Internationally, the prevalence of children born with congenital heart defect (CHD) is estimated at 8–10 per 1000. Reference Van, Konings and Slager1 In Malaysia, with the calculation of 500,000 children born per annum, at least 4000–5000 children are estimated to be born with CHD every year. 2 However, with the advancement in imaging, surgery, and relevant technology and skills sparked hope for a cure for the continuously growing number of adolescents and adults diagnosed with CHD, Reference Marelli, Mackie, Ionescu-Ittu, Rahme and Pilote3,Reference Stoutz and Leventhal4 leading to the heightened interest in the issues, experiences, and quality of life of these patients.
A myriad of challenges faced by adolescents with CHD affects their well-being such as experience of physical complications, Reference Brickner, Hillis and Lange5 mental health concerns, Reference Kovacs, Saidi and Kuhl6 relationship issues with family and peers, Reference Pahl and Grady7 adjustment issues in lifestyles, Reference Viner8 and issues in health care. Reference Pahl and Grady7 A number of studies have suggested the services of formal Adolescent Transition to Adulthood programmes Reference Hays9–Reference Said, Driscoll and Dearani15 as a way to promote well-being amongst adolescents with CHD, prevent discontinuity of care, and reduce mortality and morbidity. Unfortunately, these programmes are not widely available. Reference McPheeters, Davis, Taylor, Brown, Potter and Epstein16 Even in the United States of America, only 5% of state mental health administrators reported the availability of transition services or programmes. In Malaysia, most adolescent health programmes focused on HIV/AIDS prevention. Reference Jaafar, Mohd Noh and Muttalib17 No intervention programme provided for adolescents with CHD goes beyond physical health needs.
In the next several sections, we would present subsequent sections as follows: (1) Review of existing transition interventions; (2) Development of the “HeartBEAT” ATPP; and (3) Mixed-methods pilot testing of “HeartBEAT” ATPP.
Review of existing transition interventions
The current review synthesises empirical literature on the Adolescent Transition Program for adolescents with CHD, published between the year 2015 and 2019. Non-CHD programme and programme without empirical finding is excluded. Nine-hundred and ninety-seven articles on the Adolescent Transition Program for adolescents with CHD were identified and screened through Google Scholar. In the initial phase, 779 irrelevant researches, 55 conceptual papers and guidelines, 25 review papers, and 83 papers involving patients with multiple/other medical conditions were excluded from the analysis. Out of 55 full-text articles assessed for eligibility, only 8 papers fit into the criteria for the analysis. Forty-seven articles were excluded as they were the papers assessing the needs of the programme or their target population was medical staff.
From the synthesis of these eight articles, Reference Acuña Mora, Sparud-Lundin, Bratt and Moons18–Reference Mackie, Rempel and Kovacs25 four main dimensions, which were theoretical framework, delivery, methodology, and main finding, were analysed.
In the perspective of theoretical framework, only three out of eight researches specified the theories they used. Bandura’s self-efficacy theory was applied in the self-management efficacy promotion programme, as it is an important intrinsic motivation that contributes to self-management. Reference Lee and Jung23 Another research conducted by Acuna Mora and team (2017) used the British Medical Research Council Model as the research model in developing the programme. Reference Acuña Mora, Sparud-Lundin, Bratt and Moons18 Another programme named as resilience improvement programme, conducted by Lee and colleagues (2016) identified five key psychosocial protective factors in the programme, which were (1) positive emotions, (2) cognitive flexibility, (3) meaning, (4) social support, and (5) active coping styles. Reference Lee, Lee and Choi24 As for other articles, none of the theoretical frameworks could be identified.
The review data indicated a variation in the delivery of the programme. Three programmes developed and evaluated a single educational session as Adolescent Transition Program. Reference Goossens, Van Deyk, Zupancic, Budts and Moons20–Reference Ladouceur, Calderon and Traore22 As for Mackie et al (2018) and Charles et al (2016), they applied two educational sessions and assessed their effectiveness, and suggested that 40% of these adolescents are required for further intervention after that. Reference Charles, Rempel and Rogers19,Reference Mackie, Rempel and Kovacs25 Mora and colleagues (2017) proposed the programme to include three outpatient visits and one information day before the transit to adult services. Last but not least, a resilience improvement programme is a 1-day programme, with six sessions Reference Lee, Lee and Choi24 and the recent self-management efficacy promotion programme lasted for 6 weeks. Reference Lee and Jung23 Most of these Adolescent Transition Programs were led by nurses (transition coordinators or specialised nurses).
