Mental health disorders are a leading cause of healthcare use1 and medical evacuationReference Cohen, Brown, Kurihara, Plunkett, Nguyen and Strassels2 (removal of an individual from a field or deployment scenario for the purpose of obtaining medical treatment) within the US military. Between 2007 and 2016, depressive disorders were the second most commonly diagnosed mental health disorderReference Stahlman and Oetting3 with 281 829 individuals diagnosed, comprising 16.8% of all mental health diagnoses in the US military. Without diagnosis and treatment, depression is associated with reduced productivity, lower likelihood of promotions, attrition and suicide.Reference Hoge, Auchterlonie and Milliken4,Reference Kessler, Heeringa, Stein, Colpe, Fullerton and Hwang5 Suicide rates in the US military began rising in the mid-2000s and have exceeded civilian suicide rates since 2008.Reference Kuehn6–Reference Reger, Pruitt and Smolenski9 In both the US civilian and military populations, depression is associated with younger age, female gender, low educational attainment and income, and living alone; younger age and female gender being prominent risk factors.Reference Stahlman and Oetting3,Reference Bromet, Andrade, Hwang, Sampson, Alonso and de Girolamo10 Following military service, 70% of military veterans will exclusively use civilian medical facilities,11 so civilian providers should be aware of these risk factors among this population.
Few data are available regarding depression across the shipboard deployment cycle. Recent data show that over 20% of personnel may be at risk for moderate-to-severe depression at the time of deployment.Reference Harbertson, Hale, Michael and Scott12 Shipboard personnel do not undergo a Pre-Deployment Health Assessment like their shore-based counterparts, so early identification may be reduced in this population. This study examines risk factors associated with screening positive for depression among US Navy and Marine Corps personnel in the 12 months before deployment, during deployment and 3 months after returning from a shipboard deployment.
Method
Sampling, recruitment and data-collection methods were previously described in Harbertson et al. Reference Harbertson, Scott, Moore, Wolf, Morris and Thrasher13 Briefly, longitudinal data were collected from US Navy and Marine Corps personnel via an anonymous, self-administered paper questionnaire between February 2012 and August 2014. Pre-deployment data were collected within 2 weeks of deployment; deployment data within the last 4 weeks of deployment; and post-deployment data 3 months after return from deployment (plus or minus 2 weeks). The pre-deployment questionnaire assessed behaviour in the previous 3 months, year, and ever; the deployment questionnaire assessed behaviour during the entire deployment; and the post-deployment questionnaire assessed behaviour since returning from deployment. The questionnaire included questions on demographics, sexual behaviours, alcohol use and mental health. For analysis, individuals were excluded if age or gender data were missing and were included if they completed the Center for Epidemiologic Studies Depression Scale (CES-D) at two or more time points.Reference Radloff14
All questionnaires were completed anonymously. Questionnaires were linked using a series of eight linking questions,Reference Grube, Morgan and Kearney15–Reference DiIorio, Soet, Van Marter, Woodring and Dudley17 birth year, gender and ship number. Questionnaires with the same answer to 9 of the 11 questions we considered to be the same individual and were linked. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human participants were approved by Naval Health Research Center Institutional Review Board (NHRC.2010.0033) and Walter Reed Army Institute of Research Human Subjects Protection Branch (WRAIR #1766). Written informed consent was obtained from all participants.
Measures
The primary outcome was screening positive for depression. Scoring the CES-D included in the survey, individuals were classified as at risk for depression (ROD) with a score of 16 or higher and at risk of major depressive disorder (ROMDD) with a score of 22 or higher.Reference Radloff14,Reference Klinkman, Coyne, Gallo and Schwenk18 Alcohol use was assessed using the Cut down, Annoyed, Guilty, Eye-opener (CAGE)Reference O'Brien19 questionnaire, the abbreviated Alcohol Use Disorders Identification Test (AUDIT-C),Reference Bush, Kivlahan, McDonell, Fihn and Bradley20 drinks per week/day/occasion and binge drinking. Individuals screened positive on the CAGE questionnaire if they answered yes to two or more questions, and they screened positive for dependent alcohol use on the AUDIT-C with a score of 8 or more. Drinks per week/day/occasion were used to classify individuals as heavy, moderate-heavy, moderate, light or non-drinkers using criteria from the Department of Defense Health Related Behaviors Survey (HRBS).21
If an individual reported being single in a committed relationship, single living with a partner, or married, they were categorised as being in a relationship. If an individual said they had previously been diagnosed with a depressive disorder, an anxiety disorder, post-traumatic stress disorder, combat stress reaction or a traumatic brain injury, they were categorised as having a previous diagnosis with a mental health condition of interest. A life stress inventory based on a modified Holmes-Rahe Stress ScaleReference Holmes and Rahe22 and HRBS was included. Because of the changes to the original scale, the inventory was not scored, but variables that indicated the presence of one or more stressor or the total number of stressors were included in the analysis.
