A 23-year-old nulliparous woman, a recent immigrant from the Philippines who married a Korean, was referred to our center for close examinations on discordance of body weight between the first and second fetuses, which had developed in the late third trimester at 36+4-week gestation. On routine ultrasound examinations at a local clinic in the first and second trimesters, there were no specific findings. This twin conception was spontaneous. Her obstetric, medical, and familial history was not significant.
Targeted ultrasound examinations (Accuvix XQ, Medison, Seoul, Korea) showed a dichorionic and diamniotic twin pregnancy with definite discordance of estimated fetal weight between the first and second fetuses, weighing 2,500 g (male) and 1,700 g (female), respectively, at 36+4-week gestation. A complete sonolucent center of the lens within the hyperechoic ring on examination of the first fetus was lost in the eyes of the second fetus (Figures 1(a) and (b)). A coronal view of the fetal head revealed relatively echogenic contour of both the ocular lenses of the second fetus (Figure 1(b)). A transverse section of the fetal face at the level of the orbits showed ill-demarcated echogenicity around the junction between the hyaloid artery and the lens (Figures 1(c) and (d)).
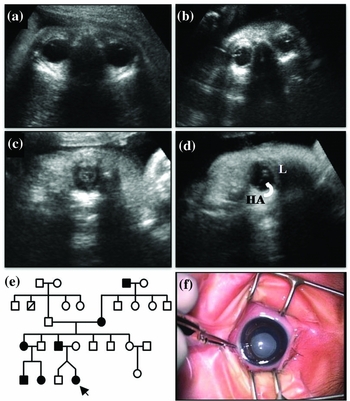
FIGURE 1 A coronal view of the fetal head. (a) Orbits of the first normal fetus (central part of the lens: completely sonolucent). (b) Highly echogenic areas of both the lenses of the second fetus. (c) Transabdominal ultrasound examinations at 36+4-week gestation show hyperechogenicity of the lens surface with irregularity of the left eye of the second fetus. (d) On a transverse image at the level of fetal orbits, an irregular thickness of the boundary between the hyaloid artery (HA, curved arrow)-lens (L) junction (arrow) was noted. The hyaloid artery appeared as a delicate echogenic line connecting the posterior part of the orbit (the optic disc) and the posterior aspect of the lens capsule. (e) Four-generation pedigree. Circles represent females, and squares represent males. Solid symbols indicate affected individuals. The affected female twin is marked with an arrow. (f) Postnatal cataract at 2 months of age. Lamellar opacity immediately after birth was replaced by dense opacity of lens at the time of cataract surgery, which was urged by rapid progression of cataracts.
These findings prompted a pedigree analysis of congenital hereditary cataracts. The father of the affected twin had contributory family history for cataracts. On a four-generation pedigree analysis, we found that the father of the affected twin, his sister with two affected children, his mother, and his maternal grandfather also had early-onset cataracts (Figure 1(e)). The family was unaware of anyone being affected in generations previous to this generation. Maternal serologic tests for toxoplasmosis, rubella, cytomegalovirus, and herpes simplex (TORCH) were carried out and there was no evidence for congenital infection. The genetic sonogram of the second fetus showed no congenital anomalies associated with karyotypical abnormalities.
At 37 weeks, the first baby, male, weighing 2,640 g and the second baby, female, weighing 1,850 g, were born with cesarean section. Apgar scores at the first 1 min and 5 min were 10 points for both the twins. Placenta was dichorionic diamniotic, and weighed 688 g. Both twins were evaluated for congenital cataracts by an ophthalmologist after birth and results were consistent with prenatal findings. In addition, Magnetic Resonance Imaging (MRI) was performed to evaluate abnormal small mass-like lesions around the ocular disc on prenatal ultrasound examinations (no related scan was shown), but failed to find any other associated ocular abnormalities.
Cataracts of the affected twin showed lamellar opacity immediately after birth. In a short time, rapid progression of lens opacity urged an ophthalmologist to remove and replace the cloudy natural lens with a synthetic lens to restore lens’ translucency at two months of age (Figure 1(f)). The major findings of the surgery were that opaque lenses with posterior capsule ruptured and crystalline materials spread into the vitreous body. The final diagnosis was cataracts complicated with posterior lenticonus.
