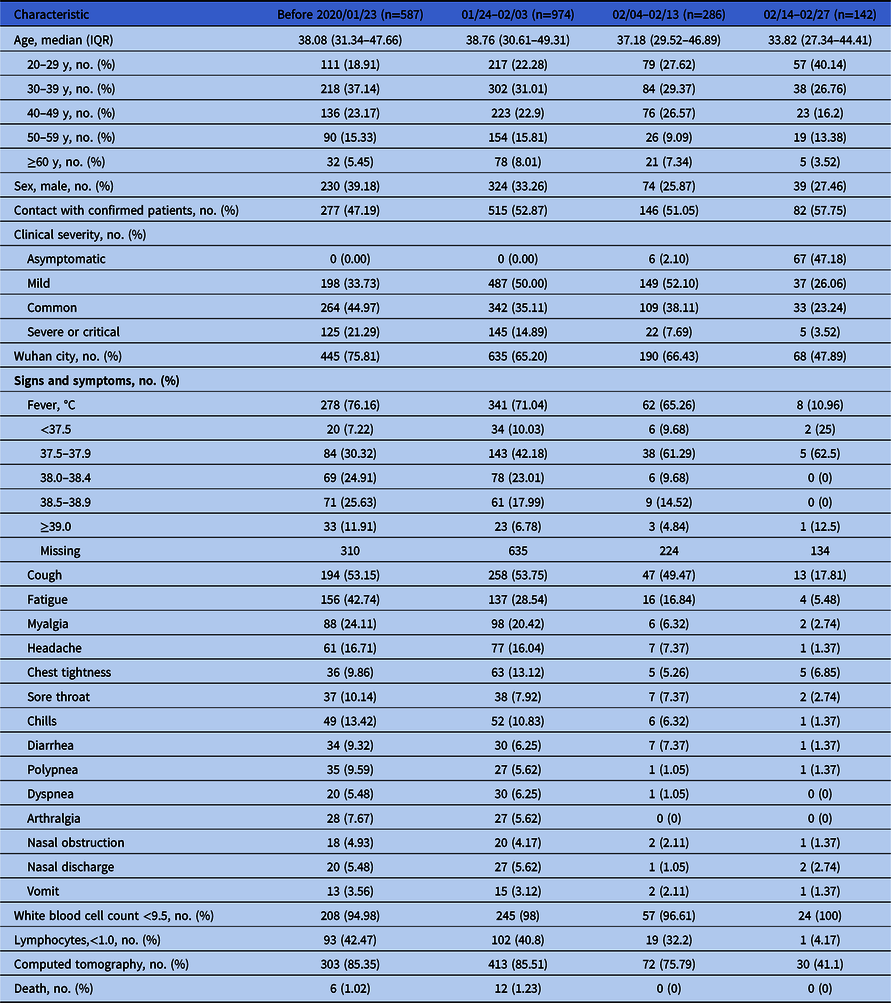
From December 27, 2019, through February 27, 2020, a total of 1,989 HCWs were laboratory-confirmed to have SARS-CoV-2 infection in Hubei Province, China. The epidemiological and clinical characteristics of HCWs, stratified by the date of symptom onset, are shown in Table 1. Fever and cough were the most common onset symptoms in HCWs during any period. In total, 297 HCWs (14.93%) were diagnosed with severe or critical cases, and 18 HCWs had died by the end date of the follow-up period. Nearly half of HCWs had no reported contact with known COVID-19 patients (969, 48.72%). Before the date of lockdown in Wuhan city (January 23, 2020), a total of 587 HCWs were laboratory-confirmed to have SARS-CoV-2 infection, and most of these cases occurred in Wuhan city (445, 75.81%). From February 14 to February 27, a total of 142 HCWs were laboratory-confirmed to have SARS-CoV-2 infection, and asymptomatic cases accounted for 47.18% of the cases (68, 47.18%).