Data analysis
Descriptive statistics, including percentages, means and s.d. were calculated to describe the entire study population. All bivariate and multivariable analyses were conducted for the full population and for the population stratified by age or gender. Generalised estimating equations were used to calculate odds ratios (OR), 95% CI and P-values for these analyses, with P<0.05 considered statistically significant. A sensitivity analysis was conducted to compare the study population with the longitudinal cohort, all participants who completed more than one questionnaire, regardless of whether or not they completed the CES-D.
Demographics,Reference Bromet, Andrade, Hwang, Sampson, Alonso and de Girolamo10,Reference Rao, Feinglass and Corrigan23 mental health,Reference Kessler, Berglund, Demler, Jin, Koretz and Merikangas24 alcohol useReference Grant and Harford25 and substance misuseReference Grant26 were considered risk factors analysed for their association with screening positive for depression. Variables were selected for inclusion in the final model based on their significance in the bivariate analysis. Variables with the highest P-values were eliminated manually using backwards elimination or replaced with another variable describing the same risk factor. All analyses were conducted using SAS software version 9.3 (SAS Institute Inc, Cary, NC, USA).
Results
In total, 773 participants completed the survey at two or more time points. Two people were excluded because their age or gender data were missing, and 173 were excluded because they did not complete the CES-D portion of the questionnaire at two or more time points, leaving a final sample size of 598 available for analysis (Table 1). Sensitivity analysis found that the study population was not significantly different from the longitudinal cohort (data not shown). The majority were men (71.2%), White (59.3%) and had completed less than an undergraduate degree (84.4%). The average age was 26.3 years (s.d. = 6.5, median 24). Most were in one of two categories: ‘single, not in a committed relationship’ or ‘married’ (31.7 and 37.7%, respectively). Average length of service was 5.4 years (s.d. = 5.6, median 3) and 77.7% had completed at least one official deployment.
Table 1 Demographic characteristics of personnel responding to at least two questionnaires and completing the Center for Epidemiologic Studies Depression Scale
GED, General Education Development test
a. Data only collected pre-deployment.
b. Data collected pre- and post-deployment; post-deployment information used for those without pre-deployment information.
During deployment, a greater proportion of respondents screened positive for ROD (60.1 v. 52.0% at T 1 and 51.4% at T 3; P = 0.01, P = 0.01) and ROMDD (32.4 v. 27.2% at T 1 and 26.4% at T 3; P = 0.06, P = 0.07) (Fig. 1 and supplementary Fig. 1 available at https://doi.org/10.1192/bjo.2019.70). A significantly greater proportion of women and respondents under 25 years old screened positive for ROMDD and ROD than those over 25 and men.
