Introduction
Tonsillectomy and adenoidectomy have been among the most commonly performed procedures in children for approximately 100 years. These procedures were the first for which Glover discovered large practice variation, in 1938, that could not be explained by differences in patients’ needs.Reference Glover1 Hence, this variation was possibly driven by differences in physicians’ beliefs about the effectiveness of surgery and the lack of high-quality evidence on indications for surgery.Reference Glover1 Glover's report is considered the foundation of research on practice variation. Therefore, the study of practice variation in small areas is still referred to as the Glover phenomenon.Reference White2
Four decades later, John E Wennberg resumed the study of geographical practice variation, using the first population-based hospital discharge database in the USA.Reference White2,Reference Wennberg and Gittelsohn3 Wennberg is also the founder of the Dartmouth Atlas Project, which aims to provide data on practice variation for the general public. The results on medical practice variation raised inescapable questions about the effectiveness and quality of healthcare, and about treatment indications, as regional intervention rates did not necessarily correspond with disease incidences.Reference Goodman4 One of the central concerns is over-utilisation of procedures, as it is thought that this results in higher costs without a clinical benefit per se for patients.Reference Wennberg, McPherson and Caper5,Reference Wennberg6
Evidence on the appropriate indications and effectiveness of these procedures improved over time, resulting in new international guidelines.Reference Paradise, Bluestone, Bachman, Colborn, Bernard and Taylor7–Reference van den Aardweg, Boonacker, Rovers, Hoes and Schilder11 It is presumed that these efforts have reduced the magnitude of regional practice variation for these procedures.Reference Goodwin12
This study aimed to investigate whether better evidence and new guidelines have indeed reduced practice variation. We provide a historical perspective on practice variation in tonsillectomy and adenoidectomy among children. We also provide the history of professional consensus on indications for these procedures and on their effectiveness. Our hypothesis was that stricter indications for tonsil surgery over time resulted in reduced practice variation and thereby improved quality of care, as Wennberg predicted.Reference Goodwin12
Materials and methods
We performed a narrative review of the literature to provide a historical account of practice variation in tonsil surgery. The search was performed by a trained librarian (JWS) on a broad scope of databases (Appendix 1). Additional information was obtained from books in the Walaeus Library (Library of Leiden University Medical Center). Data collection and the screening of eligible books and articles was performed by one author (JJCMvM). Lastly, we screened ‘grey literature’, as government documents that are not indexed might focus on practice variation as well.
We included articles that focused on practice variation in paediatric tonsillectomy or adenoidectomy rates. For tonsillectomies, we included investigations of practice variation in children up to age 18 years. For adenoidectomies, we did not impose this restriction as adenoidectomy is rarely performed in adults. We excluded articles that were not published in the English language. Data were collected on the following: year of publication, region, level of variation (hospital level, physician level, national level), methods for standardisation or adjustment of practice variation outcomes, and the actual outcomes of practice variation.
Results and discussion
Changes in indications for tonsil surgery in children
The very first report of partial tonsil surgery dates from 700 BC, and was found in the Hindu Sanskrit document Atharva-Veda.Reference McNeill13 Subsequently, the first adenoidectomy was described in 1867, after the invention of the laryngoscopy mirror.Reference Meyer14 Over time, indications changed, but, until the twentieth century, adenotonsillectomy (tonsillectomy with or without adenoidectomy) was relatively uncommon. Furthermore, it had already been reported that an operation is rarely necessary as children generally outgrow their complaints.Reference Glover1
Despite this knowledge, the numbers of adenotonsillectomies increased tremendously after the invention of anaesthesia and antiseptic techniques, and after the development of focal infection theory, as it was believed that local infections could cause systemic diseases in any part of the body.Reference Grob15–Reference McCulloch, Taylor, Sasako, Lovett and Griffin17 Consequently, an adenotonsillectomy was considered a cure for a variety of disorders early in the twentieth century, such as anorexia, rheumatism, nephritis, mental retardation and enuresis.Reference Bluestone18