There was a variation in the aspect of methodology. Six papers used the quantitative research design. Lee and colleagues applied a non-equivalent control group pretest–posttest study in years 2016 and 2019. Reference Lee and Jung23,Reference Lee, Lee and Choi24 Mackie and others (2018) implemented a cluster randomised clinical trial as their research design. One group pre- and posttest design was used in three different programmes. Reference Goossens, Van Deyk, Zupancic, Budts and Moons20–Reference Ladouceur, Calderon and Traore22 One paper applied the qualitative design, Reference Charles, Rempel and Rogers19 and one was still in a planning stage. Reference Acuña Mora, Sparud-Lundin, Bratt and Moons18
In general, most Adolescent Transition Programs highlighted positive outcomes in different areas. Lee and colleagues (2019) found their programme significantly improved patients’ disease-related knowledge and self-management performance, but not health-related quality of life. A similar finding was reported by Mackie and team (2018) research, stating a significant improvement in CHD knowledge and self-management skills in relation to the programme. The result of Ladouceur et al. (2017) showed that structured CHD education and higher academic attainment were significant factors in determining health-related knowledge. Goossens et al (2015) found that his programme significantly improved CHD knowledge, but not health behaviours. A research from Hartman Valles et al (2015) had a similar finding in CHD knowledge as well.
On the other hand, 1-day resilience improvement programme measured on different outcomes, indicated the improvement in resilience in adolescents with CHD, but no difference in their quality of life. Qualitative researches done by Charles et al (2016) reported 40% of adolescents still required further intervention after the two educational programmes provided. No finding was identified in the research of Acuna Mora et al (2017). Reference Acuña Mora, Sparud-Lundin, Bratt and Moons18
Based on the analysis above, several gaps were identified. First, a number of papers did not specify theoretical frameworks as a basis of the Adolescent Transition Program. There were inconsistencies in programme delivery and methodology of these papers. Moreover, most ATP programme measured on CHD knowledge and self-management skills, but not focusing on other mental health/psychosocial elements. It might be because ATP was a nurse-led programme and lack of involvement from psychosocial professionals.
Theoretical framework of the programme
The current study uses a shared management model proposed by Kieckhefer and Trahms (2000) and Antonovsky’s Salutogenic model, specifically sense of coherence, as a theoretical foundation of the “HeartBEAT” ATPP.
The idea of shared management model is to develop a therapeutic alliance amongst the patients with chronic illness, their family, and healthcare providers, guiding the children to become independent and healthy adults. During infancy, the healthcare providers hold a major responsibility in providing treatments, whereas the parent/family provides care and the patient receives the care. Moving to the children stage, the responsibilities have shifted to the parent/family to manage the patient’s situation. Reaching the stage of adolescent/adulthood, these patients shall learn to take charge of their illness. Reference Kieckhefer and Trahms26
Sense of coherence, the main concept in the Salutogenic model, has been frequently proven to contribute to adolescents with CHDs’ well-being and quality of life. It consists of three components, which are comprehensibility, manageability, and meaningfulness. Comprehensibility is the cognitive aspect of sense of coherence. It is defined as an understanding of what has happened in their life as clear, predictable, and in order. Reference Antonovsky27 Manageability is defined as sense of control towards their life. With high manageability, individuals would welcome challenges in their life, and believe they have sufficient instrumental and behavioural resources to deal with challenges successfully. Reference Antonovsky27 Lastly, meaningfulness is the motivational aspect of sense of coherence and emotional aspect of comprehensibility component. Antonovsky (1987) defined it as the understanding of life events in an emotional way and the extent of the life condition is worthy of commitment and involvement.
Conceptual framework of the programme
Referring to the shared management model, Reference Kieckhefer and Trahms26 Antonovsky’s Salutogenic model, Reference Antonovsky27,Reference Antonovsky28 and results from need analysis as the theoretical foundation, the conceptual framework of the programme was developed, as shown in Fig 1. Generally, adolescents with CHD faced with stressors/challenges derived from CHD and currently managing with their coping strategies could be buffered by the “HeartBEAT” ATPP (intervening variable) to improve their self-management on illness and life, and their social support.