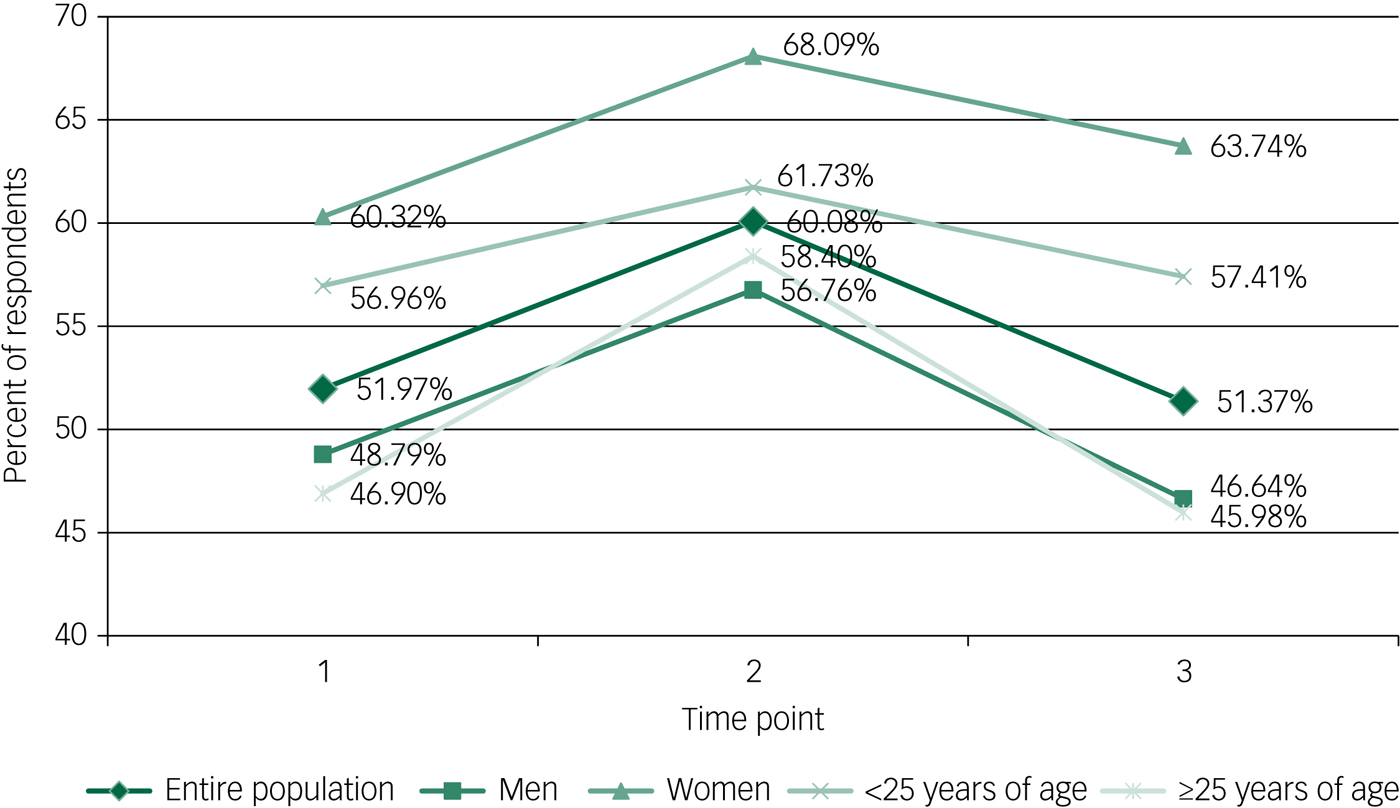
Fig. 1 Percent of respondents at risk for depression by time point.
Bivariate analysis
In unadjusted analysis, younger age and female gender were associated with screening positive for ROD (supplementary Table 1). Other factors associated with increased odds of screening positive for ROD included Hispanic/Latino ethnicity, screening positive for alcohol misuse, prior mental health conditions or having a recent stressful life experience in both the combined and stratified study populations. Lower odds of screening positive for ROD were observed among those reporting an undergraduate degree or higher, or officer or warrant officer rank in the combined study population as well as in the male-only and 25 year and over stratified analyses. Reporting being in a relationship or deploying one or more times were also associated with significantly lower odds of screening positive for ROD in the combined study population.
Multivariable analysis
Many factors associated with screening positive for ROD remained significant in multivariable regressions (Table 2, supplementary Tables 2–5). For the entire study population, older age was associated with lower odds of screening positive for ROD (OR = 0.95, 95% CI 0.91–0.98). Female gender (OR = 1.61 95% CI 1.05–2.46), prior diagnosis with a mental health condition of interest (OR = 2.58, 95% CI 1.42–4.65) and experiencing at least one stressful event (OR = 1.82, 95% CI 1.21–2.74) were significantly associated with screening positive for ROD (Table 2). Screening positive on the CAGE (OR = 1.80, 95% CI 1.05–3.08) and moderate-heavy to heavy drinking (OR = 1.47, 95% CI 1.03–2.11) had a slightly weaker association but were still significantly associated with ROD.
