If you are in a professional psychology training program, it is likely that you will be asked to be a clinical supervisor at some point in your career. In fact, based on an extensive survey of the members of the American Psychological Association (APA) division that represents clinical psychologists (Division 12; Society of Clinical Psychology), it was determined that clinical supervision is provided by 55 percent of university professors, 71 percent of hospital psychologists, and 36 percent of independent practitioners (Reference Norcross, Karpiak and SantoroNorcross et al., 2005). For many of you, this is an eagerly anticipated activity, and for others, it may be a source of some uncertainty or even anxiety. The purpose of this chapter is to demystify the idea of becoming a supervisor by providing broad theoretical models for conceptualizing the practice of supervision and practical suggestions to guide you through the process of learning to be a supervisor. We will also discuss current competency-based supervision practice and provide suggestions for how to incorporate ethical and multicultural considerations into supervision. Throughout the chapter, we will include the perspectives of an experienced clinical supervisor (E.H.W.) and the perspectives of the second author (E.F.C.) from when she was an advanced graduate student just starting her journey toward becoming a competent supervisor. In this way, we aim to provide you with different perspectives on this learning process.
Most graduate students and interns see learning to supervise as a critical and expected step in their professional development. In fact, the expectation that you will attain a reasonable level of competency in supervision prior to completing your training is now integrated in a step-wise fashion into the accreditation standards for doctoral programs and internships. Doctoral students are expected to “demonstrate knowledge of supervision models and practices,” while interns are expected to “apply this knowledge in direct or simulated practice with psychology trainees, or other health professionals … examples … include, but are not limited to, role-played supervision with others, and peer supervision with other trainees” (APA Commission on Accreditation, 2015). This means that most of you, in addition to being supervised in your training programs and internships, will also be starting the process of learning to supervise others. What is it that you will be learning to do in supervision training? Let’s turn next to defining supervision and providing a broader context for this activity.
1. Defining Supervision
Despite the fact that most of us know what supervision is and what it means to be a supervisor, the terms can be surprisingly difficult to define in a comprehensive manner. A classic and broadly accepted definition is provided here:
Supervision is an intervention provided by a more senior member of a profession to a more junior colleague or colleagues who typically (but not always) are members of that same profession. This relationship is evaluative and hierarchical, extends over time, and has the simultaneous purposes of enhancing the professional functioning of the more junior person(s); monitoring the quality of professional services offered to the clients that she, he, or they see; and serving as a gatekeeper for the particular profession the supervisee seeks to enter.
Let’s walk through this definition because the elements capture the central functions of supervision (from the Latin for oversight) in contemporary professional psychology. In the first sentence of the definition, it is stated that supervision is an intervention. What does this mean? The notion that supervision is an intervention in its own right is somewhat counterintuitive. It is interesting to note that the term is derived from the Latin word intervenire or inter (between) venire (come); to come between. In our field, psychological interventions are, at their essence, intended to alter a negative course or process in order to improve psychological functioning. If supervision is an intervention, then it is attempting to come between or alter the behavior of the person in training who is, in turn, attempting to intervene with the client. If supervision is itself a complex and multifaceted process, then it is clear that teaching someone to be a supervisor is even more so. In terms of overarching goals, we are attempting to improve the skills of the supervisor-in-training, improve the clinical skills of the supervisee (usually a less-advanced practicum student), and improve treatment outcomes for the client; that is, we are attempting to intervene on multiple levels. As we will discuss later in this chapter, these levels of interweaving goals and responsibilities tend to become very complex. The definition provided above goes on to clarify that there is an ongoing and evaluative component to supervision that includes overseeing the quality of what is being provided to the clients and serving as a gatekeeper for the profession. This last statement reminds us that supervision is not only intended to ensure high-quality treatment for current clients, but for future clients as well. In training programs, it is common to differentiate between formative evaluations, which are designed to support the growth and development of the psychotherapy trainee, versus summative evaluations, which are designed to assess competencies, determine if adequate progress is being made, and provide a gatekeeping function for the academic program or internship site and the profession. It is clear that this classic definition of supervision quoted above incorporates the full range of these essential supervisory functions.