Figure 1. Conceptual framework of the present study.
Development of the “HeartBEAT” ATPP
The sources for programme development are from the need analysis, two theoretical frameworks, and conceptual framework. The acronym of the “HeartBEAT” are as follows:
-
(Heart): Heart;
-
(B): Be;
-
(E): Empowered;
-
(A): Adolescent;
-
(T): Transition.
Programme design
For programme description, Frechtling (2007)’s logic model was used as a framework to describe the ATPP. Reference Frechtling29 From initial qualitative need assessment, the patients suggested a programme designed to equip them with self-management skills on illness and life, and to gain more social support. Thus, programme objectives and learning outcomes of the “HeartBEAT” ATPP are developed as stated in Table 1.
Table 1. Programme objectives and learning outcomes of the “HeartBEAT” ATPP

The “HeartBEAT” ATPP consists of a 2-day face-to-face programme and six sessions of online support groups, conducted by mental health professionals and doctors. Two days face-to-face programme enables the youths to build rapport with other patients and learn the knowledge and skills through practical activities. Meanwhile, six sessions of online support groups enable the trainers to monitor the patients’ progress and to provide them emotional support. The session plans are shown in Tables 2 and 3.
Table 2. Face-to-face programme schedule
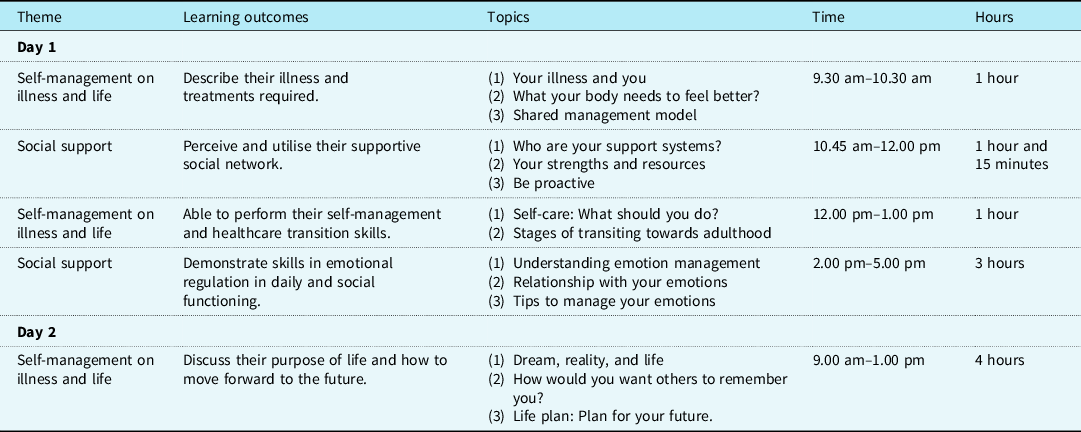
Table 3. Online support groups schedule

The training manual of the programme was created to ensure standardisation of practice amongst mental health professionals. Next, three experts were invited to conduct meta-evaluation on the conceptual framework, description of the programme, programme evaluation plan, and training manual. The expert review was conducted based on six steps of the expert review process proposed by Tessmer (1993) to ensure the content was suitable and beneficial to the adolescents. Reference Tessmer30 Last but not least, a 1-day training was conducted for five mental health professionals before the formal ATPP was implemented.
Mixed-methods pilot testing of “HeartBEAT” ATPP
Methods and materials
To examine the impact of the programme, a mixed-method design was implemented. For quantitative method, a one-group pretest–posttest design was used to evaluate the short-term impact of the interventions. Reference Martin31 The qualitative method, on the other hand, is a specifically phenomenological study, Reference Creswell32 which enabled researchers to get more details about the development and improvement of self-management skills before and after the programme.
The present researches were reviewed and approved by the IJN ethics committee and IIUM ethics committee. All trials and activities were conducted according to the Malaysian Guidelines for Good Clinical Practice to ensure the rights, integrity, and confidentiality of the respondents are protected.