In response to the consequent increase in adenotonsillectomies, the first studies on the effectiveness of adenotonsillectomies were published.Reference Layton19 In 1963, the first randomised, clinical trial comparing adenotonsillectomy to watchful waiting in children was published, which concluded that surgical treatment was effective for recurrent pharyngitis and otitis media.Reference McKee20
The focal infection theory was largely forgotten after the introduction of modern treatments, such as antibiotics.Reference Bansal, Rastogi and Vineeth21 Consequently, by the late 1960s, tonsillectomy was predominantly performed to prevent acute tonsillitis, rather than to prevent secondary streptococcal infections throughout the body.Reference Dwyer-Hemmings22
Obstructive sleep apnoea (OSA) was subsequently described as a new indication for adenotonsillectomy, as tonsil and adenoid hypertrophy is thought to be the most common cause of this condition.Reference Grob15,Reference Marcus, Moore, Rosen, Giordani, Garetz and Taylor23,Reference Ray and Bower24 Although it is one of the most common indications for surgery now, the latest Cochrane Review found that the evidence on the effectiveness of adenotonsillectomy in children with OSA was only of moderate quality.Reference Venekamp, Hearne, Chandrasekharan, Blackshaw, Lim and Schilder25
Several RCTs reported an overall benefit of adenoidectomy for the resolution of middle-ear effusion in children, with only small benefits to hearing and without any clear advantage in terms of treatment of acute otitis media.Reference van den Aardweg, Schilder, Herkert, Boonacker and Rovers26 However, no evidence was found regarding the effectiveness of adenoidectomy for recurrent or chronic nasal symptoms in children.Reference van den Aardweg, Schilder, Herkert, Boonacker and Rovers27 In 2011, a trial on this topic reported similar outcomes, and higher healthcare and societal costs, for adenoidectomy compared to watchful waiting.Reference van den Aardweg, Boonacker, Rovers, Hoes and Schilder11,28,Reference Boonacker, van den Aardweg, Broos, Hoes, Schilder and Rovers29 During an international consensus conference in 2017 on the management of otitis media with effusion (OME), it was advised that adenoidectomy only be performed in children aged over four years who suffer from OME with symptomatic adenoid hypertrophy.Reference Simon, Haggard, Rosenfeld, Jia, Peer and Calmels30
In 1984, specific indications for tonsillectomy in children with severe tonsillitis were defined, known as the Paradise criteria, and international consensus was reached on this topic.Reference Paradise, Bluestone, Bachman, Colborn, Bernard and Taylor7 According to these criteria, surgery is indicated for children aged 3–15 years who experienced at least seven episodes of tonsillitis during the previous year, or at least five episodes per year during the previous two years, or more than three episodes per year during the previous three years. Although those criteria are widely used, even for adults, the study had important limitations, such as the small number of subjects, cross-overs between treatment arms of subjects and the lack of blinding.
At the beginning of the twenty-first century, two trials that included children who did not fulfil the severe tonsillitis criteria reported no major benefit and higher costs of performing an adenotonsillectomy compared to watchful waiting, which led to stricter indications for surgery.Reference van Staaij, van den Akker, Rovers, Hordijk, Hoes and Schilder10,Reference van den Aardweg, Boonacker, Rovers, Hoes and Schilder11,28,Reference Buskens, van Staaij, van den Akker, Hoes and Schilder31 These recommendations were implemented in international guidelines (Table 1).28,32–Reference Randel35
Table 1. Indications for tonsillectomy and adenoidectomy by evidence-based guidelines
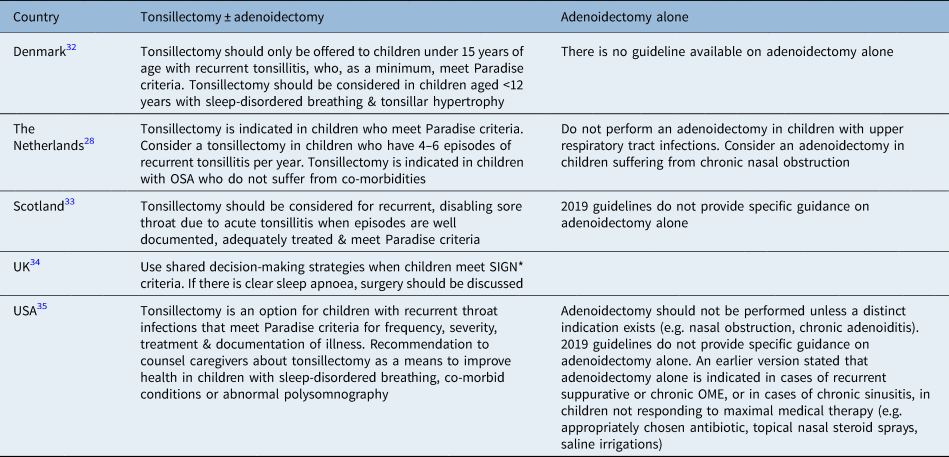
*According to the Scottish Intercollegiate Guidelines Network (‘SIGN’) criteria, sore throats should be due to tonsillitis, with five or more tonsillitis episodes per year, with the patient having had symptoms for at least a year, and the episodes should be disabling and prevent normal function. OSA = obstructive sleep apnoea; OME = otitis media with effusion
All current guidelines for tonsillectomy are still based on the Paradise criteria. Three out of five guidelines do not provide recommendations for adenoidectomy alone. In addition to the evidence on the lack of effectiveness for some children, it has been suggested that removal of the tonsils might increase long-term risks of later respiratory, allergic and infectious diseases in the adult.Reference Byars, Stearns and Boomsma36
Variation outcomes
In total, this review included 21 articles on practice variation in tonsil surgery rates.Reference Glover1,Reference Glover37–Reference Haapkylä, Karevold, Kvaerner and Pitkäranta56 Fifteen articles focused on regional practice variation in tonsillectomy rates, with or without adenoidectomy. Five papers focused on regional practice variation in adenoidectomy rates alone. Seven articles adjusted rates for age and sex, and four articles stratified rates by age, sex or insurance status.