2. Taking on Your New Role
Becoming a clinical supervisor will involve several familiar roles that are merged into a new context. It will be subtly, but importantly, different from activities you have been exposed to, gained experience in, or mastered in your graduate training or personal life. In addition, you will likely have some key questions, and possibly some concerns, as you contemplate this new role: What will be expected of me? What if I have nothing to contribute? Should I focus on the supervisee or their client? It can be helpful to remember that new roles bring rewards as well as challenges. And, as mentioned above, you will indeed be able to draw from familiar roles. There are sophisticated theoretical and research analyses of the competencies and roles in supervision that you may find helpful to draw from as you begin your work as a clinical supervisor and refer back to as you become more experienced.
3. Social Role Discrimination, Developmental, and Theoretical Models of Supervision
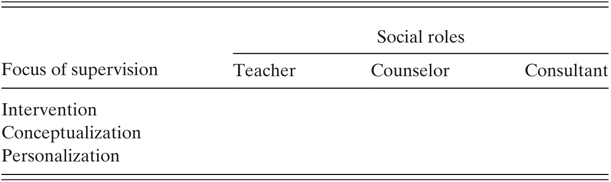
You have likely already learned in multiple contexts that theories and models serve to organize complex experiences. The social role discrimination model explicitly describes the familiar roles that you will draw from in learning to be a supervisor. This model was initially developed by Reference BernardBernard (1979) and has been elaborated by Reference Bernard and GoodyearBernard and Goodyear (2014) in their classic text. In this model, both the role and the focus taken by the supervisor throughout the course of a supervision session are identified. As supervisors become more experienced, they are encouraged to more intentionally select the role that is enacted and the focus of the supervisory session that is selected. In this model, the three central roles that have been identified are: teacher, counselor and consultant. Here are some examples of the social roles that can be identified in supervision:
Teacher: In supervision, you may be teaching your supervisee very basic skills, such as how to schedule an appointment, complete consent forms, or complete progress notes. More complex skills might include learning how to take a detailed family history, conduct a suicide risk assessment, or introduce a mindfulness exercise. In cognitive-behavioral programs, supervisors will be teaching supervisees how to provide psycho-education to their clients regarding the interrelatedness of thoughts, feelings, and behaviors, how to collaboratively engage in a functional analysis, how to assign and analyze thought records, how to conduct behavioral activation, etc.
Counselor: In this role, a supervisor might process with the supervisee the experience of feeling more anxious about particular clients more so than others or how their own experiences might impact their interactions with a client who has a similar concern. A supervisor may also discuss various fears that the supervisee may have about beginning clinical work: What if my client replies to my questions with one-word answers? What if the client asks my age or if I am their first client? What do I do if I don’t know what to say? Will my client want to come back and see me again? It is useful to note that if you are a supervisor in training, these questions from an anxious supervisee seeing their first client might in turn make you a bit anxious in your new role as a supervisor. We will talk later in this chapter about the notion of parallel process.
Consultant: In the consultant role, the supervisor may push for the supervisee to trust their own insights about their work or challenge the supervisee to think or act on their own. For example, the supervisor might encourage the supervisee to explore and discuss complex case conceptualization issues and how these might impact the treatment plan or discuss how the client’s cultural background might necessitate altering an established evidence-based treatment, providing consultation rather than driving these discussions. This more collegial role has been identified as important, but not surprisingly, it tends to be more difficult to define or identify in both theoretical writing and in observational research.
In the social role discrimination model, the focus of supervision may be on intervention skills, conceptualization skills, or personalization skills. Some examples of each are provided below.
Intervention skills: What is the supervisee actually doing in the session? The focus may include an examination and discussion of how the supervisee implemented or plans to implement a particular intervention technique or how the supervisee reflected or summarized the client’s thoughts and emotions in the session. This may also include discussions of points in the session where the supervisee felt confident in responding, was not sure how to respond, felt that a particular intervention strategy did or did not go as intended or, more generally, had a sense that a session was or was not effective. After viewing or listening to the session, the supervisor may note points in the session related to the considerations described above and may have specific suggestions for modifying intervention strategies.
Conceptualization skills: How does the supervisee understand the client(s) and the presenting problem(s)? In supervision, the conceptualization focus might involve the supervisor and supervisee collaboratively discussing factors that contribute to the maintenance of the client’s difficulties, such as avoidance, maladaptive thinking patterns, or a lack of emotion regulation skills. Such conceptualization work may also involve the supervisee and supervisor thinking through the ways in which various background factors, such as cultural considerations, may impact the way in which the client is experiencing his or her present difficulties.