Several measures were used to evaluate the effectiveness of the programme, both quantitative and qualitative. Leuven Knowledge Questionnaire of Congenital Heart Defects was used to measure knowledge on illness and treatments. It had 27 items and included 5 dimensions, which were disorder and treatment, prevention of complications, physical activity, sexuality and heredity, and contraception and pregnancy. Reference Yang, Chen, Wang, Gau, Chen and Moons33 The instrument showed high content validity, with generally over > .78 item content validity index and > .90 scale content validity index. Reference Yang, Chen, Wang, Gau, Chen and Moons33
Self-management and transition skills were assessed by STARx Questionnaire. It was an 18-item self-report assessment on the self-management and transition skills in adolescents with a chronic medical condition. There were six subscales involved, which were medication management, provider communication, engagement during appointments, disease knowledge, adult health responsibilities, and resource utilisation. Reference Cohen, Hooper and Javalkar34 The instrument was developmentally sensitive and proven to have high reliability and validity. Reference Ferris, Ms and Haberman35
Social support was measured by Medical Outcome Study Social Support Survey. It was a 19-item survey to assess the level of social support of the patients. It also included four subscales, including emotional/informational support, tangible support, affectionate support, and positive interactions. Reference Sherbourne and Stewart36 MOS-SSS was found to have high reliability, which was over .91. The convergent and discriminant validity of the survey was also ranged from .69 to .82. Reference Sherbourne and Stewart36
As for qualitative measures, interview protocols were developed to assess the patient’s life plan and capacity to manage emotions. To ensure the reliability and validity of the questions, all the interview protocols had to be reviewed by three subject matter and audience experts in the related field to ensure that these questions were suited to qualitative inquiry, patients’ educational and cultural context, abled to achieve objectives, and fulfilled ethical and legal standards.
Patients
A criterion sampling was used to select these patients. Reference Palys37 The inclusion criteria were the patients should be between 16 and 19 years old, presented with moderate and severe types of CHD, did not have genetic, developmental, and mental disorders, were not home bounded/hospital bounded due to illness, and presented with at least an average intellectual functioning. The diagnosis, gender, age, and ethnicity of the patients are listed in Table 4.
Table 4. Demographic characteristics of the patients

Initially, 14 patients were enrolled in the programme. However, after 4 months into the programme, only eight patients successfully completed the online support group and face-to-face sessions. Therefore, the results were based on these eight patients, which had reached the standard of Morse, Denzin and Lincoln (1994) who stated that at least three–six samples were required if the data of these respondents were repeated and collected in a qualitative design. Reference Morse38
Data analysis
Dependent sample t-test was deployed to assess the general effectiveness of the programme. For qualitative method, Moustakas’s (1994) phenomenological data analysis was applied to systematically identify the essence of the patient’s experience in the programme by using Atlas.ti version 8. Reference Creswell32,Reference Moustakas39
Results
Knowledge on illness and treatments
There was a significant difference in the scores of adolescents’ knowledge on their own illness and treatments required before the ATPP and after the ATPP. These findings suggested that the ATPP had significantly improved patients’ understanding towards their illness and treatments required.
Self-management and transition skills
The finding reported that even though there was a difference in patients’ self-management and healthcare transition skills before and after the ATPP, the difference was not significant, as shown in Table 5.
Table 5. The findings of pre- and posttest on knowledge on illness and treatments, self-management and transition skills, social support, and its subscales

Social support
The score of pretest in affectionate support had significantly increased posttest. Specifically, it indicated that the adolescents with CHD perceived that they received more love and care after the ATPP.
There were no significant differences for other types of support including the overall social support, emotional/informational support, tangible support, and positive social interaction where they had no significant differences between pretest and posttest, as shown in Table 5.
Purpose of life
The results showed that all the patients (n = 8) were able to identify their purpose of life and had a brief idea on how to achieve their life plans. The common themes on their life plans were to have a normal life, study, and work. They defined “normal life” as able to live as people without illness and have gone through life stages such as study, work, and get married. Below are the thoughts from PT 7.
Matlamat hidup yang saya inginkan adalah apabila saya besar nanti, saya boleh hidup dengan normal sebagaimana orang-orang yang biasa, yang tidak berpenyakit seperti saya. Itulah, saya ingin hidup secara sihat, secara sejahtera, dan berkeluaga yang bahagia.