Variation in tonsillectomy rates in Europe
Nine articles studied practice variation in tonsillectomy rates in Europe, covering the years from 1938 to 2014.Reference Glover1,Reference Glover37–Reference Weeks, Paraponaris and Ventelou44
As mentioned before, Glover was the first to report tremendous variations in age- and sex-specific tonsillectomy rates, between 1932 and 1938, among children living in similar neighbourhoods and having similar illnesses, which he explained in terms of variation in medical opinion (Table 2).Reference Glover1,Reference Glover37–Reference Weeks, Paraponaris and Ventelou44,Reference McPherson, Wennberg, Hovind and Clifford57,Reference Appleby, Raleigh, Frosini, Bevan, Gao and Lyscom58
Table 2. Papers on practice variation for tonsillectomy in Europe
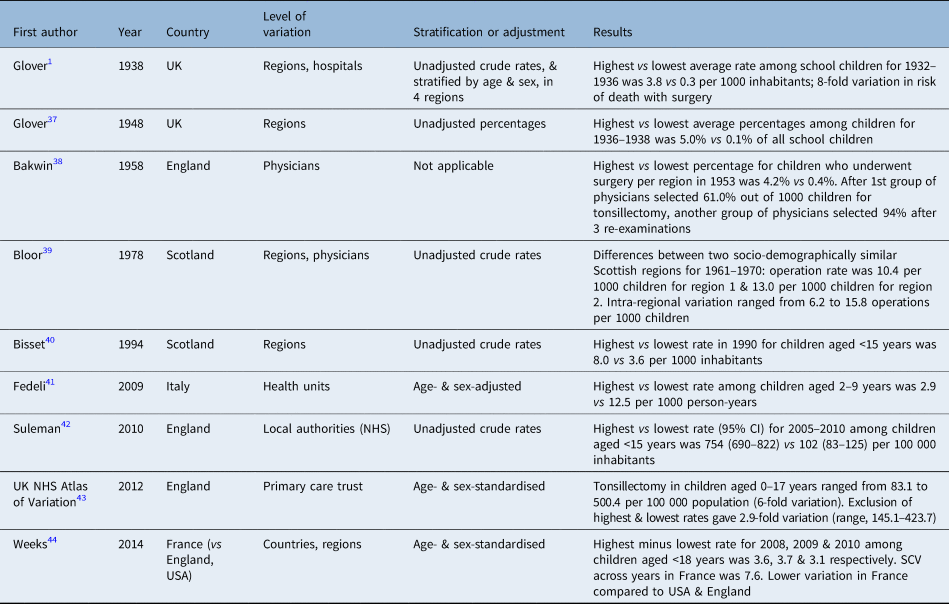
Systematic component of variation (‘SCV’): less than 3 indicates low variation; more than 5 indicates differences in practice styles or medical discretion; more than 10 indicates very high variation.Reference McPherson, Wennberg, Hovind and Clifford57,Reference Appleby, Raleigh, Frosini, Bevan, Gao and Lyscom58 NHS = National Health Service; CI = confidence interval
In 1958, even more striking variation was reported in the selection of children.Reference Bakwin38 While a first group of physicians selected 61 per cent of 1000 children for tonsillectomy, another group of physicians selected 94 per cent of these children after three re-examinations. ‘Snoring due to enlarged tonsils’ was mentioned in that publication, although interrupted breathing was not yet described.