Personalization skills: How does the supervisee blend or interface their personal style with the therapy that is being provided? This may involve the supervisor and supervisee discussing how the supervisee interacts with clients: What is the supervisee’s tone of voice like? How does the supervisee’s style change (or not) with various clients or with a client’s different affective presentations? How much is the supervisee versus the client talking in session? Generally, this skill involves the supervisor working with the supervisee to learn when and how they may want to adapt their natural therapeutic tendencies for a particular client or client presentation. As with the consultation social role discussed above, this factor is clearly important, but is more difficult to clearly define or identify in a supervision session.
The 3 × 3 table of the social role discrimination model of supervision provides a useful structure for engaging in a sophisticated process and content analysis of treatment. We encourage you to consider each of the cells as you read the rest of this chapter and to use it as a guide if you are currently learning to be a supervisor or if you are in supervision yourself. Becoming more aware of the social roles and foci we are most drawn to can help us to assess whether we are taking an approach that is well matched to the needs of the supervisee and their client.
In addition to the social role discrimination model described above, there are complex developmental models for understanding supervision. These models focus on the observation and description of common developmental pathways typically taken by the supervisor in training as they move through the learning process (Reference Bernard and GoodyearBernard & Goodyear, 2014). Some of these models have been extended beyond training and into professional practice. Most useful to consider here is that early in training, supervisors in training tend to prefer clearly articulated structure and may be most concerned about “doing it right.” This same conceptualization applies to a novice psychotherapy trainee. Therefore, we would expect that when you, as a supervisor in training, are supervising a novice graduate student therapist, you will spend relatively more time in the teacher role focusing on conceptualization and intervention skills. In parallel, the novice supervisor may want a bit more specific instruction regarding how to effectively provide supervision. As novice supervisors in training and therapists become more confident (and competent), they will likely spend more time in a consultative role and in the consideration of more complex conceptualization and personalization issues.
Theoretical models of supervision are based on psychotherapeutic models. Because many academic professional psychology programs now endorse a cognitive-behavioral therapy (CBT) model, we will briefly discuss how this model translates in to the practice of supervision.
Table 20.1 Reference BernardBernard’s (1979) 3 × 3 social role discrimination model
| Focus of supervision | Social roles | ||
|---|---|---|---|
| Teacher | Counselor | Consultant | |
| Intervention | |||
| Conceptualization | |||
| Personalization | |||
A supervisor using a CBT model would tend to work collaboratively with the trainee in supervision, would be likely to incorporate active agenda setting into the supervisory process, would identify and use role playing techniques to assist the trainee in learning new behaviors, and would be alert to dysfunctional thoughts, underlying beliefs, or schemas that might interfere with optimal functioning of the supervisee. Of course, because this is not psychotherapy, the focus remains on thoughts, feelings, and behaviors that are relevant to learning to be an effective therapist.
4. Parallel Process and Alliance in Supervision
Earlier in this chapter, we mentioned the notion of parallel process. What is this? This idea has its roots in psychodynamic theory and a full discussion is outside of the scope of this chapter. For our purposes, it is the recognition that some aspect of the psychotherapy process is being recreated or reenacted (in parallel) in the supervision. For example, a client may be dissatisfied with the psychotherapy and believes that it is not good enough or not sufficiently helping. For the client, this may reflect real problems in the treatment and could also reflect early experiences and associated core schemas in which caregivers or authority figures were not helpful, validating, or supportive. The first parallel might occur when the trainee comes to the supervisor in training and expresses dissatisfaction with the assistance that they are receiving for dealing with the challenging client. In supervision training, we add another level to this parallel process when the supervisor in training becomes anxious that they are not helping the psychotherapy trainee and experiences frustration that is then directed to the faculty supervisor. As mentioned earlier, the complexities quickly escalate in supervision training, and it can be helpful to identify parallel process when it is occurring. This can be a useful perspective to consider, even in the context of CBT and supervision that does not generally tend to focus on transference and countertransference issues.
The role that a positive working alliance has on supervision process and outcome has been extensively explored (Reference Bernard and GoodyearBernard & Goodyear, 2014; Reference Ladany, Ellis and FriedlanderLadany et al., 1999). Generally, the elements of alliance in both the psychotherapy and supervisory relationship are an agreement on goals and tasks in the context of a trusting (or bonded) relationship. The research regarding the importance of a positive working alliance is more clearly demonstrated in psychotherapy than it is in supervision, as supervision research often lags behind psychotherapy research in general (Reference Kühne, Maas, Wiesenthal and WeckKühne et al., 2019). However, there is general agreement that supervisees will disclose more in supervision and experience more satisfaction when there is a strong working alliance with the supervisor. We would therefore encourage the fostering of a relationship in which your supervisee will disclose subtle areas of concern or discomfort. The alliance is also critical to a consideration of multicultural factors in therapy and supervision. Some research in this area suggests that clinical supervision may indeed be associated with greater client symptom reduction (Reference Bambling, King, Raue, Schweitzer and LambertBambling et al., 2006), but more work is needed.