(The life goal that I want to achieve is when I grow up, I want to live a normal life just as the others who are healthy without the disease. That is, I want to live healthy, live well and raise a happy family.)
Other than focusing on their own survival and having a normal life, some patients’ life goals were related to their family and helping others. They have fought the illness because they did not want their family members to be worried about them. On top of that, they wanted their family to be proud that what they have gone through and their efforts in achieving their life goals. Within their limits, they also wished to help others. Below are the views from PT4 and PT3.
Better than sekarang, Jangan buat orang sekeliling risau, bantu orang lain dan bahagia.
(I want to better than now, and I don’t want to make people surround me worried. I would like to help others and I want to live happily.)
Emotion regulation
Most patients were able to share their coping strategies after the programme, which included distracting themselves from negative emotions, thinking positively, trying to understand situations and solving problems, and getting social support. Amongst the coping strategies, social support was the most common strategy mentioned, followed by trying to understand situations and solving issues, and trying to distract themselves from negative emotions. Below are some comments given by PT6 and PT5.
Tumpu kepada perkara lain untuk distract tumpuan. Kita jangan asyik fikir sakit jantung kita, cari perkara lain untuk distract kita.
(Focus on other things to distract the focus. We do not want to keep thinking about our heart disease, look for other things to distract us. Also look for a doctor to get advice and help with this issue.)
Kita cuba motivate balik diri seperti membaca kisah-kisah cancer survivor dan bagaimana mereka mengatasi masalah mereka. Macam orang lain boleh fight, kami juga boleh fight.
(We can try to motivate us by reading some cancer survivor’s article. Understand that how they overcome their issue. They can fight their illness, I think we can fight it too.)
Impressions of the programme
Referring to general impressions of patients and staff participating in the programme, they expressed satisfaction with the programme. To make the “HeartBEAT ATPP a better program, both patients and mental health professionals provide recommendations for both face-to-face sessions and online support group sessions. For improvement in face-to-face sessions, they wish to have more interaction with patients and mental health professionals from other groups, and to involve their parents in the programme. For improvement in online support groups, they wish to reduce the duration of online support groups, reduce some jargon (self-compassion), and to use other apps for online sessions. One of the mental health professionals also suggested to further group the patients based on the nature of their commitment, whether they are currently studying or working. She justified her recommendation since it was difficult to set a common time for the online support groups if these patients have different work and school schedules.
Discussion
This section first compares the finding of current preliminary study with other papers and discuss potential contribution factors, followed by limitation of the study and recommendation for future programme/studies, and end with an implication of the study.
The findings show that adolescents with CHD have significantly improved in the knowledge relating to their illness and treatment plan. However, even though there was an increase in self-management and healthcare transition skills, the difference was not significant. A similar result was shown in Yang and others’ research (2013). They had conducted a research on 116 adolescents with CHD, and the result showed that they scored 38.8% on average. Reference Yang, Chen, Wang, Gau and Moons40
There are several factors that might contribute to these knowledge gaps of adolescents with CHD. Yang et al (2013) found that parents’ level of knowledge significantly affected the understanding of the patients of their own illness. Ironically, the research also pointed out that the parents’ knowledge on their children’s disease was also insufficient.
Another factor is the lack of proper education programme for the adolescents from trained personnel. In the Malaysian cultural context, our patients voiced out that normally medical staff tended to communicate only to the caregivers and expected the caregivers to deliver the message to the patients, instead of directly communicating with the patients. Thus, the adolescents with CHD were not sure of the progress of their illness, and only followed the instructions of the parents and medical staff in taking care of themselves.
As for non-significant findings in self-management skills, parents might need to go through their own transition period in providing independence to their adolescents. Thus, the progress of self-management skills might not be as quick as expected. Other potential barriers could be parent’s hyper-responsibility Reference Dellafiore, Pittella and Flocco41 and the Malaysian collective culture of parenting styles. Reference Keshavarz and Baharudin42 Shackleford, Minick and Kelley (2017) proved that setting goals to envision a future could assist adolescents with CHD to achieve a better quality of life. Reference Shackleford, Minick and Kelley43 This is in keeping with the similar results in our findings, particularly while exploring how the patients were able to achieve the life goals they set. One of the themes that were often highlighted was to take good care of their own health. This proves the effectiveness of ATP in increasing their motivation of self-management through identifying their life goals.