After these publications, many studies examined European regional variation in tonsillectomy rates among children, and found a decrease in regional variation compared to the variation observed by Glover. For example, two-fold differences between operation rates and referral patterns were found between two Scottish regions and the physicians within the same region, over the years 1961 to 1970, and again for the year 1990.Reference Bloor, Venters and Samphier39,Reference Bisset and Russell40 This small difference between regions might be explained by the increasing attention to indications for tonsillectomy during that period.Reference Wennberg and Gittelsohn3,Reference Paradise, Bluestone, Bachman, Colborn, Bernard and Taylor7
Unfortunately, in later years, large regional practice variation in surgical rates was again observed in European countries.Reference Fedeli, Marchesan, Avossa, Zambon, Andretta and Baussano41–Reference Weeks, Paraponaris and Ventelou44
Variation in tonsillectomy rates in other countries
This section concerns practice variation in tonsillectomy rates, with or without adenoidectomy, in other countries. In 1973, Wennberg was the first to resume the study on small-area variation in tonsillectomy rates outside of Europe, after the publication of Glover's findings in 1938.Reference Wennberg and Gittelsohn3,Reference Wennberg6 These publications actually opened the era of practice variation research. Although large variation was observed, he did not specifically focus on tonsillectomy in children.
Six articles included in this review investigated paediatric tonsillectomy rates in the USA, Canada and Australia, published between 1977 and 2016.Reference Roos, Roos and Henteleff45–Reference Harounian, Schaefer, Schubart and Carr50 Practice variation in paediatric tonsillectomy in the USA was not researched until 2012 (Table 3). Despite new evidence and guidelines for children with milder disease by that time, high practice variation between regions in the USA was observed between 2012 and 2016, suggesting that variation in paediatric tonsillectomy care remains problematic.Reference Boss, Marsteller and Simon49,Reference Harounian, Schaefer, Schubart and Carr50 The latest paper from the USA focused on the variation in complication rates as well as regional variation in rates.Reference Harounian, Schaefer, Schubart and Carr50 Tonsillectomy rates were purported to relate to many factors, including social economic status, insurance status, levels of urbanisation and access to healthcare.Reference Boss, Marsteller and Simon49
Table 3. Papers on practice variation for tonsillectomy outside Europe
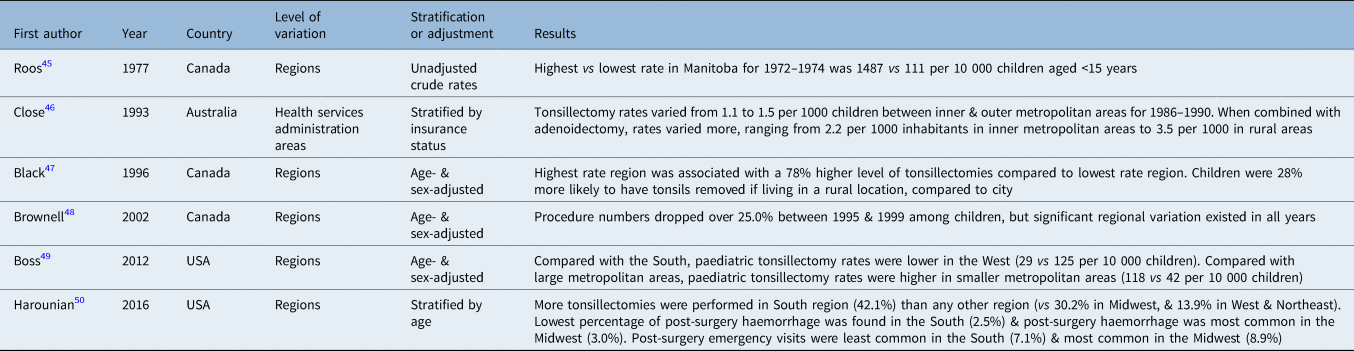
In contrast to the relatively low variation in Europe in the 1960s and 1970s, high variation was observed in all investigated regions in Canada at the time when the Paradise criteria were first published (Table 3),Reference Roos, Roos and Henteleff45 and when updated in 1996 and 2002.Reference Black, Peterson, Mansfield and Thliveris47,Reference Brownell, Kozyrkyj, Roos, Friesen, Mayer and Sullivan48 The 1996 publication was the first to mention OSA as an indication for surgery.