5. Ethical Considerations
Supervision and supervision training occurs within an ethical and legal context. While state laws vary, it is likely that supervision is addressed in the Psychology Practice Act in your state. In contrast, the APA Ethics Code (APA, 2017) applies to all of us and provides guidance and standards regarding the practice of clinical supervision. The major ethical issues related to clinical supervision include competence and client welfare, informed consent, supervisee rights, the relationship between supervisor and supervisee, and confidentiality. Standard 2 (Competence), 2.01 Boundaries of Competence (a) reminds us that “Psychologists provide services, teach, and conduct research with populations and in areas only within the boundaries of their competence, based on their education, training, supervised experience, consultation, study, or professional experience” (APA, 2017, p. 5). It is a good general rule to not supervise a psychological treatment or assessment that you, yourself, are not competent to provide. Similarly, a faculty supervisor should always be competent in the psychological service that is being provided in a supervision training context. This standard also relates to competence as a supervisor, which we will discuss in the next section. Standard 2.05 Delegation of Work to Others is interesting to consider as it relates to learning to be a supervisor: “Psychologists who delegate work to … supervisees … take reasonable steps to … authorize only those responsibilities that such persons can be expected to perform competently on the basis of their education, training, or experience … with the level of supervision being provided” (APA, 2017, p. 5, excerpted with emphasis added). What does this mean and why is it important? In both learning to be a therapist and a supervisor, if you were already fully competent, you would not need to learn how to do it and this chapter would not need to be written. The faculty or staff supervisors in your doctoral program or internship are responsible for ensuring that you have sufficient preparation and oversight to ensure competent service is being provided to the client and competent supervision to the less-advanced graduate student while you are learning. We like to consider this to be your learning edge, and it requires careful assessment and communication to ensure that the therapist or supervisor in training is challenged, but not overwhelmed. The ethical standards related to Informed Consent (10.01) remind trainees to inform clients that they are being supervised and to provide the name of the supervisor, when legal responsibility for the treatment resides with the supervisor. The Multiple Relationship standard (3.05) reminds us to be careful about potential conflicts in roles that could impair objectivity or judgment. Therefore, it is critical to inform the faculty supervisor if a personal relationship with the trainee might preclude you from providing effective supervision. This latter issue may be a common occurrence in doctoral programs and should be discussed directly. It is also important to remember that, as a supervisor in training, your interactions with the trainee are protected by educational confidentiality. Finally, Standard 7 (Education and Training) is important; we would encourage you to review it in its entirety as you begin your role as a supervisor in training. Standard 7.06 is so important that it is cited below its entirety:
7.06 Assessing Student and Supervisee Performance
(a) In academic and supervisory relationships, psychologists establish a timely and specific process for providing feedback to students and supervisees. Information regarding the process is provided to the student at the beginning of supervision.
(b) Psychologists evaluate students and supervisees on the basis of their actual performance on relevant and established program requirements. (APA, 2017, p. 10)
Faculty supervisors, supervisors in training, and training programs are jointly and mutually responsible for ensuring that evaluations occur as specified in the ethics code and in accordance with their program’s policies and procedures.
6. Multicultural Considerations and Competencies
Supervision training can be a bridge to incorporating the knowledge of multicultural and diversity issues that are learned in courses into clinical practice. In a survey of professional psychologists, it was determined that psychologists are more likely to be able to identify best multicultural practices than they are to endorse actually following these practices (Reference Hansen, Randazzo, Schwartz, Marshall, Kalis, Frazier, Burke, Kershner-Rice and NorvigHansen et al., 2006). In considering the implications for training programs, the authors recommend that in addition to typical multicultural training practices, supervisors might initiate “a frank discussion about why clinicians do not always do what they believe to be important. Identifying and openly discussing these barriers may improve the ability of practitioners to follow through when doing psychotherapy with clients who differ racially/ethnically from themselves” (Reference Hansen, Randazzo, Schwartz, Marshall, Kalis, Frazier, Burke, Kershner-Rice and NorvigHansen et al., 2006, p. 73). The authors recommend that multicultural training include a focus on the behaviors that psychologists endorse as being important but don’t practice. In this study, the five behaviors that were found to exhibit the largest discrepancies between what psychologists say they believe in and what they actually practice were: evaluating one’s multicultural competence, using culture-specific case consultation, making DSM IV cultural formulations and culture-specific diagnoses, and implementing a multicultural professional development plan. It is clear that supervision provides a key opportunity at many levels for you, as a supervisor in training, to assist the beginning therapist in the integration of multicultural concepts and competencies into clinical practice. In addition to ensuring that what is taught in multicultural courses is incorporated into practice, addressing barriers to the use of this knowledge is an important step in improving the multicultural competence of our profession in the future.