Discussion
Our case demonstrated congenital hereditary cataracts in a dizygotic twin pregnancy with discrepancy in body weight and affected status between two fetuses; one twin, the smaller female, was affected, and the other, the larger male, was unaffected. The principal finding was relatively echogenic areas around ocular lenses rather than advanced opacification of crystalline lens in previously reported cases of congenital hereditary cataracts with no other associated abnormalities (Cengiz & Baxi, Reference Cengiz and Baxi2001; Drysdale et al., Reference Drysdale, Kyle and Sepulveda1997; Monteagudo et al., Reference Monteagudo, Timor-Tritsch, Friedman and Santos1996). Congenital cataracts were mostly presented as homogeneous opacity of the lens and loss of hypoechoic center of the lens within a hyperechoic ring of the normal fetal lens (Bronshtein et al., Reference Bronshtein, Zimmer, Gershoni-Baruch, Yoffe, Meyer and Blumenfeld1991; Cengiz & Baxi, Reference Cengiz and Baxi2001; Drysdale et al., Reference Drysdale, Kyle and Sepulveda1997; Graw, Reference Graw2004; Monteagudo et al., Reference Monteagudo, Timor-Tritsch, Friedman and Santos1996; Pedreira et al., Reference Pedreira, Diniz, Schultz, Faro and Zugaib1999; Reches et al., Reference Reches, Yaron, Burdon, Crystal-Shalit, Kidron, Malcov and Tepper2007; Romain et al., Reference Romain, Awoust, Dugauquier and Van Maldergem1999). However, there are various sonographic features of cataracts in echogenicity and affected location that hinders the diagnosis of congenital cataracts before birth (Monteagudo et al., Reference Monteagudo, Timor-Tritsch, Friedman and Santos1996). In this case, a discrepancy of the affected status between the twins made it possible to compare eyes with the relative thick echogenic contour and irregularly dense inner linear lesions in the affected twin with those in the unaffected twin.
The prenatal diagnosis of congenital cataracts was also facilitated by the identification of persistent hyaloid artery and increased echogenicity of the junction between the lens and the hyaloid artery on a transverse image of the fetal face at the level of the orbits. The hyaloid artery, a branch of the ophthalmic artery, is located within the optic stalk of the eye and extends from the optic disc through the vitreous humor to the lens (Bronshtein et al., Reference Bronshtein, Zimmer, Gershoni-Baruch, Yoffe, Meyer and Blumenfeld1991). The major role of the hyaloid artery is to supply nutrient to the developing fetal lens (Bronshtein et al., Reference Bronshtein, Zimmer, Gershoni-Baruch, Yoffe, Meyer and Blumenfeld1991). An important, unusual feature of the human eye is the spontaneous regression of the hyaloid artery during in utero conversion of the primary vitreous to the secondary adult vitreous (Bronshtein et al., Reference Bronshtein, Zimmer, Gershoni-Baruch, Yoffe, Meyer and Blumenfeld1991). Achiron et al. (Reference Achiron, Kreiser and Achiron2000) reported that timing for the hyaloid artery involution was beyond 29-week gestation. There have been no studies on the usefulness of scrutinizing scans of the hyaloid artery (Achiron et al., Reference Achiron, Kreiser and Achiron2000). In our case, the hyaloid artery's disappearance at 36+4-week gestation was a good indicator in the diagnosis of congenital cataract, which was located posteriorly in the direction of the optic disc. Not all cataracts are progressive (Zetterstrom & Kugelberg, Reference Zetterstrom and Kugelberg2007). While anterior polar cataracts are usually static, cataracts associated with posterior lenticonus, lamellar and subcapsular typically progress, and for better visual prognosis early diagnosis and surgery is critical (Zetterstrom & Kugelberg, Reference Zetterstrom and Kugelberg2007).
A small mass near the optic disc present prenatally was in question. Postnatal MRI failed to reveal nature of the mass. The mass was persistently observed until two months of age. At the time of surgery, there was no tumor-like lesion around the optic disc. The mass was no more a problem after lensectomy and was considered as a fragment detached from the hydrated lens and then spontaneously absorbed into the vitreous humor. Ophthalmologic consultation on ocular abnormalities in the antenatal period by a pediatric ophthalmologist by a pediatric ophthalmologist gives parents more specific details of what can be expected and lessens the nervousness of parents about the unknown future of the affected fetus (Lehman, Reference Lehman2003).
Although congenital cataracts are usually associated with intrauterine infections (i.e., rubella), metabolic disorders, trauma, medication and chromosomal abnormalities, and congenital cataracts may also be inherited as an isolated ocular abnormality (Cengiz & Baxi, Reference Cengiz and Baxi2001; Drysdale et al., Reference Drysdale, Kyle and Sepulveda1997; Monteagudo et al., Reference Monteagudo, Timor-Tritsch, Friedman and Santos1996). Unfortunately, in this study, genetic analysis of distinct gene mutations was not performed. However, recent studies have identified genetic mutations of various encoding proteins leading to congenital inherited cataract (Santana & Waiswo, Reference Santana and Waiswo2011; Sun et al., Reference Sun, Xiao, Li, Guo and Zhang2011). Santana et al. (Reference Santana, Waiswol, Arcieri, Cabral de Vasconcellos and Barbosa de Melo2009) reported a novel mutation in the gamma-D crystallin (CRYGD) gene and an association between a mutation in the alpha-A crystallin (CRYAA) gene and nuclear congenital cataract in Brazilian families. They (Santana et al., Reference Santana, Waiswol, Arcieri, Cabral de Vasconcellos and Barbosa de Melo2009) also suggested that genetic and molecular analyses be considered for prophylactic therapy, including medication of antioxidant, vitamin and carotenoid, diet therapy, and gene therapy.
In high-risk pregnancies with a family history of cataracts, thorough prenatal ultrasound examinations, pedigree and genetic analyses, and ophthalmologic consultation are warranted because timing of surgery is crucial to prevent visual loss.
Acknowledgments
We would like to thank Drs Key Hwan Lim and Young Suk Yu for their participation in the diagnosis and follow-up of this case.