Variation in adenoidectomy rates
Less attention has been paid to regional variation in the rates of adenoidectomy without tonsillectomy (Table 4). In total, we included five papers from five different countries, published between 1977 and 2009.Reference Fedeli, Marchesan, Avossa, Zambon, Andretta and Baussano41,Reference Close, Rushworth, Rob and Rubin46,Reference Bluestone51–Reference Karevold, Haapkylä, Pitkäranta, Nafstad and Kvaerner53
Table 4. Papers on practice variation for adenoidectomy
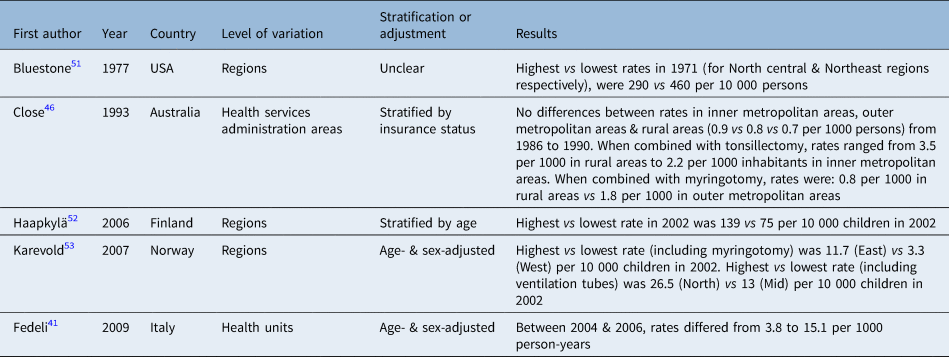
The first paper on adenoidectomy rates was based on data from the USA.Reference Bluestone51 It was reported that adenoidectomy rates varied even more widely than tonsillectomy and adenotonsillectomy rates. In Australia, larger differences were detected between inner metropolitan, outer metropolitan and rural areas, from 1986 to 1990, for tonsillectomy combined with adenoidectomy compared to tonsillectomy alone.Reference Close, Rushworth, Rob and Rubin46 Between 2002 and 2006, more than three-fold differences were found in Italy and Norway as well, whereas in Finland the highest and lowest rates differed less than two-fold.Reference Fedeli, Marchesan, Avossa, Zambon, Andretta and Baussano41,Reference Haapkylä, Karevold, Kvaerner and Pitkäranta52,Reference Karevold, Haapkylä, Pitkäranta, Nafstad and Kvaerner53
However, data on practice variation after the last RCT on the effectiveness of adenoidectomy in children with upper respiratory airway infections, published in 2011,Reference van den Aardweg, Boonacker, Rovers, Hoes and Schilder11 are lacking. The limited data on practice variation in adenoidectomy rates hamper the formulation of definitive conclusions regarding the trial results and guidelines on practice variation.
International variation in tonsil surgery rates
Although Glover referred to other articles, he was the first to report on different international incidence rates, describing tonsillectomy rates as similar in the USA and the UK.Reference Glover1
Three articles included in this review investigated international variation for tonsillectomy and adenoidectomy.Reference Van Den Akker, Hoes, Burton and Schilder54–Reference Haapkylä, Karevold, Kvaerner and Pitkäranta56 An international comparison of paediatric adenotonsillectomy rates reported contrasting results in 1998 (Table 5): rates ranged from 19 cases per 10 000 children in Canada to 118 cases per 10 000 children in Northern Ireland.Reference Van Den Akker, Hoes, Burton and Schilder54 International differences were also reported for paediatric adenoidectomy rates in 1998, which varied from 17 per 10 000 children in Canada to 129 per 10 000 children in Finland.Reference Schilder, Lok and Rovers55 The authors reported high rates in the Netherlands and Belgium as well, but found low rates of antibiotics for acute otitis media in those countries.
Table 5. Papers on international variation for tonsillectomy and adenoidectomy
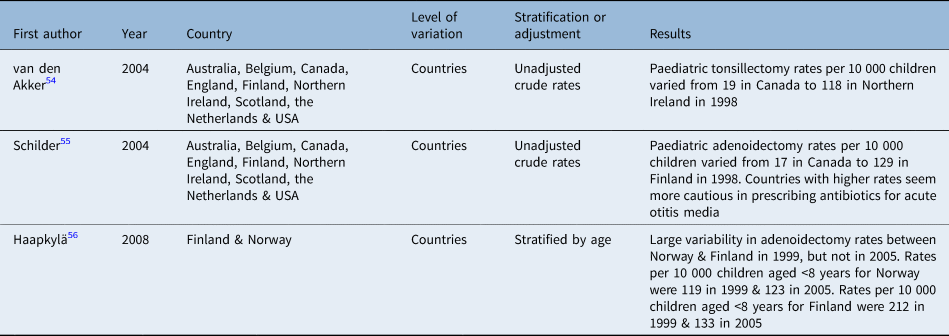
Finally, large variations in the numbers of adenoidectomies were also reported between and within Norway and Finland, from 1987 to 2005.Reference Haapkylä, Karevold, Kvaerner and Pitkäranta56 However, the ‘correct rate’ remained unknown, as differences depend on other factors such as culture, refuge to alternative treatments like antibiotics, the type of healthcare system (easy access to care, high or low costs per person) and socio-economic status, which were not studied in most included articles.Reference McPherson59–Reference de Jong, Groenewegen, Westert, Johnson and Stukel61
Conclusion and future perspectives
This review aimed to provide a historical perspective on practice variation in paediatric tonsil surgery, alongside improved evidence on effectiveness and stricter indications for surgery. Glover, who was the first to publish on practice variation in paediatric adenotonsillectomy rates, would be staggered to know that large geographic variation for these procedures still exists.