Table 1. Characteristics of 1,989 Healthcare Workers (HCWs)
We created an epidemiological curve to illustrate the progression of illness among HCWs involved in the outbreak over time (Fig. 2). Asymptomatic, mild, common, and severe or critical cases were stacked to show total daily cases by date of symptom onset. In general, the peak number of cases occurred around January 23–25, 2020. Thereafter, illness incidence declined.

Fig. 2. Epidemiological curve of SARS-CoV-2 in Hubei Province through February 27, 2020. Note. This epidemiological curve shows the progression of illness among HCWs in the outbreak over time.
The comparison of clinical characteristics between HCWs and other occupational cases
Based on sex, age, address, and the date of symptom onset we matched 1,013 HCWs and 2,026 other occupational cases. The results of the comparison of clinical characteristics between the 2 groups are presented in Table 2. Fever and cough were the most prevalent symptoms at disease onset in both HCWs (689 [68.02%] and 512 [50.54%]) and other occupational cases (1,583 [78.13] and 1,095 [54.05%]). Compared with other occupational cases, HCWs had higher rates of fatigue (30.90% vs 25.02%; P < .001), myalgia (19.15% vs 13.43%; P < .001), and chills (10.66% vs 8.09%; P = .023), but they had a lower rate of dyspnea (5.03% vs 7.35%; P = .019). HCWs also had a (borderline) significantly lower case fatality rate (0.99% vs 2.02%; P = .052).
Table 2. The Comparison of Clinical Characteristics Between Healthcare Workers (HCWs) and the Matched Cases in Other Occupations

The association between occupation (HCWs or other) and death with COVID-19
Of the overall laboratory-confirmed cases, those who were older, male, severely or critically ill, Wuhan residents, and cases with disease onset at early outbreak had significantly higher risk of death (Table S1). After adjustment for these confounders, HCWs had a lower risk of death than other occupational cases (OR, 0.50; 95% CI, 0.30–0.79) (Table 3).
Table 3. The Risk Factors of SARS-CoV-2 Deaths Among Laboratory-Confirmed Cases (n=43,126)

Note: OR, odds ratio; CI, confidence interval; HCWs, healthcare workers.
a Covariates in model included age, sex, Wuhan city, disease severity, occupations, and the date of symptom onset.
Discussion
In the study cohort, 1,989 HCWs were infected by SARS-CoV-2, including 297 (14.93%) severe or critical cases and 73 (3.67%) asymptomatic cases. Fever and cough were the most prevalent symptoms at disease onset in both HCWs and other occupational cases. Compared with other occupational cases, HCWs had higher rates of fatigue (30.90% vs 25.02%; P < .001) and myalgia (19.15% vs 13.43%; P < .001). As of March 7, 2020, 18 HCWs and 2,056 other occupational cases died due to COVID-19, for case fatality rates of 0.9% and 5.0%, respectively. HCWs also had a significantly lower risk of death than other occupational cases (OR, 0.50; 95% CI, 0.30–0.79) after adjusting for potential confounders. To the best of our knowledge, this is the largest sample among the reports on the epidemiological and clinical characteristics of SARS-CoV-2 infections among HCWs in China.
Fever and cough were the dominant symptoms among HCWs at any period of time since the SARS-CoV-2 outbreak (Table 1), which is in line with recent findings based on the general population. Reference Huang, Wang and Li1,Reference Guan, Ni and Hu14,Reference Wang, Hu and Hu15 Notably, HCWs had significantly higher rates of myalgia and fatigue than other occupational cases. One of the possible reasons for this may be that HCWs had heavier workloads, longer working hours, and higher work pressure than other occupations during this special period. Another plausible reason might be that HCWs have a more comprehensive understanding of the disease and may report more symptoms than other occupations.