7. The Process of Learning to be a Supervisor
7.1 From the Perspective of Someone When She Was a Supervisor in Training (E.F.C.)
Learning to be a supervisor brought up many of the same feelings that I had when I was first learning to be a therapist: excitement, anxiety, and fear, among others. As I began this journey, I also found myself having similar thoughts to those that I had when I started with my first clients: Will what I’m saying make sense? Will this person leave the session feeling satisfied? Will I know how to respond to this person’s questions/comments? Do I really have anything to offer? Thus, in many ways, this process felt very similar to beginning my work as a therapist – I found myself having a wealth of mixed emotions, as well as a good deal of doubts and worries about my own abilities. However, just as we have familiar roles that we can draw on as we take on our new role as “therapist,” by the time we are ready to become supervisors, we have even more familiar (and likely more comfortable) roles that we are able draw upon (e.g., teacher, therapist). By the time you are a supervisor in training, you will have accumulated a wealth of graduate school experiences that have all likely prepared you for this new role in some way. Although it is probably natural to have some sense of the “imposter phenomenon” when taking on your new role as a supervisor (e.g., “Sometimes I’m not quite sure what to do with my own clients, and now I’m supposed to be guiding someone else in this process?!”), it is important to recognize all of the skills that you do have and that you can draw upon in this new role. For me, that was an extremely helpful thought “reframe” to keep in mind.
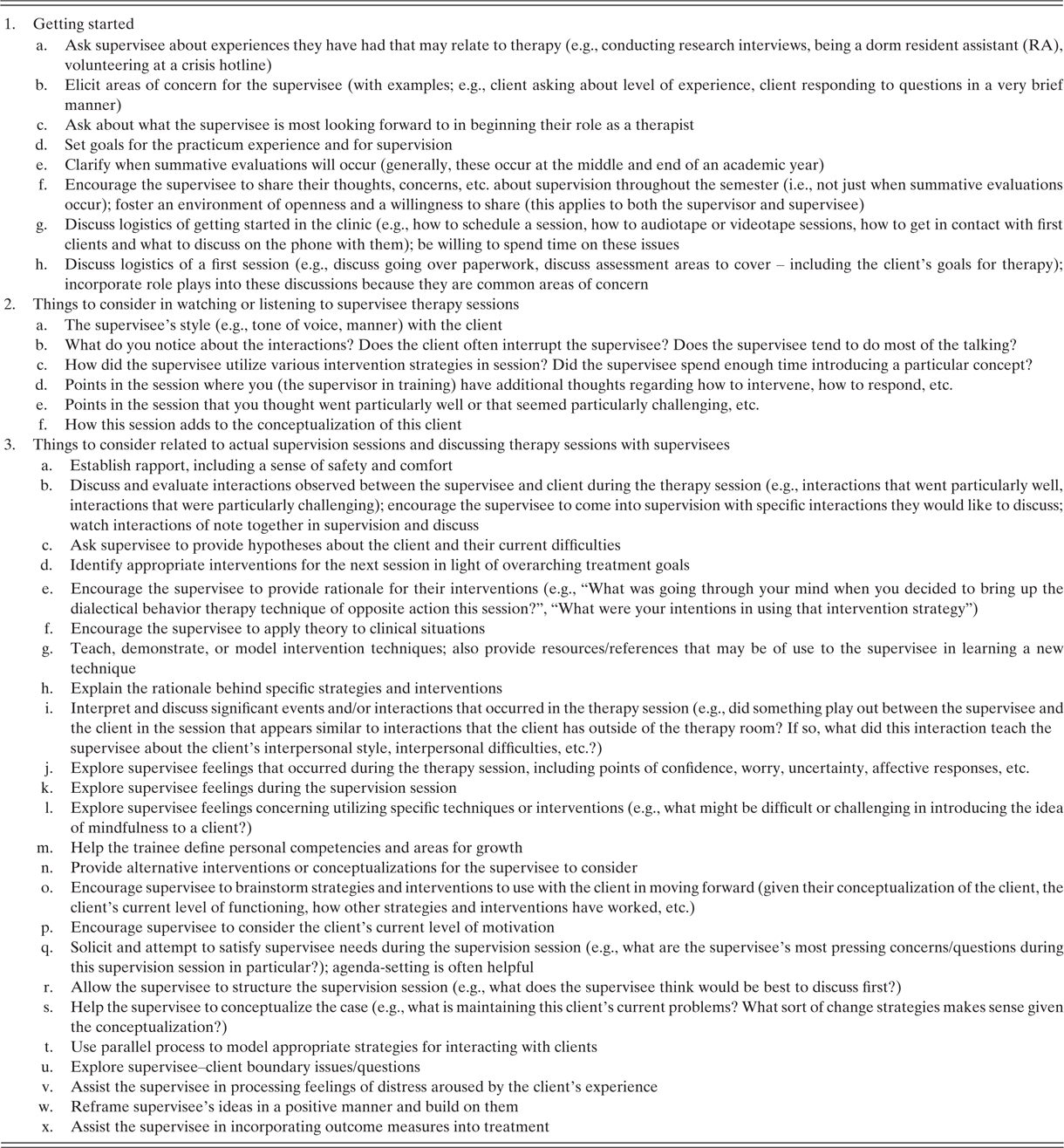
In my journey towards becoming a competent supervisor, I found “supervision of supervision” to be an incredibly helpful aspect of the learning process. Having the opportunity to bounce ideas off of an experienced supervisor with many years of experience was invaluable, as was drawing from some of my most positive supervision experiences. I often found myself thinking back to my early work as a therapist and what I found most helpful in supervision. What sorts of strategies did my most helpful supervisors employ with me? Thus, in learning to be a supervisor, keep in mind that not only do you have familiar roles that you can draw upon, but that you also have a good deal of experience as a “supervisee” yourself. Some specific suggestions (adapted and expanded from Reference NeufeldtNeufeldt, 1994) are presented in Table 20.2.
Table 20.2 Key strategies for supervisors in training in working with supervisees
7.2 From the Perspective of the Faculty Supervisor (E.H.W.)