The quality of evidence on the effectiveness of tonsil surgery in children has increased considerably during the last century. Guidelines have been developed with indications for surgery that are more evidence-based, and the Paradise criteria still apply after almost forty years.Reference Paradise, Bluestone, Bachman, Colborn, Bernard and Taylor7,Reference Paradise, Bluestone, Colborn, Bernard, Rockette and Kurs-Lasky8,Reference van Staaij, van den Akker, Rovers, Hordijk, Hoes and Schilder10,28,32–Reference Randel35 However, guidelines on adenoidectomy alone are scarce. This might explain the variation in surgical rates, warranting more research on this topic. Furthermore, data for the most recent years are lacking.
Despite new methods to gain insight into the causes of practice variation,Reference Appleby, Raleigh, Frosini, Bevan, Gao and Lyscom58 determination of the optimal procedure rate remains problematic.Reference McPherson59 This is because treatment decisions can be influenced by individual, social and healthcare factors.Reference Birkmeyer, Reames, McCulloch, Carr, Campbell and Wennberg60,Reference de Jong, Groenewegen, Westert, Johnson and Stukel61 These reasons for variation, such as age and socio-economic differences between regions, were not always considered: the described studies evaluated and reported practice variation, but hardly any study was able to correlate explanatory factors with regional variation. Investigation of the explanatory factors might help physicians and decision-makers to better understand methods of tackling unwarranted variation. Future practice variation research should at least adjust for age differences between areas.
It is hard to differentiate between bacterial and viral tonsillitis, as both show similar symptoms. Furthermore, the current guidelines lack objective standards to differentiate between bacterial and viral tonsillitis in primary care. Although more objective tests exist, such as the rapid streptococcal antigen test, cost-effectiveness studies are needed for routine implementation in primary care.Reference Di Muzio, Barucco and Guerriero62,Reference Little, Hobbs, Moore, Mant, Williamson and McNulty63 In addition, the Centor criteria, which differentiate between group A β-haemolytic streptococcus and non-β-haemolytic streptococcus as an underlying cause for tonsillitis, are subjective and are not applicable to the paediatric population.Reference Roggen, van Berlaer, Gordts, Pierard and Hubloue64 Therefore, future research should also focus on diagnostics, such as biomarkers for diagnosis and disease severity, to better inform decision-making.
In conclusion, no evidence has yet been found to demonstrate that the new guidelines and better indications for surgery have reduced practice variation in tonsil surgery. International efforts are needed to reconsider why we are still unable to tackle practice variation in tonsil surgery.