Based on the data from the WHO, the case fatality rate of SARS-CoV-2 infection varies in different regions or countries. For instance, as of September 30, 2020, the case fatality rate was 11.5% in Italy, 9.4% in the United Kingdom, 8.7% in Belgium, 6.4% in Sweden, 5.8% in France, 5.6% in Netherlands, 4.2% in Spain, and 2.9% in America. 16 In China, the official data presented a case fatality rate of 5.2% (4,746 deaths in 91,041 confirmed cases). However, data to show the case fatality rate of SARS-CoV-2 among HCWs are limited, and no study has yet indicated whether HCWs have a higher risk of death from COVID-19. Our study results contributed to the current literature, showing that through March 7, 2020, the case fatality rate of 1,989 infected HCWs was 0.9% in Hubei Province of China and that HCWs had a significantly lower risk of death from COVID-19. Generally, frontline HCWs experienced heavier workloads and higher psychological stress than other occupational cases during this pandemic period. HCWs have a more comprehensive understanding of diseases and are, on average, younger than those in other occupations, and potentially important protective factors may be related to these factors. Another potential explanation might be the easy access to medical resources that comes with being a HCW.
Notably, nearly half of HCWs with confirmed COVID-19 reported no known contact with COVID-19 patients, implying that the potential infection risks do not only come from the hospital environment (eg, patients, other HCWs, or fomites), but also from community transmission. These findings are in line with recent findings in Singapore. Reference Wong, Tan, Leo, Lee and Toh17 According to previous studies, Reference Suwantarat and Apisarnthanarak18,Reference Zou, Lin and Du19 nosocomial infection of SARS in HCWs was affected by clinical condition of SARS patients, hospital environments, and their personal protective measures. Therefore, training for HCWs, especially in densely populated areas or countries with insufficient medical resources and insufficient experience in prevention or treatment of infectious diseases, should be conducted.
Moreover, our findings suggest that although only a small proportion of HCWs are asymptomatic infections, most of them occurred in the late stage of the outbreak. The explanation might be, at least in part, the result of testing protocols that were used to identify symptomatic cases in the early stage of the outbreak. Reference Pan, Liu and Wang20 Additionally, with the improvement of medical resources, HCWs were more likely to seek testing at an earlier stage of illness or to seek testing while asymptomatic and after exposure to confirmed or suspected COVID-19 cases. Non–symptom-based screening for HCWs also indicated that most infected HCWs were asymptomatic. Reference Mostafa, Kandil and El-Sayed21 Given the transmission possibility of asymptomatic cases, Reference Bai, Yao and Wei22 achieving early detection and expanding the scope of COVID-19 testing among HCWs might help to improve early isolation and early management. Early detection contributes to a reduction in infection rate. Therefore, local public health departments and hospitals should strengthen their detection strategies among HCWs to reduce the risk of nosocomial infection, to minimize clusters among HCWs, and to avoid transmission to patients.
This study has several limitations. First, since HCWs are more likely to be tested earlier in the course of disease than other occupational groups, the potential for detection bias and changes in testing protocols over the course of the study period may have influenced our findings. Second, although some clinical laboratory indicators (eg, blood gas and inflammatory markers) have been reported to be associated with an increased risk of mortality, Reference Xu, Xu and Zhang23 the absence of these data might bias the estimated association in the present study. Third, the incubation period could not be estimated here. Lastly, the existence of recall bias (eg, the date of symptoms onset) might inevitably affect our assessment.
In summary, compared with cases in other occupation groups, our results suggest that HCWs have a lower risk of death in the Hubei Province but have higher rates of fatigue and myalgia. Nearly half of HCWs with confirmed COVID-19 reported no known contact with COVID-19 patients, which highlights the need to maintain strict vigilance and precautionary measures at all times. Additionally, to protect the health and safety of this essential national workforce, it is crucial to strengthen the detection strategies and to reinforce infection control among HCWs.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/ice.2020.1321
Acknowledgment
We give special thanks to all the HCWs on the frontline.
Financial support
This research was conducted without funding.
Conflicts of interest
All authors report no conflicts of interest relevant to this article.