Looking at the findings of social support, the results showed that the patients had a relatively high overall social support even before the programme. Family characteristics and affectionate support are important factors in perceived social support and quality of life. Reference Tak and McCubbin44,Reference Tye, Kandavello and Gan45 In ATPP, all the parents of these adolescents with CHD were supportive of this programme and willing to send them to attend the course, despite the distance and financial involvement. Some parents even frequently reminded the patients to commit to the online support group, so that they were able to benefit from the programme.
The current preliminary findings showed that all the patients (n = 8) were able to identify their emotions, demonstrate coping strategies, and identify their social support during health deterioration. ATP served as a secure and less threatening platform for these adolescents to discuss their possible health deterioration and was aware that they were not the only patients who had such concerns. Moreover, mental health professionals were available to ensure their coping strategies were healthy and adaptive.
Limitation and recommendation of the study
The key limitations of the current project were small sample size, limited criteria of respondents (moderate-to-severe CHD and without any genetic disorders and mental illness), and high dropout rate. Low sample size (and thus low statistical power) might contribute to a lack of significance. Testing this intervention in a randomised controlled trial with a larger sample in the future would help investigate this.
Common reasons provided by those adolescents and parents not to include or drop out from the programme include tight schedule and distance issues for face-to-face sessions. Minority felt that they were already equipped with sufficient knowledge and skills. There are other potential challenges, such as patients who reluctant to know more about their illness, and patients with poor social supports.
To increase retention of the patients and recommend for a larger study in the future, the researchers suggested modifying the intervention in a few areas. First, a face-to-face session might need to be conducted in an individual session rather than in-group as it was challenging to fit the schedule for all the patients. Second, this current research applied close group (a fixed number of group members completed the programme) on both face-to-face sessions and online support groups. The researchers are considering changing some session into an open group, so that new members can join in and to ease patients’ time management issue.
Implication and summary of the study
In general, the ATPP has significantly increased the patients’ knowledge in their illness, treatment plan, and self-management. All the patients were able to identify their purpose of life and direction in the future after the ATPP. However, the increase in their self-management and healthcare transition skills is not significant.
The current paper and past literature suggest that the patients’ knowledge of their own illness and self-management is relatively low. Reference Yang, Chen, Wang, Gau and Moons40,Reference Van Deyk, Pelgrims and Troost46 Thus, it is imperative to include healthcare policies and clinical guidelines that all adolescents with CHD should go through a proper Adolescent Transition Program or a similarly relevant programme to prevent complications that might arise due to ignorance and lack of self-care. The timing of referral and the characteristics of the patients should be included in the programme and clearly stated to maximise the outcome of the programme.
The current findings on self-management skills also imply the need to have a programme for the parents of adolescents with CHD to smoothen the transition process, reduce their anxiety and tendency of overprotection, and to assist the teenagers and parents to support each other. Individual and family counselling could be performed if the patients are identified as having other major issues and are not ready or unsuitable to participate in the ATPP.
Acknowledgements
The authors would like to show our gratitude to the adolescents with CHD, their parents, and healthcare providers who took part in this study and appreciate the contribution of the Pediatric and Congenital Heart Center, Institut Jantung Negara, in assisting us to recruit the respondents. We would also like to thank the IJN Foundation for financial support, and the Department of Psychology, Kulliyyah of Islamic Revealed Knowledge and Human Sciences for their kind support. Special thanks to Tye Chong Aun, Cheng Eng Mooi, Tye Sue Wei, and Goh Soo Ling for their moral support.
The conclusion and opinions expressed here are those of the authors and not necessarily those of the funder.
Financial support
This research partly received the research funding from the IJN Foundation.
Conflicts of interest
Two authors are the employees at Institut Jantung Negara.
Ethical standards
The study was reviewed, evaluated and approved by IJN (Institut Jantung Negara) Ethics Committee (IJNEC) and the IIUM Research Ethics Committee (IREC).