Competing interests
None declared
Appendix 1. Literature search
PubMed
Small area analysis
((“Tonsillectomy”[mesh] OR “tonsillectomy”[tw] OR “tonsillectomies”[tw] OR tonsillectom*[tw] OR “tonsilectomy”[tw] OR tonsilectom*[tw] OR “Adenoidectomy”[mesh] OR “adenoidectomy”[tw] OR “adenoidectomies”[tw] OR adenoidectom*[tw] OR “adenotonsillectomy”[tw] OR adenotonsillectom*[tw] OR “adenotonsilectomy”[tw] OR adenotonsilectom*[tw] OR “tonsil surgery”[tw] OR “tonsils surgery”[tw] OR “Adenoids/surgery”[Mesh] OR (tonsil*[tw] AND (surger*[tw] OR surgical*[tw]))) AND (“Small-Area Analysis”[Mesh] OR “small-area analysis”[tw] OR “practice variations”[tw] OR “practice variation”[tw] OR “geographic variation”[tw] OR “geographic variations”[tw] OR (“Geographic Locations”[mesh] AND “trends”[Subheading]) OR ((“countries”[tiab] OR “country”[tiab] OR geographic*[tiab] OR “international”[ti]) AND (“trends”[Subheading] OR “trend”[tiab] OR “trends”[tiab] OR “difference”[tiab] OR “differences”[tiab] OR “different”[tiab])) OR “Professional Practice/trends”[Mesh]) NOT ((“Adult”[mesh]) NOT (“Infant”[mesh] OR “Child”[mesh] OR “Adolescent”[mesh])))
Historical articles
((“Tonsillectomy”[mesh] OR “tonsillectomy”[tw] OR “tonsillectomies”[tw] OR tonsillectom*[tw] OR “tonsilectomy”[tw] OR “Adenoidectomy”[mesh] OR “adenoidectomy”[tw] OR “adenoidectomies”[tw] OR adenoidectom*[tw] OR “adenotonsillectomy”[tw] OR “adenotonsilectomy”[tw] OR “tonsil surgery”[tw] OR “tonsils surgery”[tw] OR “Adenoids/surgery”[Mesh] OR (tonsil*[tw] AND (surger*[tw] OR surgical*[tw]))) AND (“Child”[Mesh] OR “child”[tw] OR “children”[tw] OR “Infant”[Mesh] OR “infant”[tw] OR “infants”[tw] OR “infancy”[tw] OR “newborn”[tw] OR “newborns”[tw] OR “new-born”[tw] OR “new-borns”[tw] OR “neonate”[tw] OR “neonates”[tw] OR “neonatal”[tw] OR “neo-nate”[tw] OR “neo-nates”[tw] OR “neo-natal”[tw] OR “neonatology”[tw] OR “NICU”[ti] OR “premature”[tw] OR “prematures”[tw] OR “pre-mature”[tw] OR “pre-matures”[tw] OR “preterm”[tw] OR “pre-term”[tw] OR “postnatal”[tw] OR “post-natal”[tw] OR “baby”[tw] OR “babies”[tw] OR “suckling”[tw] OR “sucklings”[tw] OR “toddler”[tw] OR “toddlers”[tw] OR “childhood”[tw] OR “schoolchild”[tw] OR “schoolchildren”[tw] OR “childcare”[tw] OR “child-care”[tw] OR “young”[ti] OR “youngster”[tw] OR “youngsters”[tw] OR “preschool”[tw] OR “pre-school”[tw] OR “kid”[tw] OR “kids”[tw] OR “boy”[tw] OR “boys”[tw] OR “girl”[tw] OR “girls”[tw] OR “Adolescent”[Mesh] OR “adolescent”[tw] OR “adolescents”[tw] OR “adolescence”[tw] OR “pre-adolescent”[tw] OR “pre-adolescents”[tw] OR “pre-adolescence”[tw] OR “schoolage”[tw] OR “schoolboy”[tw] OR “schoolboys”[tw] OR “schoolgirl”[tw] OR “schoolgirls”[tw] OR “pre-puber”[tw] OR “pre-pubers”[tw] OR “pre-puberty”[tw] OR “prepuber”[tw] OR “prepubers”[tw] OR “prepuberty”[tw] OR “puber”[tw] OR “pubers”[tw] OR “puberty”[tw] OR “puberal”[tw] OR “teenager”[tw] OR “teenagers”[tw] OR “teens”[tw] OR “youth”[tw] OR “youths”[tw] OR “underaged”[tw] OR “under-aged”[tw] OR “Pediatrics”[Mesh] OR “Pediatric”[tw] OR “Pediatrics”[tw] OR “Paediatric”[tw] OR “Paediatrics”[tw] OR “PICU”[ti] OR (”child”[all fields] NOT child[au]) OR children*[all fields] OR schoolchild*[all fields] OR “infant”[all fields] OR “infants”[all fields] OR “infancy”[all fields] OR adolesc*[all fields] OR pediat*[all fields] OR paediat*[all fields] OR neonat*[all fields] OR toddler*[all fields] OR “teen”[all fields] OR “teens”[all fields] OR teenager*[all fields] OR preteen*[all fields] OR newborn*[all fields] OR postneonat*[all fields] OR postnatal*[all fields] OR “puberty”[all fields] OR preschool*[all fields] OR suckling*[all fields] OR “juvenile”[all fields] OR “new born”[all fields] OR “new borns”[all fields] OR new-born*[all fields] OR neo-nat*[all fields] OR neonat*[all fields] OR perinat*[all fields] OR underag*[all fields] OR “under age”[all fields] OR “under aged”[all fields] OR youth*[all fields] OR kinder*[all fields] OR pubescen*[all fields] OR prepubescen*[all fields] OR “prepuberty”[all fields] OR “school age”[all fields] OR “schoolage”[all fields] OR “school ages”[all fields] OR schoolage*[all fields] OR “one year old”[ti] OR “two year old”[ti] OR “three year old”[ti] OR “four year old”[ti] OR “five year old”[ti] OR “six year old”[ti] OR “seven year old”[ti] OR “eight year old”[ti] OR “nine year old”[ti] OR “ten year old”[ti] OR “eleven year old”[ti] OR “twelve year old”[ti] OR “thirteen year old”[ti] OR “fourteen year old”[ti] OR “fifteen year old”[ti] OR “sixteen year old”[ti] OR “seventeen year old”[ti] OR “eighteen year old”[ti] OR “1 year old”[ti] OR “2 year old”[ti] OR “3 year old”[ti] OR “4 year old”[ti] OR “5 year old”[ti] OR “6 year old”[ti] OR “7 year old”[ti] OR “8 year old”[ti] OR “9 year old”[ti] OR “10 year old”[ti] OR “11 year old”[ti] OR “12 year old”[ti] OR “13 year old”[ti] OR “14 year old”[ti] OR “15 year old”[ti] OR “16 year old”[ti] OR “17 year old”[ti] OR “18 year old”[ti] OR “two years old”[ti] OR “three years old”[ti] OR “four years old”[ti] OR “five years old”[ti] OR “six years old”[ti] OR “seven years old”[ti] OR “eight years old”[ti] OR “nine years old”[ti] OR “ten years old”[ti] OR “eleven years old”[ti] OR “twelve years old”[ti] OR “thirteen years old”[ti] OR “fourteen years old”[ti] OR “fifteen years old”[ti] OR “sixteen years old”[ti] OR “seventeen years old”[ti] OR “eighteen years old”[ti] OR “2 years old”[ti] OR “3 years old”[ti] OR “4 years old”[ti] OR “5 years old”[ti] OR “6 years old”[ti] OR “7 years old”[ti] OR “8 years old”[ti] OR “9 years old”[ti] OR “10 years old”[ti] OR “11 years old”[ti] OR “12 years old”[ti] OR “13 years old”[ti] OR “14 years old”[ti] OR “15 years old”[ti] OR “16 years old”[ti] OR “17 years old”[ti] OR “18 years old”[ti]) AND (”0001/01/01”[PDAT] : “1950/12/31”[PDAT]))
History of tonsil surgery
(”Tonsillectomy/history”[Mesh] OR ((”Tonsillectomy”[majr] OR “tonsillectomy”[ti] OR “tonsillectomies”[ti] OR tonsillectom*[ti] OR “tonsilectomy”[ti] OR “Adenoidectomy”[majr] OR “adenoidectomy”[ti] OR “adenoidectomies”[ti] OR adenoidectom*[ti] OR “adenotonsillectomy”[ti] OR “adenotonsilectomy”[ti] OR “tonsil surgery”[ti] OR “tonsils surgery”[ti] OR “Adenoids/surgery”[majr] OR (tonsil*[ti] AND (surger*[ti] OR surgical*[ti]))) AND (”History”[majr] OR “history”[Subheading] OR “history”[ti] OR historical*[ti])))
PubMed Central
((”Tonsillectomy”[ti] OR “tonsillectomy”[ti] OR “tonsillectomies”[ti] OR tonsillectom*[ti] OR “tonsilectomy”[ti] OR “Adenoidectomy”[ti] OR “adenoidectomy”[ti] OR “adenoidectomies”[ti] OR adenoidectom*[ti] OR “adenotonsillectomy”[ti] OR “adenotonsilectomy”[ti] OR “tonsil surgery”[ti] OR “tonsils surgery”[ti] OR “Adenoids/surgery”[ti] OR (tonsil*[ti] AND (surger*[ti] OR surgical*[ti]))) AND (”History”[ti] OR “history”[ti] OR historical*[ti]))
IndexCAT
(Title:(Tonsillectomy)) OR Title:(Adenoidectomy)
((Tonsillectomy OR Adenoidectomy OR “tonsil surgery” OR “tonsils surgery”) AND (Child OR children OR Infant OR infants OR Adolescent OR adolescents OR pediatric OR paediatric))
Web of Science (http://isiknowledge.com/wos)
(ts=(”Tonsillectomy” OR “tonsillectomy” OR “tonsillectomies” OR tonsillectom* OR “tonsilectomy” OR “Adenoidectomy” OR “adenoidectomy” OR “adenoidectomies” OR adenoidectom* OR “adenotonsillectomy” OR “adenotonsilectomy” OR “tonsil surgery” OR “tonsils surgery” OR tonsil*) AND ti=(”History” OR historical*))