Table 2 Longitudinal model describing risk factors for screening positive for depression among all respondents
Results in bold are significant.
N/A, not applicable; CAGE, Cut down, Annoyed, Guilty, Eye-opener.
Among female participants (supplementary Table 2), being in the 21–22 and 23–24 year old age groups (OR = 11.98 (95% CI 2.91–49.36) and 8.18 (95% CI 2.13–31.35), respectively), experiencing at least one stressful event (OR = 3.59, 95% CI 1.54–8.34), and reporting Black race (OR = 2.78, 95% CI 1.22–6.30), one (OR = 3.24, 95% CI 1.33–7.88) or two or more (OR = 4.56, 95% CI 1.77–11.77) previous deployments, and prior diagnosis with an anxiety disorder (OR = 2.72, 95% CI 1.09–6.80) were significantly associated with screening positive for ROD.
Among male respondents (supplementary Table 3), consuming alcohol in the previous 12 months (OR = 3.11, 95% CI 1.43–6.80), screening positive on the CAGE (OR = 2.79, 95% CI 1.49–5.24) and prior diagnosis with a mental health condition of interest (OR = 3.11, 95% CI 1.43–6.80) were associated with screening positive for ROD. Although there was no association with having a recent stressful experience, those with more stressful experiences were somewhat more likely to screen positive for ROD (OR = 1.18, 95% CI 1.08–1.29). Those who were single but living with a partner (OR = 0.32, 95% CI 0.13–0.76) or married (OR = 0.46, 95% CI 0.24–0.89) had lower odds of screening positive for ROD.
Among those aged 24 years and younger (supplementary Table 4), being female (OR = 3.17, 95% CI 1.65–6.09) and having a recent stressful experience (OR = 2.36, 95% CI 1.28–4.38) were more likely to screen positive for ROD. The association between moderate-heavy to heavy drinking (OR = 1.71, 95% CI 1.00–2.90) and likelihood to screen positive for ROD was significant but weaker than the other associations.
Among participants ≥25 years of age (supplementary Table 5), participants who were Hispanic/Latino (OR = 2.52, 95% CI 1.02–6.24) or had a prior diagnosis with a mental health condition of interest (OR = 3.86, 95% CI 1.67–8.91) had higher odds of screening positive for ROD. Those who had experienced more stressful events also had somewhat higher odds of screening positive for ROD (OR = 1.20, 95% CI 1.08–1.33). Those who were single but living with a partner (OR = 0.29, 95% CI 0.09–0.97), married (OR = 0.35, 95% CI 0.14–0.86), or divorced, separated, or widowed (OR = 0.22, 95% CI 0.06–0.83) were less likely to screen positive for ROD than those who were single.
Discussion
Younger personnel, women, people who screened positive for alcohol misuse, people previously diagnosed with a mental health condition of interest and those who had experienced one or more stressful events had higher odds of screening positive for ROD. Black race or Hispanic ethnicity and being single was associated with screening positive for ROD in women and those 25 years or older. Among women only, more deployments were associated with screening positive for ROD.