I am going to keep my section short because most readers of this book are likely to be graduate students, interns, or early career psychologists. When we began to offer supervision training in our program, I was excited, but also daunted. In my own training, the ability to be an effective supervisor was assumed rather than taught. My first professional position was in a university psychological services center. As was common practice at the time, I was assigned practicum students, interns, and psychiatric residents to supervise with limited preparation in my own training for how to do so. Therefore, for me, as for many of my professional peers, there were no clear models for either how to be supervisors ourselves or for how to teach others to supervise. Over the years, I have adopted a model that includes formal elements (readings, regular meetings, and videotaping) and more informal discussion of the process and the experience. As described above in the section on parallel process, I have quickly learned that the responsibility for a client, a novice graduate student therapist, and an advanced graduate student supervisor can be complex – even when things are going well. I have found it useful to balance our consideration of the needs of all parties involved and to be sensitive to the alliance and parallel process at all levels. For faculty supervisors who are considering becoming involved in supervision training, I will share that, for me, the supervision of supervision in an academic doctoral program has been an immensely rewarding and energizing experience. It has provided me with an impetus to read the supervision literature and to be able to notice and articulate to someone else (hopefully with some coherence!) what it is that I do when I supervise. It has become a central and valued aspect of my own professional development. In fact, as another instance of parallel process, writing the original version of this chapter with someone who was an advanced graduate student at the time who was learning to supervise in our academic training clinic pushed me to crystallize my thinking about the process and to familiarize myself with the classic and current supervision literature. In terms of specific recommendations for faculty supervisors, I would encourage the incorporation of direct observation of the therapy sessions that are being supervised by the supervisor in training and, when possible, the direct observation of a supervisory session. It is interesting to note that a survey of internship training directors revealed a stronger consensus regarding supervision competencies than there is on effective training models or methods (Reference Rings, Genuchi, Hall, Angelo and CornishRings et al., 2009), suggesting that while there is theory and research to draw from, as a field we have not yet identified a specific and preferred training model for learning to be an ethical and competent supervisor. Hopefully this chapter will provide useful strategies for you to consider as you begin your training in this realm.