A substantial proportion of participants screened positive for ROD or ROMDD, with the highest prevalence reported during deployment. The prevalence of screening positive for ROD or ROMDD is higher than observed in previous studies among US military personnel.Reference Hoge, Auchterlonie and Milliken4,Reference Kessler, Heeringa, Stein, Colpe, Fullerton and Hwang5,Reference Shen, Arkes and Lester27,Reference Vasterling, Proctor, Aslan, Ko, Jakupcak and Harte28 These previous studies were generally conducted immediately post-deployment and used different criteria for determining ROD. Between May 2003 and April 2004, 4.5% of US Army and Marines personnel returning from Operation Iraqi Freedom (OIF) gave one positive response on the Patient Health Questionnaire-2, and 19.1% had any mental health concern.Reference Hoge, Auchterlonie and Milliken4 A longitudinal study of enlisted personnel returning from OIF beginning in 2003 found that 36.5% of respondents had a score between 9 and 26 on the CES-D 12 months post-deployment.Reference Vasterling, Proctor, Aslan, Ko, Jakupcak and Harte28 From October 2009 to March 2013, 7% of all respondents completing their first Pre-Deployment Health Assessment screened positive for ROD.Reference Shen, Arkes and Lester27 Among non-deployed Army personnel in 2011, 4.8% were found to have ROMDD in the previous 30 days.Reference Kessler, Heeringa, Stein, Colpe, Fullerton and Hwang5 The highest proportion among these studies, 36.5%, was obtained using less stringent scoring requirements than our study and remains substantially lower than the 50.1% screening positive for ROD post-deployment, the most comparable time point. The characteristics associated with screening positive for ROD within this population, such as younger age and female gender, mirror those in the broader US military population and the US civilian population,Reference Stahlman and Oetting3,Reference Hasin, Sarvet, Meyers, Saha, Ruan and Stohl29 but the proportion of this study's population screening positive for depression is much higher. The lowest prevalence for the entire study population was 51.4% at T 3 whereas only 8.1% of the entire US population over 20 screened positive for a moderate ROD between 2013 and 2016.Reference Brody, Pratt and Hughes30
This discrepancy could be caused by a number of factors. The study population is younger and has a higher proportion of women than the general US military and US Navy populations.31 However, the proportion of men and individuals aged 25 years and older screening positive for ROD were still higher when compared with studies among the US military or civilian populations.Reference Hoge, Auchterlonie and Milliken4,Reference Kessler, Heeringa, Stein, Colpe, Fullerton and Hwang5,Reference Shen, Arkes and Lester27–Reference Hasin, Sarvet, Meyers, Saha, Ruan and Stohl29 Screening studies among US college students have found the proportion of students screening positive for ROD to be between 23.5 and 38.5%.Reference Wilson, Bohnert, Ambrose, Davis, Jones and Magee32–Reference Wolanin, Hong, Marks, Panchoo and Gross34 Among study participants under 25 years of age, 57% screened positive for ROD at T 1. The difference may be because of unmeasured factors or quite possibly the deployment itself, particularly given the stress associated with a sudden change of status. That the proportion screening positive for ROD increased dramatically during deployment and returned to pre-deployment levels after returning supports the idea that deployment may contribute to ROD. Although similar stresses to deployment may be experienced by first-year college students, few studies stratified their results by student year. In the one that did, a higher proportion of first years screened positive for ROD than did other years, although this proportion (34.9%) was still lower than that of this study's population.Reference Wilson, Bohnert, Ambrose, Davis, Jones and Magee32 A study of shipboard military personnel in the UK found that they also reported mental health issues more frequently than personnel on land-based deployments,Reference Whybrow, Jones, Evans, Minshall, Smith and Greenberg35 which further suggests that shipboard deployments themselves may contribute to screening positive for ROD.
In stratified analysis, women with one or more deployments, prior anxiety disorder or identification as Black race were associated with higher prevalence of screening positive for ROD. In addition, among those 25 years of age or older, identification of Hispanic/Latino status was also associated with ROD. In military populations, socioeconomic status is largely determined by rank, although there are complex relationships between rank and other variables, including race and ethnicity.31 However, non-socioeconomic factors, including differential attitudes towards mental health and care seeking or social stresses, may also contribute to the association of race and ethnicity and depression in this population. Prior deployment history or prior anxiety disorder history could serve as screening questions to identify higher risk women for appropriate treatment.
Screening positive on the CAGE questionnaire (men) or moderate/heavy drinking (under 25) was associated with screening positive for ROD. The CAGE questionnaire is intended to detect alcoholism, which is strongly associated with ROD as both a potential cause and symptom.Reference Grant and Harford25 Alcohol misuse is associated with a variety of issues of concern to the military and civilian community (motor vehicle accidents, productivity loss, dependency and many others)Reference Brown, Bray and Hartzell36 so targeting these groups for alcohol use interventions could result in health improvements beyond depression risk. Similarly, because the association between depression and alcohol is bidirectional, reducing ROD could result in less alcohol use with similar benefits. Also, the association between prior depression diagnosis and current screen positive for ROD could be used to screen for high-risk men.
Strengths and limitations
Although there was a sizeable proportion of individuals who did not complete their CES-D screen, the anonymous voluntary survey likely encouraged truthful reporting. However, the absence of identifiers may have led to missed or incorrect linkage, reducing or biasing the longitudinal study population and limiting our ability to detect correct associations. We used convenience sampling techniques to capture the greatest number of participants, and logistic constraints did not allow universal enrolment on each ship. However, we approached and recruited participants from every department, with intent to generate a diverse sample. Approximately one-quarter of the individuals in the linked data-set did not complete the CES-D, which could generate bias. However, the group who completed the CES-D is demographically very similar to the entire study population.
The CES-D has comparable diagnostic validity to other depression screening tools.Reference Brown, Bray and Hartzell36 The cut-off score of 16 may identify false positives,Reference Shean and Baldwin37 but inclusion of the major depressive disorder screening likely improves specificity. The entire study population has a greater proportion of personnel under 25 and women than the US Navy or US military at large, which are high-risk groups for depression.31 Although this affects generalizability to other populations, it is still likely generalisable to other shipboard populations and may apply to other services across any deployment or similar young civilian populations undergoing prolonged sequestration, such as dormitory college students.
Implications
The large proportion of people screening positive for ROD merits further attention. The numbers and associations found regarding depression over the shipboard deployment cycle highlight a need for mental health services. A return to a pre-deployment proportion screening positive for ROD following deployment suggests that deployment may not have a permanent effect on mental health. However, the pre- and post-deployment proportions screening positive for ROD are still higher than seen in comparable military population in similar circumstances.Reference Cohen, Brown, Kurihara, Plunkett, Nguyen and Strassels2,Reference Shen, Arkes and Lester27,Reference Vasterling, Proctor, Aslan, Ko, Jakupcak and Harte28 Even if the mental health effects from deployment are temporary, addressing mental health concerns during deployment are still necessary for this population's overall health and well-being. More intensive mental health resources could be targeted to high-risk groups throughout the deployment cycle. Interventions shown to be effective among land-based deploying military personnel, such as secondary screening to ensure that individuals on a psychotherapeutic medication are on a stable dose and have enough doses for the duration of the deployment, could be added to pre-deployment screenings for high-risk groups before shipboard deployment.Reference Warner, Appenzeller, Parker, Warner and Hoge38 One-on-one interventions, such as cognitive–behavioural therapy, are logistically unrealistic during a shipboard deployment; however, telemedicine sessions could be intermittently available to continue or initiate care with land-based providers.Reference Hilty, Ferrer, Parish, Johnston, Callahan and Yellowlees39 In the military, leadership behaviour to encourage social engagement and target faulty perceptions of isolation have been shown to improve unit cohesion.Reference Vasterling, Proctor, Aslan, Ko, Jakupcak and Harte28 Other programmes such as group cognitive–behavioural therapy, exercise and mindfulness have demonstrated some effectiveness at treating or preventing the onset of depressive symptoms.Reference Resick, Wachen, Dondanville, Pruiksma, Yarvis and Peterson40–Reference Farb, Anderson, Ravindran, Hawley, Irving and Mancuso42 Further research is needed to assess the effectiveness and feasibility of such interventions in a shipboard deployment cycle.
In conclusion, this study found that, although the risk factors associated with screening positive for ROD were similar to civilian and other military populations, the proportion of military personnel that screened positive for ROD throughout the shipboard deployment cycle exceeded prevalence reported among other military populations and civilians. This suggests that shipboard deployment presents particular stressors to mental health or that unknown factors associated with shipboard deployment may increase likelihood of depressive symptoms. Future studies should explore the benefit of adding a brief mental health screeningReference Shean and Baldwin37 or including the pre-deployment health assessment survey for shipboard populations to identify those most at risk for depression and ensure they have adequate medication plans and counselling support during deployment. Implementation of evidence-based interventions feasible in such isolated settings as described previously could be explored in follow-on studies.
Funding
This work was supported by a cooperative agreement (W81XWH-07-2-0067) between the Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc., and the US Department of Defense, under Work Unit No. 60546.
Acknowledgements
Additional analyses and publication drafts are in development. Data are not available to outside investigators at this time.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjo.2019.70.






eLetters
No eLetters have been published for this article.